Abstract
While there is consensus in the literature that blood vessels are confined to the outer anulus fibrosus of normal adult intervertebral disc, debate continues whether there is a vascular in-growths into inner parts of the intervertebral disc during degeneration. We therefore tested the hypothesis that vascular in-growth is not a distinct feature of disc degeneration. The specific endothelial cell marker CD 31 (PECAM) was used to immunohistochemically investigate 42 paraffin-embedded complete mid-sagittal human intervertebral disc sections of various ages (0–86 years) and varying extent of histomorphological degeneration. Additionally, 20 surgical disc samples from individuals (26–69 years) were included in this study. In discs of fetal to infantile age, blood vessels perforated the cartilaginous end plate and extended into the inner and outer anulus fibrosus, but not into the nucleus pulposus. In adolescents and adults, no blood vessels were seen except for the outer zone of the anulus fibrosus adjacent to the insertion to ligaments. The cartilaginous end plate remained free of vessels, except for areas with circumscribed destruction of the end plate. In advanced disc degeneration, no vessels were observed except for those few cases with complete, scar-like disc destruction. However, some rim lesions and occasionally major clefts were surrounded by a small network of capillary blood vessels extending into deeper zones of the anulus fibrosus. A subsequent morphometric analysis, revealed slightly “deeper” blood vessel extension in juvenile/adolescent discs when compared to young, mature and senile adult individuals with significantly “deeper” extension in the posterior than anterior anulus. The analysis of the surgical specimens showed that only sparse capillary blood vessels which did not extend into the nucleus pulposus even in major disc disruption. Our results show that vascular invasion deeper than the periphery was not observed during disc degeneration, which supports the hypothesis that vascular in-growth is not a distinct feature of disc degeneration.
Keywords: Age-related disc degeneration, Intervertebral disc, Blood supply, Lumbar region, Immunohistochemistry
Introduction
The adult intervertebral disc is the largest avascular structure of the human body resulting in long diffusion distances for the nutritional supply of disc cells. This significantly reduces the cellular capacity to survive under critical nutritional/metabolic conditions and may also explain the low potential of disc tissues to restore its structure and function during aging. The poor nutritional situation of disc cells particularly those in the nucleus pulposus has been assumed to play a pivotal role in disc degeneration [10]. Locally synthesized mediators, e.g., pro-inflammatory cytokines would consequently need long diffusion ways in order to reach the peripheral neural innervation of the anulus fibrosus or the systemic blood flow. Recently, it has been hypothesized that there is a relationship between neo-vascularization and innervation of the usually avascular and aneural intervertebral disc at the sites of discogenic back pain [7]. While there is consensus in the literature that blood vessels are confined to the outer anulus fibrosus of normal adult intervertebral disc, debate continues whether there is a vascular in-growths into inner parts of the intervertebral disc during degeneration [4, 7, 8, 11, 12, 15, 16]. So far, neo-vascularization has predominantly been studied using surgical disc specimens (i.e., mostly herniated disc material) [4, 11, 15, 19, 20, 23]. However, a precise spatial exploration of vascular in-growth into the disc during disc degeneration is difficult to perform in surgical specimens. In a histologic study investigating complete sagittal sections of lumbar motion segments, Boos et al. found that blood vessels regress from the intervertebral disc during growth and can only be found in the outer anulus fibrosus of normal adult discs [3]. No neo-vascularization of the inner parts of the intervertebral discs was observed during disc degeneration [3]. Since these observations were only based on histological findings, a reliable exclusion of disc neo-vascularization was not possible.
The objective therefore was to perform an immunohistochemical study using the specific endothelial cell marker CD 31 (PECAM) [1, 18] to investigate the temporo-spatial distribution of blood vessels during growth and degeneration on autopsy as well as surgical specimens. The rationale for the use of sagittal sections of complete lumbar motion segments was to allow for a precise spatial allocation of disc vascularization. Surgical specimens were included with the rationale to explore disc specimens from patients undergoing surgery for putative discogenic back pain and disc herniation. With this approach, we hypothesized that vascular invasion deeper than the disc periphery does not occur during disc degeneration and that neo-vascularization is not a distinct feature of disc degeneration.
Material and methods
Study population
Autopsy group
A total of 42 complete mid-sagittal intervertebral disc specimens including the adjacent cartilaginous end plates were investigated in this study. The age of the specimens ranges from 35 weeks of gestation to 86 years: eight fetal/infantile (27 weeks to 2 years), eight juvenile (2–10 years), six adolescent (13–21 years), six young adults (22–25 years), six adults (31–47 years), and eight senile specimens (58–85 years). The specimen were obtained from 19 female and 23 male individuals. The disc levels investigated covered all lumbar discs with the following distribution: L1/2 (n = 8), L2/3 (n = 9), L3/4 (n = 9), L4/5 (n = 8), and L5/S1 (n = 8). All individuals had died of an acute death. The clinical notes available at autopsy did not reveal a chronic back problem in any of the individuals investigated.
Surgical group
In addition to the autopsy samples, we used a series of surgical tissue samples obtained from 20 individuals undergoing spinal surgery for disc degeneration, protrusion and disc extrusion. The distribution of the disc levels was as follows: T11/12 (n = 1), T12/L1 (n = 3), L1/2 (n = 3), L2/3 (n = 2), L4/5 (n = 3), and L5/S1 (n = 8). Clinical data on low back pain history, related disability and imaging findings (radiographs, magnetic resonance images) were available for all cases.
Tissue processing
During routine autopsy, the lumbar spines were exposed by an anterior approach and osteotomized at each pedicle level (L1 to S1) to obtain the anterior column with the anterior and posterior longitudinal ligament remaining intact without mutilation of the cadaver. The specimens were frozen at −20°C and then cut into motion segments with a band saw. A 5 mm mid-sagittal slice of each motion segment (intervertebral disc with adjacent vertebral bodies) was obtained. Fetal and infantile spine were cut in half and processed in total. The surgical material was particularly selected to provide a cake-piece-like shape with orientation of the anulus fibrosus and nucleus pulposus (anterior spinal fusion operations). In the case of disc herniations, disc samples (protrusions and extrusions) were harvested including the posterior anulus in the area of the herniation. In cases of a sequester, the complete fragment was processed.
Subsequently, all slices were fixed in 4% buffered formaldehyde for 24 h and decalcified (autopsy group) in 0.1 M EDTA (pH 7.2) and embedded into paraffin wax. From the resulting tissue blocks, serial paraffin sections (2–4 μm) were cut and placed on glass slides for routine stainings (hematoxylin-eosin (HE), Masson-Goldner (MG), alcian blue stain with periodic acid-Schiff (Alc-PAS) and immunohistochemistry as previously described [2, 3, 14].
Determination of histological tissue degeneration
In order to correlate the immunohistochemical findings with the histologic degree of age-related disc degeneration the routine histologic staining results were used to calculate the histological degeneration score (HDS) as described previously in detail [3]. Briefly, the extent of chondrocyte clustering, cleft and tear formation, granular matrix changes and mucoid tissue transformation were evaluated and ranked according to the evaluation protocol [3]. The resulting values were used for correlation with the penetration depths of blood vessels.
Immunohistochemistry
Randomly selected tissue sections were deparaffinized and subsequently enzymatically pre-treated to enhance immunoreactivity. All immunostainings were performed as previously described in detail [2, 13, 14]. Briefly, the appropriate sections were pre-treated with 0.2% pepsin (Sigma Chem., Deisenhofen, Germany) and subsequently incubated with the specific monoclonal primary antibody directed against CD 31 (DAKO, Hamburg, Germany). After several washings, the antigen-antibody complex was visualized by a biotinylated secondary antibody and a streptavidin-enzyme conjugate (LSAB-technique) with diaminobenzidine (Biogenex/DCS, Heidelberg, Germany) as chromogene. All sections were then evaluated under light microscopy.
Data collection and qualitative analysis
The presence of CD31 positive endothelial cells outlining blood vessels of different size was analyzed with regard to the histoanatomic location within the disc (i.e., nucleus pulposus, anterior, and posterior anulus fibrosus as well as upper and lower end plates, respectively). Therefore, the presence/absence of blood vessels was recorded on a qualitative level. The assessments were done independently by three investigators (AN, RS, NB) which all possess extensive experience in histologic examinations of the disc and minor disagreement was resolved in conference.
Quantitative morphometric analysis of blood vessel “extension” into the outer anulus fibrosus
In order to evaluate the extension of blood vessels into the outer anulus fibrosus, we performed a morphometric analysis on the autopsy series. This was done separately for the anterior and posterior anulus fibrosus and the upper and lower end plate. Since the individual dimensions of the discs were considerably different due to age, gender, body size, and potential concomitant disc alterations, we did not use a metric distance from the insertion zone to the deepest detectable blood vessel, but decided to count the number of distinct collagen lamellae. Interestingly, the number of clearly identifiable collagen lamellae of the outer anulus fibrosus was only slightly different between individuals of various age, gender and body size. Thereby, the most inner collagen lamellae penetrated by blood vessel was assessed and used for further calculations. The correlation between age/degeneration (HDS) and penetration depth was explored using a Spearman rank correlation test. Differences with regard to vascular penetration between anterior and posterio anulus was investigated by a Wilcoxon signed rank test. The level of significance was set at 0.05, two-tailed.
Results
Control experiments
In order to ensure the specificity of the immunoreaction, we used in each batch normal serum instead of the primary antibody. All control experiments provided negative results. In parallel, in all sections a positive staining of regular blood vessels of the peridiscal connective tissue (e.g., in the longitudinal ligaments) or within the adjacent bone marrow served as internal positive staining control.
Qualitative observations in the autopsy group
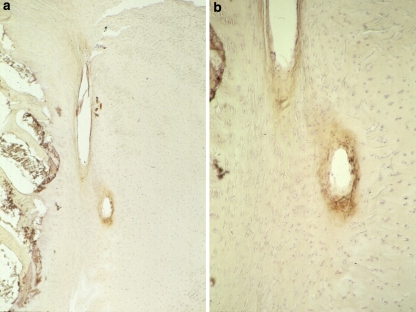
Blood vessels in fetal and infantile discs
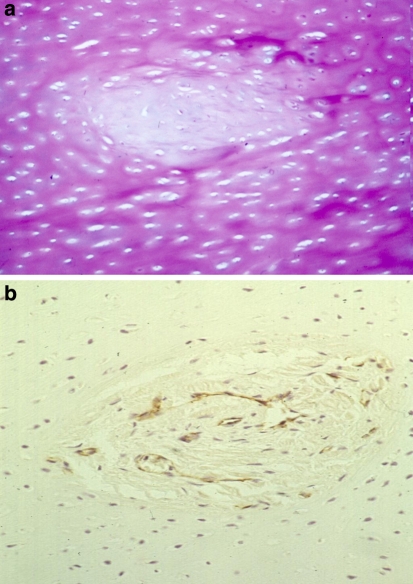
In discs of fetal and infantile age (Tables 1, 2), we observed several blood vessels perforating the cartilaginous end plate and extending into the anulus fibrosus (Fig. 1a, b). This was seen both adjacent to the inner and outer anulus fibrosus, the latter providing a layer of cartilage which corresponds to the growth zone of the future growth plate and which lines the outer anulus to the vertebral bone. The nucleus pulposus remained free of vascular structures (Fig. 2). Additionally, small blood vessels of capillary size were seen in the transition zone of the ligamentous insertion and the outer anulus fibrosus. However, there seemed to be no connection between those small-sized vessels of the outer anulus fibrosus and those extending through the end plate into the inner part of the anulus fibrosus. In fantile discs, we observed focal obliteration of vascular channels as a possible first sign of vascular regression (Fig. 2a, b)
Table 1.
Qualitative temporo-spatial distribution of blood vessels within intervertebral disc
| Age | Number of specimens | Nucleus pulposus | Inner anulus fibrosus | Outer anulus fibrosus | Transitional zone/Lig. |
|---|---|---|---|---|---|
| Fetal/infantile | 8 | 0 | 5/8 | 8/8 | 8/8 |
| Juvenile | 8 | 0 | 0 | 0 | 8/8 |
| Adolescent | 6 | 0 | 0 | 0 | 8/6 |
| Young adult | 6 | 0 | 0 | 0 | 2/6 |
| Adult | 6 | 0 | 0 | 4/6a | 4/6a |
| Senile | 8 | 0 | 0 | 2/8a | 2/8a |
aWithin tissue defects and granulation tissue
Table 2.
Qualitative temporo-spatial distribution of blood vessels in the cartilaginous end plate (upper and lower end plate analyzed separately per disc)
| Age | Number of specimens (upper and lower EP) | Anterior endplate | Central endplate | Posterior endplate |
|---|---|---|---|---|
| Fetal/infantile | 16 | 12/16 | 4/16 | 10/16 |
| Juvenile | 16 | 0 | 0 | 0 |
| Adolescent | 12 | 0 | 0 | 0 |
| Young adult | 12 | 2/12a | 0 | 2/12a |
| Adult | 12 | 6/12a | 4/12a | 4/12a |
| Senile | 16 | 6/16a | 4/16a | 8/16a |
aWith tissue defects and granulation tissue
Fig. 1.
Vascular supply in postnatal intervertebral discs intervertebral disc using the vascular cell marker CD-31. The disc is invaded by large, often ectatic and thin-walled blood vessels that seem to form large vascular arcades within the disc cartilage. Vergrößerung: Original magnification a ×100; b ×250
Fig. 2.
Infantile intervertebral discs (2 years) reveal a focal obliteration of vascular channels (a H&E, b CD31 staining). The previous vascular channels seem to show some fibrosis, possibly the very first signs of vascular regression (b). Original magnification a ×250; b ×250
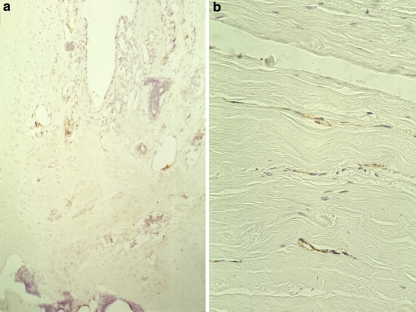
Blood vessels in juvenile, adolescent, and adult discs
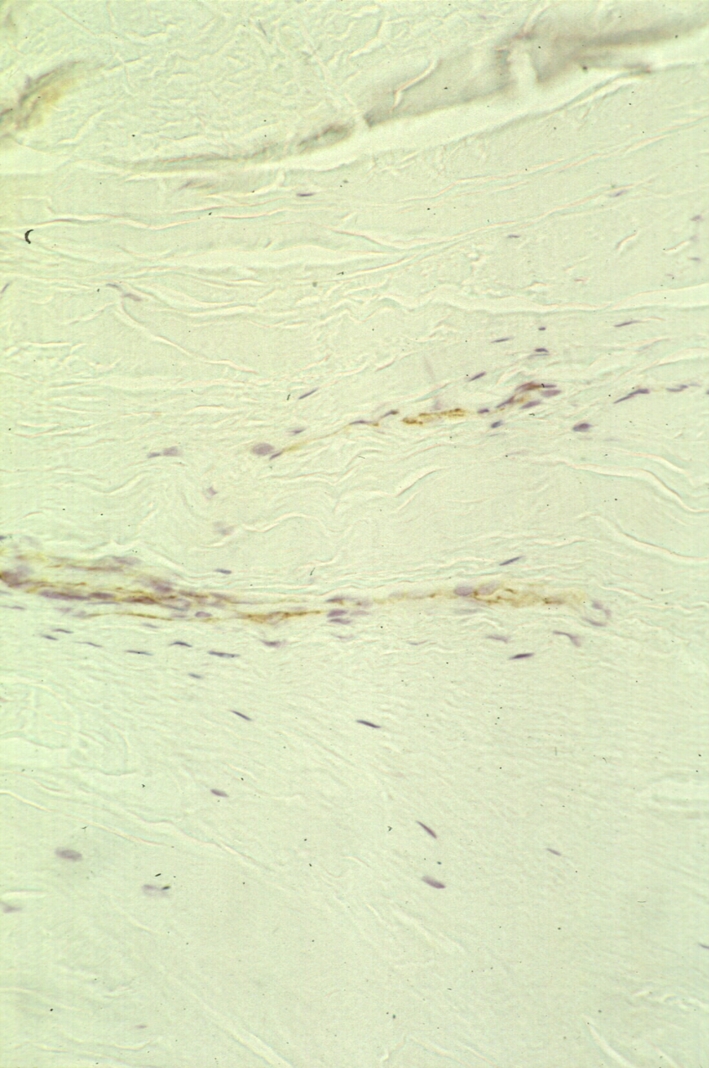
In older individuals, no blood vessels were seen in normal disc tissues, except for the outer zone of the anulus fibrosus adjacent to the insertion to ligaments (Figs. 3, 4). Here, small capillary blood vessels were seen together with some larger, distended venous vessels. The cartilaginous end plate was also free of blood vessels, while the bone end plate (which is part of the vertebral bone) contains extensive blood spaces of the vertebral blood sinuses. However, in discs of somewhat older individuals, small blood vessels extend deeper into the outer anulus as in younger individuals (Fig. 5). In areas with circumscribed destruction of the end plate, a focal blood vessel invasion was seen also into the cartilaginous end plate. In degenerated nuclear disc tissue, no vessels were observed except for those few cases with complete, scar-like destruction of the disc. However, in anulus fibrosus tissue, some rim lesions and occasionally major clefts were surrounded by a small network of capillary blood vessels extending into deeper zones of the anulus fibrosus (Fig. 6a). Small vascular invasion was also observed in the outer anulus fibrosus (Fig. 6b).
Fig. 3.

Adolescent intervertebral discs (16 years) are free of blood vessels (staining with CD31). There are only some vessels in the outer AF close to the ligaments. Original magnification: ×400
Fig. 4.
Young adult intervertebral discs (25 years) are also free of vessels (staining for CD31). There are some vascular arcades at the interface between the outer anulus fibrosus and the ligaments (arrow). Original magnification: ×400
Fig. 5.
Discs of older individuals (37 years) without major degeneration reveal some small blood vessels in the OAF, that extend significantly deeper into this zone as in the young adult group. Original magnification: ×400
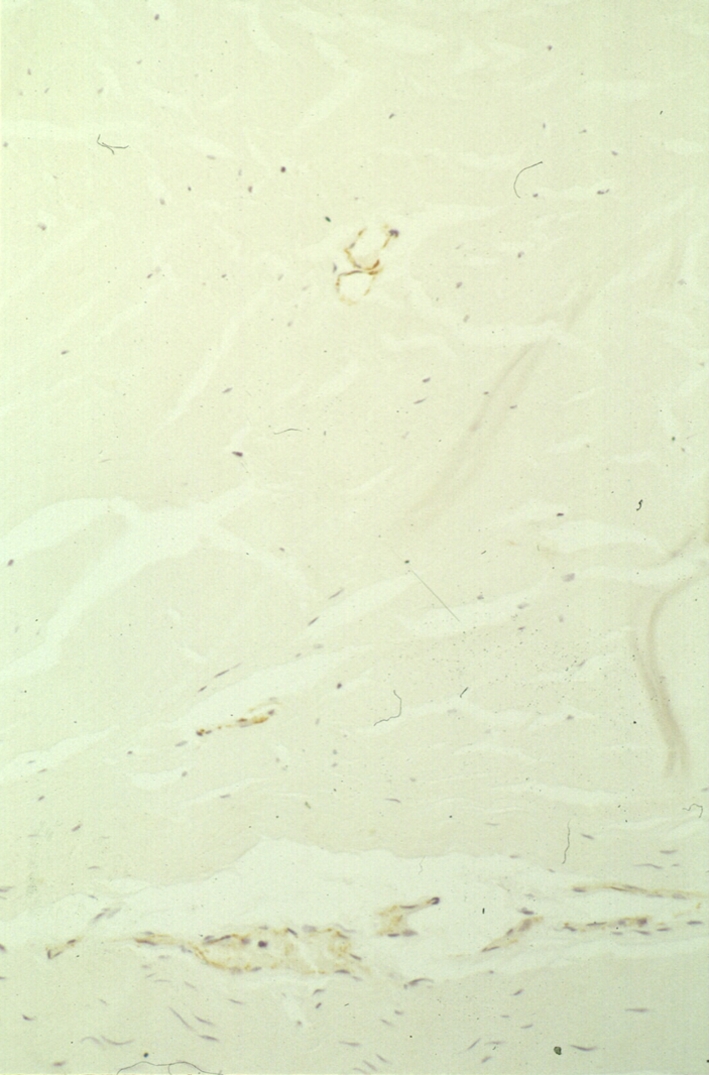
Fig. 6.
Severely disturbed intervertebral discs of an elderly individual (77 years) show a focal ingrowth of blood vessels adjacent to degenerative lesions, sometimes in a granulation like pattern. An annular tear is associated with granulation tissue formation, which in turn contains small blood vessels (a). Small vascular invasion of the outer anulus fibrosus in the presence of a cleft formation (b). Original magnification: a ×400; b ×400
Quantitative morphometric evaluation of the blood vessel “extension depth” into the outer anulus fibrosus in the autopsy group
In order to quantify the depth of blood vessels extending into the outer anulus fibrosus, we performed a morphometric analysis by counting the collagen lamellae of the AF between the ligament insertion and the “deepest” blood vessel (Table 3). The values were evaluated separately for the anterior and the posterior anulus fibrosus. The posterior outer anulus contained vessels extending deeper into the disc than in the anterior anulus. Fetal and infantile discs showed generally a deeper penetration by blood vessels into the outer anulus fibrosus (both anterior and posterior). The young adults had the least deepest penetration by blood vessels. In old age discs, the extension of blood vessels was deeper than in young adults, which was related to the generation of granulation tissue subsequent to tissue defects.
Table 3.
Quantitative morphometric analysis of blood vessel penetration in the anterior and posterior anulus fibrosus
| Age | Anterior anulusa | Posterior anulus |
|---|---|---|
| Fetal/infantile | 6.63 ± 0.92 | 7.12 ± 0.64 |
| Juvenile | 5.63 ± 2.72 | 5.87 ± 2.29 |
| Adolescent | 2.33 ± 1.75 | 3.83 ± 2.04 |
| Young adult | 1.50 ± 1.22 | 3.16 ± 0.98 |
| Adult | 2.83 ± 1.83 | 5.13 ± 4.02 |
| Senile | 2.00 ± 1.07 | 4.69 ± 2.84 |
aMean ± SD of number of collagen lamellae penetrated by blood vessels
Correlative analysis of blood vessel penetration with age and degeneration
When age was correlated with the penetration depth of blood vessels a significant inverse correlation was found for the anterior (ρ = −0.634, P > 0.0001) and posterior anulus (ρ = −0.618, P < 0.0001). No significant correlation was found when the extent of disc degeneration as assessed by the HDS [3] was compared to blood vessel penetration depth in adult (>21 years) anterior anulus (ρ = −0.043, P = 0.857) and posterior anulus (ρ = 0.332, P < 0.153). In general, the penetration depth of blood vessel was “deeper” within the posterior compared to the anterior anulus (P < 0.006).
Qualitative observations in the surgical disc samples
In general, the anatomic depiction of these specimens was compromised with regard to a clear distinction between anulus and nucleus. Despite this limitation, our samples allowed to evaluate presence or absence of blood vessels in tissue regions presumably representing nucleus pulposus tissue. All surgical samples contained clearly identifiable parts of the anulus fibrosus. Here, we could identify blood vessels in all 20 disc samples in the periphery of the tissue as expected. None of the 20 disc samples from symptomatic individuals, revealed blood vessel in-growth in regions representing inner anulus or nucleus pulposus. However, those samples with annular tears and clefts or rim lesions revealed small capillary in-growth of blood vessels along the defects, similar to that seen in fragmented material of herniated and/or sequestered disc material.
Discussion
This study provides clear evidence that juvenile, adolescent and adult human intervertebral discs without evidence of major disc degeneration are avascular. This confirms a previous own histological study on this issue without immunohistochemical analysis [3]. In contrast, we have clearly shown that inner regions of the anulus fibrosus and the cartilaginous end plate are vascularized in the fetal and early postnatal period. In our series, this vascular supply is seen until the age of approximately 2 years. The only exception of this lack of blood supply in normal discs is seen in the outermost zone of the anulus fibrosus where we observed small capillary vessels in all age categories. Here, the blood vessels of the longitudinal ligaments reach into the outer anulus fibrosus. This is seen in fetal and juvenile disc samples, but also in adolescent and (young and old) adult discs regardless of age.
Our quantitative morphometric data support the notion that there exist major differences in the age-associated extension of blood vessels into the outer anulus fibrosus. While there is a strong negative correlation of vascular penetration and age over the whole age range, this significant correlation is lost when only adult (>21 years) discs are considered. The “deeper” extension in the posterior than anterior anulus may indicate less tight collagen network structures, which can more easily be penetrated.
Neo-vascularization of the intervertebral discs in the context of disc herniation has been reported in several papers and appears to be a consistent finding [5, 6, 15, 16, 19–21, 23]. Less information is available on the question whether vascular in-growth occurs in the process of disc degeneration [4, 11, 16, 17]. It is assumed that the in-growth of blood vessels is associated with a concomitant in-growth of nerve fibers [7–9]. Freemont et al. [8] investigated the occurrence of nerve fiber in-growth in surgical specimens obtained from patients undergoing anterior fusion operations. The authors observed deep nerve in-growth into the inner third of the anulus fibrosus, the nucleus pulposus, or both in 4 biopsy samples out of a total of 16 patients (25%) from asymptomatic levels and in 17 samples out of 30 patients (57%) from painful (based on positive provocative discography) levels. Nerves usually accompanied blood vessels, but in 14 of 30 samples from back-pain patients isolated nerve fibers were seen. In a subsequent paper, Freemont et al. [9] reported that vessels entered the avascular IVD through the discal end plates. Furthermore, the authors reported that painless discs exhibited vessels within them, which entered through the anulus fibrosus. Similarly, Johnson et al. [11] investigated disc specimens obtained during anterior fusion operations and found that blood vessels were observed furthermost into the disc than nerves or Schwann cells. Much of the nerve and Schwann cell in-growth was found in vascularized areas of the disc, where the lamellar structure of the anulus fibrosus was disrupted. However, nerves were not observed in the nucleus pulposus of any discs examined.
In the present study on autopsy material without a known history of back pain, even samples showing significant age-related histological changes did not exhibit blood vessels in the inner anulus fibrosus and nucleus pulposus. The only exception is in cases of a complete destruction of the disc with replacement by scar-like tissue, which contains some blood vessels. However, disc degeneration was associated with two important alterations of blood vessel supply: (1) Annular tears were frequently associated with a small capillary network running concomitant with clefts and tears. This feature of vascular proliferation parallels that of granulation tissue. (2) Degenerative lesions of the cartilaginous end plate were often associated with an in-growth of capillary buds into the cartilage tissue. Thereby, degeneration seems to be associated with enhanced vascularization of the more peripheral zones of the discs. In this setting, our observations are well in line with the few previous studies, particularly with those from Freemont et al. [8]. Additionally, there is extensive agreement with the observations by Johnson et al. [11]. However, we were not able to reproduce the findings by Freemont et al. [8] who described enhanced vascularization of surgical disc tissue samples including a relatively high frequency of vascularized nucleus pulposus. We acknowledge that substantial differences can be related to the source of the disc material. In our study, we used autopsy material for which we do not have conclusive information on the patients’ back pain history. However, none of our patients had a reported back problem mentioned in the clinical notes available at autopsy. In our surgical sample group, the spatial depiction was less clear than in the autopsy group. However, we could identify the annular region in all 20 disc samples. In none of the cases, we have observed a vascular in-growth from the periphery to the more central part of the disc.
The clinical relevance of the study of blood vessels and innervation is related to the potential explanation of discogenic pain pathogenesis. Freemont et al. [8, 9] hypothesized that nociception is caused by direct stimulation of nerve fibers (neoneuralization) via nociceptive pain mediators (e.g., substance P) within the intervertebral disc. However, the induction of discogenic pain must not merely be linked to disc innervation, but is even more likely to be induced or promoted by the liberation of pro-inflammatory cytokines or other pain-inducing factors. In this context, it is of interest that we recently observed an association between the synthesis of TNF-α, one of the most potent pro-inflammatory cytokines, and the formation of tissue clefts [22]. This indicates that potentially pain-inducing factors can be synthesized within the disc and then rapidly transported through those clefts to blood vessels (and thereby to distant neuroceptive structures, e.g., in the perispinal space) and/or directly to nociceptive structures in the outer anulus fibrosus or the peridiscal tissue. This may especially be valid for those discs with extensive clefts as seen in advanced degeneration. Since the disruption was seen increasingly with age the rapid spread of intradiscal substances to the peridiscal space is an interesting concept of disc pathophysiology and pain induction.
Limitation of this study are predominately related to the study population. While autopsy specimens allow for a precise anatomical analysis of the penetration of blood vessels; we have only investigate mid-sagittal sections. We cannot rule out that other, e.g., more lateral regions of the anulus fibrosus may contain more or “deeper” penetrating vessels. Surgical specimen have the limitation of an impaired spatial resolution of the disc compartments as outlined above. Furthermore, we have no absolute proof that a specific disc is really the source for the patient’s symptoms despite a positive provocative discography.
In summary, our findings on complete cross-sections of whole motion segments of human lumbar discs and surgical samples show that vascular invasion deeper than the periphery was not observed during disc degeneration which supports the hypothesis that vascular in-growth is not a distinct feature of disc degeneration.
Footnotes
This study was supported by a grant from the AO/ASIF Foundation Switzerland (00-B72) and a grant from the AO Spine (SRN 02/103).
References
- 1.Albelda SM, Muller WA, Buck CA, Newman PJ. Molecular and cellular properties of PECAM-1 (endoCAM/CD31): a novel vascular cell-cell adhesion molecule. J Cell Biol. 1991;114:1059–1068. doi: 10.1083/jcb.114.5.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boos N, Nerlich A, Wiest I, Mark K, Aebi M. Immunolocalization of type X collagen in human lumbar intervertebral discs during ageing and degeneration. Histochem Cell Biol. 1997;108:471–480. doi: 10.1007/s004180050187. [DOI] [PubMed] [Google Scholar]
- 3.Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt K, Nerlich AG. 2002 volvo award in basic science: histologic classification of age-related changes in lumbar intervertebral discs. Spine. 2002;27:2631–2644. doi: 10.1097/00007632-200212010-00002. [DOI] [PubMed] [Google Scholar]
- 4.Brown MF, Hukkanen MV, McCarthy ID, Redfern DR, Batten JJ, Crock HV, Hughes SP, Polak JM. Sensory and sympathetic innervation of the vertebral endplate in patients with degenerative disc disease. J Bone Joint Surg Br. 1997;79:147–153. doi: 10.1302/0301-620X.79B1.6814. [DOI] [PubMed] [Google Scholar]
- 5.Carreon LY, Ito T, Yamada M, Uchiyama S, Takahashi HE (1997) Neovascularization induced by anulus and its inhibition by cartilage endplate. Its role in disc absorption. Spine 22:1429–1434; discussion 1446–1447 [DOI] [PubMed]
- 6.Cooper RG, Freemont AJ, Hoyland JA, Jenkins JP, West CG, Illingworth KJ, Jayson MI. Herniated intervertebral disc-associated periradicular fibrosis and vascular abnormalities occur without inflammatory cell infiltration. Spine. 1995;20:591–598. doi: 10.1097/00007632-199503010-00016. [DOI] [PubMed] [Google Scholar]
- 7.Freemont AJ, Jeziorska M, Hoyland JA, Rooney P, Kumar S. Mast cells in the pathogenesis of chronic back pain: a hypothesis. J Pathol. 2002;197:281–285. doi: 10.1002/path.1107. [DOI] [PubMed] [Google Scholar]
- 8.Freemont AJ, Peacock TE, Goupille P, Hoyland JA, O’Brien J, Jayson MIV. Nerve ingrowth into diseased intervertebral disc in chronic back pain. Lancet. 1997;350:178–181. doi: 10.1016/S0140-6736(97)02135-1. [DOI] [PubMed] [Google Scholar]
- 9.Freemont AJ, Watkins A, Le Maitre C, Baird P, Jeziorska M, Knight MT, Ross ER, O’Brien JP, Hoyland JA. Nerve growth factor expression and innervation of the painful intervertebral disc. J Pathol. 2002;197:286–292. doi: 10.1002/path.1108. [DOI] [PubMed] [Google Scholar]
- 10.Horner HA, Urban JP. 2001 volvo award winner in basic science studies: effect of nutrient supply on the viability of cells from the nucleus pulposus of the intervertebral disc. Spine. 2001;26:2543–2549. doi: 10.1097/00007632-200112010-00006. [DOI] [PubMed] [Google Scholar]
- 11.Johnson WE, Evans H, Menage J, Eisenstein SM, El Haj A, Roberts S. Immunohistochemical detection of Schwann cells in innervated and vascularized human intervertebral discs. Spine. 2001;26:2550–2557. doi: 10.1097/00007632-200112010-00007. [DOI] [PubMed] [Google Scholar]
- 12.Kauppila LI. Ingrowth of blood vessels in disc degeneration. Angiographic and histological studies of cadaveric spines. J Bone Joint Surg Am. 1995;77:26–31. doi: 10.2106/00004623-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Nerlich AG, Boos N, Wiest I, Aebi M. Immunolocalization of major interstitial collagen types in human lumbar intervertebral discs of various ages. Virchows Arch. 1998;432:67–76. doi: 10.1007/s004280050136. [DOI] [PubMed] [Google Scholar]
- 14.Nerlich AG, Schleicher E, Boos N. 1997 volvo award in basic science. Immunohistochemical markers of age-related changes in the human lumbar intervertebral disc. Spine. 1997;22:2781–2795. doi: 10.1097/00007632-199712150-00001. [DOI] [PubMed] [Google Scholar]
- 15.Pai RR, D’sa B, Raghuveer CV, Kamath A. Neovascularization of nucleus pulposus. A diagnostic feature of intervertebral disc prolapse. Spine. 1999;24:739–741. doi: 10.1097/00007632-199904150-00002. [DOI] [PubMed] [Google Scholar]
- 16.Repanti M, Korovessis PG, Stamatakis MV, Spastris P, Kosti P. Evolution of disc degeneration in lumbar spine: a comparative histological study between herniated and postmortem retrieved disc specimens. J Spinal Disord. 1998;11:41–45. doi: 10.1097/00002517-199802000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Rudert M, Tillmann B. Detection of lymph and blood vessels in the human intervertebral disc by histochemical and immunohistochemical methods. Anat Anz. 1993;175:237–242. doi: 10.1016/s0940-9602(11)80009-9. [DOI] [PubMed] [Google Scholar]
- 18.Stockinger H, Gadd SJ, Eher R, Majdic O, Schreiber W, Kasinrerk W, Strass B, Schnabl E, Knapp W. Molecular characterization and functional analysis of the leukocyte surface protein CD31. J Immunol. 1990;145:3889–3897. [PubMed] [Google Scholar]
- 19.Tolonen J, Grönblad M, Virri J, Seitsalo S, Rytomaa T, Karaharju E. Basic fibroblast growth factor immunoreactivity in blood vessels and cells of disc herniations. Spine. 1995;20:271–276. doi: 10.1097/00007632-199502000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Tolonen J, Grönblad M, Virri J, Seitsalo S, Rytomaa T, Karaharju EO. Platelet-derived growth factor and vascular endothelial growth factor expression in disc herniation tissue: and immunohistochemical study. Eur Spine J. 1997;6:63–69. doi: 10.1007/BF01676576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Virri J, Gronblad M, Savikko J, Palmgren T, Seitsalo S, Ruuskanen M, Karaharju E. Prevalence, morphology, and topography of blood vessels in herniated disc tissue. A comparative immunocytochemical study. Spine. 1996;21:1856–1863. doi: 10.1097/00007632-199608150-00004. [DOI] [PubMed] [Google Scholar]
- 22.Weiler C, Nerlich AG, Bachmeier BE, Boos N. Expression and distribution of tumor necrosis factor alpha in human lumbar intervertebral discs. A study in surgical specimens and autopsy controls. Spine. 2005;30:44–54. doi: 10.1097/01.brs.0000174529.07959.c0. [DOI] [PubMed] [Google Scholar]
- 23.Yasuma T, Arai K, Yamauchi Y. The histology of lumbar intervertebral disc herniation. The significance of small blood vessels in the extruded tissue. Spine. 1993;18:1761–1765. doi: 10.1097/00007632-199310000-00008. [DOI] [PubMed] [Google Scholar]