Abstract
Background. Portal vein thrombosis (PVT) is a well recognized complication of patients with end-stage cirrhosis and its incidence ranges from 2 to 26%. The aim of this study was to analyze the results and long-term follow-up of a consecutive series of liver transplants performed in patients with PVT and compare them with patients transplanted without PVT. Patients and methods. Between July 1995 and June 2006, 26 liver transplants were performed in patients with PVT (8.7%). Risk factors and variables associated with the transplant and the post-transplant period were analyzed. A comparative analysis with 273 patients transplanted without PVT was performed. Results. The patients comprised 53.8% males, average age 40, 7 years. PVT was detected during surgery in 65%. Indications for transplantation were: post-necrotic cirrhosis 73%, cholestatic liver diseases 23%, and congenital liver fibrosis 4%. Child-Pugh C: 61.5%. Techniques were trombectomy in 21 patients with PVT grades I, II, IV, and extra-anatomical mesenteric graft in 5 with grade III. Morbidity was 57.7%, recurrence of PVT was 7.7%, and in-hospital mortality was 26.9%. Greater operative time, transfusion requirements, and re-operations were found in PVT patients. One-year survival was 59.6%: 75.2% for grade 1 and 44.8% for grades 2, 3, and 4. Discussion. The study demonstrated a PVT prevalence of 8.7%, a higher incidence of partial thrombosis (grade 1), and successful management of PVT grade 4 with thrombectomy. Liver transplant in PVT patients was associated with an increased operative time, transfusion requirements, re-interventions, and lower survival rate according to PVT extension.
Keywords: liver transplantation, portal vein thrombosis, surgical management
Introduction
Portal vein thrombosis (PVT) is a well recognized complication of patients with end-stage cirrhosis and its incidence ranges from 2 to 26% in different series 1. The etiology, not yet fully understood, is based on the thrombotic tendency related to several factors: altered liver anatomy that increases the intrahepatic resistance to portal flow, endothelial injury due to an elevated portal pressure, and coagulation abnormalities 2,3. Considered for two decades an absolute contraindication for liver transplantation (LTx), in 1985 the first report of a successful transplantation in two patients with PVT was published 4. Advances in the intraoperative management of this entity and encouraging results produced an increase in the number of transplants performed with PVT that at the present time is from 2 to 19% 5. Although screening of the portal vein (PV) patency is routinely performed in the preoperative evaluation of candidates, unsuspected PVT continues to be found intraoperatively. Nowadays, the procedure is performed even in cases of extended thrombosis with inflammatory changes of the portal vein axis 2. However, PVT continues to be associated with a considerable perioperative risk for LTx candidates.
Patients and methods
Records of patients transplanted at the Liver Transplant Unit of the Hospital Dr Cosme Argerich, Buenos Aires, Argentina were retrospectively reviewed. From July 2005 to June 2006, 323 LTx were performed and 26 patients with intraoperatively confirmed PVT were included in the study (8.7%). Patients with tumor thrombus of the PV were excluded. Based on intraoperative assessment, PVT was retrospectively classified according to Yerdel et al. into four grades, as follows. Grade 1: partial PVT (< 50% of the lumen) with or without minimal extension into the superior mesenteric vein (SMV). Grade 2:>50% occlusion with or without minimal extension into the SMV. Grade 3: complete thrombosis of both PV and proximal SMV. Distal SMV is open. Grade 4: complete thrombosis of the PV and proximal and distal SMV.
The preoperative study of the candidates for LTx consisted of systematic Doppler sonography. In cases where suspicion of PVT was high, conventional angiography or spiral CT arterial portography were performed.
Risk factors analyzed for PVT were as follows: age, sex, etiology, Child-Pugh classification, previous treatments for portal hypertension (sclerotherapy, shunt surgery, transjugular intrahepatic portosystemic shunt – TIPS), and previous upper abdominal surgery.
Orthotopic liver transplantation was performed using whole cadaveric grafts with classic venovenous bypass technique in 17 patients and piggy-back in 9 patients. The PV was dissected entirely to determine the extent of the thrombus and, in selected cases with distal extension, inframesocolonic SMV was also dissected.
Follow-up consisted of Doppler ultrasound on the first, third, fifth, and seventh postoperative day, and the first and third month, and then every time it was considered clinically necessary.
Intraoperative and postoperative variables analyzed were: surgical technique according to PVT grade, cold ischemia time, anhepatic phase and whole transplant duration, blood requirements, re-interventions, recurrence of PVT, early and late postoperative deaths, and survival.
A comparative analysis was performed with 273 patients without PVT transplanted in the same period.
Statistical analysis
Qualitative variables expressed as frequencies and percentages were compared using the χ2 test. For quantitative variables expressed as mean values and standard deviation comparison was done applying the Student's t test. The Kaplan–Meier method was used to calculate actuarial survival rates and inter-group comparisons were performed by means of the log-rank test. Statistical significance was considered to exist when p<0.05. Statistical analyses were performed using SPSS v12.0.
Results
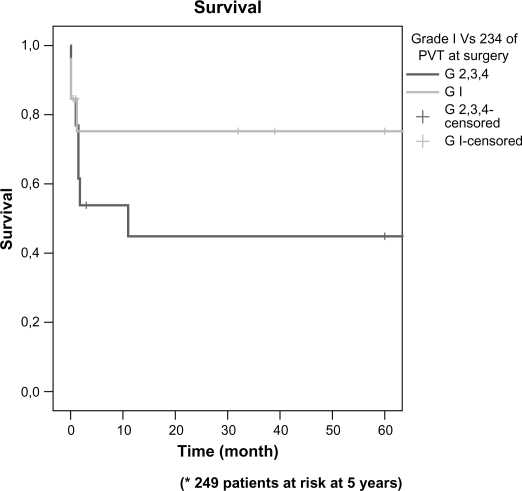
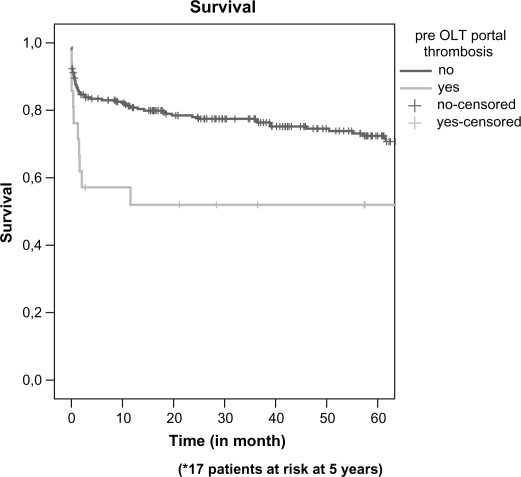
Among 26 patients with PVT, 14 were males and 12 were females with a median age of 40 years (range 17–61). PVT was diagnosed preoperatively in 9 patients (35%) and during the transplant procedure in 17 (65%). Indications for LTx were predominantly related to post-necrotic cirrhosis in 73% (19/26) of the cases (alcoholic 6, cryptogenic 5, post-hepatitis C 5, post-hepatitis B 2, autoimmune 1), cholestatic liver diseases in 23% (6/26) (primary sclerosing cholangitis (PSC) 4, primary biliary cirrhosis 2), and congenital hepatic fibrosis in 4% (1/26). Child-Pugh class C was present in 61.5%. Before transplantation 53.8% (14/26) had undergone sclerotherapy, 7.6% (2/26) TIPS, and 42.3% (11/26) upper abdominal surgery with cholecystectomy as the most common procedure (63%). There was no previous portosystemic shunt. Of the 26 patients with PVT, 13 had grade 1 (50%), 5 grade 2 (19%), 5 grade 3 (19%), and 3 grade 4 (12%). Operative management consisted of thrombectomy with or without endovenectomy in 21 patients with PVT grades 1, 2, and 4, and venous jump graft from the superior mesenteric vein in 5 patients with PVT grade 3 6. Fifteen (57%) patients received preventive anticoagulant therapy with low molecular weight heparin followed by aspirin for 6 months. The average complication rate in patients with PVT was 57.7% – infectious complications in 46.2% (5/12), and reoperations in 39%. The overall incidence of PV rethrombosis was 7.7% (two patients). The first was transplanted for congenital hepatic fibrosis, and at the 16th postoperative day presented left PV thrombosis and required a left hepatectomy. At the 23rd day a second rethrombosis recurred in the main portal trunk and right branch, the patient was included in the waiting list for retransplantation but died due to multi-organ failure. The second death corresponds to a patient who presented a simultaneous arterial thrombosis, PV rethrombosis, and graft failure in the early post-transplantation period. Five patients (two PVT grade 1, two PVT grade 2, and one PVT grade 3) required retransplantation. In-hospital mortality and late mortality were 26.9% and 19.2%, respectively (Table I). The overall actuarial 1-year survival rate in PVT patients (59%) was lower than in non-PVT patients (80.5%, p<0.001) (Figure 1). According to PVT classification, patients with grade 1 demonstrated a trend towards better 1- and 5-year survival rates than grades 2, 3, and 4 (75.2% vs 44.8%; p=0.4) (Figure 2) Two of the three patients with PVT grade IV treated by thrombectomy were alive at 68 and 128 months post-transplant, respectively.
Table I. Causes of mortality in patients with PVT who underwent liver transplantation.
| Period | Cause | n | Survival |
|---|---|---|---|
| Early | Post-reperfusion cardiac arrest (T) | 1 | Day 0 |
| Primary non-function (JG) | 2 | Day 1 | |
| Rethrombosis + arterial thrombosis (JG) | 1 | Day 1 | |
| MOF (sepsis) (T) | 1 | Day 1 | |
| Pontine myelinolysis (T) | 1 | Day 49 | |
| Rethrombosis + sepsis (T) | 1 | Day 52 | |
| Late | Sepsis (T) | 1 | 2 months |
| Arterial thrombosis (2nd day after re-transplantation) (T) | 1 | 2 months | |
| Chronic rejection (T) | 1 | 11 months | |
| VHC recurrence (T) | 1 | 69 months | |
| Pneumopathy (T) | 1 | 88 months |
Intraoperative management of PVT: T, thrombectomy; JG, venous jump graft from SMV.
Figure 1. .
Overall patient survival rates in patients with and without PVT.
Figure 2. .
Overall survival in patients with grade 1 PVT and combined grades 2–4 PVT.
A comparative analysis performed with 273 patients transplanted without PVT also showed significance in the following variables: previous surgery, transfusion requirements, reoperations, and portal rethrombosis (Table II).
Table II. Comparative analysis of liver transplantation in patients with and without PVT.
| Parameter | With PVT (n=26) | Without PVT (n=273) | p value |
|---|---|---|---|
| Age (years) | 41.9 | 40.3 | 0.4 |
| Sex (%) | |||
| Male | 53.8 | 43.5 | 0.3 |
| Female | 46.2 | 56.5 | |
| Previous surgery (%) | 42.31 | 24.1 | 0.03 |
| Cold ischemia time (min) | 543.04 | 523.4 | 0.6 |
| Operative time (h) | 8.65 | 7.8 | 0.3 |
| Anhepatic phase (min) | 66.04 | 57.23 | 0.08 |
| RBC (u) | 14.52 | 10.14 | 0.03 |
| Plasma (u) | 13.08 | 12.65 | 0.1 |
| Platelets (u) | 6.24 | 5.28 | 0.02 |
| Reoperations (%) | 39 | 24.7 | 0.03 |
| Rethrombosis | 2/26 | 2/273 | 0.001 |
| 1-year survival (%) | 59.60 | 80.5 | 0.0003 |
Discussion
The incidence of PVT in our series was 8.7%, similar to the results reported by most liver transplant centers since the 1990s, which range from 2 to 16% 7. Although different etiologies of liver failure have been associated with PVT, our data showed a significant association with post-necrotic cirrhosis (73%), especially with Laennec's, hepatitis C virus (VHC), and cryptogenic cirrhosis 8. Unlike others, a higher rate of PVT was found in PSC (15%) 7,8.
Several risk factors for PVT, such as male gender, Child-Pugh C, previous treatments for portal hypertension (sclerotherapy, TIPS, shunt surgery, splenectomy), and previous surgical interventions were described 9,10. The predominance in males is likely to be related to the higher incidence of Laennec's cirrhosis in this population 9,11. Treatments for bleeding indicate a more pronounced portal hypertension that justifies the higher incidence of PVT due to the hemodynamic changes in the PV (low or reversed flow) 10. In our study 54% of the patients with PVT had been treated by sclerotherapy.
It is standard practice in the pre-LTx evaluation to perform Duplex ultrasonography (US) of the hepatic vasculature. Accuracy in detecting PVT ranges from 26% to 87%. This is explained by a high incidence of false negatives due to the extension of PVT, the identification of portal collaterals as the PV, and the post-US thrombosis of the PV while patients are awaiting transplantation 12,13. Other radiological methods include angiography, angio-MRI, and less often spiral CT arterial portography 2,9,12. Despite exhaustive radiological evaluation before LTx, cases of undiagnosed PVT continue to be found during surgery. In our series this (65%) could be justified by the high incidence of PVT grade 1 14. Several PVT classifications have been proposed 6,9,10,14. We consider Yerdel's the most adequate because it correlates the thrombosis extension with the surgical technique and outcome 9.
An adequate portal inflow to the graft is essential for good liver function. Different approaches have been proposed to restore PV patency at the time of OLT, such as thrombectomy, the use of venous interposition grafts, the use of PV collaterals, and cavoportal hemitransposition 6,15. In grades 1 and 2 with totally patent SMV, thrombectomy is the procedure of choice 5,13,16. The intraoperative strategy should be to determine first the extent of the thrombosis with proximal dissection of the PV and progressive separation of the thrombus from the surrounding vessel wall by the eversion technique. Also, as thrombi are usually organized, Fogarty catheter thrombectomy is not amenable 13. In patients with proximally occluded but distally open SMV (grade 3), we prefer the extra-anatomic jump graft with donor iliac vein 9,17. It is tunneled through the transverse mesocolon, anterior to the pancreas and posterior to the pylorus, avoiding extensive peripancreatic dissection of the anatomic graft with its attendant morbidity 13,16. If the thrombosis extends to the distal SMV (grade 4), different procedures have been described to restore portal inflow: anastomosis of the donor PV to the recipient left gastric vein or a suitable tributary, jump graft to a recanalized SMV, PV arterialization, thrombectomy, cavoportal hemitransposition, and combined liver–intestine transplantation 6,9,13. Stieber et al. were the first to report successful outcome in patients with extensive PVT after thrombectomy 6. In contrast to a previous study, two-thirds of patients with PVT grade 4 treated by this method are still alive with normal graft function at 5 years 9. As Tzakis et al. reported, cavoportal hemitransposition has been proposed as a means of overcoming the problem of extensive PV thrombosis 15. However, the most common complications of this procedure are severe ascites and variceal bleeding due to the persistent portal hypertension 18. Better patient selection and the use of the renoportal hemitransposition have demonstrated long-term survival 18,19. Recently, endovascular techniques during LTx have shown their value in solving some liver graft perfusion problems in patients with PVT grades 3 or 4 20,21.
The greater technical difficulty in patients with pre-existing PVT has demonstrated an increased risk of complications like hepatic artery thrombosis, relaparotomy, postoperative pancreatitis, sepsis, and renal failure in different studies 9,12,16. Operative time and anhepatic phase could be longer and transfusion requirements higher, as was observed in this study 7,13,16. A higher incidence of primary nonfunction or dysfunction could be related to more complex surgical procedures in fragile patients with severe portal hypertension 9. Despite surgical progress, the perioperative mortality rates of LTx in the presence of PVT remains high, ranging from 9 to 42% 12.
Rethrombosis of the PV in this series occurred in only 7.7% of our PVT patients, which compares favorably with the published rates from 6.2% to 28.6% 2,13,14. It carries a poor prognosis, and mortality of rethrombosis in our series was 100%. However, there are no uniform criteria for the use of prophylactic measures. Some advocate preventive regimens with low molecular weight heparin, dextran, coumadin derivatives, or aspirin, while others only use systemic anticoagulation in patients with hypercoagulable states 8,9,12,13.
In general, 1-year survival after LTx in patients with PVT ranges from 59% to 88%, and has a close relationship to the PVT extension 5. In this study the overall 1-year survival in PVT patients (59%) was lower than in non-PVT patients (80.5%). It is interesting that 1-year and 5-year survival in PVT patients was identical, reflecting that once they have survived the peri-transplant period, the outcome is identical to non-PVT patients. According to the severity of PVT we found a trend toward a difference in survival between grade 1 (75%) vs grades 2, 3, and 4 (45%), but this was not statistically significant.
Experience in the management of PVT has demonstrated that patients with minimally thrombosed PV (grade 1), can undergo successful transplantation with similar results to non-PVT patients 8,9,13.
In conclusion, we confirm that PVT is not a contraindication to LTx at the present time. Our study demonstrated a PVT prevalence of 8.7%, and a higher incidence of partial thrombosis (grade 1) that explains the elevated rate of intraoperative diagnosis. LTx in PVT patients was associated with an increase of the operative time, the transfusion requirements, the incidence of re-interventions, and a lower survival rate according to PVT extension. In PVT grade 4, successful management with thrombectomy avoided the utilization of other proposed techniques.
Acknowledgements and disclosures
No disclosures.
References
- 1.Francoz C, Belghiti J, Vilgrain V, Sommacale D, Paradis V, Condat B, et al. Splanchnic vein thrombosis in candidates for liver transplantation: usefulness of screening and anticoagulation. Gut. 2005;54:691–7. doi: 10.1136/gut.2004.042796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Orlando G, De LL, Toti L, Zazza S, Angelico M, Casciani CU, et al. Liver transplantation in the presence of portal vein thrombosis: report from a single center. Transplant Proc. 2004;36:199–202. doi: 10.1016/j.transproceed.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Bayraktar Y, Harmanci O. Etiology and consequences of thrombosis in abdominal vessels. World J Gastroenterol. 2006;12:1165–74. doi: 10.3748/wjg.v12.i8.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw BW, Jr, Iwatsuki S, Bron K, Starzl TE. Portal vein grafts in hepatic transplantation. Surg Gynecol Obstet. 1985;161:66–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Robles R, Fernandez JA, Hernandez Q, Marin C, Ramirez P, Sanchez-Bueno F, et al. Eversion thromboendovenectomy in organized portal vein thrombosis during liver transplantation. Clin Transplant. 2004;18:79–84. doi: 10.1111/j.1399-0012.2004.00120.x. [DOI] [PubMed] [Google Scholar]
- 6.Stieber AC, Zetti G, Todo S, Tzakis AG, Fung JJ, Marino I, et al. The spectrum of portal vein thrombosis in liver transplantation. Ann Surg. 1991;213:199–206. doi: 10.1097/00000658-199103000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gimeno FA, Calvo J, Loinaz C, Meneu JC, Perez B, Gomez R, et al. Comparative analysis of the results of orthotopic liver transplantation in patients with and without portal vein thrombosis. Transplant Proc. 2005;37:3899–903. doi: 10.1016/j.transproceed.2005.10.085. [DOI] [PubMed] [Google Scholar]
- 8.Molmenti EP, Roodhouse TW, Molmenti H, Jaiswal K, Jung G, Marubashi S, et al. Thrombendvenectomy for organized portal vein thrombosis at the time of liver transplantation. Ann Surg. 2002;235:292–6. doi: 10.1097/00000658-200202000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yerdel MA, Gunson B, Mirza D, Karayalcin K, Olliff S, Buckels J, et al. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation. 2000;69:1873–81. doi: 10.1097/00007890-200005150-00023. [DOI] [PubMed] [Google Scholar]
- 10.Gayowski TJ, Marino IR, Doyle HR, Echeverri L, Mieles L, Todo S, et al. A high incidence of native portal vein thrombosis in veterans undergoing liver transplantation. J Surg Res. 1996;60:333–8. doi: 10.1006/jsre.1996.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loinaz C, Gomez R, Jimenez C, Gonzalez-Pinto I, Garcia I, Gimeno A, et al. Liver transplantation in patients with portal thrombosis: results in 76 patients. Transplant Proc. 2002;34:248–9. doi: 10.1016/s0041-1345(01)02746-4. [DOI] [PubMed] [Google Scholar]
- 12.Dumortier J, Czyglik O, Poncet G, Blanchet MC, Boucaud C, Henry L, et al. Eversion thrombectomy for portal vein thrombosis during liver transplantation. Am J Transplant. 2002;2:934–8. doi: 10.1034/j.1600-6143.2002.21009.x. [DOI] [PubMed] [Google Scholar]
- 13.Seu P, Shackleton CR, Shaked A, Imagawa DK, Olthoff KM, Rudich SR, et al. Improved results of liver transplantation in patients with portal vein thrombosis. Arch Surg. 1996;131:840–4. doi: 10.1001/archsurg.1996.01430200050009. [DOI] [PubMed] [Google Scholar]
- 14.Charco R, Fuster J, Fondevila C, Ferrer J, Mans E, Garcia-Valdecasas JC. Portal vein thrombosis in liver transplantation. Transplant Proc. 2005;37:3904–5. doi: 10.1016/j.transproceed.2005.09.120. [DOI] [PubMed] [Google Scholar]
- 15.Tzakis AG, Kirkegaard P, Pinna AD, Jovine E, Misiakos EP, Maziotti A, et al. Liver transplantation with cavoportal hemitransposition in the presence of diffuse portal vein thrombosis. Transplantation. 1998;65:619–24. doi: 10.1097/00007890-199803150-00004. [DOI] [PubMed] [Google Scholar]
- 16.Bertelli R, Nardo B, Montalti R, Beltempo P, Puviani L, Cavallari A. Liver transplantation in recipients with portal vein thrombosis: experience of a single transplant center. Transplant Proc. 2005;37:1119–21. doi: 10.1016/j.transproceed.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 17.Lerut JP, Mazza D, van Leeuw V, Laterre PF, Donataccio M, de Ville de Goyet J, et al. Adult liver transplantation and abnormalities of splanchnic veins: experience in 53 patients. Transpl Int. 1997;10:125–32. doi: 10.1007/s001470050025. [DOI] [PubMed] [Google Scholar]
- 18.Ceulemans B, Aerts R, Monbaliu D, Coosemans W, Verslype C, Van SW, et al. Liver transplantation using cavoportal transposition: an effective treatment in patients with complete splanchnic venous thrombosis. Transplant Proc. 2005;37:1112–14. doi: 10.1016/j.transproceed.2004.12.047. [DOI] [PubMed] [Google Scholar]
- 19.Azoulay D, Adam R, Castaing D, Muresan S, Essomba A, Vibert E, et al. [Liver transplantation with cavoportal or renoportal anastomosis: a solution in cases of diffuse portal thrombosis.] Gastroenterol Clin Biol 2002;26:325–30 (in French). [PubMed] [Google Scholar]
- 20.Marini M, Gomez-Gutierrez M, Cao I, Selles C, Aguirrezabalaga J, Otero A, et al. Endovascular treatment of splenomesenteric-portal vein thromboses during orthotopic liver transplantation. J Vasc Interv Radiol. 2005;16:1135–42. doi: 10.1097/01.RVI.0000167851.00221.B0. [DOI] [PubMed] [Google Scholar]
- 21.Gomez-Gutierrez M, Quintela J, Marini M, Gala B, Suarez F, Cao I, et al. Portal vein thrombosis in patients undergoing orthotopic liver transplantation: intraoperative endovascular radiological procedures. Transplant Proc. 2005;37:3906–8. doi: 10.1016/j.transproceed.2005.10.063. [DOI] [PubMed] [Google Scholar]