Abstract
To reconstruct highly destructed unstable rheumatoid arthritis (RA) cervical lesions, the authors have been using C1/2 transarticular and cervical pedicle screw fixations. Pedicle screw fixation and C1/2 transarticular screw fixation are biomechanically superior to other fixation techniques for RA patients. However, due to severe spinal deformity and small anatomical size of the vertebra, including the lateral mass and pedicle, in the most RA cervical lesions, these screw fixation procedures are technically demanding and pose the potential risk of neurovascular injuries. The purpose of this study was to evaluate the accuracy and safety of cervical pedicle screw insertion to the deformed, fragile, and small RA spine lesions using computer-assisted image-guidance systems. A frameless, stereotactic image-guidance system that is CT-based, and optoelectronic was used for correct screw placement. A total of 21 patients (16 females, 5 males) with cervical disorders due to RA were surgically treated using the image-guidance system. Postoperative computerized tomography and plane X-ray was used to determine the accuracy of the screw placement. Neural and vascular complications associated with screw insertion and postoperative neural recovery were evaluated. Postoperative radiological evaluations revealed that only 1 (2.1%; C4) of 48 screws inserted into the cervical pedicle had perforated the vertebral artery canal more than 25% (critical breach). However, no neurovascular complications were observed. According to Ranawat’s classification, 9 patients remained the same, and 12 patients showed improvement. Instrumentation failure, loss of reduction, or nonunion was not observed at the final follow-up (average 49.5 months; range 24–96 months). In this study, the authors demonstrated that image-guidance systems could be applied safely to the cervical lesions caused by RA. Image-guidance systems are useful tools in preoperative planning and in transarticular or transpedicular screw placement in the cervical spine of RA patients.
Keywords: Cervical spine, Image guidance, Rheumatoid arthritis, Cervical pedicle screw, Transarticular screw
Introduction
There are various cervical disorders caused by rheumatoid arthritis (RA). The most common disorders include atrantoaxial (C1/2) instability and subluxation in the mid- and lower-cervical spine [6, 21]. These conditions sometimes cause myelopathy, severe pain, or both, either of which impairs the quality of life of RA patients [19]. In such cases, reconstruction surgery may be indicated. Posterior procedures using sublaminar wiring or hook systems have been employed; however, these sometimes result in loss of reduction and/or nonunion [20, 24]. Innovative methods such as C1/2 transarticular and cervical pedicle screw techniques provide greater biomechanical stability compared to conventional posterior fusion techniques [9, 14]. Jones et al. [10] reported that cervical pedicle screws have a significantly higher resistance to pull-out forces than lateral mass screws. However, due to severe spinal deformity and small anatomical size of the vertebra including the lateral mass and pedicle in most of the RA cervical lesions, these screw fixation procedures are technically demanding and pose the potential risk of neurovascular injuries [7, 16, 27]. Frameless stereotactic technology was first designed for intra-cranial surgery for guidance of unseen lesions [8]. Computer-assisted techniques were introduced in spine surgery in the 1990s to improve accuracy and safety of operative procedures [3, 18]. CT-based optoelectronic navigation was originally introduced by Nolte et al. [18]. Amiot et al. [3] later performed this technique in vitro with a magnetic-field based navigator, however this never really gained clinical acceptance. Laine et al. [15] presented evidence for improvement of accuracy under clinical conditions using this technique. In 1996, we started the laboratory testing the clinical application of computer-assisted spine surgery [11, 12]. To improve the accuracy of screw placement, we have adopted an image-guidance system and herein report the usefulness and the limitations of this technique, in the area of surgical reconstruction of RA cervical spine lesions.
Materials and methods
Between January 1998 and January 2004, a total of 21 patients (16 females, 5 males) with cervical disorders due to RA were surgically treated using the image-guidance system. The mean age at the time of surgery was 60.8 years (range 51–78 years). Twelve of the 21 patients displayed typical mutilating-type joint involvements with severe cervical lesion. The cervical disorders were atlanto-axial subluxation (AAS) in six cases, AAS and vertical subluxation of the atlas (VS) in three, subaxial subluxation (SAS) in four and AAS + VS + SAS in eight. According to Ranawat’s classification [19], the neurological deficits were class 2 in five cases, class 3A in seven, and class 3B in nine. The Ranawat’s classification is defined as follows; class 1, no neural deficit; class 2, subjective weakness with hyper-reflexia and dysesthesia; class 3A, objective findings of paresis and long-tract signs, but ambulation possible; class 3B, quadriparesis with resultant inability to walk or to feed oneself.
Occipital or cervical pain was classified into four grades according to Ranawat’s criteria [19]: Grade 0, None; Grade 1, mild, intermittent, requiring only aspirin analgesia; Grade 2, moderate, cervical collar required; Grade 3, severe, pain not relieved by either aspirin or collar. Preoperative pain assessments were Grade 0 in one case, Grade 1 in seven cases, Grade 2 in eleven cases, and Grade 3 in two cases.
Preoperative MR angiography was performed in all patients to evaluate conditions of the bilateral vertebral artery. Patients with 50% stenosis or more were classified as stenosis patients, while those with invisible vertebral artery were classified as occlusion patients. In case of vertebral artery occlusion or stenosis, no pedicle screws were used in the artery-dominant side to avoid vertebrobasilar ischaemia and concurrent stroke if pedicle diameter was narrow.
A frameless stereotactic image-guidance system (Stealth Station and Stealth Station TREONTM; Medtronic, Sofamor Danek, Memphis, TN, USA) was used for correct screw placement and fixation of the cervical spine. The basic data used for navigation were preoperative CT scan imaging data, consisting of consecutive axial slices, 1 mm in thickness of the cervical spine of the RA patients. The data were transferred to the system computer and were reconstructed into two-dimensional (2-D) and three-dimensional (3-D) images on a video monitor. Other mechanical components consisted of a computer workstation, a surgical reference frame, a probe rod to indicate the position in the surgical field, infrared light-emitting diodes (LEDs) that were attached to the probe rod, an electro-optical camera as a position sensor connected to the computer, and a drill guide. Infrared beams were tracked by the electro-optical camera system and the position of the respective LEDs was identified in real time in the surgical field.
Registration was performed in order to accurately match the computer-reconstructed 3-D surgical space with the real surgical space, by identifying four or more points on the vertebrae and the corresponding points of the vertebrae on the 3-D CT image on the monitor (matched-pair point registration). Though more precise matching of the two spaces is usually obtained by repeated registration procedures with 30 or more randomized points indicated by the probe on the surface of the vertebral body (surface registration), this group’s procedure employs only five to six registration points for two consecutive lamina, to shorten the surgical time. More accurate positioning is possible by using the top of the spinous process and bilateral inferior facet caudal tip as points.
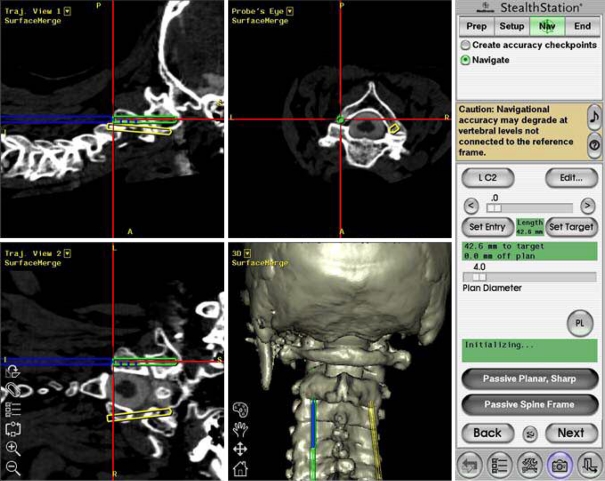
We established a surgical plan a day before surgery and confirmed insertion point of screws, applicability of 3.5 mm screws, point-for-point registration, plus in Magerl’s screw procedure, screw position in relation to vertebral artery. This planning procedure took 20–40 min. Evaluation during the surgical plan for navigation provides further benefit by identifying pedicles with insertion risks and excluding such pedicles from operation (about 10% of all pedicles were excluded). Then, the entrance holes, direction, diameter, and depth of the screws were depicted with a cursor on the monitor, and the surgery was initiated. After exposure of the posterior bony elements of the spine, the reference frame was fixed to the spinous processes and the registration procedures described above were performed. After completion of the registration by matched-pair point and surface registration, the screws were inserted under the guidance of the navigation system. The position of the probe or drill guide was superimposed in real-time on CT images on the monitor, and the screws were introduced into the pedicles at the planned position indicated on the monitor (Fig. 1). The required time between fixation of reference frame to spinous process and insertion of pedicle screw to each segment (1 or 2 vertebrae) was 10–15 min. After all screws were set, the reference frame for registration was removed and additional surgical procedures including decompression or bone graft were followed. If pedicle screw insertion was ineligible, sublaminar cable fixation by SecureStrand was performed.
Fig. 1.
Computer display shown at surgery. The position of the device and surgical plan are shown in four views. The narrow gray arrow indicates the position and direction of the device, and the wide white arrow indicates the planned screw trajectory
The following surgical procedures were performed with the aid of image-guidance systems: C1/2 transarticular screw (Trans Bone Screw; KiscoMedica, St Priest, France) fixation (Magerl’s procedure [17]) in six patients, cervicothoracic fusion using transpedicular screws (Cervical Pedicle Screw System; Depuy Spine, Inc., Raynham, MA) in four patients, occipitocervical or occipitothoracic fusion using the Olerud cervical system (Nord Opedic, Askim, Sweden) in six patients, and RRS Loop Spinal System (Robert Leid, Tokyo, Japan) in five patients (Table 1). All patients had autogenous iliac bone grafts. Patients were permitted to stand and walk from the day after the operation without a collar, since pedicle screw fixation provided enough stability to ambulate without it. Radiological assessment of screw placement was performed using Kast’s criteria [13]. All patients underwent reconstruction CT scans with plain a.p., lateral and oblique X-ray films of instrumented levels after surgery.
Table 1.
Clinical profile and details of surgical procedures
| Case | Age at surgery (years) | Gender | Follow-up (months) | Cervical disorder | Surgical procedure | Extent of fusion | Laminectomy or Laminoplasty | Device |
|---|---|---|---|---|---|---|---|---|
| 1 | 54 | M | 96 | AAS | Magerl & Brooks | C1-2 | C3-7 | TBS |
| 2 | 56 | F | 89 | AAS + VS + SAS | O-T fusion | C0-T2 | C1,C3-5 | Olerud |
| 3 | 63 | F | 74 | AAS + VS + SAS | O-T fusion | C0-T1 | N | Olerud |
| 4 | 63 | F | 72 | AAS + VS + SAS | O-T fusion | C0-T1 | C1,C3-6 | Olerud |
| 5 | 62 | F | 70 | AAS + VS + SAS | O-T fusion | C0-T1 | C1 | Olerud |
| 6 | 72 | M | 66 | AAS + VS + SAS | O-T fusion | C0-T1 | C1,C3-7 | Olerud |
| 7 | 62 | M | 58 | AAS + VS + SAS | O-C fusion | C0-7 | C1 | Olerud |
| 8 | 76 | F | 51 | SAS | C-T fusion | C4-T1 | C5-6 | CPSS |
| 9 | 54 | M | 50 | AAS | Magerl & Brooks | C1-2 | N | TBS |
| 10 | 62 | F | 48 | AAS + VS | O-C fusion | C0-5 | C1 | RRS |
| 11 | 58 | F | 45 | SAS | C-T fusion | C6-T2 | C7-T1 | CPSS |
| 12 | 78 | F | 42 | AAS + VS + SAS | O-T fusion | C0-T1 | C1 | RRS |
| 13 | 67 | F | 40 | AAS | Magerl & Brooks | C1-2 | N | TBS |
| 14 | 54 | F | 39 | AAS + VS | O-C fusion | C0-2 | C1 | RRS |
| 15 | 63 | F | 36 | AAS + VS | O-C fusion | C0-2 | C1 | RRS |
| 16 | 53 | M | 32 | AAS + VS + SAS | O-C fusion | C0-7 | C1, C3-6 | RRS |
| 17 | 54 | F | 29 | SAS | C-T fusion | C5-T1 | C6 | CPSS |
| 18 | 67 | F | 27 | AAS | Magerl & Brooks | C1-2 | C3-6 | TBS |
| 19 | 51 | F | 27 | AAS | Magerl & Brooks | C1-2 | N | TBS |
| 20 | 57 | F | 25 | SAS | C fusion | C3-4 | C3-6 | CPSS |
| 21 | 51 | F | 24 | AAS | Magerl & Brooks | C1-2 | N | TBS |
AAS atlanto-axial subluxation, VS vertical subluxation, SAS subaxial subluxation,
O-C occipitocervical, O-T occipitothoracic, C cervical, N no
TBS trans bone screw, CPSS cervical pedicle screw system, RRS RRS loop spinal system
Clinical results were based on invitations of patients to follow-up. The surgeon performed the follow-up investigation and performed radiographic assessment.
Results
A total of 81 screws, including twelve C1/2 transarticular screws and 69 transpedicular screws (C2; 11 screws, C3; 5, C4; 6, C5; 3, C6; 7, C7; 16, T1; 17, T2; 4), were inserted using image-guidance system. Based on Kast’s criteria [13], correct placement of the 12 transarticular screws and 69 transpedicular screws (48 cervical pedicle screws and 21 thoracic pedicle screws) was assessed.
Correct screw position
Screws either completely within cortical walls of the pedicle or with a maximal cortical perforation of 1 mm as seen on CT. This group comprised 75 (93%) of implanted screws, including transarticular and thoracic pedicle screws.
Minor breach
Lateral or ventral perforation of the vertebral body (2 screws; T1, T2), slight affection of the lateral recess without dural contact (1 screw: C5) or narrowing of the vertebral artery canal less than 25% of its diameter (2 screws; C4, C6). In summary, 5 screws (6% of all screws) showed a minor breach radiologically.
Major breach
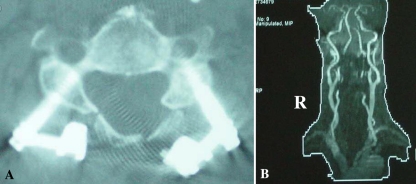
Encroachment of the vertebral artery canal of more than 25% (1 screw: C4, case 6) or caudal perforation of the pedicle with potential nerve root compression or injury (0 screws) were observed. Further, major breaches like medial pedicle perforation with dural laceration and risk of radicular or medullar compression or injury were not observed in this series. The group of major breaches comprised only one (1.2%) of implanted screws (81 screws) or one (2.1%) of all implanted cervical pedicle screws (48 screws), without injury to the vertebral artery. Although the authors had confirmed no pedicle wall perforation during the probing procedure, CT evaluation showed lateral pedicle wall perforation (major breach) in one screw (C4 pedicle screw) (Fig. 2). This perforation may have been caused during reduction and/or screw-rod connecting maneuvers in which unexpected excessive load had acted on the screw. Postoperative MR angiography revealed no vertebral artery occlusion (Fig. 2).
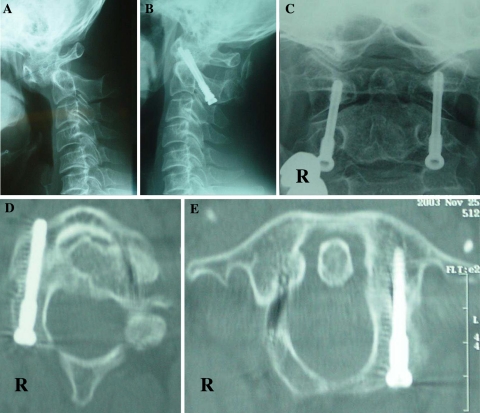
Fig. 2.
a Patient (case 6) with screw displacement C4 with narrowing of the vertebral channel more than 25% (left screw); major breach. b Postoperative MR angiography revealed no vertebral artery occlusion
Preoperative vertebral artery evaluation by MR angiography showed four (19%; three cases with AAS + VS + SAS and one case with AAS + VS) unilateral stenosis and one (4.8%; AAS + VS + SAS) unilateral occlusion. Average operative time was 275 min (range 148–505 min) and the average intraoperative blood loss was 380 ml (range 20–630 ml). According to Ranawat’s classification, 9 patients remained the same (2→2; 4 patients, 3A→3A; 3, 3B→3B; 2) and 12 patients showed improvement (2→1; 1 patient, 3A→2; 4, 3B→3A; 7) (Table 2). Seven of the 9 patients who could not walk (3B) before surgery could walk (3A) post surgery. All patients maintained the improved ADL level throughout the postoperative course. In 18 of the 21 cases (86%), occipital or neck pain as classified by Ranawat’s criteria for pain had improved.
Table 2.
The neurological deficit class before surgery and at the final assessment
| Preoperative neurological deficit class | Follow-up neurological deficit class | |||
|---|---|---|---|---|
| 3B | 3A | 2 | 1 | |
| 3B | 2 | 7 | ||
| 3A | 3 | 4 | ||
| 2 | 4 | 1 | ||
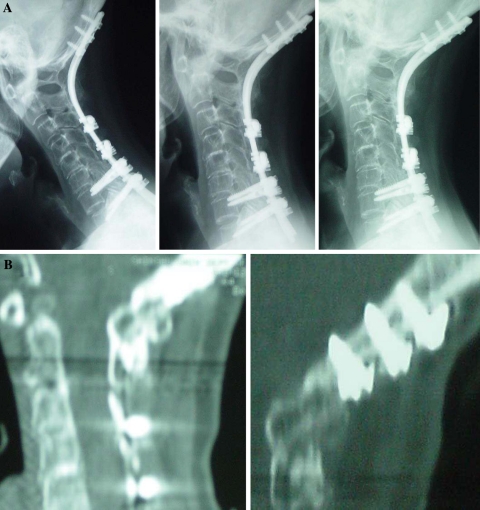
No instrumentation failure, loss of reduction, or nonunion had occurred at the final follow-up (average 49.5 months; range 24–96 months). Bony fusion was defined as an absence of segmental motion in functional lateral X-rays with presence of solid bony union observed in reconstruction CT (Fig. 3, case 5). Solid union was achieved in all 21 patients.
Fig. 3.
a Dynamic lateral view X-ray images of a 63-year-old female (case 5) indicates osseous integration, 2 years postoperative. b Reconstruction CT indicates bony fusion, 2 years postoperative
Case presentations
Two typical cases with extremely narrow pedicles are shown. With conventional transarticular or transpedicle screw insertion techniques, iatrogenic neurovascular injuries due to malposition of the screws may have resulted.
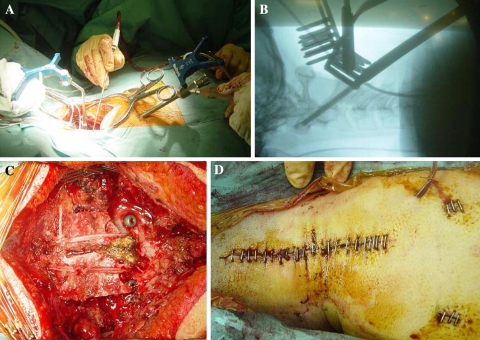
Case 9
This patient was a 54-year-old man with AAS. Transarticular screw fixation (Trans Bone Screw; KiscoMedica, France) was inserted using the navigation system and image intensifier, lateral view. Posterior bone graft was performed with Brooks’ method using SecureStrand sublaminar cables (Pioneer Surgical Technology, Marquette, MI) (Fig. 4). After 50 months post-surgery, the patient showed improvement from 2 (preoperatively) to 1 according to Ranawat’s classification, and occipital pain was reduced (2→1) (Fig. 5).
Fig. 4.
a Case 9: a 54-year-old man during atlanto-axial fixation. The reference frame is placed on the C2 spinous process and a navigatable guide is inserted, in an incision separate from that of the reference frame. b Lateral view from image intensifier during surgery. c Magerl’s and Brooks’ procedures were performed using SecureStrand sublaminar cables. d Main skin incision and two small incisions
Fig. 5.
a Preoperative flexion lateral X-ray in case 9 indicates atlanto-axial subluxation. b Postoperative lateral X-ray. c Postoperative antero-posterior X-ray. d & e Postoperative reconstructive CT shows transarticular screws correctly passing through the pedicle of C2 and C1/2 joints
Case 10
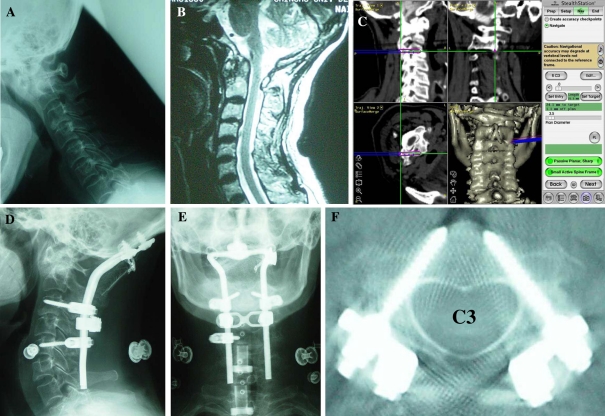
This patient was a 62-year-old woman with non-reducible AAS and VS. In preoperative planning, the authors judged that it was not possible to insert the pedicle screw into the C2, C4, and, C5 (hemilateral) pedicles. The following procedures were performed using the navigation system: C1 laminectomy, insertion of bilateral C3 and hemi lateral C5 pedicle screw (RRS Loop Spinal System; Robert Leid, Tokyo, Japan), sublaminar cable fixation from C2 to C5 (using SecureStrand sublaminar cables), and insertion of occipital screw. Posterior bone graft from C0 to C5 was performed after instrumentation. Neurological deficits and occipital pain had resolved, and surgery enabled the patient to walk again. The postoperative CT scan (C3 level) shows accurate placement of the pedicle screws, which were inserted into extremely narrow pedicles (Fig. 6). After 48 months post-surgery, the patients showed improvement from 3B (preoperatively) to 3A according to Ranawat’s classification.
Fig. 6.
a Preoperative flexion lateral X-ray in a 62-year-old female (case 10) indicates atlanto-axial subluxation and vertical subluxation. b Preoperative sagittal T2-WI MRI shows cord compression due to C1 laminae. c Computer display shown at surgery. d, e Postoperative X-ray. f Postoperative CT scan (C3 level) shows pedicle screw was inserted accurately
Discussion
Cervical reconstruction surgery should be considered to maintain the quality of life and daily activities in RA patients with severe cervical involvements. A recent study indicated that the natural course of RA patients with myelopathy managed by conservative treatments is poor [25]. In their study, all patients did not recover and were bedridden. Furthermore, all patients had died within 3 years [25]. Casey [5] reported that no benefit was obtained except pain relief by surgical treatment of patients of Ranawat’s class 3B. In contrast, the current study showed the potential importance of surgery for class 3B patients, which provided excellent clinical results.
One of the main goals of cervical reconstruction surgery in RA patients is to eliminate instability by achieving immediate and long-term stability. Pedicle screw fixation and C1/2 transarticular screw fixation are biomechanically superior to other conventional procedures using wiring or clamping [1, 9, 14, 17]. Furthermore, pedicle screw fixation is a useful technique because laminectomy or laminoplasty can be performed simultaneously.
Conventional screw insertion techniques for both C1/2 screw and pedicle screw placement in the subaxial cervical spine rely on anatomical landmarks and intraoperative fluoroscopy. However, in RA patients, several specific illness-related problems of the cervical spine make surgical treatment extremely difficult. The use of corticosteroid medication for several years and immobilization of the spine caused by multiple musculoskeletal deformities and dysfunctions lead to considerable osteoporosis. Moreover, due to erosion of the anatomical structures, bony landmarks are not always reliable. Especially when the vertebral artery runs an abnormal course, screw placement has a potential risk of neurovascular injury, and vertebral artery injury on the dominant side can cause cerebellar infarction and possibly fetal sequelae [2, 22, 23]. Moreover, due to severe spinal deformity and small anatomical size of the vertebra (the lateral mass and pedicle) in the most RA cervical lesions, screw placement procedures are highly technically demanding and pose the potential risk of neurovascular injuries even though intraoperative fluoroscopy is used. The current study clearly shows from clinical results that computer-assisted screw insertion in the rheumatoid cervical spine enables a significant reduction in the screw malplacement rates (1/48; 2.1%) as compared to conventional insertion techniques, using image intensifier (5.3%; Abumi K et al. [1]). There are currently no published reports on perforation rates with cervical pedicle screws in rheumatoid cervical spine lesions. All procedures performed at this facility were performed using a navigation system, therefore no control data is available. Borm et al. [4] reported that transarticular C1–C2 screw fixation was performed in 14 cases using computer navigation (STN 4.0; Zeiss Company, Oberkochen Germany). In this study, there was one medial perforation of a C2 pedicle wall and one malposition of the screw in C2 without reaching the lateral mass of C1 (2/28; 7.1%). In contrast, there were no malpositions of the transarticular 4 screw fixation among our cases. Regarding C1-2 transarticular screw fixation, it is very easy to navigate at C2 levels using image-guidance systems. However, C1 is easily moved in the prone position even if a Halo-vest apparatus is adapted for patients with atlantoaxial subluxation. In such a case, it is difficult to navigate the screw in the lateral mass of the atlas, and a two-dimensional image intensifier during surgery should be employed. However, this type of image intensifier was not used in pedicle screw insertion in this study. When pedicle perforation was suspected, it was investigated on X-ray image using a marker. Importantly, although the risk of screw perforation can be reduced using a navigation system, its incidence does not disappear completely. Due to the fragile bone quality of the RA cervical spine, care must be taken during rod or plate application procedures and reduction maneuvers which may cause cut-out and displacement of the screw from its original position. To prevent these injuries, preoperative evaluation of the vertebral artery and planning of screw insertion are indispensable. Generally, insertion of screws into the pedicle of less than 3.5 mm in diameter should be avoided even with navigation assistance.
Preoperative vertebral artery evaluation by MR angiography revealed unilateral stenosis or occlusion in 23.8% of patients, all of whom were complicated with VS. Abnormality of vertebral artery is highly likely in RA patients because of cervical deformity. Tumialan et al. [26] reported cerebral and cerebellar infarction in rheumatoid cervical spine patients caused by vertebral artery injury, observed during anterior corpectomy. In consideration of that report, in case of vertebral artery occlusion or stenosis, no pedicle screws were used on the artery-dominant side to avoid vertebrobasilar ischaemia and concurrent stroke if pedicle diameter was narrow. This approach shows significant benefits of preoperative planning using the navigation system.
The accuracy of a computer-assisted image-guidance system for correct pedicle screw fixation of the cervical spine has been confirmed in laboratory tests [12], but its clinical results in RA patients have not been clarified. Although the current study was not large in number of patients, the results of surgery under the image-guidance system were encouraging. Use of this system in cervical instrumentation surgery for RA patients can aid in reducing the risk of screw misplacement.
Conclusion
In this study, the authors demonstrated that image-guidance systems can be applied safely to the cervical lesions caused by RA. Image-guidance systems are useful tools in preoperative planning and in transpedicular screw placement in the cervical spine of RA patients. However, incidence of screw perforation does not disappear completely. Due to the fragile bone quality of RA cervical spine, care must be taken during rod or plate application procedures and reduction maneuvers.
Contributor Information
Jun Takahashi, Phone: +81-263-372659, FAX: +81-263-358844, Email: jtaka@hsp.md.shinshu-u.ac.jp.
Yasuhiro Shono, Phone: +81-11-8315151, FAX: +81-11-8313851.
Mikio Kamimura, Phone: +81-263-857300, FAX: +81-263-857350.
Sohei Ebara, Phone: +81-467-851122, FAX: +81-467-839798.
References
- 1.Abumi K, Kaneda K, Shono Y, Fujiya M. One-stage posterior decompression and reconstruction of the cervical spine by using pedicle screw fixation systems. J Neurosurg (Spine 1) 1999;90:19–26. doi: 10.3171/spi.1999.90.1.0019. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Amiot LP, Labelle H, DeGuise JA, Sati M, Brodeur P, Rivard CH. Computer-assist pedicle screw fixation. A feasibility study. Spine. 1995;20:1208–1212. doi: 10.1097/00007632-199505150-00019. [DOI] [PubMed] [Google Scholar]
- 4.Borm W, Konig RW, Albrecht A, Richter HP, Kast E. Percutaneous transarticular atlantaxial screw fixation using a cannulated screw system and image guidance. Minim Invasive Neurosurg. 2004;47:111–114. doi: 10.1055/s-2004-818449. [DOI] [PubMed] [Google Scholar]
- 5.Casey ATH, Crockard HA, Bland JM, Stevens J, Moskovich R, Ransford AO. Surgery on the rheumatoid cervical spine for the non-ambulant myelopathic patients-too much, too late? Lancet. 1996;347:1004–1007. doi: 10.1016/S0140-6736(96)90146-4. [DOI] [PubMed] [Google Scholar]
- 6.Clark CR. Rheumatoid involvement of the cervical spine. An overview. Spine. 1994;19:2257–2258. doi: 10.1097/00007632-199410150-00002. [DOI] [PubMed] [Google Scholar]
- 7.Fuji T, Oda T, Kato Y, Fujita S, Tanaka M. Accuracy of atlantoaxial transarticular screw insertion. Spine. 2000;25:1760–1764. doi: 10.1097/00007632-200007150-00004. [DOI] [PubMed] [Google Scholar]
- 8.Golfinos JG, Fitzpatrick BC, Smith LR, Spetzler RF. Clinical use of a flameless stereotactic arm: results of 325 cases. J Neurosurg. 1995;83:197–205. doi: 10.3171/jns.1995.83.2.0197. [DOI] [PubMed] [Google Scholar]
- 9.Grob D, Crisco JJ, 3rd, Panjabi MM, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atrantoaxial fixation techniques. Spine. 1992;17:480–490. doi: 10.1097/00007632-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 11.Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K. Accurate pedicle screw insertion under control using a computer-assisted image guiding system: laboratory test and clinical study. J Orthop Sci. 1999;4:197–206. doi: 10.1007/s007760050094. [DOI] [PubMed] [Google Scholar]
- 12.Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K. Safe and accurate cervical pedicle screw insertion guided by a computer assisted image-guidance system. J Spinal Disord. 2000;13:218–225. doi: 10.1097/00002517-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Kast E, Mohr K, Richter HP, Borm W. Complication of transpedicular screw fixation in the cervical spine. Eur Spine J. 2006;15:327–334. doi: 10.1007/s00586-004-0861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems: an assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;17:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 15.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomized controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:234–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atrantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 17.Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine I. Berlin Heidelberg New York: Springer; 1987. pp. 322–327. [Google Scholar]
- 18.Nolte LP, Zamorano LJ, Jiang Z, Wang Q, Langlotz F, Berlemann U. Image-guided insertion of transpedicular screws. A laboratory set-up. Spine. 1995;20:497–500. doi: 10.1097/00007632-199502001-00016. [DOI] [PubMed] [Google Scholar]
- 19.Ranawat CS, O’Leary P, Pellici P. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg. 1979;61A:1003–1010. [PubMed] [Google Scholar]
- 20.Santavirta S, Konttinen Y, Laasonen E, Honkanen V, Antti-Poika I, Kauppi M. Ten-year results of operations for rheumatoid cervical spine disorders. J Bone Joint Surg. 1991;73B:116–120. doi: 10.1302/0301-620X.73B1.1991743. [DOI] [PubMed] [Google Scholar]
- 21.Sharp J, Purser DW, Lawrence JS. Rheumatoid arthritis of the cervical spine in the adult. Ann Rheum Dis. 1958;17:303–313. doi: 10.1136/ard.17.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shintani A, Zervas NT. Consequence of ligation of the vertebral artery. J Neurosurg. 1972;36:447–450. doi: 10.3171/jns.1972.36.4.0447. [DOI] [PubMed] [Google Scholar]
- 23.Smith MD, Emery SE, Dudley A, Murray KJ, Leventhal M. Vertebral artery injury during anterior decompression of the cervical spine. A retrospective review of ten patients. J Bone Joint Surg. 1993;75B:410–415. doi: 10.1302/0301-620X.75B3.8496209. [DOI] [PubMed] [Google Scholar]
- 24.Sumi M, Kataoka O, Ikeda M, Sawamura S, Uno K, Siba R. Atlantoaxial dislocation: a follow-up study of surgical results. Spine. 1997;22:759–764. doi: 10.1097/00007632-199704010-00009. [DOI] [PubMed] [Google Scholar]
- 25.Sunahara N, Matsunaga S, Mori T, Ijiri K, Sakou T. Clinical course of conservatively managed rheumatoid arthritis patients with myelopathy. Spine. 1997;22:2603–2608. doi: 10.1097/00007632-199711150-00004. [DOI] [PubMed] [Google Scholar]
- 26.Tumialan LM, Wippold FJ, 2nd, Morgan RA. Tortuous vertebral artery injury complicating anterior cervical spinal fusion in a symptomatic rheumatoid cervical spine. Spine. 2004;29:E343–E348. doi: 10.1097/01.BRS.0000134593.98662.D0. [DOI] [PubMed] [Google Scholar]
- 27.Wright NM, Lauryssen C. Vertebral artery injury in C1–2 transarticular screw fixation: results of a survey of the AANS/CNS Association of Neurological Surgeon/Congress of Neurological Surgeons. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]