Abstract
Hyperglycemic episodes, which complicate even well-controlled cases of diabetes, lead to increased polyol pathway flux, activation of protein kinase C and accelerated non-enzymatic formation of advanced glycation end products. Many of these pathways become activated in response to the production of superoxide anion. Superoxide can interact with nitric oxide, forming the potent cytotoxin peroxynitrite. Peroxynitrite attacks various biomolecules in the vascular endothelium, vascular smooth muscle and myocardium, eventually leading to cardiovascular dysfunction via multiple mechanisms. This review focuses on emerging evidence suggesting that peroxynitrite plays a key role in the pathogenesis of the cardiovascular complications of diabetes, which underlie the development and progression of diabetic retinopathy, neuropathy and nephropathy.
Introduction
Diabetes mellitus is one of the most prevalent (the estimated lifetime risk of developing diabetes for individuals born in 2000 is 32.8% for males and 38.5% for females) and costly chronic diseases, which significantly reduces life expectancy [1]. The majority of diabetic complications are related to pathophysiological alterations in the vasculature, with macro- and microvascular disease being the most common cause of morbidity and mortality in patients with diabetes mellitus. Atherosclerosis is the most common macrovascular complication of diabetes, and increases the risk for stroke, myocardial infarction and peripheral artery disease, the latter being the leading cause of limb amputation in civilized countries. Microvascular complications comprise retinopathy and nephropathy — the leading causes of blindness and renal failure [1].
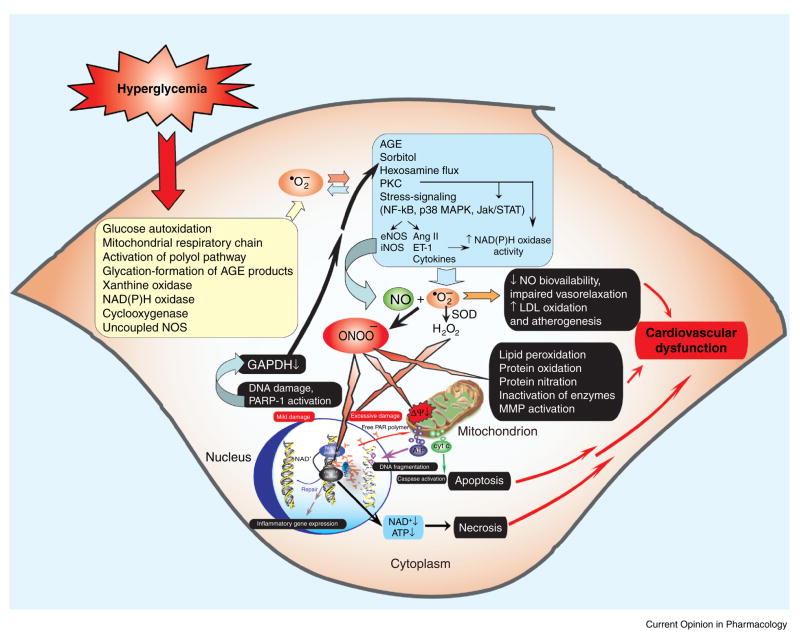
Hyperglycemic episodes, which complicate even well-controlled cases of diabetes, are closely associated with increased oxidative and nitrosative stress, which can trigger the development of diabetic cardiovascular complications (Figure 1). This review focuses on the role of nitrosative stress, particularly that of the reactive oxidant peroxynitrite (formed from the reaction of superoxide with nitric oxide), in the pathogenesis of diabetic complications.
Figure 1.
Mechanisms of cardiovascular dysfunction in diabetes: role of superoxide and peroxynitrite. Hyperglycemia induces increased superoxide anion (•O2−) production via activation of multiple pathways including xanthine and NAD(P)H oxidases, cyclooxygenase, uncoupled NOS, glucose autoxidation, the mitochondrial respiratory chain, polyol, and advanced glycation end products (AGEs). Superoxide activates AGEs, PKC, polyol (sorbitol), hexosamine and stress-signaling pathways, leading to increased expression of inflammatory cytokines, angiotensin II (Ang II), endothelin-1 (ET-1) and NAD(P)H oxidases, which in turn generate more superoxide via multiple mechanisms. Hyperglycemia-induced superoxide generation might also favour increased expression of NOSs through the activation of NF-κB, which increases the generation of NO. Superoxide anion quenches NO, thereby reducing the efficacy of a potent endothelium-derived vasodilator system. Superoxide can also be converted to hydrogen peroxide (H2O2) by superoxide dismutase (SOD) and interact with NO to form a reactive oxidant, peroxynitrite (ONOO−), which induces cell damage via lipid peroxidation, inactivation of enzymes and other proteins by oxidation and nitration, and activation of matrix metalloproteinases (MMPs). Peroxynitrite also acts on mitochondria to decrease the membrane potential (Ψ) and trigger the release of proapoptotic factors such as cytochrome c (Cyt c) and apoptosis-inducing factor (AIF). These factors mediate caspase-dependent and -independent apoptotic death pathways. Peroxynitrite, in concert with other oxidants (e.g. H2O2), causes strand breaks in DNA, activating the nuclear enzyme PARP-1. Mild damage to DNA activates the DNA repair machinery. By contrast, once excessive oxidative- and nitrosative stress-induced DNA damage occurs, overactivated PARP-1 initiates an energy-consuming cycle by transferring ADP-ribose units (small red spheres) from NAD+ to nuclear proteins, resulting in rapid depletion of the intracellular NAD+ and ATP pools, slowing the rate of glycolysis and mitochondrial respiration, and eventually leading to cellular dysfunction and death. Poly(ADP-ribose) glycohydrolase (PARG) degrades poly(ADP-ribose) (PAR) polymers, generating free PAR polymer and ADP-ribose, which signals to the mitochondria to induce AIF release. PARP-1 activation also leads to the inhibition of cellular glyceraldehyde- 3-phosphate dehydrogenase (GAPDH) activity which, in turn, favours the activation of PKC, AGEs and the hexosamine pathway, leading to increased superoxide generation. PARP-1 also regulates the expression of a variety of inflammatory mediators, which might facilitate the progression of diabetic cardiovascular complications.
Pathogenesis of diabetic endothelial dysfunction: role of oxidative stress
Endothelial dysfunction in many diseases precedes and predicts, as well as predisposes, for subsequent, more severe vascular alterations. As such, endothelial dysfunction has been documented in various forms of diabetes, and even in pre-diabetic individuals [2–7].
The pathogenesis of endothelial dysfunction in diabetes is complex. The diabetic state is associated with increased oxidative stress, which plays an important role in the development of diabetic complications. Hyperglycemia triggers increased polyol pathway flux, altered cellular redox state, increased formation of diacylglycerol and the subsequent activation of specific protein kinase C isoforms, and accelerated non-enzymatic formation of advanced glycation end products [8–10]. Activation of many of these pathways results from the production of oxygen-derived oxidants, such as superoxide anion (Figure 1). Superoxide production, therefore, plays a significant role in the pathogenesis of the diabetes-associated endothelial dysfunction [9–11]. The cellular sources of superoxide anion are multiple and include NADH/NADPH and xanthine oxidases, the mitochondrial respiratory chain, the arachidonic acid cascade (including lipoxygenase and cycloxygenase), and microsomal enzymes [8]. Hyperglycemia-induced superoxide generation contributes to the increased expression of NAD(P)H oxidase which, in turn, generates more super-oxide anion. Among these pathways, mitochondrial generation of superoxide appears to play the most crucial role in diabetic complications. Hyperglycemia also favors increased expression of inducible nitric oxide synthase (iNOS) through the activation of nuclear factor-κB (NF-κB), which can increase the generation of nitric oxide (NO) [7,12]. Superoxide anion can quench NO, thereby reducing the efficacy of the potent endothelium-derived vasodilator system that participates in the homeostatic regulation of the vasculature [9].
Pathogenesis of diabetic endothelial dysfunction: role of nitrosative stress and peroxynitrite
Superoxide anion is able to interact with nitric oxide, which is produced physiologically by constitutive sources such as the endothelial isoform of nitric oxide synthase. This process results in the formation of the strong oxidant peroxynitrite, which attacks various biomolecules leading (among other processes) to the production of a modified amino acid, nitrotyrosine [13]. Nitrotyrosine was initially considered a specific marker of peroxynitrite generation, but now is generally regarded an index of reactive nitrogen species, rather than a specific indicator of peroxynitrite formation [14].
Peroxynitrite attacks various biomolecules, leading to cardiovascular dysfunction via multiple mechanisms [15•]. One of these pathways involves DNA strand breakage and consequent activation of the nuclear enzyme poly(ADP-ribose) polymerase (PARP; for reviews, see [15•,16]). PARP-1 activation emerges as a key process in the development of diabetic cardiovascular dysfunction both in diabetic animals and in humans [3,17,18] and might also contribute to the development of other diabetic complications such as nephropathy, neuropathy and retinopathy [19•]. Recent work on endothelial cells in conditions of elevated extracellular glucose has identified a novel mechanism by which PARP activation regulates the development of various pathways related to diabetic complications. In this scheme, elevated superoxide generation from the mitochondria (directly, or indirectly via the generation of peroxynitrite) induces DNA strand breaks and activates PARP which, in turn, induces the poly(ADP-ribosyl)ation of glyceraldehyde-3-phosphate dehydrogenase. The resulting metabolic alterations activate NF-κB, aldose reductase and the polyol pathways [20,21].
Accumulating evidence supports the hypothesis that diabetes is associated with increased nitrosative stress and peroxynitrite formation in numerous tissues, both in experimental animals and in humans [22]. For example, increased nitrotyrosine plasma levels are detectable in type 2 diabetic patients [23] and iNOS-dependent peroxynitrite production is increased in platelets from diabetic individuals [24]. Hyperglycemia induces increased nitrotyrosine formation in the artery wall of monkeys [25] and in diabetic patients during a period of postprandial hyperglycemia [26,27]. Increased nitrotyrosine immunoreactivity has also been demonstrated in the microvasculature of type 2 diabetic patients, which correlates with fasting blood glucose, endothelial dysfunction, and increased levels of HbA1c, intracellular adhesion molecule and vascular cellular adhesion molecule [3]. Toxic actions of peroxynitrite and/or nitrotyrosine in the cardiovascular system are also supported by evidence showing that the degree of cell death and/or dysfunction correlates with levels of nitrotyrosine in endothelial cells, myocytes and fibroblasts from heart biopsies of diabetic patients [28], hearts of streptozotocin-induced diabetic rats [29], and working hearts of rats during hyperglycemia [30]. Nitrotyrosine is directly harmful to endothelial cells [31], and high glucose-induced oxidative and nitrosative stress pathologically alters the prostanoid profile of human endothelial cells [4,32]. It has recently been suggested that there may be several phases in the pathogenesis of high glucose-induced endothelial injury: the short-term effect appears to depend upon combined oxidative and nitrosative stress with peroxynitrite formation, whereas the long-term effect is related to the generation of reactive oxygen species. In both cases, protein kinase C ultimately mediates the changes in vascular permeability [33].
Angiotensin II — a known factor in the pathogenesis of diabetic cardiovascular complications — can induce superoxide formation, which is mediated (at least in part) by vascular NAD(P)H oxidases. Reactive oxidant species, in turn, can exert direct oxidative effects, but can also signal through pathways involving mitogen-activated protein kinases, tyrosine kinases and transcription factors, leading to events such as inflammation, hypertrophy, remodeling and angiogenesis [34]. Recent work demonstrates that angiotensin II can also induce intra-endothelial peroxynitrite formation [35,36], as well as PARP activation [36].
Consistent with the role of peroxynitrite/nitrotyrosine in the pathogenesis of diabetic vascular dysfunction, neutralization of peroxynitrite with the metalloporphyrin peroxynitrite decomposition catalyst FP15 ameliorated the endothelial and cardiac dysfunction in a streptozotocin-induced murine model of diabetes [37].
Diabetic cardiomyopathy: role of nitrosative stress and peroxynitrite
Diabetic cardiomyopathy has been recognized for many decades and is characterized by complex changes in the biochemical, mechanical, structural and electrical properties of the heart, which can underlie the development of early diastolic or late systolic dysfunction (or both), and the increased incidence of cardiac arrhythmias in diabetic patients. Diabetes is now considered a potent independent risk factor for mortality in patients hospitalized with heart failure, particularly in females [38].
Accumulating pre-clinical and clinical evidence suggests that increased sympathetic activity, an activated cardiac reninangiotensin system, myocardial ischemia or functional hypoxia, and elevated circulating levels of glucose can result in oxidative and nitrosative stress in the cardiovascular system of diabetic animals and humans. As such, oxidative and nitrosative damage might be critical in the early onset of diabetic cardiomyopathy [28–30,37,39]. In cardiomyocytes grown in culture medium containing elevated glucose, pathophysiological alterations can be attenuated by antioxidants, NOS inhibitors and peroxynitrite-neutralizing agents, suggesting that these alterations are induced by oxidative and nitrosative stress [40]. Nitrotyrosine was also detected in cardiac myocytes from myocardial biopsy samples obtained from diabetic and diabetic-hypertensive patients [28] and in a mouse model of streptozotocin-induced diabetes [29]. Perfusion of isolated hearts with high glucose led to upregulation of iNOS, an increase in coronary perfusion pressure and an increase in NO and superoxide generation, conditions favoring the production of peroxynitrite; this was accompanied by the formation of nitrotyrosine and cardiac cell apoptosis [30].
As mentioned above, experimental and clinical evidence suggest that nitrosative stress and peroxynitrite play an important role in the pathogenesis of diabetic cardiomyopathy. It appears that pharmacological neutralization of peroxynitrite improves vascular and/or cardiac function, not only in experimental models of diabetes but also in other pathophysiological conditions of the heart that are associated with increased peroxynitrite formation. These include acute myocardial infarction, chronic ischemic heart failure, doxorubicin-induced cardiomyopathy and diabetic cardiomyopathy [41–43,15•]. The mechanism by which neutralization of peroxynitrite protects against cardiovascular dysfunction involves protection against vascular and myocardial tyrosine nitration, PARP activation and lipid peroxidation, as all of these have previously been linked to diabetic cardiomyopathy as well as to peroxynitrite-induced cardiac injury [15•]. Additional mechanisms of peroxynitrite-mediated diabetic cardiac dysfunction include inhibition of myofibrillar creatine kinase [41] and succinyl-CoA:3-oxoacid CoA-transferase [44] and activation of metalloproteinases [15•].
The observations described above support the concept that peroxynitrite is a major mediator of myocardial injury in various pathophysiological conditions, and its effective neutralization can be of significant therapeutic benefit [15•]. Accumulating experimental evidence suggests that peroxynitrite might also be involved in the pathogenesis of primary diabetes [37], diabetic microvascular injury in retinopathy [45–47], nephropathy [48,49] and neuropathy [50•,51,52•], but the detailed description of these studies is beyond the scope of the present review [22].
Conclusions and implications
Several lines of evidence reviewed herein support the view that nitrosative stress and peroxyntrite-induced damage play a pivotal role in the pathogenesis of diabetic cardiovascular complications (see Figure 1). Neutralization of reactive nitrogen species and inhibition of downstream effector pathways, including the inhibition of PARP activation, emerge as novel approaches for the prevention or reversal of diabetic cardiovascular complications, as well as of neuropathy, nephropathy and retinopathy. Of note, hyperglycemia is a strong trigger of reactive oxygen and nitrogen species formation in the cardiovascular system; therefore, tight glycemic control in diabetics could be one of the best ways to prevent reactive species production and initiation of downstream pathways of myocardial injury. It remains to be seen whether various therapeutic drugs with well-known cardiovascular protective effects (e.g. antioxidants, statins, β-blockers, angiotensin-converting enzyme inhibitors) are able to suppress peroxynitrite formation and PARP activation in the cardiovascular system.
Acknowledgments
The authors of this paper are supported by the Intramural Research of NIH/NIAAA (to PP), the European Foundation for the Study of Diabetes (EFSD), the Hungarian Scientific Research Fund (OTKA) and the NIH (to CS).
Footnotes
This review comes from a themed issue on Cardiovascular and renal Edited by Christoph Thiemermann and Magdi Yaqoob
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
- 1.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 2.Ruderman NB, Williamson JR, Brownlee M. Glucose and diabetic vascular disease. FASEB J. 1992;6:2905–2914. doi: 10.1096/fasebj.6.11.1644256. [DOI] [PubMed] [Google Scholar]
- 3.Szabo C, Zanchi A, Komjati K, Pacher P, Krolewski AS, Quist WC, LoGerfo FW, Horton ES, Veves A. Poly(ADP-Ribose) polymerase is activated in subjects at risk of developing type 2 diabetes and is associated with impaired vascular reactivity. Circulation. 2002;106:2680–2686. doi: 10.1161/01.cir.0000038365.78031.9c. [DOI] [PubMed] [Google Scholar]
- 4.Cosentino F, Eto M, De Paolis P, van der Loo B, Bachschmid M, Ullrich V, Kouroedov A, Delli Gatti C, Joch H, Volpe M, Luscher TF. High glucose causes upregulation of cyclooxygenase-2 and alters prostanoid profile in human endothelial cells: role of protein kinase C and reactive oxygen species. Circulation. 2003;107:1017–1023. doi: 10.1161/01.cir.0000051367.92927.07. [DOI] [PubMed] [Google Scholar]
- 5.Caballero AE, Arora S, Saouaf R, Lim SC, Smakowski P, Park JY, King GL, LoGerfo FW, Horton ES, Veves A. Microvascular and macrovascular reactivity is reduced in subjects at risk for type 2 diabetes. Diabetes. 1999;48:1856–1862. doi: 10.2337/diabetes.48.9.1856. [DOI] [PubMed] [Google Scholar]
- 6.Calles-Escandon J, Cipolla M. Diabetes and endothelial dysfunction: a clinical perspective. Endocr Rev. 2001;22:36–52. doi: 10.1210/edrv.22.1.0417. [DOI] [PubMed] [Google Scholar]
- 7.Cosentino F, Hishikawa K, Katusic ZS, Luscher TF. High glucose increases nitric oxide synthase expression and superoxide anion generation in human aortic endothelial cells. Circulation. 1997;96:25–28. doi: 10.1161/01.cir.96.1.25. [DOI] [PubMed] [Google Scholar]
- 8.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 9.Ceriello A. New insights on oxidative stress and diabetic complications may lead to a ‘causal’ antioxidant therapy. Diabetes Care. 2003;26:1589–1596. doi: 10.2337/diacare.26.5.1589. [DOI] [PubMed] [Google Scholar]
- 10.Guzik TJ, Mussa S, Gastaldi D, Sadowski J, Ratnatunga C, Pillai R, Channon KM. Mechanisms of increased vascular superoxide production in human diabetes mellitus: role of NAD(P)H oxidase and endothelial nitric oxide synthase. Circulation. 2002;105:1656–1662. doi: 10.1161/01.cir.0000012748.58444.08. [DOI] [PubMed] [Google Scholar]
- 11.Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, Yorek MA, Beebe D, Oates PJ, Hammes HP, Giardino I, Brownlee M. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000;404:787–790. doi: 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- 12.Spitaler MM, Graier WF. Vascular targets of redox signalling in diabetes mellitus. Diabetologia. 2002;45:476–494. doi: 10.1007/s00125-002-0782-0. [DOI] [PubMed] [Google Scholar]
- 13.Beckman JS, Koppenol WH. Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and ugly. Am J Physiol. 1996;271:C1424–C1437. doi: 10.1152/ajpcell.1996.271.5.C1424. [DOI] [PubMed] [Google Scholar]
- 14.Halliwell B. What nitrates tyrosine? Is nitrotyrosine specific as a biomarker of peroxynitrite formation in vivo? FEBS Lett. 1997;411:157–160. doi: 10.1016/s0014-5793(97)00469-9. [DOI] [PubMed] [Google Scholar]
- 15•.Pacher P, Schulz R, Liaudet L, Szabo C. Nitrosative stress and pharmacological modulation of heart failure. Trends Pharmacol Sci. 2005;26:302–310. doi: 10.1016/j.tips.2005.04.003. A recent overview on the mechanisms of peroxynitrite-induced cardiovascular dysfunction in various forms of heart failure. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Virág L, Szabó C. The therapeutic potential of PARP inhibition. Pharmacol Rev. 2002;54:375–429. doi: 10.1124/pr.54.3.375. [DOI] [PubMed] [Google Scholar]
- 17.Garcia Soriano F, Virág L, Jagtap P, Szabó É, Mabley JG, Liaudet L, Marton A, Hoyt DG, Murthy KG, Salzman AL, Southan GJ, Szabo C. Diabetic endothelial dysfunction: the role of poly (ADP-ribose) polymerase activation. Nat Med. 2001;7:108–113. doi: 10.1038/83241. [DOI] [PubMed] [Google Scholar]
- 18.Pacher P, Liaudet L, Soriano FG, Mabley JG, Szabó É, Szabó C. The role of poly(ADP-ribose) polymerase in the development of myocardial and endothelial dysfunction in diabetes mellitus. Diabetes. 2002;51:514–521. doi: 10.2337/diabetes.51.2.514. [DOI] [PubMed] [Google Scholar]
- 19•.Pacher P, Szabo C. Role of poly(ADP-ribose) polymerase-1 (PARP) activation in the pathogenesis of diabetic complications: endothelial dysfunction, as a common underlying theme. Antioxid Redox Signal. 2005;7:1568–1580. doi: 10.1089/ars.2005.7.1568. A recent overview on the role of PARP activation in diabetic complications. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du X, Matsumura T, Edelstein D, Rosetti L, Zsengellér Z, Szabó C, Brownlee M. Inhibition of GAPDH activity by poly(ADP-ribose) polymerase activates three major pathways of hyperglycemic damage in endothelial cells. J Clin Invest. 2003;112:1049–1057. doi: 10.1172/JCI18127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jagtap P, Szabo C. Poly(ADP-ribose) polymerase and the therapeutic effects of its inhibitors. Nat Rev Drug Discov. 2005;4:421–440. doi: 10.1038/nrd1718. [DOI] [PubMed] [Google Scholar]
- 22.Pacher P, Obrosova IG, Mabley JG, Szabo C. Role of nitrosative stress and peroxynitrite in the pathogenesis of diabetic complications. Emerging new therapeutical strategies. Curr Med Chem. 2005;12:267–275. doi: 10.2174/0929867053363207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ceriello A, Mercuri F, Quagliaro L, Assaloni R, Motz E, Tonutti L, Taboga C. Detection of nitrotyrosine in the diabetic plasma: evidence of oxidative stress. Diabetologia. 2001;44:834–838. doi: 10.1007/s001250100529. [DOI] [PubMed] [Google Scholar]
- 24.Tannous M, Rabini RA, Vignini A, Moretti N, Fumelli P, Zielinski B, Mazzanti L, Mutus B. Evidence for iNOS-dependent peroxynitrite production in diabetic platelets. Diabetologia. 1999;42:539–544. doi: 10.1007/s001250051192. [DOI] [PubMed] [Google Scholar]
- 25.Pennathur S, Wagner JD, Leeuwenburgh C, Litwak KN, Heinecke JW. A hydroxyl radical-like species oxidizes cynomolgus monkey artery wall proteins in early diabetic vascular disease. J Clin Invest. 2001;107:853–860. doi: 10.1172/JCI11194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ceriello A, Taboga C, Tonutti L, Quagliaro L, Piconi L, Bais B, Da Ros R, Motz E. Evidence for an independent and cumulative effect of postprandial hypertriglyceridemia and hyperglycemia on endothelial dysfunction and oxidative stress generation: effects of short- and long-term simvastatin treatment. Circulation. 2002;106:1211–1218. doi: 10.1161/01.cir.0000027569.76671.a8. [DOI] [PubMed] [Google Scholar]
- 27.Ceriello A, Quagliaro L, Catone B, Pascon R, Piazzola M, Bais B, Marra G, Tonutti L, Taboga C, Motz E. Role of hyperglycemia in nitrotyrosine postprandial generation. Diabetes Care. 2002;25:1439–1443. doi: 10.2337/diacare.25.8.1439. [DOI] [PubMed] [Google Scholar]
- 28.Frustaci A, Kajstura J, Chimenti C, Jakoniuk I, Leri A, Maseri A, Nadal-Ginard B, Anversa P. Myocardial cell death in human diabetes. Circ Res. 2000;87:1123–1132. doi: 10.1161/01.res.87.12.1123. [DOI] [PubMed] [Google Scholar]
- 29.Kajstura J, Fiordaliso F, Andreoli AM, Li B, Chimenti S, Medow MS, Limana F, Nadal-Ginard B, Leri A, Anversa P. IGF-1 overexpression inhibits the development of diabetic cardiomyopathy and angiotensin II-mediated oxidative stress. Diabetes. 2001;50:1414–1424. doi: 10.2337/diabetes.50.6.1414. [DOI] [PubMed] [Google Scholar]
- 30.Ceriello A, Quagliaro L, D’Amico M, Di Filippo C, Marfella R, Nappo F, Berrino L, Rossi F, Giugliano D. Acute hyperglycemia induces nitrotyrosine formation and apoptosis in perfused heart from rat. Diabetes. 2002;51:1076–1082. doi: 10.2337/diabetes.51.4.1076. [DOI] [PubMed] [Google Scholar]
- 31.Mihm MJ, Jing L, Bauer JA. Nitrotyrosine causes selective vascular endothelial dysfunction and DNA damage. J Cardiovasc Pharmacol. 2000;36:182–187. doi: 10.1097/00005344-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Zou MH, Shi C, Cohen RA. High glucose via peroxynitrite causes tyrosine nitration and inactivation of prostacyclin synthase that is associated with thromboxane/prostaglandin H(2) receptor-mediated apoptosis and adhesion molecule expression in cultured human aortic endothelial cells. Diabetes. 2002;51:198–203. doi: 10.2337/diabetes.51.1.198. [DOI] [PubMed] [Google Scholar]
- 33.Pricci F, Leto G, Amadio L, Iacobini C, Cordone S, Catalano S, Zicari A, Sorcini M, Di Mario U, Pugliese G. Oxidative stress in diabetes-induced endothelial dysfunction involvement of nitric oxide and protein kinase C. Free Radic Biol Med. 2003;35:683–694. doi: 10.1016/s0891-5849(03)00401-5. [DOI] [PubMed] [Google Scholar]
- 34.Cai H, Griendling KK, Harrison DG. The vascular NAD(P)H oxidases as therapeutic targets in cardiovascular diseases. Trends Pharmacol Sci. 2003;24:471–478. doi: 10.1016/S0165-6147(03)00233-5. [DOI] [PubMed] [Google Scholar]
- 35.Mihm MJ, Wattanapitayakul SK, Piao SF, Hoyt DG, Bauer JA. Effects of angiotensin II on vascular endothelial cells: formation of receptor-mediated reactive nitrogen species. Biochem Pharmacol. 2003;65:1189–1197. doi: 10.1016/s0006-2952(03)00012-1. [DOI] [PubMed] [Google Scholar]
- 36.Szabó C, Pacher P, Zsengellér Z, Vaslin A, Komjáti K, Benkö R, Mabley JG, Kollai M. Angiotensin II mediated endothelial dysfunction: role of poly(ADP-ribose) polymerase activation. Mol Med. 2004;10:28–35. doi: 10.2119/2004-00001.szabo. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Szabó C, Mabley JG, Moeller SM, Shimanovich R, Pacher P, Virag L, Soriano FG, Van Duzer JH, Williams W, Salzman AL, Groves JT. Pathogenetic role of peroxynitrite in the development of diabetes and diabetic vascular complications: studies with FP15, a novel potent peroxynitrite decomposition catalyst. Mol Med. 2002;8:571–580. [PMC free article] [PubMed] [Google Scholar]
- 38.Sobel BE, Schneider DJ. Cardiovascular complications in diabetes mellitus. Curr Opin Pharmacol. 2005;5:143–148. doi: 10.1016/j.coph.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 39.Cai L, Wang J, Li Y, Sun X, Wang L, Zhou Z, Kang YJ. Inhibition of superoxide generation and associated nitrosative damage is involved in metallothionein prevention of diabetic cardiomyopathy. Diabetes. 2005;54:1829–1837. doi: 10.2337/diabetes.54.6.1829. [DOI] [PubMed] [Google Scholar]
- 40.Esberg LB, Ren J. Role of nitric oxide, tetrahydrobiopterin and peroxynitrite in glucose toxicity-associated contractile dysfunction in ventricular myocytes. Diabetologia. 2003;46:1419–1427. doi: 10.1007/s00125-003-1183-8. [DOI] [PubMed] [Google Scholar]
- 41.Mihm MJ, Coyle CM, Schanbacher BL, Weinstein DM, Bauer JA. Peroxynitrite induced nitration and inactivation of myofibrillar creatine kinase in experimental heart failure. Cardiovasc Res. 2001;49:798–807. doi: 10.1016/s0008-6363(00)00307-2. [DOI] [PubMed] [Google Scholar]
- 42.Pacher P, Liaudet L, Bai P, Mabley JG, Kaminski PM, Virag L, Deb A, Szabo E, Ungvari Z, Wolin MS, Groves JT, Szabo C. Potent metalloporphyrin peroxynitrite decomposition catalyst protects against the development of doxorubicin-induced cardiac dysfunction. Circulation. 2003;107:896–904. doi: 10.1161/01.cir.0000048192.52098.dd. [DOI] [PubMed] [Google Scholar]
- 43.Pacher P, Liaudet L, Mabley J, Komjati K, Szabo C. Pharmacologic inhibition of poly(adenosine diphosphate-ribose) polymerase may represent a novel therapeutic approach in chronic heart failure. J Am Coll Cardiol. 2002;40:1006–1016. doi: 10.1016/s0735-1097(02)02062-4. [DOI] [PubMed] [Google Scholar]
- 44.Turko IV, Marcondes S, Murad F. Diabetes-associated nitration of tyrosine and inactivation of succinyl-CoA:3-oxoacid CoA-transferase. Am J Physiol Heart Circ Physiol. 2001;281:2289–2294. doi: 10.1152/ajpheart.2001.281.6.H2289. [DOI] [PubMed] [Google Scholar]
- 45.El-Remessy AB, Behzadian MA, Abou-Mohamed G, Franklin T, Caldwell RW, Caldwell RB. Experimental diabetes causes breakdown of the blood-retina barrier by a mechanism involving tyrosine nitration and increases in expression of vascular endothelial growth factor and urokinase plasminogen activator receptor. Am J Pathol. 2003;162:1995–2004. doi: 10.1016/S0002-9440(10)64332-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.El-Remessy AB, Abou-Mohamed G, Caldwell RW, Caldwell RB. High glucose-induced tyrosine nitration in endothelial cells: role of eNOS uncoupling and aldose reductase activation. Invest Ophthalmol Vis Sci. 2003;44:3135–3143. doi: 10.1167/iovs.02-1022. [DOI] [PubMed] [Google Scholar]
- 47.Du Y, Smith MA, Miller CM, Kern TS. Diabetes-induced nitrative stress in the retina, and correction by aminoguanidine. J Neurochem. 2002;80:771–779. doi: 10.1046/j.0022-3042.2001.00737.x. [DOI] [PubMed] [Google Scholar]
- 48.Thuraisingham RC, Nott CA, Dodd SM, Yaqoob MM. Increased nitrotyrosine staining in kidneys from patients with diabetic nephropathy. Kidney Int. 2000;57:1968–1972. doi: 10.1046/j.1523-1755.2000.00046.x. [DOI] [PubMed] [Google Scholar]
- 49.Onozato ML, Tojo A, Goto A, Fujita T, Wilcox CS. Oxidative stress and nitric oxide synthase in rat diabetic nephropathy: effects of ACEI and ARB. Kidney Int. 2002;61:186–194. doi: 10.1046/j.1523-1755.2002.00123.x. [DOI] [PubMed] [Google Scholar]
- 50•.Obrosova IG, Mabley JG, Zsengeller Z, Charniauskaya T, Abatan OI, Groves JT, Szabo C. Role for nitrosative stress in diabetic neuropathy: evidence from studies with a peroxynitrite decomposition catalyst. FASEB J. 2005;19:401–403. doi: 10.1096/fj.04-1913fje. This study demonstrates that the pharmacological neutralization of per-oxynitrite is beneficial against diabetic neuropathy. [DOI] [PubMed] [Google Scholar]
- 51.Obrosova IG, Drel VR, Pacher P, Ilnytska O, Wang ZQ, Stevens MJ, Yorek MA. Oxidative-nitrosative stress and poly(ADP-ribose) polymerase (PARP) activation in experimental diabetic neuropathy: the relation is revisited. Diabetes. 2005;54:3435–3441. doi: 10.2337/diabetes.54.12.3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52•.Obrosova IG, Pacher P, Szabo C, Zsengeller Z, Hirooka H, Stevens MJ, Yorek MA. Aldose reductase inhibition counteracts oxidative-nitrosative stress and poly(ADP-ribose) polymerase activation in tissue sites for diabetes complications. Diabetes. 2005;54:234–242. doi: 10.2337/diabetes.54.1.234. This study shows that aldose reductase inhibition counteracts diabetes-induced nitrosative stress and PARP activation in sciatic nerve and retina. [DOI] [PMC free article] [PubMed] [Google Scholar]