The case: A 24-year-old woman presented with a history of multiple medical, surgical and psychiatric issues as well as learning difficulties and mild dysmorphic facial features. During her lifetime, she had seen 12 different specialists and 7 allied health professionals and she had 5 inpatient stays and more than 15 outpatient or day hospital visits.
The patient had a history of asymptomatic mild congenital pulmonary stenosis that required only antibiotic prophylaxis; reflux esophagitis that had been treated with ranitidine followed by omeprazole; constipation; seborrheic scalp treated with ketoconazole; and facial acne. The patient also had bilateral wax build up in her small ear canals that required frequent syringing, dental problems (small teeth, bruxism and multiple caries), obesity since age 19, daytime incontinence since age 21, and hypertension since age 22 treated with hydrochlorothiazide. The patient had a history of multiple episodes of bronchitis (treated with antibiotics, salbutamol and a combination of budesonide and formoterol) that improved with reduced smoking.
At age 15, the patient had a 2-cm subcutaneous lump (found to be a neurilemoma) excised from her left temporal scalp. At age 23, she had a laparoscopic cholecystectomy because of cholelithiasis, and during surgery a hepatic artery anomaly was incidentally noted. At age 24, she had sclerotherapy to treat bilateral varicose veins and a colonoscopy because of mild rectal bleeding, during which a tubular adenoma was identified and removed.
The patient's psychiatric history revealed a diagnosis of attention deficit disorder without hyperactivity at age 16, which had been treated with methylphenidate followed by dextroamphetamine. At age 19, she had depressive symptoms including social isolation and suicidal thoughts, which had been treated with venlafaxine. The patient also had symptoms that suggested psychosis (emotional lability, rambling speech, paranoid thinking), which had been treated with a short course of olanzapine during a 3-week hospital stay at age 21. During a third psychiatric admission, which lasted for 8 months at age 22, she received a diagnosis of schizoaffective disorder because of grossly disorganized behaviour and auditory hallucinations, which had been treated with quetiapine and divalproex. The patient's history also included periodic emotional outbursts and occasional use of alcohol and marijuana from ages 19–22.
The patient had been born weighing 3.2 kg after an uncomplicated pregnancy with an induced vaginal delivery at 41 weeks. During infancy the patient had delays in growth and development. She also had mild hypotonia and some failure to thrive during infancy but these conditions resolved by age 2. She had an in-toeing gait during early childhood because of bilateral, congenital internal femoral torsion that did not require treatment. She had received desmopressin for childhood enuresis and speech therapy for a lisp and stuttering. Audiometry showed normal auditory processing. Beginning in grade 3, the patient had received special education for global deficits, which were most marked in arithmetic. She repeated several grades and graduated from a modified high school program. Clinicians who had been involved in her care had periodically noted mild dysmorphic facies (Figure 1).

Figure 1: Mild dysmorphic facial features of a woman with 22q11.2 deletion syndrome (left, aged 11 years; right, aged 25 years).
The patient's family history showed that 1 relative had mild learning difficulties and that paternal and maternal relatives had mood disorders. There was no family history of psychosis, birth defects, fetal loss or consanguinity.
On examination, the patient was found to have hypertelorism, strabismus, a bulbous nasal tip and small ears (Figure 1). She also had lower left facial hemiparesis, a slightly hypernasal voice and lisp, bilateral cubitus valgus and minor finger and toe abnormalities. She was 164.6 cm tall (55th percentile), weighed 108 kg (body mass index 40) and her head circumference was 58.5 cm (99th percentile). Test results were normal for thyroid stimulating hormone (2.60 [normal 0.4–4.5] mU/L), ionized calcium (1.22 [normal 1.15–1.30] mmol/L) and platelet count (202 [normal 140–400] × 109/L). An abdominal ultrasound did not show renal or splenic anomalies.
The patient's history and the examination findings were consistent with a clinical diagnosis of 22q11.2 deletion syndrome. A molecular cytogenetic test, fluorescence in situ hybridization using a standard 22q11.2 probe (TUPLE1, Vysis), confirmed the diagnosis. The patient and her family received genetic counselling, and they and her clinicians were given available clinical practice guidelines for adults with 22q11.2 deletion syndrome.1
22q11.2 deletion syndrome, previously known as DiGeorge syndrome or velocardiofacial syndrome, is the most common microdeletion syndrome known (estimated prevalence of 1 in 4000 live births), yet it remains underrecognized, especially in adults.1,2 Clinical variability, multisystem disease, subtle features, lack of medical genetics services, the recent availability of molecular cytogenetic testing in 1994 and, most importantly, the unfamiliarity of clinicians with this syndrome all contribute to delayed and missed diagnoses. Clinic visits and admissions to hospital present opportunities to diagnose 22q11.2 deletion syndrome, but without knowledge of this syndrome and its features, patients will not receive the correct diagnosis.
The deletion is hemizygous (affecting only 1 chromosome) and involves the 22q11.2 region of the long arm of chromosome 22. In most newly diagnosed cases (> 90%), and in our case, the parents are unaffected because this is a de novo mutation. Both parents of patients with 22q11.2 deletion syndrome should be tested for the deletion because expression may be mild.1 Fertility is generally unaffected in individuals with 22q11.2 deletion syndrome. Patients with a confirmed diagnosis require genetic counselling about the 50% chance of transmitting the deletion with each pregnancy and about the wide range of congenital and later-onset conditions associated with this syndrome.1 Common later-onset conditions include endocrine disorders, such as hypothyroidism and hypoparathyroidism,1 and schizophrenia or schizoaffective disorder (about 25% of cases).1,2
Diagnosis of 22q11.2 deletion syndrome in infancy is often based on characteristic features, such as major conotruncal cardiac and other birth defects (e.g., velopharyngeal insufficiency, thymic hypoplasia) and neonatal hypocalcemia.3 In the absence of these findings or in cases with a milder presentation, diagnosis in infancy may be missed. Therefore, recognizing this highly variable syndrome, particularly in adolescence and adulthood, requires an enhanced index of suspicion.1,3
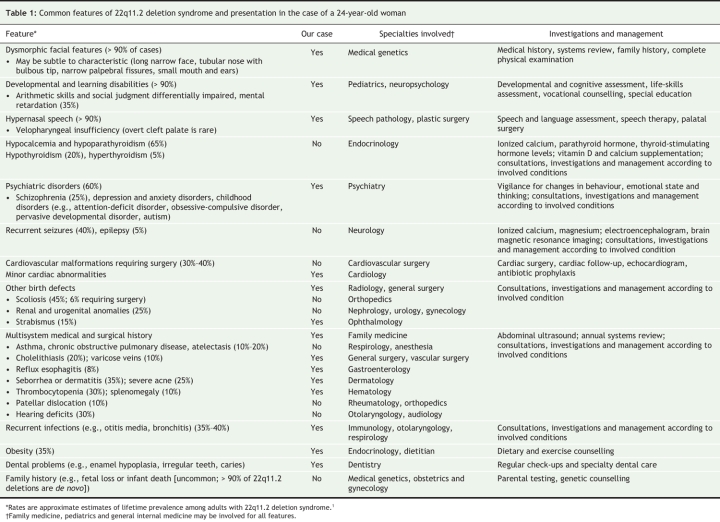
The common manifestations of 22q11.2 deletion syndrome are listed in Table 1. These patients often require multiple outpatient and inpatient visits for associated conditions that involve several medical specialties. There is preliminary evidence of an increasing burden of disease over time, and there may be increased mortality.1 Although learning difficulties are common, less than 40% of patients have mental retardation, and many adults with 22q11.2 deletion syndrome hold full-or part-time jobs.
Table 1
Early diagnosis facilitates anticipatory care. This includes screening for and coordinated management of associated conditions (Table 1), most of which respond to standard treatments.1 Specialty clinics for 22q11.2 deletion syndrome can provide support and up-to-date information for families and professionals. As in the case of our patient, in addition to providing a unifying explanation for a complex history, a diagnosis of 22q11.2 deletion syndrome can relieve parental guilt or blame and can facilitate access to special programs and funding opportunities (e.g., extended dental coverage) and peer-support networks.
Establishing a diagnosis of 22q11.2 deletion syndrome is important for both genetic counselling and long-term management of associated medical, surgical and psychiatric conditions.1,3,4 Clinicians should consider 22q11.2 deletion syndrome in cases of even mild dysmorphic facial features, learning difficulties, hypernasal speech and multisystem medical history, especially in the presence of a psychiatric illness or any congenital anomalies. A consultation with genetics services can provide a clinical diagnosis and clarify if specific genetic testing is warranted.
Ronak K. Kapadia BSc Faculty of Medicine Dalhousie University Halifax, NS Anne S. Bassett MD Clinical Genetics Research Program Centre for Addiction and Mental Health Department of Psychiatry University of Toronto Toronto, Ont.
Acknowledgments
We thank the patient and her family for their participation and insights, and an astute boarding home operator for bringing this case to our attention. We thank Drs. Gary Costain and J. Alfred Morais for reviewing the manuscript.
Footnotes
This article has been peer reviewed.
This research was supported by grants from the Canadian Institutes of Health Research and the National Alliance for Research on Schizophrenia and Depression. Ronak Kapadia is a recipient of a Mach-Gaensslen Foundation of Canada studentship, and Anne Bassett holds the Canada Research Chair in Schizophrenia Genetics.
Competing interests: None declared.
REFERENCES
- 1.Bassett AS, Chow EWC, Husted J, et al. Clinical features of 78 adults with 22q11 deletion syndrome. Am J Med Genet A 2005;138:307-13. [DOI] [PMC free article] [PubMed]
- 2.Bassett AS, Chow EWC. 22q11 deletion syndrome: a genetic subtype of schizophrenia. Biol Psychiatry 1999;46:882-91. [DOI] [PMC free article] [PubMed]
- 3.Oskarsdottir S, Persson C, Eriksson BO, et al. Presenting phenotype in 100 children with the 22q11 deletion syndrome. Eur J Pediatr 2005;164:146-53. [DOI] [PubMed]
- 4.Hay BN. Deletion 22q11: spectrum of associated disorders. Semin Pediatr Neurol 2007;14:136-9. [DOI] [PubMed]