Abstract
Introduction. Unlike malignant liver tumours, the indications for hepatic resection for benign disease are not well defined. This is particularly true for focal nodular hyperplasia (FNH). Here we summarize a single-centre experience of the diagnosis and management of FNH. Materials and methods. Using a prospectively collected database, a retrospective analysis of consecutive patients who were managed at our centre for FNH between January 1997 and December 2006 was performed. Results. The cohort was divided into two groups of patients: those who were managed surgically (n=15) and those managed conservatively (n=37). There was no correlation between tumour size and number of lesions with oral contraceptive use (p=0.07 and 0.90, respectively) and pregnancy (p=0.45 and 0.60, respectively). However, tumour size (p=0.006) and number of lesions (p=0.02) were associated with the occurrence of pain in these patients. Pain was the commonest symptom of patients (13/15) who were managed surgically. All patients underwent radiological imaging before diagnosis. The sensitivities of ultrasound, CT scanning and MRI scanning in characterizing these lesions were 30%, 70% and 87%, respectively. There were no postoperative deaths and three postoperative complications that were successfully managed non-operatively. With a median follow-up of 24 months in the surgically treated group, one patient has developed recurrent symptoms of pain. Conclusion. In this series, there was no mortality directly due to the surgical procedure and a modest morbidity, justifying surgical resections in selected patients.
Keywords: focal nodular hyperplasia, hepatic resection, benign liver tumours
Introduction
Focal nodular hyperplasia (FNH) is one of the most common benign neoplasms of the liver and accounts for 8% of all primary hepatic tumours. It is more commonly found in women, although it can present with smaller lesions and atypical features in men 1. Frequently, the lesion is picked up incidentally but can also present with vague abdominal symptoms due to the mass effect causing pain and bloatedness. Contrast-enhanced MRI scanning has been shown to be the most sensitive modality for characterizing this lesion 2. However, imaging techniques such as Doppler ultrasound and CT scanning are also frequently used. The distinction between benign and malignant lesions still remains difficult, but crucial, as the treatment of the two conditions remains distinctly different.
FNH is not a premalignant lesion 3,4. Therefore, unlike premalignant and malignant tumours, the indications for hepatic resection for benign disease are not as well defined. This is particularly true for FNH, where the indications for surgery include progressive disease, increasing pain and lesions where malignancy cannot be excluded.
Although there continues to be marked improvement in outcomes of hepatic resections, the procedure is still associated with a mortality and morbidity rate of < 5% and 30%, respectively, emphasizing the importance of clear indications for surgery in benign diseases such as FNH. Here we summarize a single-centre experience of the diagnosis and management of FNH including those treated surgically and conservatively.
Materials and methods
Between January 1997 and June 2006, patients with focal nodular hyperplasia at our centre were evaluated. The patients’ medical, radiological and surgical records were reviewed retrospectively. Data collected included patient age, sex, symptoms, risk factors, comorbidity, liver function tests, tumour markers, radiological findings, preoperative diagnosis, indications for operations, surgical procedures, postoperative diagnosis, length of hospital stay, postoperative complications and progress on follow-up. All patients and radiographic studies were presented and discussed at a weekly multi-disciplinary hepatobiliary meeting between surgeons, hepatologists, radiologists and pathologist.
The patients were retrospectively divided into surgically and non-surgically managed groups and compared. Patients considered for surgical resection for symptomatology, underwent further investigations to exclude other diagnoses such as cholelithiasis and gastritis. Patients with suspicious lesions underwent additional preoperative investigations to evaluate the extent of disease. If the lesion remained radiologically suspicious, surgical resection was carried out. Conservative management was indicated in non-symptomatic lesions with a clear diagnosis of FNH. These patients were followed up with radiological imaging at 6 months.
Statistical analysis was performed using SPSS 12.0.1 for Windows (SPSS, Chicago, IL, USA). Categorical and continuous variables were analysed using χ2 and independent sample t test, respectively.
Results
In the 10-year study period, a total of 52 patients were diagnosed with FNH at our unit. The diagnosis of lesions was based on radiological and pathological findings for both the surgically and non-surgically managed groups (Table I).
Table I. FNH diagnostic criteria for surgically and non-surgically managed groups.
| Diagnostic criteria | Number (clinical features) |
|---|---|
| Surgical group (n=15) | |
| Definitive radiological diagnosis | 6 (all resected for pain) |
| Inconclusive radiological diagnosis; definitive preoperative pathological diagnosis | 2 (all resected for pain) |
| Suspicious lesion on radiological investigation | 4* |
| Suspicious lesion on radiological and preoperative pathological investigation | 3* |
| Non-surgical group (n=37) | |
| Definitive radiological diagnosis | 30 (minor symptoms, n=10; asymptomatic, n=20) |
| Inconclusive radiological diagnosis; definitive pathological diagnosis | 7 |
*FNH diagnosed on postoperative histopathology.
The two groups were comparable for patient demographics (Table II). The median age of the surgically and conservatively managed groups was 40 and 36 years, respectively, with 47 women sufferers (90%) in the whole cohort. In total, 64% (30 patients) of these women were on the oral contraceptive pill (OCP) at the time of diagnosis and 62% (29 patients) had a previous pregnancy. There was no significant difference in ASA grade, liver function and tumour marker levels between the groups.
Table II. Characteristics of surgically and conservatively managed patients.
| Characteristic | Surgical group (n=15) | Conservative group (n=37) | Statistical difference between groups |
|---|---|---|---|
| Demographics | |||
| Age | 40 (20–66) | 36 (24–56) | |
| Sex (female:male) | 14:1 | 33:4 | NS |
| OCP use | 11/14 | 19/33 | |
| Pregnancy | 8/14 | 21/33 | |
| Symptoms | |||
| Pain | 13/15 (moderate/severe) | 13/37 (mild) | 0.001 |
| Incidental | 1 | 19 | 0.001 |
| Clinical investigations | |||
| Suspicious lesion | 7 | 0 | <0.0001 |
| ASA | |||
| Grade 1 | 14/15 | 34/37 | NS |
| Grade 2 | 1/15 | 3/37 | |
| Tumour size (cm) | 6.1 | 3.2 | 0.01 |
| No. of lesions | 2 | 2 | NS |
| Biochemical investigations | |||
| Normal LFTs | 13 | 30 | NS |
| Normal tumour markers | 11/11 | 27/28 | NS |
LFT, liver function test.
All patients underwent radiological imaging before diagnosis. The most frequent radiological imaging modality used at our centre for investigating these lesions was MRI scanning (Table III). The sensitivities of ultrasound, CT scanning and MRI scanning in characterizing these lesions were 30%, 70% and 87%, respectively. Aside from these modalities, four HIDA scans were performed to rule out gallbladder dyskinesia as a cause of pain.
Table III. Use and sensitivities of US, CT and MRI scanning for FNH.
| Imaging modality | Number performed | Sensitivity in diagnosing FNH [number (%)] |
|---|---|---|
| Ultrasound | 27/52 | 8 (30%) |
| CT scanning | 34/52 | 24 (70%) |
| MRI scanning | 46/52 | 40 (87%) |
The indication for surgical resection was a suspicious lesion on radiological investigation or persistent pain in a clear diagnosis of FNH. This is evident on comparing the two groups, where a significantly greater number of patients had pain and suspicious lesions in the surgical group (Table II).
The surgical procedures performed on these patients included three trisegmentectomies, three lobecomies, one segmentectomy and eight non-anatomical resections. On histopathological analysis of the resected specimen occasionally other neoplasms were found incidentally with the FNH lesions. These included five adenomas and one hepatocellular carcinoma (HCC).
The median hospital stay was 9 days in the surgical group. There were no postoperative deaths. One patient developed chest infections requiring parenteral antibiotic therapy, one subhepatic abcess that required percutaneous drainage and one wound infection.
With a median follow-up of 24 months (range 6–72 months), there has been one death in the patients treated for FNH. This was in a patient who was found to have a HCC in the resected specimen.
Of the surgically treated group two patients have developed recurrence of FNH, at 29 and 48 months post resection, respectively, with the former developing minor symptoms of pain. In the conservatively managed group, with a median follow-up of 23 months (range 3–84 months), five patients group continue to complain of atypical pain and are currently under investigation for this prior to consideration of resection.
Discussion
Along with haemangiomas, FNH is currently one of the most common benign lesions of the liver. It is predominantly found in women, with most series reporting the incidence in men to be < 15% 5. Luciani et al reported that when occurring in men, these lesions are frequently atypical, occurring at a later age and of a smaller size 1. In this study of 52 patients, we report a 47:5 female to male ratio. Of note, comparing men to women, the mean age at diagnosis was 43 compared to 37 (p=0.18) and mean tumour size was 4.6 cm compared to 3.8 cm, respectively (p=0.47).
Unlike hepatic adenomas, the role of the OCP and pregnancy in the development and complications of FNH remains controversial 2,6,7. Here 64% and 62% of the 47 women in the study were on the OCP and had had pregnancies before the diagnosis of FNH. There was no correlation between tumour size and number of lesions with OCP use (p=0.07 and 0.90, respectively) and pregnancy (p=0.45 and 0.60, respectively). These findings were similar to previously published findings 8. The OCP was not stopped in conservatively managed patients with a clear diagnosis of FNH and there was no change in character on follow-up radiology.
Pain was the commonest symptom of patients with this lesion and persistence of this pain was used as an indication for surgery in these patients. For the whole cohort of patients, tumour size (p=0.006) and number of lesions (p=0.02) were associated with the occurrence of pain. Because the persistence of pain was an indication for surgery, there were a significantly greater number of patients in the surgically managed group who suffered with pain and a significantly larger number of patients in the conservatively managed group that had lesions discovered incidentally.
Radiological imaging is invaluable in diagnosing the conditions. Many recent publications have shown that MRI scanning remains the gold standard for this purpose 2,9. In this study the majority (88%) of patients had MRI scanning to characterize these lesions. However, the sensitivity of a clear diagnosis of FNH remained suboptimal at 87%. Lesions that were thought to be suspicious on radiological imaging were considered for resection. Resections were performed on seven FNH lesions that were thought to look suspicious on radiological investigations.
In the surgically managed group, three trisegmentectomies, three lobectomies, one segmentectomy and eight non-anatomical resections were performed. Formal anatomical resections were carried out in radiologically suspicious lesions. On histopathological analysis of the resected specimens, five of these lesions were found to have a simultaneous adenoma and one of these lesions was found to have a HCC. The simultaneous occurrence of FNH and hepatic adenomas is thought to be favoured by angiogenic abnormalities, tumour-induced growth factors, thrombosis and local arteriovenous shunting or co-incidental 7. Associations between FNH and HCC have rarely been described, with two published reports of FNH associated with the fibrolamellar variant of HCC 10,11,12.
With a median postoperative stay of 9 days, there was minimal morbidity and no mortality in this cohort. Three patients developed postoperative complications from a wound infection, chest infection and a subhepatic abscess that were successfully managed non-operatively. There was generally a low morbidity associated with the open surgical resections. In a bid to further improve on the morbidity of liver resections for benign disease, some centres have shown encouraging results in laparoscopic resections, with results that are at least as good as open surgery 13,14.
On long-term follow-up (mean of 22 months), there was one mortality in a patient who was found to have a concomitant HCC. This patient went on to develop portal vein thrombosis from tumour progression and, having shown no response to chemotherapy, succumbed to his illness 24 months post resection. Two patients in the surgically managed groups have developed recurrent disease and one of these was symptomatic 29 months after surgery. This compares with five patients with atypical pain in the non-operative group, who are currently under investigation to rule out other disease as a cause, prior to consideration for resection.
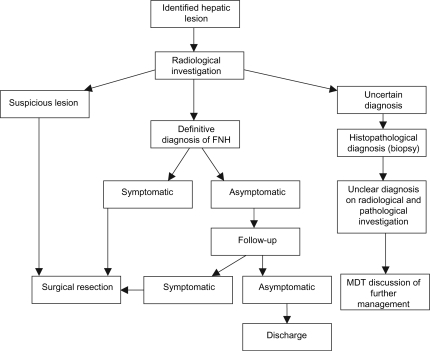
In conclusion, FNH is a benign lesion of the liver that can cause pain that is associated with the increase in size of the lesion. Surgical resection is usually performed for persistent pain or for lesions that are suspicious on radiological and pathological investigations. We propose a management algorithm for the diagnosis and management of these patients (Figure 1). In this series, using these criteria, there has been no mortality directly due to the surgical procedure and a modest morbidity, justifying surgical resections in selected patients.
Figure 1. .
Algorithm for management of FNH. MDT, multi-disciplinary team.
Acknowledgements and disclosures
No disclosures.
References
- 1.Luciani A, Kobeiter H, Maison P, Cherqui D, Zafrani ES, Dhumeaux D, et al. Focal nodular hyperplasia of the liver in men: is presentation the same in men and women? Gut. 2002;50:877–80. doi: 10.1136/gut.50.6.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cherqui D, Rahmouni A, Charlotte F, Boulahdour H, Metreau JM, Meignan M, et al. Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology. 1995;22:1674–81. [PubMed] [Google Scholar]
- 3.Kerlin P, Davis GL, McGill DB, Weiland LH, Adson MA, Sheedy PF II. Hepatic adenoma and focal nodular hyperplasia: clinical, pathologic, and radiologic features. Gastroenterology. 1983;84:994. [PubMed] [Google Scholar]
- 4.Pain JA, Gimson AES, Williams R, Howard ER. Focal nodular hyperplasia of the liver: results of treatment and options in management. Gut. 1991;32:524. doi: 10.1136/gut.32.5.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen BN, Flejou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441–54. doi: 10.1097/00000478-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Baum JK, Bookstein JJ, Holtz F, Klein EW. Possible association between benign hepatomas and oral contraceptives. Lancet. 1973;2:926–9. doi: 10.1016/s0140-6736(73)92594-4. [DOI] [PubMed] [Google Scholar]
- 7.Laurent C, Trillaud H, Lepreux S, Balabaud C, Bioulac-Sage P. Association of adenoma and focal nodular hyperplasia: experience of a single French academic center. Comp Hepatol. 2003;2:6. doi: 10.1186/1476-5926-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathieu D, Kobeiter H, Maison P, Rahmouni A, Cherqui D, Zafrani ES, et al. Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology 2000;118:560–4(Erratum in: Gastroenterology 2000;119:280). [DOI] [PubMed] [Google Scholar]
- 9.Vilgrain V. Focal nodular hyperplasia. Eur J Radiol. 2006;58:236–45. doi: 10.1016/j.ejrad.2005.11.043. [DOI] [PubMed] [Google Scholar]
- 10.Saul SH, Titelbaum DS, Gansler TS, Varello M, Burke DR, Atkinson BF, et al. The fibrolamellar variant of hepatocellular carcinoma: its association with focal nodular hyperplasia. Cancer. 1987;60:3049–55. doi: 10.1002/1097-0142(19871215)60:12<3049::aid-cncr2820601232>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 11.Saxena R, Humphreys S, Williams R, Portmann B. Nodular hyperplasia surrounding fibrolamellar carcinoma: a zone of arterialized liver parenchyma. Histopathology. 1994;25:275–8. doi: 10.1111/j.1365-2559.1994.tb01328.x. [DOI] [PubMed] [Google Scholar]
- 12.Chen TC, Chou TB, Ng KF, Hsieh LL, Chou YH. Hepatocellular carcinoma associated with focal nodular hyperplasia. Report of a case with clonal analysis. Virchows Arch. 2001;438:408–11. doi: 10.1007/s004280000348. [DOI] [PubMed] [Google Scholar]
- 13.Vibert E, Perniceni T, Levard H, Denet C, Shahri NK, Gayet B. Laparoscopic liver resection. Br J Surg. 2006;93:67–72. doi: 10.1002/bjs.5150. [DOI] [PubMed] [Google Scholar]
- 14.Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, et al. Hepatobiliary and Pancreatic Section of the Royal Belgian Society of Surgery and the Belgian Group for Endoscopic Surgery. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg. 2002;236:90–7. doi: 10.1097/00000658-200207000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]