Abstract
A report of our experiences involving the treatment six male patients with a new method of closing perforations in the pharynx and upper esophagus, following surgery of the cervical spine region. Perforation of the pharynx and upper esophagus are rare complications following cervical spine surgery. The grave consequences of these complications necessitate in most cases immediate surgical therapy. In most cases, the first step involves the removal of the cervical plate and screws. The defect was then closed using a vascular pedicled musculofascia flap derived from the infrahyoid musculature. In all cases, the flap healed into place without complications. The patients began taking oral nutrients after an average of seven postoperative (5–12) days. In none of the cases did functional disorders or complications arise during the follow-up period (1–5 years). The infrahyoid muscle flap is well suited for reconstruction of the posterior pharyngeal wall and the upper esophagus.
Keywords: Pharynx, Esophagus, Perforation, Infrahyoid muscle flap, Ventral spondylodesis, Complication
Introduction
Pharyngeal and esophageal perforations are burdened with a high morbidity and mortality rate. An early diagnosis determines and influences the patient’s further condition. Complications can be reduced by an appropriate and rapid therapeutic intervention [3].
While small-circumscribed perforations can be treated conservatively, larger and direct perforations require rapid surgical intervention. There is a variety of surgical procedures for treating such injuries. As well as direct suturing, mucosal flaps, autotransplants and jejunocolonic interposition grafts are utilised. In 1981 Rubin described the use of a sternocleidomastoid muscle (SCM) flap as another surgical alternative [5, 8].
This article will report on a vascular pedicled flap for surgical fistulae intervention in the area of the pharynx following anterior cervical spine surgery.
Materials and methods
A retrospective study from 1999 to 2004 treating six patients at a Trauma Center for pharyngeal fistulae following anterior cervical spine surgery.
Case report
A 67-year-old male patient presented with recurrent pharyngocutaneous fistula in the right cervical region over the preceding 3 years.
In November 1998, following an accident resulting in a complete functional quadriplegia at the level of C5–C6, the patient underwent a ventral stabilization as the primary therapy. A revision operation involving ventral osteosynthesis replacement was carried out a few days later as a result of postoperative instability. Recurrent infections and abscesses in the right cervical area complicated the postoperative course. Multiple operative and conservative therapies were attempted, however, without succeeding in closing the fistula or improving the clinical condition.
Following transfer to our clinic, radiological examination showed protrusion of the screws into the esophagus (Figs. 1, 2 ). A revision operation was carried out via the existing scars in the right cervical region. Releasing the scarred SCM from the larynx and thyroid, a perforation in the posterior part of the pharynx at the level of C5–C6 over the cervical plate and screws was observed. After removing the cervical plate and screws, and hence enabling complete visualization of the defect (3 cm×7 cm), a right-sided infrahyoid muscle flap was prepared. The superior branch of the ansa cervicalis laterocranial to the hyoid bone was localized. Preservation of the arteriae thyreoidea superior and venae thyreoideae superiores was necessary to supply the musculofascia graft. The infrahyoid musculature was subsequently released at the hyoid bone. The muscles were elevated after separation in the middle line medial-to-lateral from the larynx and thyroid. The length of the flap will be defined through variations of the clavicular discontinuation level. Further preparation was carried out in the caudo-cranial direction along the carotid artery and the jugular vein including the ansa cervicalis (Figs. 3, 4 ).
Fig. 1.

Preoperative video fluoroscopy. The arrow shows the pharyngeal perforation
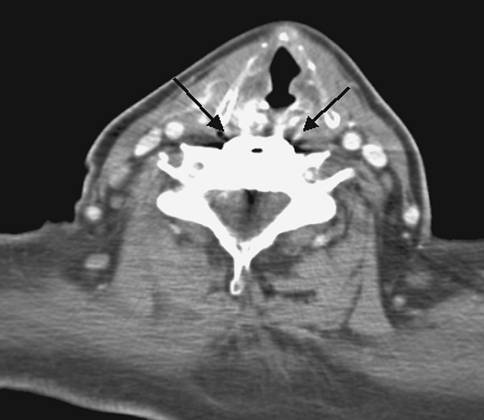
Fig. 2.
Preoperative CT scan. The arrow indicates the cervical plate and screws
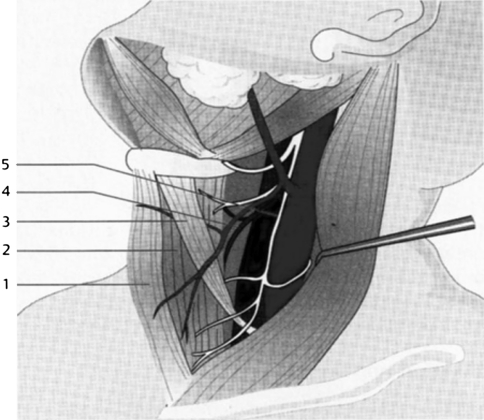
Fig. 3.
The infrahyoid musculature has a pedicle including the superior thyroid artery and vein (4) and the superior branch of the ansa cervicalis [7]
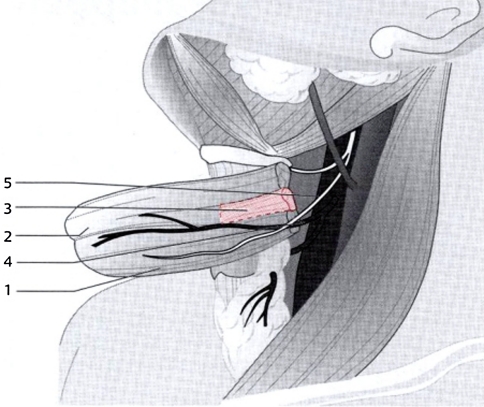
Fig. 4.
Separation of the musculofascia flap and preparation of the vasculature (4) and the ansa cervicalis nervi hypoglossi (5) [7]
The pedicled flap was rotated into the defect region at the pharynx posterior side. The defect edges on the pharynx were excised and the graft was sutured in two layers. Subsequently, the wound was closed and a drainage inserted. The patient was fed via a nasogastric tube for the following 7 days. Healing of the wound was of primary importance. X-ray examinations 7 days postoperative showed a proper esophageal passage (Figs. 5, 6 ).
Fig. 5.

Postoperative video fluoroscopy (7 days). The pharynx and esophagus are visualised with no indications of a fistula or stenosis
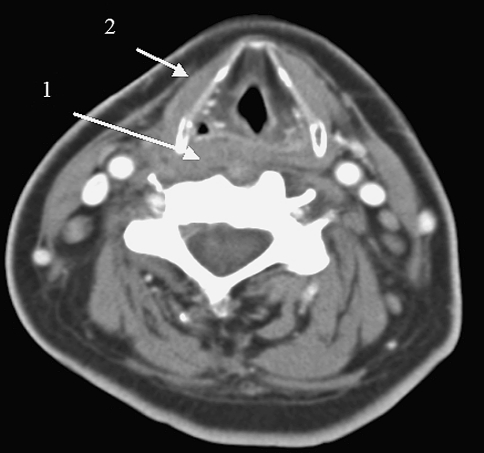
Fig. 6.
Postoperative CT scan: the cervical plate and screws have been removed; the pharynx has been reconstructed using an infrahyoid flap (1); the arrow indicates the missing sternohyoid muscle (2), used for pharyngeal reconstruction
Results
During the period 1999 to 2003, six male patients were treated for a pharyngeal fistula, using an infrahyoid flap as described, following cervical spine surgery. The mean age of the patients was 64.2 (24–76) years. The fistulae existed on an average for 131.8 (15–420) days. A mean of 2.5 (0–5) operations had been carried out in order to treat the fistulae. In all cases prior to reoperation a pharyngeal fistula was visible at the level of C4 through C6 by radiological examination. In each case the cervical plate and screws were removed intraoperatively. The fistula was closed as described. Postoperatively, patients were fed for 7.5 (5–12) days via a nasogastric tube. In all of the cases no complications occurred and the flap healed into place without any problems. Oral nutrition was started 7.5 (5–12) days postoperatively following radiological ruling out of a fistula. Regular endoscopic examinations showed epithelization of the infrahyoid flap after 4–6 weeks. During the follow-up period (1–5 years), no further fistulae appeared in these patients (see Table 1).
Table 1.
Patient information
| Name | Age (years) | Spinal level | Fistula duration (days) | Number of operations | Removal of nasogastric tube (days) | Complications |
|---|---|---|---|---|---|---|
| O.L. ♀ | 49 | C5–C7 | 210 | 4 | 9 | Ø |
| S.I. ♀ | 57 | C5–C6 | 15 | 0 | 6 | Ø |
| B.F. ♀ | 51 | C5–C6 | 54 | 2 | 12 | Ø |
| R.J. ♀ | 24 | C4–C6 | 61 | 2 | 4 | Ø |
| D.M. ♀ | 67 | C5–C6 | 420 | 5 | 7 | Ø |
| K.R. ♀ | 29 | C5–C6 | 31 | 2 | 7 | Ø |
Discussion
Esophageal injuries after osteosynthesis of the cervical spine are rare or infrequent complications. The frequency of implant penetration into the esophagus is given as 1 in 500 (0.2%) by Tew and Mayfield [9] and 0 in 100 (0%) by Aebi et al. [1]. The frequency of abscess formation following an operative revision of a cervical spine injury was given as 4 in 400 (1%) by Kelly et al. [4]. Causes for the injuries cited included incorrect screw length, injuries to the mucosa as a result of incorrect preparation or implant plates, or postoperative instability [6].
As well as iatrogenic esophageal lesions caused by sharp surgical instruments during cervical spine surgery, other such injuries may also be caused by mediastinoscopy or endoscopy. On the whole, the proximal esophagus is particularly vulnerable to injury as a result of its topographical location near the cervical spine. Traumatic lesions of the cervical esophagus were described in 20–40% of all esophageal injuries. The cricopharyngeal region (C5–C6) is at particularly high risk because of the attachment of the esophageal mucosa to the fascia [6].
To reduce mortality, the diagnosis should be confirmed by imaging CT and video fluoroscopy as soon as possible. Timing and treatment of the perforation depends on how early it is diagnosed. In general, early, aggressive intervention reduced morbidity and mortality [3]. If the perforation is found immediately, at the time of initial surgery or procedures, a simple suture should suffice. If the perforation is detected during the first hours or days after operation, surgical closure, careful drainage and thorough irrigation of the area operated upon should be performed in order to reduce the risk of a wound infection.
If there is a delay in detecting a perforation, there will usually be a neck fistula with or without an abscess. Treatment of abscesses should include the removal and closure of the fistulous tract, reinforcement using muscle flaps and placement of drains in the inflamed area. If the abscess is not accompanied by a fistula, incision and drainage with continuous suctioning of saliva from the esophagus is to be performed [6].
Application of an SCM flap is a further surgical alternative for closing an esophageal fistula [5, 8]. In our view, the lack of a clearly defined arterial blood supply, the late oral intake (59.2 days [5]), the limitations of modelling and consequent risk of stenosis limit the applicability of this regional flap. Other reconstructive techniques, e.g., jejunal grafts or esophageal resection are technically more demanding, requiring a greater surgical effort and having a higher morbidity [3].
In 1977 Clairemont was first to describe the preparation of an infrahyoid muscle flap [2]. In 1978 Weerda described a procedure for tracheal reconstruction [11]. Wang et al. (1986) [10] and Remmert et al. (1994) [7] expanded this procedure to reconstructive procedures for tongue defects. Innervation of the flap using the ansa cervicalis as described for reconstructive surgery of the tongue is of less importance for treatment of pharyngeal defects but can, however, have a positive effect on the swallowing ability.
The flap in comparison with other procedures, in particular the muscle graft from the m. sternocleidomastoideus, offers clearer advantages. The flap, possessing a definite arterial and venous supply, is simple to prepare via the necessary operative approach to the defect or the wound, and is of a suitable thickness for reconstructive defects on posterior esophagus. It is possible to treat defects with a diameter of up to 4 cm × 7 cm. The flap is also suitable for reconstructive defects following tumor operations.
Conclusion
Injury to the pharynx and upper esophagus requires rapid operative revision. Various operative procedures are available for treatment. The infrahyoid muscle flap presented here is recommended because of its ease of preparation, its assured arterial and venous supply, and its good modeling for the treatment of larger defects (4 cm × 7 cm).
References
- 1.Aebi M, Mohler J, Zach GA, Morscher E. Indication, surgical technique, and results of 100 surgically-treated fractures and fracture-dislocations of the cervical spine. Clin Orthop Relat Res. 1986;203:244–257. [PubMed] [Google Scholar]
- 2.Clairmont AA, Conley JJ. Surgical technique—the strap muscle flap. J Otolaryngol. 1977;6:200–202. [PubMed] [Google Scholar]
- 3.Jones WG, 2nd, Ginsberg RJ. Esophageal perforation: a continuing challenge. Ann Thorac Surg. 1992;53:534–543. doi: 10.1016/0003-4975(92)90294-E. [DOI] [PubMed] [Google Scholar]
- 4.Kelly MF, Spiegel J, Rizzo KA, Zwillenberg D. Delayed pharyngoesophageal perforation: a complication of anterior spine surgery. Ann Otol Rhinol Laryngol. 1991;100:201–205. doi: 10.1177/000348949110000307. [DOI] [PubMed] [Google Scholar]
- 5.Navarro R, Javahery R, Eismont F, Arnold DJ, Bhatia NN, Vanni S, Levi AD. The role of the sternocleidomastoid muscle flap form esophageal fistula repair in anterior cervical spine surgery. Spine. 2005;30:E617–E622. doi: 10.1097/01.brs.0000182309.97403.ca. [DOI] [PubMed] [Google Scholar]
- 6.Orlando ER, Caroli E, Ferrante L. Management of the cervical esophagus and hypopharynx perforations complicating anterior cervical spine surgery. Spine. 2003;28:E290–E295. doi: 10.1097/00007632-200308010-00023. [DOI] [PubMed] [Google Scholar]
- 7.Remmert S, Majocco A, Sommer K, Ahrens KD, Weerda H. A new method of tongue reconstruction with neurovascular infrahyoid muscle–fascia flaps. Laryngorhinootologie. 1994;73:198–201. doi: 10.1055/s-2007-997110. [DOI] [PubMed] [Google Scholar]
- 8.Rubin JS. Sternocleidomastoid myoplasty for the repair of chronic cervical esophageal fistulae. Laryngoscope. 1986;96:834–836. doi: 10.1288/00005537-198608000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Tew JM, Mayfield FH. Complications of surgery of the anterior cervical spine. Clin Neurosurg. 1976;23:424–434. doi: 10.1093/neurosurgery/23.cn_suppl_1.424. [DOI] [PubMed] [Google Scholar]
- 10.Wang HS, Shen JW, Ma DB, Wang JD, Tian AL. The infrahyoid myocutaneous flap for reconstruction after resection of head and neck cancer. Cancer. 1986;57:663–668. doi: 10.1002/1097-0142(19860201)57:3<663::AID-CNCR2820570344>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 11.Weerda H. One stage reconstruction of the trachea with an island flap. Arch Otorhinolaryngol. 1978;221:211–214. doi: 10.1007/BF01886297. [DOI] [PubMed] [Google Scholar]