Development of resistance against linezolid, an alternative drug for the therapy of multidrug-resistant tuberculosis (2), was assessed to be rare (5). We aimed to generate linezolid-resistant Mycobacterium tuberculosis strains from 10 different, fully susceptible M. tuberculosis parental strains. Ten linezolid-resistant colonies could be isolated from six different parental strains. The frequency of the in vitro appearance of linezolid-resistant mutants was 2 × 10−8 to 5 × 10−9. Previous investigations with a genetically engineered Mycobacterium smegmatis derivative that harbored only one of the original two copies of the rrn operon revealed a similar rate of 4.5 × 10−9 (6).
MIC value determination gave identical results performed with both Bactec 460 TB system and Bactec MGIT 960 (Becton Dickinson Diagnostic Systems, Sparks, MD). MIC values of the linezolid-resistant strains varied from 4 to 32 μg/ml, whereas all parent strains had MIC values of ≤1 μg/ml.
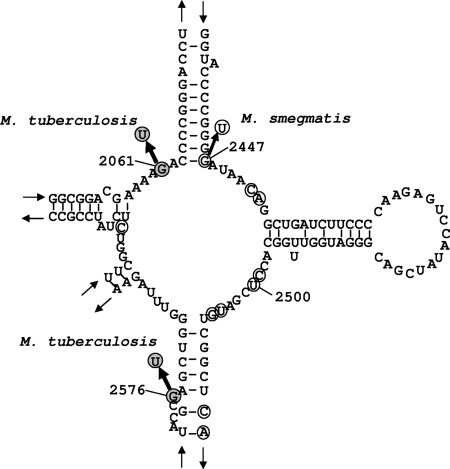
Genotypic characterization of the linezolid-resistant strains was performed by sequencing of the 23S rRNA gene (5). Overall, in five strains mutations in the 23S rRNA gene were found. Four strains (derived from three different parental strains) with a MIC value of 32 μg/ml showed an identical G-to-T base pair exchange at position 2061; another strain with a MIC value of 16 μg/ml showed a G-to-T base pair exchange at position 2576 (Fig. 1). As a control, the respective parental strains had no alteration in the 23S rRNA gene when aligned with the M. tuberculosis H37 wild-type sequence. The remaining five strains with MIC values from 4 to 8 μg/ml showed no mutations in the 23S rRNA gene.
FIG. 1.
Secondary structure of the central loop of domain V of M. tuberculosis 23S rRNA (modification of the structures presented in references 6 and 7). The base exchanges determined in the in vitro-selected linezolid-resistant M. tuberculosis strains are indicated (dark gray circles). Nucleotides that are putatively associated with linezolid resistance in Halobacterium halobium, Enterococcus faecalis, Enterococcus faecium, and M. smegmatis are also included (circles).
To investigate whether in vitro-generated linezolid resistance influences the growth rate, suspensions of parental susceptible and resistant strains were inoculated into MGIT tubes (0.1 ml of a 1:100 dilution of a McFarland 0.5 suspension). The average time to detection (TTD) of parental strains was 5.93 ± 1.84 days (mean ± standard deviation). Linezolid-resistant strains without mutation in the 23S rRNA showed a TTD of 5.81 ± 1.81 days. However, linezolid-resistant strains with mutations in the 23S rRNA showed an elevated TTD of 10.10 ± 3.49 days.
The isolated M. tuberculosis mutants can be divided into two classes corresponding to in vitro-generated linezolid-resistant M. smegmatis clones (6). In that study, one class showed wild-type growth characteristics in cultures, lower MIC values of 4 to 8 μg/ml, and no mutation in the 23S rRNA, pointing to a nonribosomal mechanism of resistance (6). Mutants of the other class had alterations in domain V of 23S rRNA, high MIC values of ≥64 μg/ml, and a decreased growth rate in culture. In contrary to the study by Sander et al., who found exclusively G2447T mutations in M. smegmatis, different mutations were found in M. tuberculosis and other bacterial species (1, 3, 4). Whereas the G2576T mutation is well known and often described as the predominant mutation in various other gram-positive bacteria, such as Enterococcus faecalis and Staphylococcus aureus (3, 4, 7), to our knowledge the G2061T mutation found in four M. tuberculosis strains is described here for the first time.
Acknowledgments
We thank, K. Ott, F. Schaefer, and I. Radzio, Forschungszentrum Borstel, Germany, for excellent technical assistance.
Footnotes
Published ahead of print on 10 December 2007.
REFERENCES
- 1.Carsenti-Dellamonica, H., M. Galimand, F. Vandenbos, C. Pradier, P. M. Roger, B. Dunais, M. Sabah, G. Mancini, and P. Dellamonica. 2005. In vitro selection of mutants of Streptococcus pneumoniae resistant to macrolides and linezolid: relationship with susceptibility to penicillin G or macrolides. J. Antimicrob. Chemother. 56:633-642. [DOI] [PubMed] [Google Scholar]
- 2.Fortún, J., P. Martín-Dávila, E. Navas, M. J. Pérez-Elías, J. Cobo, M. Tato, E. Gómez-G. De la Pedrosa, E. Gómez-Mampaso, and S. Moreno. 2005. Linezolid for the treatment of multidrug-resistant tuberculosis. J. Antimicrob. Chemother. 56:180-185. [DOI] [PubMed] [Google Scholar]
- 3.Meka, V. G., and H. S. Gold. 2004. Antimicrobial resistance to linezolid. Clin. Infect. Dis. 39:1010-1015. [DOI] [PubMed] [Google Scholar]
- 4.Prystowsky, J., F. Siddiqui, J. Chosay, D. L. Shinabarger, J. Millichap, L. R. Peterson, and G. A. Noskin. 2001. Resistance to linezolid: characterization of mutations in rRNA and comparison of their occurrences in vancomycin-resistant enterococci. Antimicrob. Agents Chemother. 45:2154-2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richter, E., S. Rüsch-Gerdes, and D. Hillemann. 2007. First linezolid-resistant clinical isolates of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 51:1534-1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sander, P., L. Belova, Y. G. Kidan, P. Pfister, A. S. Mankin, and E. C. Böttger. 2002. Ribosomal and non-ribosomal resistance to oxazolidinones: species-specific idiosyncrasy of ribosomal alterations. Mol. Microbiol. 46:1295-1304. [DOI] [PubMed] [Google Scholar]
- 7.Xiong, L., P. Kloss, S. Douthwaite, N. M. Andersen, S. M. Swaney, D. L. Shinabarger, and A. S. Mankin. 2000. Oxazolidinone resistance mutations in 23S rRNA of Escherichia coli reveal the central region of domain V as the primary site of drug action. J. Bacteriol. 182:5325-5331. [DOI] [PMC free article] [PubMed] [Google Scholar]