Abstract
The goal of this prospective, randomized, blinded trial was to determine if ligament balancing techniques for rotating platform TKA affect postoperative knee kinematics. Sixteen patients with unilateral rotating platform TKA consented to participate in this institutional review board approved study. Eight patients were randomly selected to receive ligament balancing with an instrumented joint spreader device and eight patients received ligament balancing using fixed thickness spacer blocks. A single plane shape matching technique was used for kinematic analysis of static deep knee flexion and dynamic stair activities. There were no differences in knee kinematics between groups during static deep flexion activities. The spreader group demonstrated kinematics more similar to the normal knee during the ascending phase of the dynamic stair activity. Knee kinematics in static knee flexion were unaffected by ligament balancing technique, while knees balanced with the spreader demonstrated a medial pivot motion pattern during stair ascent. This medial pivot motion pattern may improve long-term results by more closely replicating normal knee kinematics.
Keywords: Spreader balancing device, Soft tissue balancing, Knee kinematics, TKA, Rotating platform, Randomized control trial
Introduction
Rotating-platform total knee arthroplasty (TKA) has become increasingly popular because this type of design provides good tibiofemoral conformity and low contact stresses without imposing rotational constraint [28]. These designs have been used for well over 20 years with excellent survivorship [10]. Recent kinematic studies of rotating platform knee arthroplasties have shown excellent stability in extension, but frequent anterior translation of the femur with respect to the tibia in flexed postures [6]. These anterior femoral translations may reduce maximum weightbearing flexion [4] and implant longevity [9], and therefore merit further study.
Tibiofemoral translations are influenced by ligament balance [4, 16, 21, 30], muscle and external forces, and implant design. Ligament balance is thought to play a particularly important role in the function of rotating-platform knee arthroplasties, and numerous balancing techniques have been reported [8, 12, 13, 18]. However, no well designed clinical studies of ligament balance and knee kinematics have been reported.
By performing a prospective, randomized, blinded trial of two ligament balancing techniques for rotating platform TKA, we sought to determine if ligament balancing technique affected postoperative knee kinematics. We hypothesized that ligament balancing with a calibrated spreader/balancer would provide better controlled knee kinematics, specifically reduced anterior femoral translations with flexion, than ligament balancing with fixed thickness spacer blocks.
Materials and methods
Sixteen patients with unilateral osteoarthritis of the knee and with no history of knee injuries or trauma consented to participate in this prospective, randomized, blinded, and institutional review board approved study. All subjects received the same rotating platform, PCL-retaining total knee prosthesis (TC-PLUS SB Solution, Plus Orthopedics AG, Rotkreuz, Switzerland, Fig. 1). The subjects were randomly assigned to two groups preoperatively: eight knees received the prosthesis using a ligament balancing technique employing fixed thickness spacer blocks (control group), while the other eight knees received the same prosthesis employing a calibrated spreader/balancer device to equalize the joint gaps and ligament balance in flexion and extension (spreader group) (Fig. 2).
Fig. 1.

All patients received a rotating platform total knee arthroplasty (TC-PLUS SB Solution, Plus Orthopedics, Rotkreuz, Switzerland)
Fig. 2.
One group of knees was treated using fixed thickness spacer blocks for ligament balancing (control group, left) and the other group was treated using a calibrated tensioning device (spreader group, right)
All surgeries were performed by the senior surgeon (FK) at South–West London Elective Orthopaedic Centre, Epsom, United Kingdom. All study subjects were operated in the supine position under spinal anesthesia and sedation, and each was administered prophylactic antibiotic prior to inflation of the tourniquet. Standard extramedullary and intramedullary instrumentation were used in all knees for preparation of the tibia and femur, respectively. Standard sequential soft-tissue releasing techniques [22, 29] were utilized in the control and spreader groups, which included resection or release of (1) the anterior fibres of PCL, (2) medial and posteromedial capsule, (3) medial osteophytes, and (4) superficial MCL. In the control group spacer blocks were used in extension and 90 degree flexion to guide soft tissue releases to create balanced and equal flexion–extension gaps. In the spreader group a balancer device (laminar spreader, Plus Orthopedics AG) (Fig. 2) was used in extension and 90 degree flexion to guide soft tissue releases to create balanced and equal flexion–extension gaps. Soft-tissue balance was assessed at 0 and 90 degrees of flexion with patella equally subluxed during measurements in both spreader and spacer block groups in order to accommodate appropriate measuring device into the joint space. A standard force of 20 N was applied to the medial and lateral jaws of the balancing device during this technique [23]. The posterior cruciate ligament (PCL) was retained in all knees with a bone block on the proximal tibia, recessing anterior fibers when necessary to achieve suitable balance.
Study subjects were assessed with pre-operative plain anteroposterior and lateral weightbearing radiographs of the knee and immediately postoperative non-weightbearing anteroposterior and lateral weightbearing radiographs. Patients were assessed post-operatively and over an average follow-up time of 11 ± 3 months (range: 7–15 months). The Knee Society Score [14] was employed as the scoring instrument. There were no differences between the control and spreader groups for height, weight, age, sex distribution, preoperative deformity or preoperative clinical scores (Table 1).
Table 1.
Patient demographics and clinical assessments (mean ± 1SD)
| Control | Spreader | P value | |
|---|---|---|---|
| Age at operation (years) | 71.0 ± 8.4 | 72.2 ± 6.6 | 0.96 |
| Height (cm) | 167 ± 7.6 | 165 ± 7.8 | 0.65 |
| Weight (kg) | 75.0 ± 22.6 | 70.3 ± 12.9 | 0.72 |
| Sex (M/F) | 3/5 | 4/4 | 1.0a |
| Varus/valgus distribution | 8/0 | 7/1 | 1.0a |
| Pre-op knee score | 42.1 ± 10.3 | 50.0 ± 11.7 | 0.13 |
| Pre-op function score | 50.0 ± 18.9 | 55.0 ± 20.4 | 0.50 |
| Post-op knee score | 90.5 ± 5.9 | 93.5 ± 1.8 | 0.51 |
| Post-op function score | 81.3 ± 23.4 | 88.1 ± 15.1 | 0.72 |
| Follow-up (months) | 10.3 ± 3.1 | 11.3 ± 2.3 | 0.44 |
aFisher’s exact test
Follow-up consisted of clinical and fluoroscopic assessment performed at Mayday University hospital, Croydon, United Kingdom. Fluoroscopic imaging (Siemens Polystar TOP, Siemens AG, Munich, Germany) consisted of (1) weightbearing maximum flexion lunge activity, (2) kneeling on a padded bench to maximum comfortable flexion and (3) a 4 cycles of a step-up/down on a 25 cm step. For the stair activity, the subjects faced the same direction throughout the cycle, therefore, the step-down was a backward motion that reversed the step ascent motion. Patients were instructed on the study activities prior to recording, and were given an opportunity to practice until comfortable. Lateral fluoroscopic views of the knee were recorded in the maximally flexed positions for the lunge and kneeling activities, as were four repeat trials of step-up/down on the stair. The fluoroscopic images were recorded at 15 frames per second onto an S-VHS VCR. Views of calibration targets also were acquired for distortion correction and optical calibration.
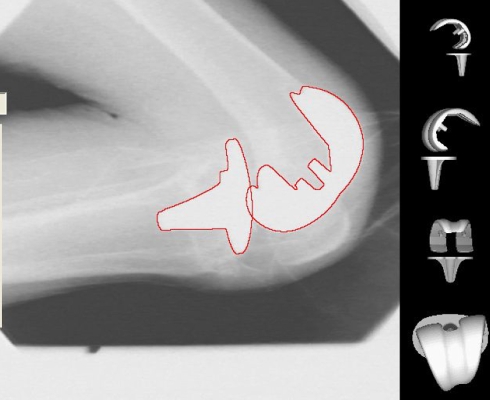
The three-dimensional (3D) positions and orientations of the implant components were determined using model based shape matching techniques [3, 5], including previously reported techniques, manual matching, and image space optimization routines (Fig. 3). The fluoroscopic images were digitized and corrected for static optical distortion. The optical geometry of the fluoroscopy system (principal distance, principal point) was determined from images of calibration targets [3, 5]. The implant surface model was projected onto the geometry corrected image, and its 3D pose was iteratively adjusted to match its silhouette with the silhouette of the subject’s TKA components. The results of this shape matching process have standard errors of approximately 0.5° to 1.0° for rotations and 0.5–1.0 mm for translations in the sagittal plane [3, 5].
Fig. 3.
Model based shape matching techniques are used to determine the three-dimensional pose of the arthroplasty components from fluoroscopic images. The fluoroscopic image shows the outlines, in red, of the implant surface models superimposed in their registered positions. The images along the right margin show medial, lateral, coronal and transverse views of the implant components’ relative orientations
The relative motions of the femoral and tibial components were determined from the 3D pose of each TKA component using the convention of Tupling and Pierrynowski [26]. The locations of condylar contact were estimated as the lowest point on each femoral condyle relative to the transverse plane of the tibial baseplate. Anteroposterior translations of the condyles were computed with respect to the anteroposterior midpoint of the tibial baseplate. Motion of the mobile bearing was not analyzed since the mobile bearing insert was not visible in the X-ray images and could not be tracked without addition of metallic markers.
Researchers were unblinded to subject group membership only after all kinematic data had been produced. Statistical comparisons of the fluoroscopic images were performed (SPSS ver 13, SPSS Inc., Chicago, US) using two-way repeated measures ANOVA with post hoc pair-wise comparisons (Tukey/Kramer) at a 0.05 level of significance. All other parameters were evaluated using non-parametric tests.
Results
Both the Knee Score and the Function Score were slightly lower for the control group (Table 1). This tendency existed pre-operatively but was not statistically significant.
For the maximum kneeling activity, no significant differences were found in knee angles or translations (Table 2). Maximum implant flexion for the control and spreader groups averaged 102° ± 13° and 108° ± 10° (P = 0.34), respectively. Tibial component valgus for the control and spreader groups averaged 0° ± 2° and −1° ± 2° (P = 0.56), respectively. Tibial external rotation for the control and spreader groups averaged −5° ± 7° and −5° ± 6° (P = 0.87), respectively. Medial tibial contact was located 2.7 ± 12.2 and 1.8 ± 8.2 mm (P = 0.87) posterior to the midline of the tibial plateau for the control and spreader groups, respectively. Lateral tibial contact was located at 10.5 ± 11.4 and 11.1 ± 11.8 mm (P = 0.93) posterior to the midline of the tibial plateau for the control and spreader groups, respectively.
Table 2.
Knee pose during maximum flexion kneeling (mean ± 1SD)
| Group | Flexion (°) | Valgus (°) | Tibial Ext. Rot. (°) | Medial AP (mm) | Lateral AP (mm) |
|---|---|---|---|---|---|
| Control | 102.0 ± 12.8 | 0.1 ± 2.1 | −4.7 ± 7.4 | −2.7 ± 12.2 | −10.5 ± 11.4 |
| Spreader | 107.9 ± 10.1 | −0.5 ± 1.8 | −5.3 ± 6.3 | −1.8 ± 8.2 | −11.1 ± 11.8 |
| P value | 0.34 | 0.56 | 0.87 | 0.87 | 0.93 |
For the maximum lunge activity, no significant differences were found in knee angles or translations (Table 3). Knee flexion for the control and spreader groups averaged 95° ± 15° and 102° ± 11° (P = 0.36), respectively. Tibial component valgus for the control and spreader groups averaged 0° ± 1° and −1° ± 2° (P = 0.62), respectively. Tibial external rotation for the control and spreader groups averaged −9° ± 6° and −6° ± 7° (P = 0.29), respectively. Medial tibial contact was located 0.3 ± 8.2 mm and 6.7 ± 7.7 mm (p = 0.1.5) posterior to the midline of the tibial plateau for the control and spreader groups, respectively. Lateral tibial contact was located 16.5 ± 8.7 mm and 16.8 ± 9.9 mm (p = 0.96) posterior to the midline of the tibial plateau for the control and spreader groups, respectively.
Table 3.
Knee pose during maximum flexion lunge (mean ± 1SD)
| Group | Flexion (°) | Valgus (°) | Tibial Ext. Rot. (°) | Medial AP (mm) | Lateral AP (mm) |
|---|---|---|---|---|---|
| Control | 95.3 ± 15.1 | −0.1 ± 1.4 | −9.6 ± 5.9 | −0.3 ± 8.2 | −16.5 ± 8.7 |
| Spreader | 101.6 ± 10.6 | −0.6 ± 2.1 | −5.7 ± 7.3 | −6.7 ± 7.7 | −16.8 ± 9.9 |
| P value | 0.36 | 0.62 | 0.29 | 0.15 | 0.96 |
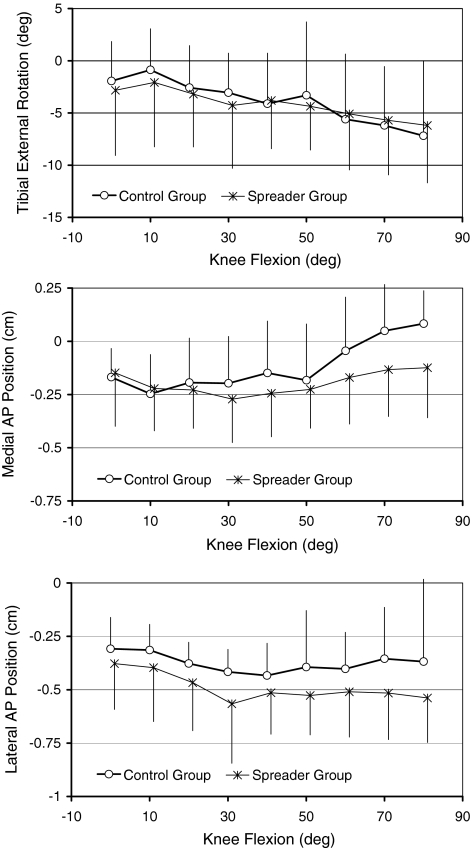
For the stair activity, knees in the spreader group exhibited more posterior medial (P = 0.04, RM-ANOVA) and lateral (P < 0.005, RM-ANOVA) condylar contact than the control knees. There was no difference in average tibial rotation between the two groups, and no pair-wise comparisons at specific flexion ranges resulted in significant differences (Fig. 4). On average, both groups of knees had approximately 2° tibial internal rotation at 0° flexion, and rotated to 7° tibial internal rotation at 80° flexion. Medial contact was observed to remain at approximately 2 mm posterior to the AP midpoint from 0° to 50° flexion, then moved anterior to 80° flexion. The control group showed greater anterior translation of medial contact from 50° to 80° flexion than did the spreader group. Lateral contact was more posterior in the spreader group throughout the stair activity. Both groups showed posterior translation of lateral contact of 2–3 mm from 0° to 30° flexion, with very little net translation from 30° to 80° flexion.
Fig. 4.
Knee motions during the stair activity differed between the control and spreader groups. Condylar positions were significantly more posterior in the spreader group. There were no significant differences in tibial rotation, nor were there significant pair-wise differences for rotations or translations
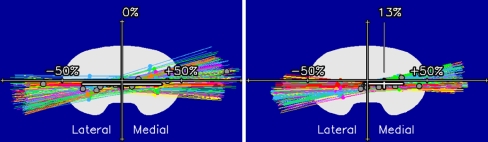
Tibiofemoral kinematics during the step activity also were compared using average centers of rotation (COR) for femoral motion with respect to the tibial base-plate (Fig. 5) [6]. The COR provides a concise measure of femoral AP translation—if the COR is central (close to 0%), the femur rotates about the center of the tibia with little AP translation. A medial COR (between 0% and +50%) indicates the femur translates posterior with external rotation during flexion. A lateral COR (between −50 and 0%) indicates the femur translates anterior with external rotation during flexion. For the entire step-up/down cycle, the centers of rotation were at 0% (central) and 13% (medial) (P = 0.058) for the control and spreader groups, respectively. When step-up kinematics were compared, the spreader group showed a COR located more medially (28%) than the control group (0%, P < 0.05, Table 4). There was no difference in COR for step-down kinematics (Table 4). Both groups of knees showed tibial internal rotation with knee flexion, 8.5° and 7.6° for the control and spreader groups, respectively. These differences were not statistically significant.
Fig. 5.
Average centers of rotation for the entire stair activity were in the center of the tibial plateau (0%) for the control group (left) and to the medial side (13%) for the spreader group (right). This difference was not significant (P = 0.058)
Table 4.
Medial/lateral center of rotation (COR) during the stair activity (mean ± 1SD)
| Group | Extension phase (%) | Flexion phase (%) |
|---|---|---|
| Control | −3 ± 19 | −4 ± 2 |
| Spreader | 28 ± 41 | −3 ± 3 |
| P value | <0.05 | >0.05 |
None of the subjects demonstrated valgus or varus angles larger than 2 degrees during motion, consequently there was no obvious evidence of condylar lift-off.
Discussion
One goal of TKA is to reproduce normal knee kinematics. Ligament and soft-tissue balance are thought to play critical roles in obtaining optimal kinematic behavior. Theoretical merits of many balancing techniques and instruments have been discussed [13, 25, 27, 30]. This prospective, randomized and blinded study evaluated two ligament balancing techniques with posterior cruciate retaining rotating platform total knee arthroplasty to determine if balancing technique affected knee kinematics. Randomizing patients for surgical treatment and blinding the investigators to group membership until after all data had been processed reduced the potential for selection, measurement, and interpretation bias to affect the study findings. All subjects demonstrated satisfactory knee function based on clinical scores, there were no clinical complications in any knee, and no evidence of condylar lift-off was found during dynamic activity.
The two knee groups exhibited no significant differences in knee kinematics for the weightbearing lunge and passive kneeling activities. This similarity is not unexpected given the posterior cruciate was retained in all knees. It is interesting to note that tibiofemoral AP position in these knees appears to differ from previous reports with mobile bearing knee arthroplasties. Banks et al. [4] reported lunge kinematics for a mixed group of rotating platform and rotating-and-translating arthroplasties during the same lunge activity, and observed 102° average flexion, 7.7° average tibial internal rotation, and 2.2 mm posterior femoral position with respect to the tibial AP midpoint. The control and spreader groups exhibited approximately the same knee angles, but 8.4 and 11.8 mm posterior femoral position, respectively. Greater posterior femoral translation with flexion is suggestive of more physiologic posterior cruciate ligament function and knee mechanics, although there is insufficient information to attribute those translations specifically to surgical technique, implant design, or a combination of factors. The amount of tibial rotation observed in the flexed postures is similar to other previous reports for knee arthroplasties [6, 15] but is much smaller than the amount of tibial rotation observed in healthy knees in similar postures [1, 20].
Ligament balancing technique did affect knee kinematics during the dynamic stair activity. Condylar contact locations were observed to remain more posterior on the tibia and to have a more medial center of rotation during step-up in the spreader group. These findings suggest the spreader balancing technique provided more normal balance or stability to the medial compartment of the knee, resulting in less medial contact translation during the stair activity. Medial contact in the control group was observed to move anterior with flexion on the stair activity, indicating greater functional laxity in that compartment.
Simple comparisons of knee kinematics across groups are possible using the center of rotation characterization. A medial center of rotation has been described in the healthy normal knee [2, 17]. The spreader group showed a medial center of rotation during stair ascent, indicating medial contact did not move significantly while lateral contact moved anterior with knee extension and femoral internal rotation. The control group showed a center of rotation close to the middle of the tibia for the stair activity, indicating that the femur rotated internally during knee extension with little AP translation (medial contact moved posterior and lateral contact moved anterior with extension). The center of rotation in the spreader group knees differed between the ascending (medial COR) and descending (central COR) phases of the step-up/down activity (Table 4). This suggests that the spreader balancing technique provided greater anterior medial stability than the technique employing fixed thickness spacer blocks, but posterior medial stability was equivalent between the two balancing techniques. Banks and Hodge [7] reported on a mixed group of 44 rotating platform and rotating-and-translating mobile bearing knee arthroplasties during the same stair activity, and found average tibial rotations of 9° and average centers of rotation at −19% (lateral). These motions were associated with anterior femoral translation with flexion, which has been observed in numerous knee arthroplasty designs [11, 19, 24]. The knees in the present study showed similar amounts of tibial rotation, but both groups showed centers of rotation that were more medially located. Thus, the knees in this study exhibited less anterior femoral translation with flexion compared to the knees in the previous report, suggesting both balancing techniques provided beneficial tibiofemoral stability compared to the group average of well-functioning mobile-bearing knee arthroplasties.
This double-blinded prospective randomized study used fluoroscopic kinematic measurements to determine if two ligament balancing techniques would affect knee motions in several activities. Kinematics in flexion were similar, with both groups showing a more posterior femoral position than previously has been reported for similar implant designs. Knees operated with a spreader/balancer device showed a more medial center of rotation in ascending a stair activity, and both groups showed average centers of rotation that were more medial than previously had been reported for similar implant designs. Kinematics closer to the normal knee may yield improved knee performance and implant longevity. However, these kinematic differences are clinically insignificant upon short-term follow up, and their long-term significance remains to be studied.
Acknowledgments
This study was supported by Plus Orthopedics AG (Switzerland). The experiments in this study, which was carried out in London, England, complied with the current laws of Great Britain. Funding: This study was supported by Plus Orthopedics AG.
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Contributor Information
K. Gamada, Email: kazgamada@ortho-pt.com
S. A. Banks, Phone: +1-352-3926109, FAX: +1-352-3927303, Email: banks@ufl.edu
References
- 1.Andriacchi TP, Dyrby CO, Johnson TS (2003) The use of functional analysis in evaluating knee kinematics. Clin Orthop 44–53 [DOI] [PubMed]
- 2.Asano T, Akagi M, Tanaka K, Tamura J, Nakamura T (2001) In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clin Orthop 157–166 [DOI] [PubMed]
- 3.Banks S (1992) Model based 3D kinematic estimation from 2D perspective silhouettes: application with total knee prosthesis. PhD Dissertation. Massachusetts Institute of Technology, Cambridge
- 4.Banks S, Bellemans J, Nozaki H, Whiteside LA, Harman M, Hodge WA (2003) Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res 131–138 [DOI] [PubMed]
- 5.Banks SA, Hodge WA (1996) Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng 43:638–649 [DOI] [PubMed]
- 6.Banks SA, Hodge WA (2004) 2003 Hap Paul Award paper of the international society for technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty 19:809–816 [DOI] [PubMed]
- 7.Banks SA, Hodge WA (2004) Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res 187–193 [DOI] [PubMed]
- 8.Bathis H, Perlick L, Tingart M, Luring C, Perlick C, Grifka J (2004) Flexion gap configuration in total knee arthroplasty following high tibial osteotomy. Int Orthop 28:366–369 [DOI] [PMC free article] [PubMed]
- 9.Blunn GW, Walker PS, Joshi A, Hardinge K (1991) The dominance of cyclic sliding in producing wear in total knee replacements. Clin Orthop 253–260 [PubMed]
- 10.Buechel FF Sr, Buechel FF Jr, Pappas MJ, D’Alessio J (2001) Twenty-year evaluation of meniscal bearing and rotating platform knee replacements. Clin Orthop 388:41–50 [DOI] [PubMed]
- 11.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (2001) The influence of femoral rollback on patellofemoral contact loads in total knee arthroplasty. J Arthroplasty 16:909–918 [DOI] [PubMed]
- 12.Clemens U, Miehlke RK (2005) Advanced navigation planning including soft tissue management. Orthopedics 28:s1259–1262 [DOI] [PubMed]
- 13.Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973 [DOI] [PubMed]
- 14.Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop 248:13–14 [PubMed]
- 15.Kanekasu K, Banks SA, Honjo S, Nakata O, Kato H (2004) Fluoroscopic analysis of knee arthroplasty kinematics during deep flexion kneeling. J Arthroplasty 19:998–1003 [DOI] [PubMed]
- 16.Komistek RD, Scott RD, Dennis DA, Yasgur D, Anderson DT, Hajner ME (2002) In vivo comparison of femorotibial contact positions for press-fit posterior stabilized and posterior cruciate-retaining total knee arthroplasties. J Arthroplasty 17:209–216 [DOI] [PubMed]
- 17.Kurosawa H, Walker PS, Abe S, Garg A, Hunter T (1985) Geometry and motion of the knee for implant and orthotic design. J Biomech 18:487–499 [DOI] [PubMed]
- 18.Kuster MS, Bitschnau B, Votruba T (2004) Influence of collateral ligament laxity on patient satisfaction after total knee arthroplasty: a comparative bilateral study. Arch Orthop Trauma Surg 124:415–417 [DOI] [PubMed]
- 19.Li G, Zayontz S, Most E, Otterberg E, Sabbag K, Rubash HE (2001) Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty 16:150–156 [DOI] [PubMed]
- 20.Nagura T, Dyrby CO, Alexander EJ, Andriacchi TP (2002) Mechanical loads at the knee joint during deep flexion. J Orthop Res 20:881–886 [DOI] [PubMed]
- 21.Nozaki H, Banks SA, Suguro T, Hodge WA (2002) Observations of femoral rollback in cruciate-retaining knee arthroplasty. Clin Orthop Relat Res 308–314 [DOI] [PubMed]
- 22.Peters CL, Mohr RA, Bachus KN (2001) Primary total knee arthroplasty in the valgus knee: creating a balanced soft tissue envelope. J Arthroplasty 16:721–729 [DOI] [PubMed]
- 23.Ritschl P, Machacek F, Gruber F, Fuiko R, Wülser M (2006) Mechanical properties of soft tissues relevant for ligament balanced TKR measured in-vitro. CAOS, Montreal
- 24.Stiehl JB, Komistek RD, Cloutier JM, Dennis DA (2000) The cruciate ligaments in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplasties. J Arthroplasty 15:545–550 [DOI] [PubMed]
- 25.Takahashi T, Wada Y, Yamamoto H (1997) Soft-tissue balancing with pressure distribution during total knee arthroplasty. J Bone Joint Surg Br 79:235–239 [DOI] [PubMed]
- 26.Tupling SJ, Pierrynowski MR (1987) Use of cardan angles to locate rigid bodies in three-dimensional space. Med Biol Eng Comput 25:527–532 [DOI] [PubMed]
- 27.Wallace AL, Harris ML, Walsh WR, Bruce WJ (1998) Intraoperative assessment of tibiofemoral contact stresses in total knee arthroplasty. J Arthroplasty 13:923–927 [DOI] [PubMed]
- 28.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech 35:543–548 [DOI] [PubMed]
- 29.Yagishita K, Muneta T, Ikeda H (2003) Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty 18:313–320 [DOI] [PubMed]
- 30.Zalzal P, Papini M, Petruccelli D, de Beer J, Winemaker MJ (2004) An in vivo biomechanical analysis of the soft-tissue envelope of osteoarthritic knees. J Arthroplasty 19:217–223 [DOI] [PubMed]