Abstract
Mycobacterium leprae DNA gyrases carrying various mutations, previously described in clinical strains, were investigated for quinolone susceptibility by inhibition of supercoiling and DNA cleavage promotion. We demonstrated that the gyrA mutations leading to G89C or A91V confer fluoroquinolone resistance whereas the gyrB mutation leading to D205N does not.
Mycobacterium leprae still causes serious chronic disease, and treatment may fail because of poor drug adherence and emergence of resistance (4, 10, 11, 13, 18, 19). Fluoroquinolones are new drugs for the treatment of leprosy (6, 8-10, 16), but their use can lead to acquired quinolone resistance in M. leprae (4, 11, 13). DNA gyrase, a heterotetramer (GyrA2GyrB2) enzyme solving DNA topological problems associated with DNA replication, transcription, and recombination (5), is the sole target of quinolones in M. leprae (7).
M. leprae has the longest doubling time (∼14 days) among bacteria and cannot be cultivated in vitro (12). Consequently, the only way to test antibiotic activity is the mouse footpad leprosy model, which is labor intensive and expensive and requires 8- to 12-month experiments (12). Therefore, our aim was to evaluate the consequences of the DNA gyrase mutations described in M. leprae clinical strains (4, 11, 13) on the quinolone inhibition of DNA gyrase as a prerequisite for the development of rapid genetic susceptibility tests. We demonstrated that the GyrA G89C and A91V alterations are implicated in resistance to quinolones whereas the GyrB D205N alteration is not.
Plasmids carrying M. leprae genes gyrA and gyrB containing the mutations corresponding to the GyrA G89C or A91V (4, 13) and GyrB D205N (11) alterations were generated from the respective wild-type gyrA and gyrB genes of M. leprae cloned previously (14), with the QuikChange site-directed mutagenesis kit (Stratagene). For the oligonucleotides used for mutagenesis, see Table S1 in the supplemental material. Wild-type and modified GyrA and GyrB proteins were purified as described previously (14). DNA supercoiling and DNA cleavage experiments were carried out as described previously (1, 2, 14). Nalidixic acid, oxolinic acid, ofloxacin, moxifloxacin, gatifloxacin, and garenoxacin were from Sigma or from the respective laboratories.
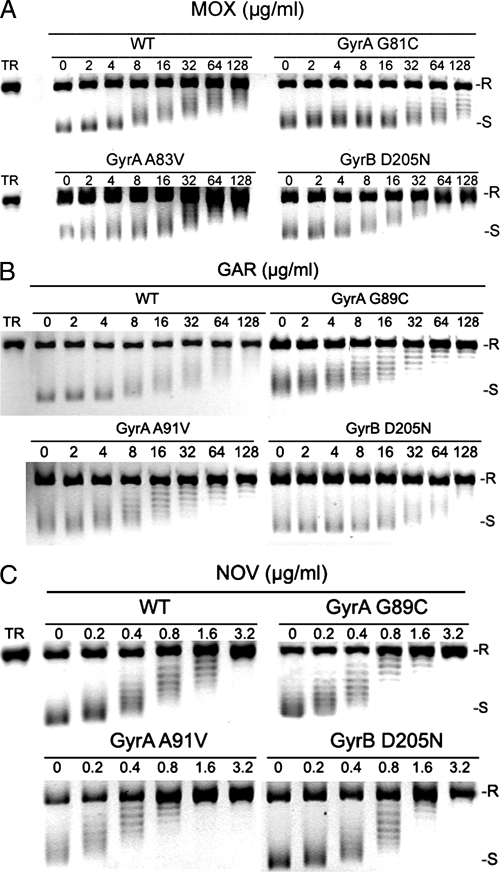
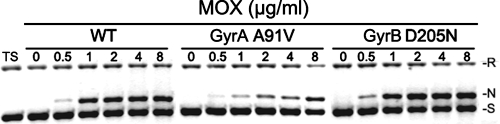
The 50% inhibitory concentrations (IC50s) of gatifloxacin, moxifloxacin, and ofloxacin for the enzymes modified in GyrA were 3- to 11-fold higher (GyrA G89C) and 5- to 8-fold higher (GyrA A91V) than for the wild-type enzyme (Fig. 1; Table 1). The concentrations of fluoroquinolones and garenoxacin required for the conversion of 25% of the DNA to the linear form (CC25s) were 12- to 17-fold higher for the DNA gyrase GyrA A91V than those measured for the wild-type enzyme (Fig. 2; Table 1). As observed previously for the wild-type Mycobacterium tuberculosis and M. leprae DNA gyrases (1, 14), the two classical nonfluorinated quinolones nalidixic acid and oxolinic acid did not lead to the formation of a DNA cleavable complex with the DNA gyrase GyrA A91V (Table 1). DNA cleavage performed with the DNA gyrase GyrA G89C was too weak to allow CC25 measurement. We hypothesized that this defect, previously described in M. tuberculosis DNA gyrase, also modified for G88C (15), could be the consequence of a disulfur bond created in the mutant enzyme between Cys89 (or Cys88) and another cysteine of the DNA gyrase (a good candidate is Cys89 of the other GyrA subunit) which could hamper the cleavage process.
FIG. 1.
Inhibitory activities of moxifloxacin (A), garenoxacin (B), and novobiocin (C) on the supercoiling activities of M. leprae wild-type (WT) and mutant DNA gyrases. Relaxed pBR322 (0.4 μg) was incubated with DNA gyrases reconstituted from wild-type or mutant subunits (carrying mutations G89C and A91V in GyrA and D205N in GyrB) in the absence or presence of the indicated amounts (in μg/ml) of moxifloxacin (MOX), garenoxacin (GAR), or novobiocin (NOV). Reactions were stopped, and the DNA products were analyzed by electrophoresis in 1% agarose gel. Lane TR represents relaxed pBR322 DNA. R and S denote relaxed and supercoiled DNAs, respectively.
TABLE 1.
DNA supercoiling inhibition (IC50s) and DNA cleavable complex formation (CC25s) promoted by various fluorinated and nonfluorinated quinolones and by coumarin with wild-type or modified DNA gyrases of M. leprae
| Drug | R6 | IC50 (μg/ml)a
|
CC25 (μg/ml)
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| WT | G89C | A91V | D205N | WT | G89C | A91V | D205N | ||
| Fluoroquinolones | |||||||||
| Gatifloxacin | F | 3.5 | 20 | 20 | 4.5 | 0.3 | Nob | 4 | 0.3 |
| Moxifloxacin | F | 6 | 30 | 25 | 6 | 0.8 | No | 12 | 0.7 |
| Ofloxacin | F | 15 | 160 | 80 | 20 | 9 | No | 110 | 8 |
| Nonfluorinated quinolones | |||||||||
| Garenoxacin | H | 6 | 5 | 8 | 16 | 1 | No | 17 | 1 |
| Nalidixic acid | H | 300 | 150 | 170 | 600 | No | No | No | No |
| Oxolinic acid | Bridge C6-C7 | 400 | 180 | 200 | 700 | No | No | No | No |
| Coumarin | |||||||||
| Novobiocin | 0.25 | 0.3 | 0.2 | 0.3 | NDc | ND | ND | ND | |
Specific activities of 3.2 × 103, 2.8 × 103, 103, 1.5 × 103, and 3 × 103 U/mg for wild-type (WT) GyrA, wild-type GyrB, mutant GyrA G89C, mutant GyrA A91V, and mutant GyrB D205N, respectively.
No, no DNA cleavage observed.
ND, not determined.
FIG. 2.
Quinolone (moxifloxacin)-mediated DNA cleavage by M. leprae wild-type (WT) and mutant DNA gyrases. Supercoiled pBR322 DNA (0.4 μg) was incubated with DNA gyrases reconstituted from wild-type or mutant subunits (carrying mutation A91V in GyrA or D205N in GyrB) in the absence or presence of the indicated amounts (in μg/ml) of moxifloxacin (MOX). After addition of sodium dodecyl sulfate and proteinase K, DNA samples were analyzed by electrophoresis in 1% agarose. Lane TS represents supercoiled pBR322 DNA. R, N, and S denote relaxed, nicked, and supercoiled DNAs, respectively.
The IC50s of the three nonfluorinated quinolones tested, i.e., garenoxacin, oxolinic acid, and nalidixic acid, were identical or twofold lower for the GyrA-modified DNA gyrases compared to the values obtained for the wild-type enzyme (Table 1). Similar results were previously observed for oxolinic and nalidixic acids with M. tuberculosis wild-type and mutant GyrA enzymes (15). These results were explained by the positioning of the quinolone along the mycobacterial DNA gyrase and particularly by the interaction between the R6 and R7 substituents of the quinolone and residues 88 and 90 of M. tuberculosis DNA gyrase (corresponding to amino acids 89 and 91 in the M. leprae numbering). The fact that garenoxacin IC50s did not increase for any of the M. leprae GyrA mutants is rather interesting. However, its potential impact on leprosy treatment is garbled by the fact that garenoxacin development was recently stopped. Surprisingly, the CC25s of garenoxacin increased 10-fold, i.e., as moxifloxacin. However, the supercoiling inhibition assay and the cleavable-complex assay are distinct since the former is a measure of catalytic inhibition whereas the latter probes an established equilibrium between the ternary DNA-enzyme-drug complexes (3).
We demonstrated that the GyrA G89C and A91V modifications are responsible for fluoroquinolone resistance in M. leprae, as previously shown in M. tuberculosis (2, 15), as well as G81C in Escherichia coli (17). The glycine at position 89 in M. leprae (position 81 in E. coli) is a small and flexible neutral amino acid, whereas cysteine is polar and bulkier than glycine. The alanine at position 91 in M. leprae (position 83 in E. coli) is a relatively small amino acid, whereas valine has higher steric hindrance and is likely to hamper the good positioning of the quinolone in the complex DNA-DNA gyrase.
The gyrB mutation leading to the substitution at position 205 (amino acid 183 in the E. coli numbering system) was reported in a single M. leprae clinical isolate considered to be quinolone resistant because the patient did not improve after ofloxacin treatment (11). We showed that the IC50s and CC25s of quinolones for the enzyme carrying GyrB D205N were similar to those obtained with the wild-type enzyme, demonstrating that the mutation, located outside the GyrB quinolone resistance-determining region (defined by amino acids 426 to 464, in the E. coli numbering), per se does not confer fluoroquinolone resistance on M. leprae (Fig. 1 and 2; Table 1). Since position 205 in GyrB is located in the ATPase domain, which is the site of coumarin interaction, we measured the novobiocin IC50s for the GyrB D205N-modified enzyme and for the DNA gyrases modified in GyrA as controls. No difference in the novobiocin IC50s was observed, showing that D205N is not involved in coumarin resistance either (Table 1). Our findings underlined the need to bear in mind that mutation does not automatically mean resistance. Therefore, the demonstration of the role in quinolone resistance of each novel DNA gyrase mutation observed is an essential prerequisite for interpreting the results of genetic susceptibility tests.
Supplementary Material
Acknowledgments
This work was supported by grants from the Ministère de l'Education Nationale et de la Recherche (grant UPRES 1541), the Fondation pour la Recherche Médicale, and the Association Française Raoul Follereau.
Footnotes
Published ahead of print on 10 December 2007.
Supplemental material for this article may be found at http://aac.asm.org/.
REFERENCES
- 1.Aubry, A., X. S. Pan, L. M. Fisher, V. Jarlier, and E. Cambau. 2004. Mycobacterium tuberculosis DNA gyrase: interaction with quinolones and correlation with antimycobacterial drug activity. Antimicrob. Agents Chemother. 48:1281-1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aubry, A., N. Veziris, E. Cambau, C. Truffot-Pernot, V. Jarlier, and L. M. Fisher. 2006. Novel gyrase mutations in quinolone-resistant and -hypersusceptible clinical isolates of Mycobacterium tuberculosis: functional analysis of mutant enzymes. Antimicrob. Agents Chemother. 50:104-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrett, J. F., J. I. Bernstein, H. M. Krause, J. J. Hilliard, and K. A. Ohemeng. 1993. Testing potential gyrase inhibitors of bacterial DNA gyrase: a comparison of the supercoiling inhibition assay and “cleavable complex” assay. Anal. Biochem. 214:313-317. [DOI] [PubMed] [Google Scholar]
- 4.Cambau, E., E. Perani, I. Guillemin, P. Jamet, and B. Ji. 1997. Multidrug-resistance to dapsone, rifampicin, and ofloxacin in Mycobacterium leprae. Lancet 349:103-104. [DOI] [PubMed] [Google Scholar]
- 5.Champoux, J. J. 2001. DNA topoisomerases: structure, function, and mechanism. Annu. Rev. Biochem. 70:369-413. [DOI] [PubMed] [Google Scholar]
- 6.Chan, G. P., B. Y. Garcia-Ignacio, V. E. Chavez, J. B. Livelo, C. L. Jimenez, M. L. Parrilla, and S. G. Franzblau. 1994. Clinical trial of sparfloxacin for lepromatous leprosy. Antimicrob. Agents Chemother. 38:61-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cole, S. T., K. Eiglmeier, J. Parkhill, K. D. James, N. R. Thomson, P. R. Wheeler, N. Honore, T. Garnier, C. Churcher, D. Harris, K. Mungall, D. Basham, D. Brown, T. Chillingworth, R. Connor, R. M. Davies, K. Devlin, S. Duthoy, T. Feltwell, A. Fraser, N. Hamlin, S. Holroyd, T. Hornsby, K. Jagels, C. Lacroix, J. Maclean, S. Moule, L. Murphy, K. Oliver, M. A. Quail, M. A. Rajandream, K. M. Rutherford, S. Rutter, K. Seeger, S. Simon, M. Simmonds, J. Skelton, R. Squares, S. Squares, K. Stevens, K. Taylor, S. Whitehead, J. R. Woodward, and B. G. Barrell. 2001. Massive gene decay in the leprosy bacillus. Nature 409:1007-1011. [DOI] [PubMed] [Google Scholar]
- 8.Ji, B., and J. Grosset. 2000. Combination of rifapentine-moxifloxacin-minocycline (PMM) for the treatment of leprosy. Lepr. Rev. 71(Suppl.):S81-S87. [DOI] [PubMed] [Google Scholar]
- 9.Ji, B., and J. H. Grosset. 1990. Recent advances in the chemotherapy of leprosy. Lepr. Rev. 61:313-329. [DOI] [PubMed] [Google Scholar]
- 10.Katoch, V. M. 2002. Advances in the diagnosis and treatment of leprosy. Expert Rev. Mol. Med. 2002:1-14. [DOI] [PubMed] [Google Scholar]
- 11.Kim, S. K., S. B. Lee, T. J. Kang, and G. T. Chae. 2003. Detection of gene mutations related with drug resistance in Mycobacterium leprae from leprosy patients using Touch-Down (TD) PCR. FEMS Immunol. Med. Microbiol. 36:27-32. [DOI] [PubMed] [Google Scholar]
- 12.Levy, L., and B. Ji. 2006. The mouse foot-pad technique for cultivation of Mycobacterium leprae. Lepr. Rev. 77:5-24. [PubMed] [Google Scholar]
- 13.Maeda, S., M. Matsuoka, N. Nakata, M. Kai, Y. Maeda, K. Hashimoto, H. Kimura, K. Kobayashi, and Y. Kashiwabara. 2001. Multidrug-resistant Mycobacterium leprae from patients with leprosy. Antimicrob. Agents Chemother. 45:3635-3639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matrat, S., S. Petrella, E. Cambau, W. Sougakoff, V. Jarlier, and A. Aubry. 2007. Expression and purification of an active form of the Mycobacterium leprae DNA gyrase and its inhibition by quinolones. Antimicrob. Agents Chemother. 51:1643-1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matrat, S., N. Veziris, C. Mayer, V. Jarlier, C. Truffot-Pernot, J. Camuset, E. Bouvet, E. Cambau, and A. Aubry. 2006. Functional analysis of DNA gyrase mutant enzymes carrying mutations at position 88 in the A subunit found in clinical strains of Mycobacterium tuberculosis resistant to fluoroquinolones. Antimicrob. Agents Chemother. 50:4170-4173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pattyn, S. R. 1991. Anti-Mycobacterium leprae activity of several quinolones studied in the mouse. Int. J. Lepr. Other Mycobact. Dis. 59:613-617. [PubMed] [Google Scholar]
- 17.Ruiz, J. 2003. Mechanisms of resistance to quinolones: target alterations, decreased accumulation and DNA gyrase protection. J. Antimicrob. Chemother. 51:1109-1117. [DOI] [PubMed] [Google Scholar]
- 18.Scollard, D. M., L. B. Adams, T. P. Gillis, J. L. Krahenbuhl, R. W. Truman, and D. L. Williams. 2006. The continuing challenges of leprosy. Clin. Microbiol. Rev. 19:338-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. 1982. Chemotherapy of leprosy for control programmes. World Health Organization, Geneva, Switzerland. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.