Abstract
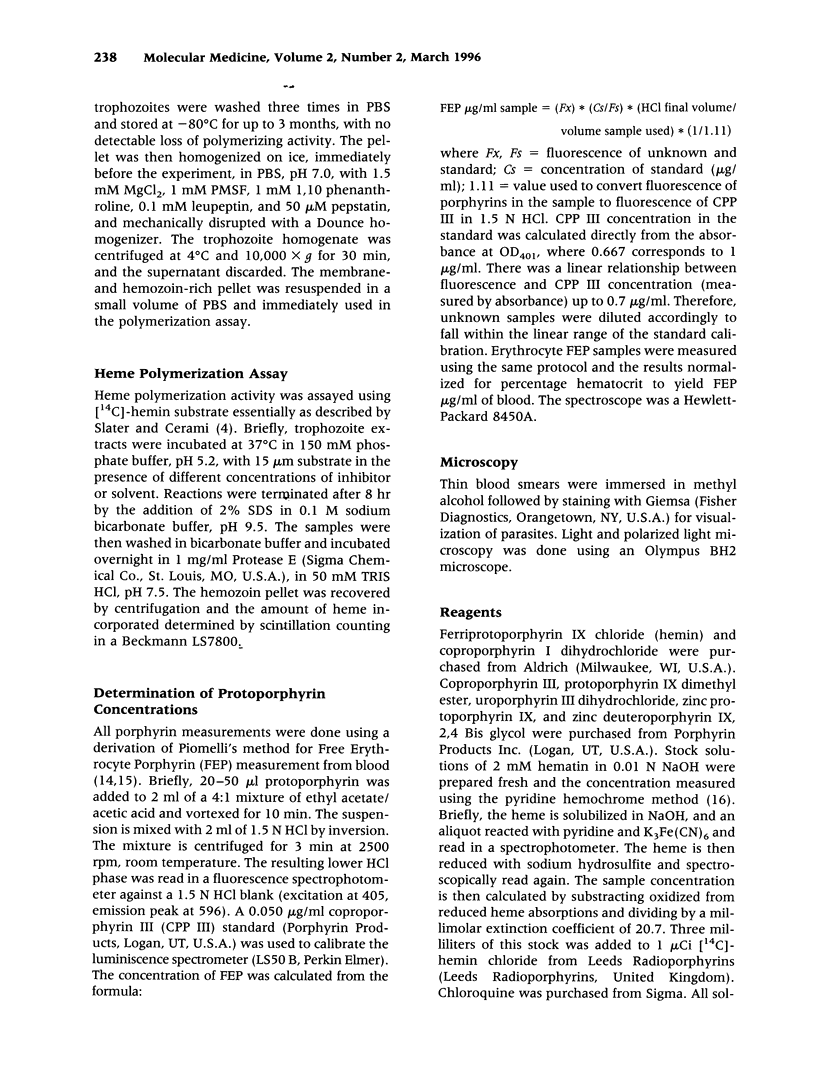
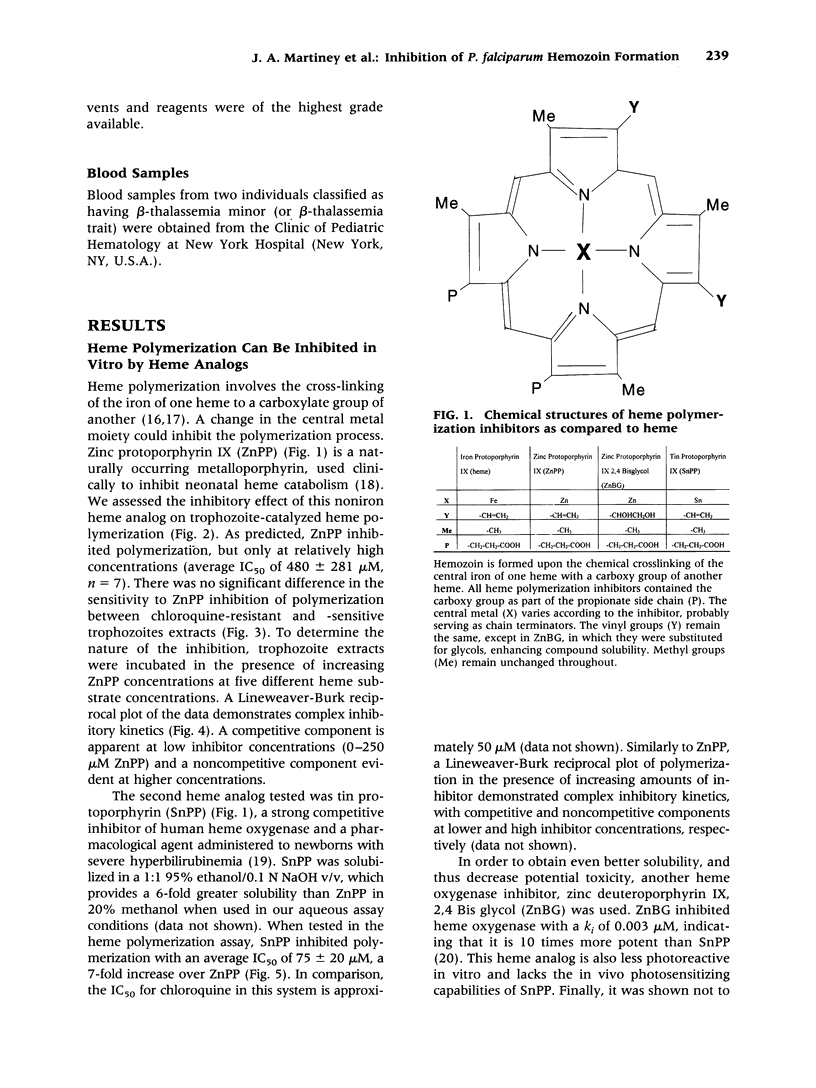
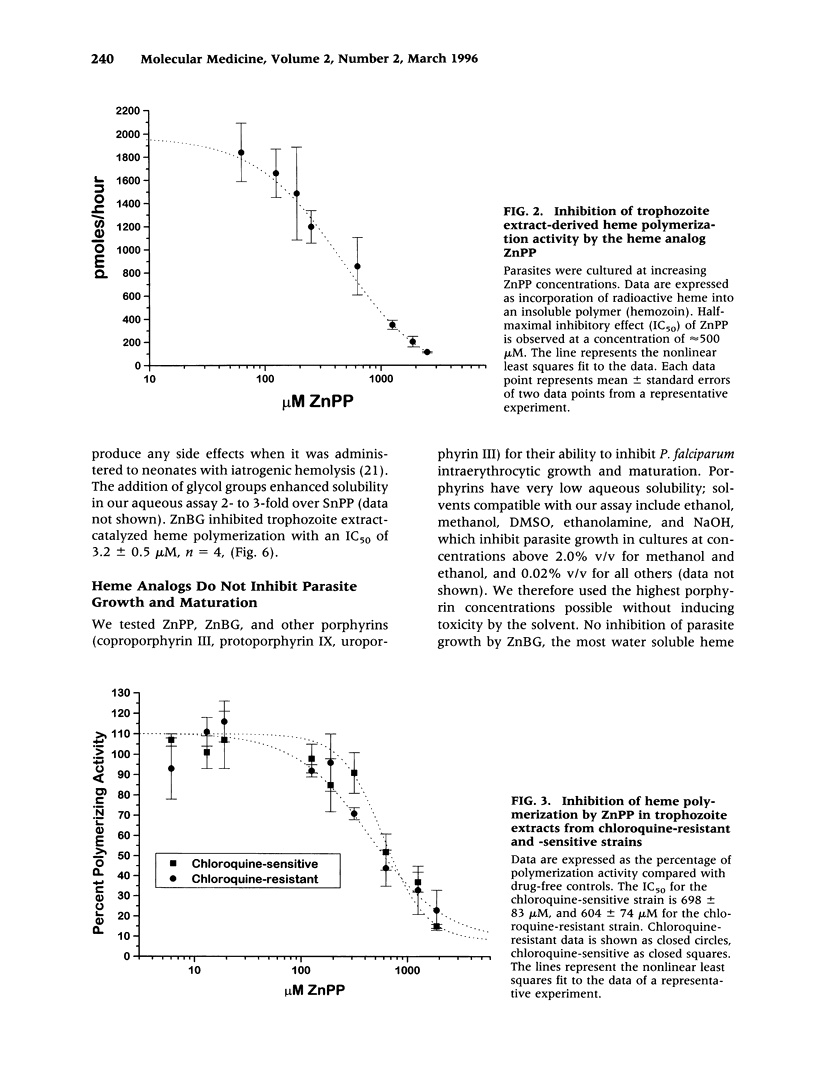
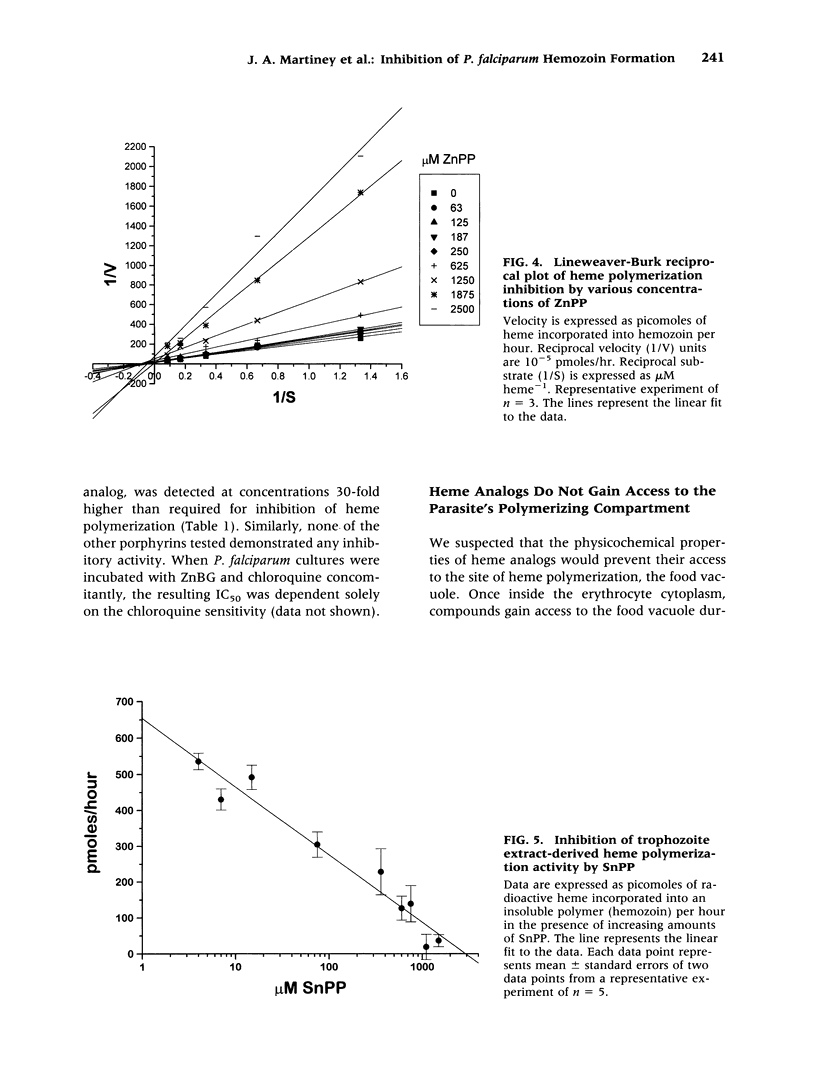
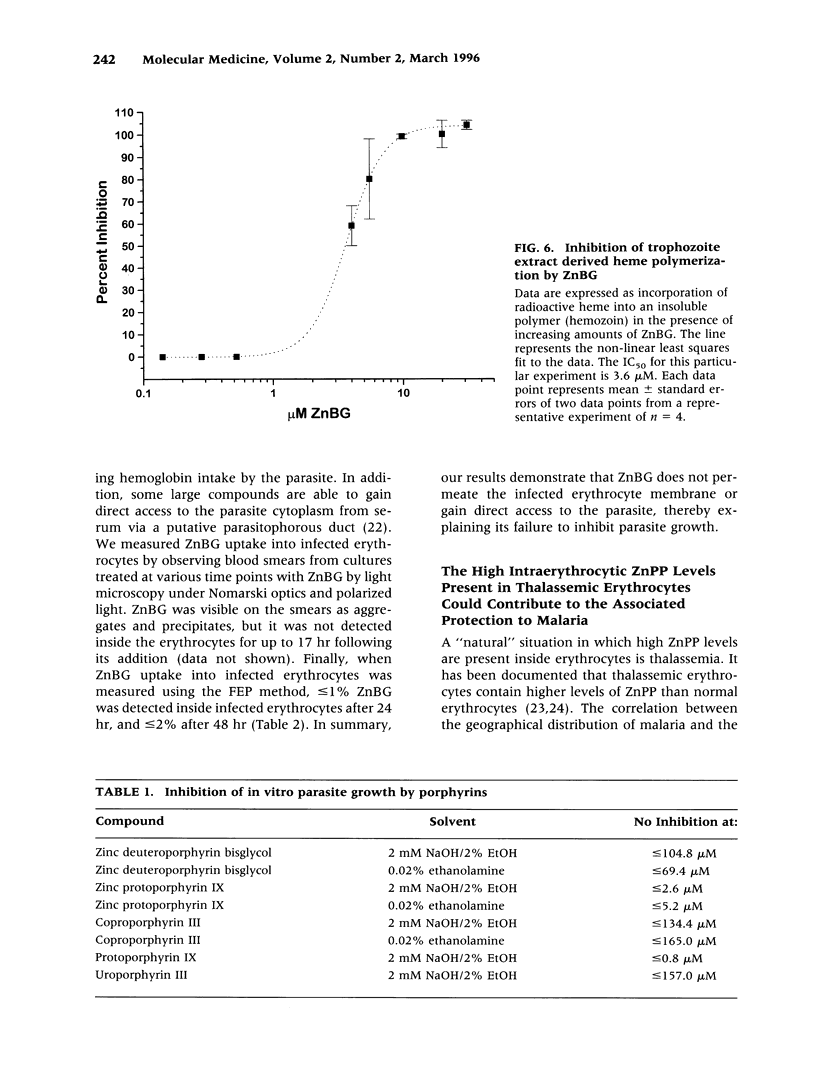
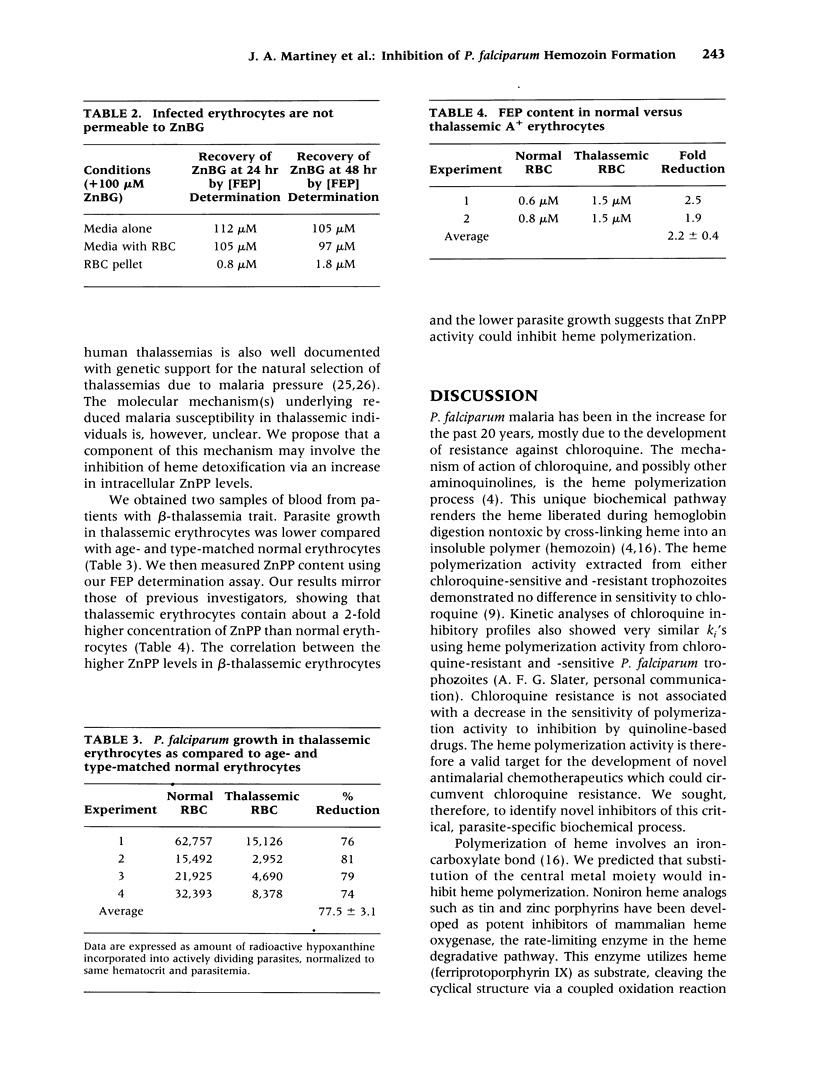
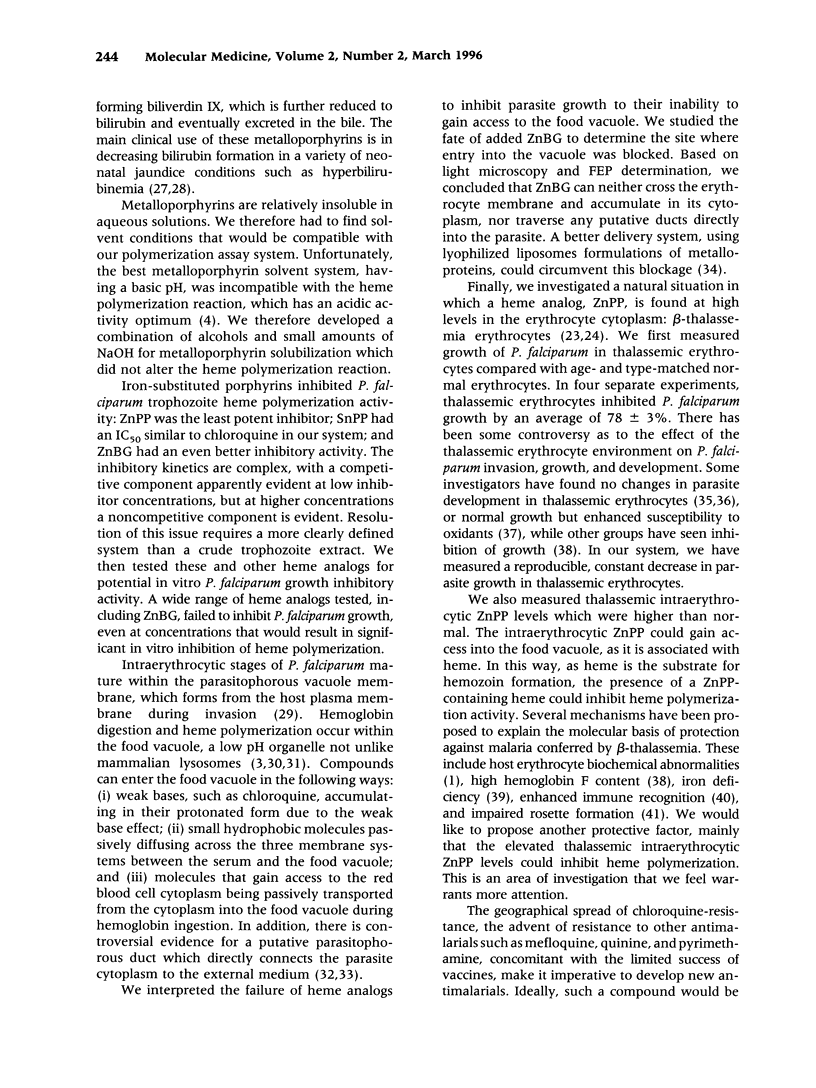
BACKGROUND: Human falciparum malaria, caused by the intracellular protozoa Plasmodium falciparum, results in 1-2 million deaths per year. P. falciparum digests host erythrocyte hemoglobin within its food vacuole, resulting in the release of potentially toxic free heme. A parasite-specific heme polymerization activity detoxifies the free heme by cross-linking the heme monomers to form hemozoin or malaria pigment. This biochemical process is the target of the widely successful antimalarial drug chloroquine, which is rapidly losing its effectiveness due to the spread of chloroquine resistance. We have shown that chloroquine resistance is not due to changes in the overall catalytic activity of heme polymerization or its chloroquine sensitivity. Therefore, the heme polymerization activity remains a potential target for novel antimalarials. In this study, we investigated the ability of heme analogs to inhibit heme polymerization and parasite growth in erythrocytes. MATERIALS AND METHODS: Incorporation of radioactive hemin substrate into an insoluble hemozoin pellet was used to determine heme polymerization. Incorporation of radioactive hypoxanthine into the nucleic acid of dividing parasites was used to determine the effects of heme analogs on parasite growth. Microscopic and biochemical measurements were made to determine the extent of heme analog entry into infected erythrocytes. RESULTS: The heme analogs tin protoporphyrin IX (SnPP), zinc protoporphyrin IX (ZnPP), and zinc deuteroporphyrin IX, 2,4 bisglycol (ZnBG) inhibited polymerization at micromolar concentrations (ZnPP << SnPP < ZnBG). However, they did not inhibit parasite growth since they failed to gain access to the site of polymerization, the parasite's food vacuole. Finally, we observed high ZnPP levels in erythrocytes from two patients with beta-thalassemia trait, which may inhibit heme polymerization. CONCLUSIONS: The heme analogs tested were able to inhibit hemozoin formation in Plasmodium falciparum trophozite extracts. The increased ZnPP levels found in thalassemic erythrocytes suggest that these may contribute, at least in part, to the observed antimalarial protection conferred by the beta-thalassemia trait. This finding may lead to the development of new forms of antimalarial therapy.
Full text
PDF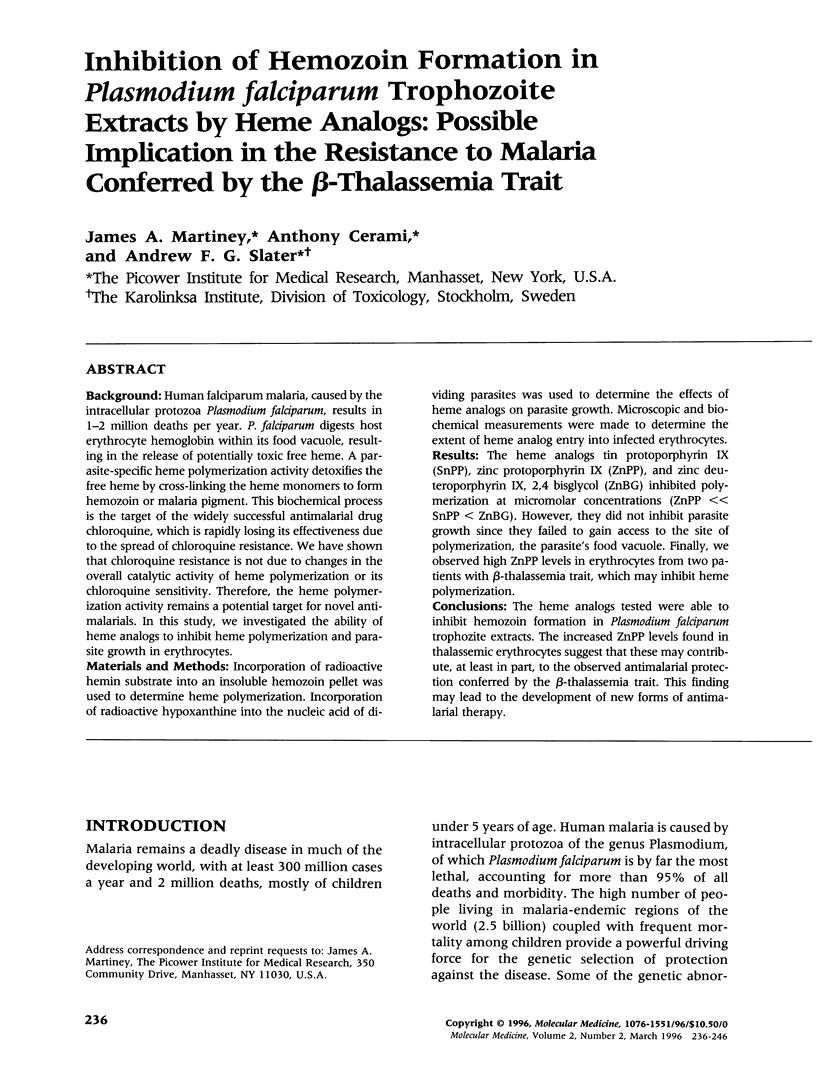

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bendrat K., Berger B. J., Cerami A. Haem polymerization in malaria. Nature. 1995 Nov 9;378(6553):138–139. doi: 10.1038/378138a0. [DOI] [PubMed] [Google Scholar]
- Cannon J. B., Martin C., Drummond G. S., Kappas A. Targeted delivery of a heme oxygenase inhibitor with a lyophilized liposomal tin mesoporphyrin formulation. Pharm Res. 1993 May;10(5):715–721. doi: 10.1023/a:1018911816814. [DOI] [PubMed] [Google Scholar]
- Carlson J., Nash G. B., Gabutti V., al-Yaman F., Wahlgren M. Natural protection against severe Plasmodium falciparum malaria due to impaired rosette formation. Blood. 1994 Dec 1;84(11):3909–3914. [PubMed] [Google Scholar]
- Chou A. C., Fitch C. D. Heme polymerase: modulation by chloroquine treatment of a rodent malaria. Life Sci. 1992;51(26):2073–2078. doi: 10.1016/0024-3205(92)90158-l. [DOI] [PubMed] [Google Scholar]
- Desjardins R. E., Canfield C. J., Haynes J. D., Chulay J. D. Quantitative assessment of antimalarial activity in vitro by a semiautomated microdilution technique. Antimicrob Agents Chemother. 1979 Dec;16(6):710–718. doi: 10.1128/aac.16.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn A., Stoffel R., Matile H., Bubendorf A., Ridley R. G. Malarial haemozoin/beta-haematin supports haem polymerization in the absence of protein. Nature. 1995 Mar 16;374(6519):269–271. doi: 10.1038/374269a0. [DOI] [PubMed] [Google Scholar]
- Flint J., Hill A. V., Bowden D. K., Oppenheimer S. J., Sill P. R., Serjeantson S. W., Bana-Koiri J., Bhatia K., Alpers M. P., Boyce A. J. High frequencies of alpha-thalassaemia are the result of natural selection by malaria. Nature. 1986 Jun 19;321(6072):744–750. doi: 10.1038/321744a0. [DOI] [PubMed] [Google Scholar]
- Friedman M. J. Oxidant damage mediates variant red cell resistance to malaria. Nature. 1979 Jul 19;280(5719):245–247. doi: 10.1038/280245a0. [DOI] [PubMed] [Google Scholar]
- Gluzman I. Y., Francis S. E., Oksman A., Smith C. E., Duffin K. L., Goldberg D. E. Order and specificity of the Plasmodium falciparum hemoglobin degradation pathway. J Clin Invest. 1994 Apr;93(4):1602–1608. doi: 10.1172/JCI117140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D. E., Slater A. F., Beavis R., Chait B., Cerami A., Henderson G. B. Hemoglobin degradation in the human malaria pathogen Plasmodium falciparum: a catabolic pathway initiated by a specific aspartic protease. J Exp Med. 1991 Apr 1;173(4):961–969. doi: 10.1084/jem.173.4.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han P., Fung K. P., Teo C. P., Tam L. P. Alpha-thalassaemia and beta-thalassaemia traits: biological difference based on red cell indices and zinc protoporphyrin. Clin Lab Haematol. 1990;12(2):169–176. [PubMed] [Google Scholar]
- Hill A. V., Flint J., Weatherall D. J., Clegg J. B. Alpha-thalassaemia and the malaria hypothesis. Acta Haematol. 1987;78(2-3):173–179. doi: 10.1159/000205870. [DOI] [PubMed] [Google Scholar]
- Jensen J. B., Trager W. Plasmodium falciparum in culture: use of outdated erthrocytes and description of the candle jar method. J Parasitol. 1977 Oct;63(5):883–886. [PubMed] [Google Scholar]
- Kappas A., Drummond G. S., Manola T., Petmezaki S., Valaes T. Sn-protoporphyrin use in the management of hyperbilirubinemia in term newborns with direct Coombs-positive ABO incompatibility. Pediatrics. 1988 Apr;81(4):485–497. [PubMed] [Google Scholar]
- Lambros C., Vanderberg J. P. Synchronization of Plasmodium falciparum erythrocytic stages in culture. J Parasitol. 1979 Jun;65(3):418–420. [PubMed] [Google Scholar]
- Luzzi G. A., Merry A. H., Newbold C. I., Marsh K., Pasvol G., Weatherall D. J. Surface antigen expression on Plasmodium falciparum-infected erythrocytes is modified in alpha- and beta-thalassemia. J Exp Med. 1991 Apr 1;173(4):785–791. doi: 10.1084/jem.173.4.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luzzi G. A., Torii M., Aikawa M., Pasvol G. Unrestricted growth of Plasmodium falciparum in microcytic erythrocytes in iron deficiency and thalassaemia. Br J Haematol. 1990 Apr;74(4):519–524. doi: 10.1111/j.1365-2141.1990.tb06344.x. [DOI] [PubMed] [Google Scholar]
- Lyberatos C., Chalevelakis G., Platis A., Stathakis N., Panani A., Gardikas C. Erythrocyte content of free protoporphyrin in thalassaemic syndromes. Acta Haematol. 1972;47(3):164–167. doi: 10.1159/000208511. [DOI] [PubMed] [Google Scholar]
- Nagel R. L., Roth E. F., Jr Malaria and red cell genetic defects. Blood. 1989 Sep;74(4):1213–1221. [PubMed] [Google Scholar]
- Nurse G. T. Iron, the thalassaemias, and malaria. Lancet. 1979 Nov 3;2(8149):938–940. [PubMed] [Google Scholar]
- Olliaro P. L., Goldberg D. E. The plasmodium digestive vacuole: metabolic headquarters and choice drug target. Parasitol Today. 1995 Aug;11(8):294–297. doi: 10.1016/0169-4758(95)80042-5. [DOI] [PubMed] [Google Scholar]
- Pasvol G., Wilson R. J. The interaction of malaria parasites with red blood cells. Br Med Bull. 1982 May;38(2):133–140. doi: 10.1093/oxfordjournals.bmb.a071749. [DOI] [PubMed] [Google Scholar]
- Piomelli S. A micromethod for free erythrocyte porphyrins: the FEP test. J Lab Clin Med. 1973 Jun;81(6):932–940. [PubMed] [Google Scholar]
- Piomelli S., Brickman A., Carlos E. Rapid diagnosis of iron deficiency by measurement of free erythrocyte porphyrins and hemoglobin: the FEP/hemoglobin ratio. Pediatrics. 1976 Jan;57(1):136–141. [PubMed] [Google Scholar]
- Rodgers P. A., Vreman H. J., Stevenson D. K. Heme catabolism in rhesus neonates inhibited by zinc protoporphyrin. Dev Pharmacol Ther. 1990;14(4):216–222. [PubMed] [Google Scholar]
- Slater A. F., Cerami A. Inhibition by chloroquine of a novel haem polymerase enzyme activity in malaria trophozoites. Nature. 1992 Jan 9;355(6356):167–169. doi: 10.1038/355167a0. [DOI] [PubMed] [Google Scholar]
- Slater A. F. Chloroquine: mechanism of drug action and resistance in Plasmodium falciparum. Pharmacol Ther. 1993 Feb-Mar;57(2-3):203–235. doi: 10.1016/0163-7258(93)90056-j. [DOI] [PubMed] [Google Scholar]
- Slater A. F. Malaria pigment. Exp Parasitol. 1992 May;74(3):362–365. doi: 10.1016/0014-4894(92)90162-4. [DOI] [PubMed] [Google Scholar]
- Slater A. F., Swiggard W. J., Orton B. R., Flitter W. D., Goldberg D. E., Cerami A., Henderson G. B. An iron-carboxylate bond links the heme units of malaria pigment. Proc Natl Acad Sci U S A. 1991 Jan 15;88(2):325–329. doi: 10.1073/pnas.88.2.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson D. K., Rodgers P. A., Vreman H. J. The use of metalloporphyrins for the chemoprevention of neonatal jaundice. Am J Dis Child. 1989 Mar;143(3):353–356. doi: 10.1001/archpedi.1989.02150150111027. [DOI] [PubMed] [Google Scholar]
- Taraschi T. F., Pouvelle B. There is no ducking the duct. Parasitol Today. 1994 Jun;10(6):212–213. doi: 10.1016/0169-4758(94)90113-9. [DOI] [PubMed] [Google Scholar]
- Trager W., Jensen J. B. Human malaria parasites in continuous culture. Science. 1976 Aug 20;193(4254):673–675. doi: 10.1126/science.781840. [DOI] [PubMed] [Google Scholar]
- Vreman H. J., Lee O. K., Stevenson D. K. In vitro and in vivo characteristics of a heme oxygenase inhibitor: ZnBG. Am J Med Sci. 1991 Dec;302(6):335–341. doi: 10.1097/00000441-199112000-00002. [DOI] [PubMed] [Google Scholar]
- Warhurst D. C. Haemozoin and the mode of action of blood schizontocides: more controversy. Parasitol Today. 1995 Jun;11(6):204–205. doi: 10.1016/0169-4758(95)80076-x. [DOI] [PubMed] [Google Scholar]


