Abstract
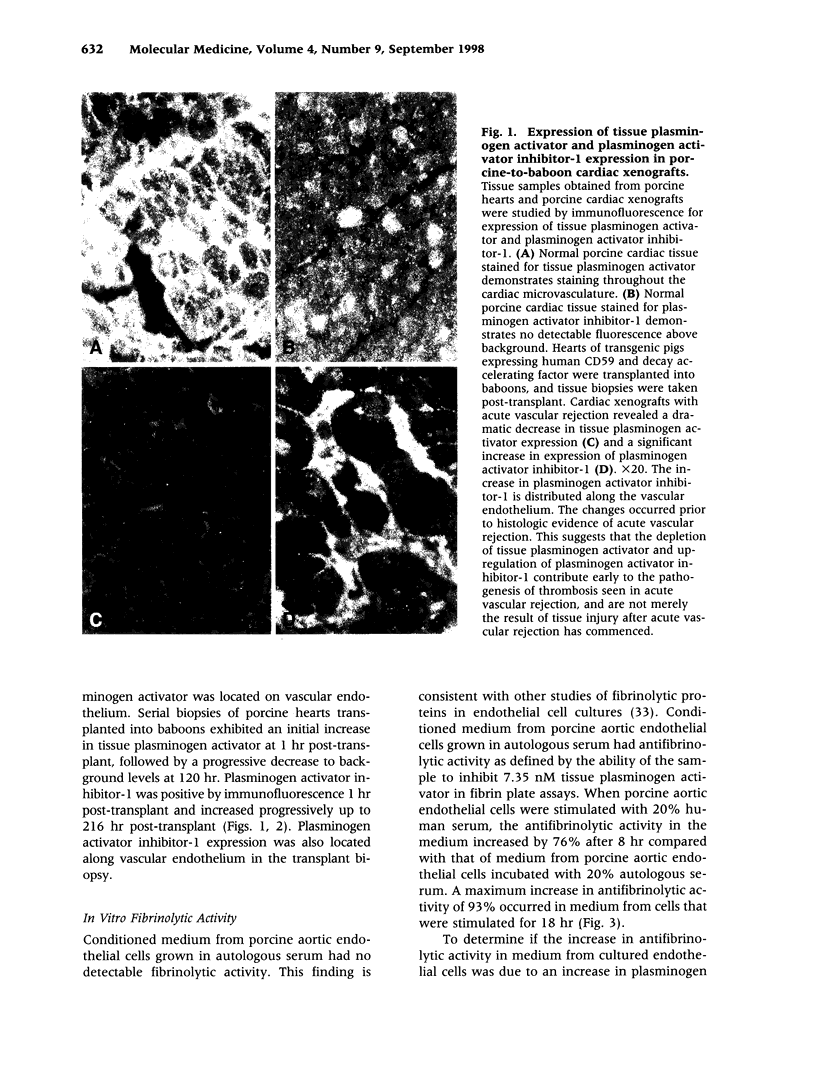
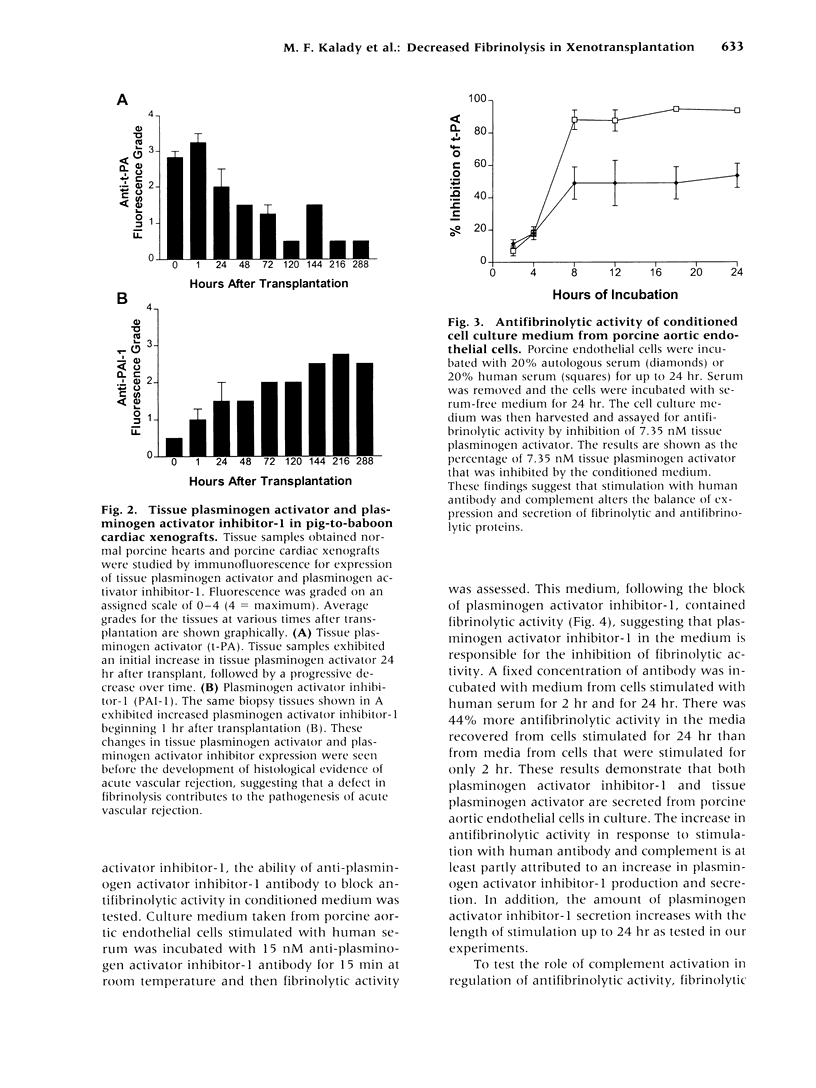
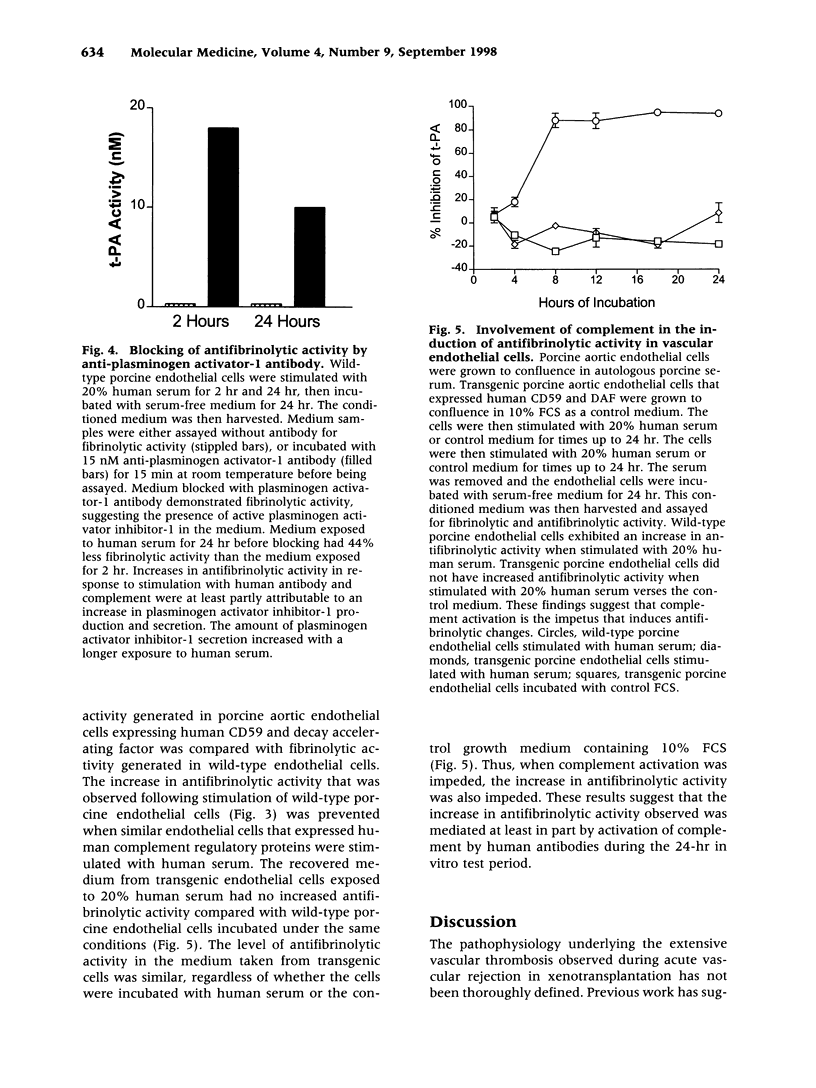
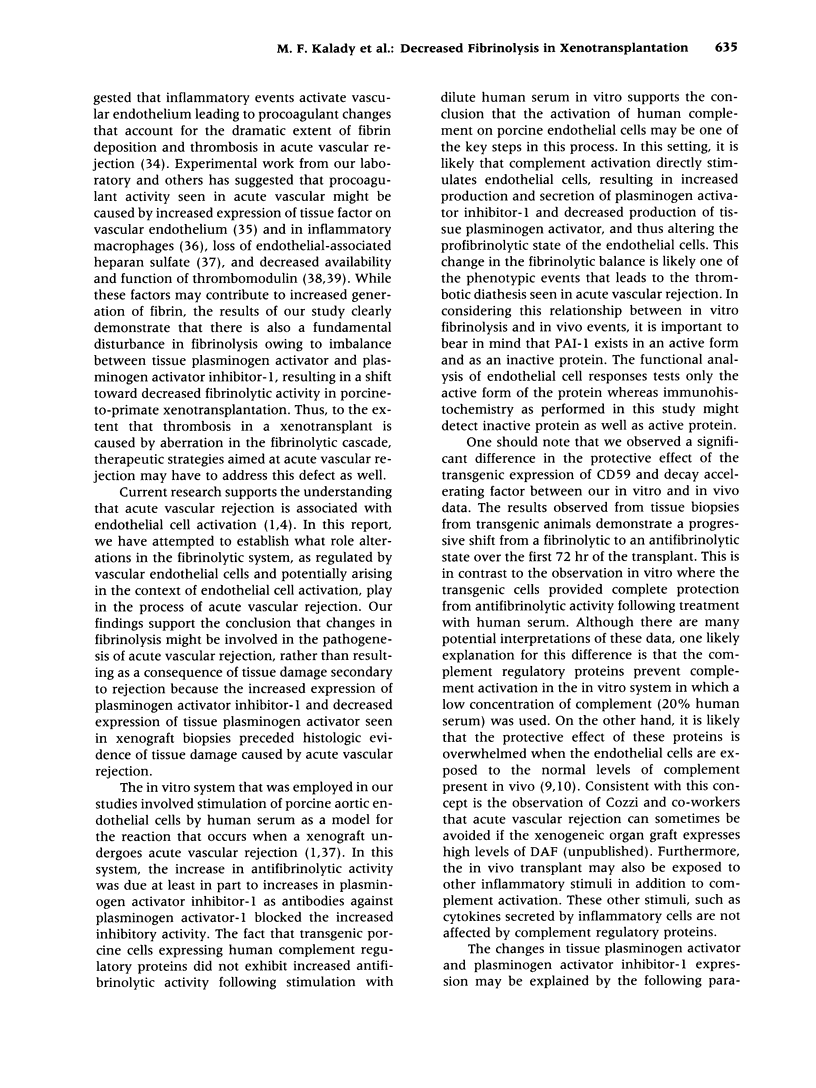
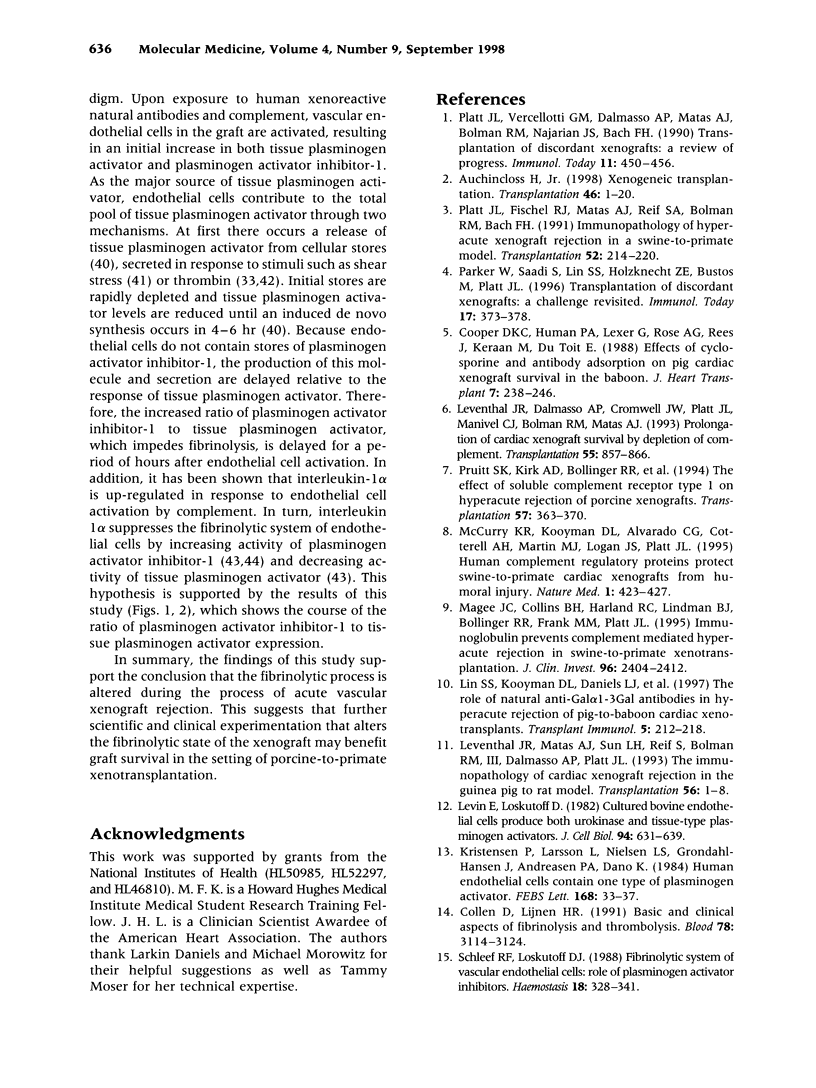
BACKGROUND: One major barrier to successful xenotransplantation is acute vascular rejection, a process pathologically characterized by microvascular thrombosis and diffuse fibrin deposition in transplant blood vessels. This pathologic picture may result from a disturbance in the coagulant or fibrinolytic pathways that regulate normal vascular patency. This study evaluated the regulation of fibrinolytic activity defined by tissue plasminogen activator and plasminogen activator inhibitor-1 as it may exist in the setting of acute vascular rejection. MATERIALS AND METHODS, RESULTS: Serial biopsies from cardiac xenotransplants evaluated by immunofluorescence microscopy demonstrated progressive decreases in tissue plasminogen activator and increases in plasminogen activator inhibitor-1. In vitro studies measuring fibrinolytic activity of cell culture medium from porcine aortic endothelial cells stimulated with human serum or autologous porcine serum revealed that human serum triggered as much as 93% increase in antifibrinolytic activity. CONCLUSIONS: These findings demonstrate that porcine vascular endothelial cells change toward an antifibrinolytic state following stimulation with human xenoreactive antibodies and complement. The shift is at least partly explained by an increased ratio of plasminogen activator inhibitor-1 to tissue plasminogen activator, and is at least in part mediated by the activation of complement. This increased antifibrinolytic activity may contribute to the thrombotic diathesis seen in acute vascular rejection in pig-to-primate xenografts.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Auchincloss H., Jr Xenogeneic transplantation. A review. Transplantation. 1988 Jul;46(1):1–20. doi: 10.1097/00007890-198807000-00001. [DOI] [PubMed] [Google Scholar]
- Aznar J., Estellés A., Tormo G., Sapena P., Tormo V., Blanch S., España F. Plasminogen activator inhibitor activity and other fibrinolytic variables in patients with coronary artery disease. Br Heart J. 1988 May;59(5):535–541. doi: 10.1136/hrt.59.5.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth N. A., Bennett B., Wijngaards G., Grieve J. H. A new life-long hemorrhagic disorder due to excess plasminogen activator. Blood. 1983 Feb;61(2):267–275. [PubMed] [Google Scholar]
- Byrne G. W., McCurry K. R., Martin M. J., McClellan S. M., Platt J. L., Logan J. S. Transgenic pigs expressing human CD59 and decay-accelerating factor produce an intrinsic barrier to complement-mediated damage. Transplantation. 1997 Jan 15;63(1):149–155. doi: 10.1097/00007890-199701150-00027. [DOI] [PubMed] [Google Scholar]
- Collen D., Lijnen H. R. Basic and clinical aspects of fibrinolysis and thrombolysis. Blood. 1991 Dec 15;78(12):3114–3124. [PubMed] [Google Scholar]
- Cooper D. K., Human P. A., Lexer G., Rose A. G., Rees J., Keraan M., Du Toit E. Effects of cyclosporine and antibody adsorption on pig cardiac xenograft survival in the baboon. J Heart Transplant. 1988 May-Jun;7(3):238–246. [PubMed] [Google Scholar]
- Diamond S. L., Eskin S. G., McIntire L. V. Fluid flow stimulates tissue plasminogen activator secretion by cultured human endothelial cells. Science. 1989 Mar 17;243(4897):1483–1485. doi: 10.1126/science.2467379. [DOI] [PubMed] [Google Scholar]
- Emeis J. J., Kooistra T. Interleukin 1 and lipopolysaccharide induce an inhibitor of tissue-type plasminogen activator in vivo and in cultured endothelial cells. J Exp Med. 1986 May 1;163(5):1260–1266. doi: 10.1084/jem.163.5.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamsten A., Wiman B., de Faire U., Blombäck M. Increased plasma levels of a rapid inhibitor of tissue plasminogen activator in young survivors of myocardial infarction. N Engl J Med. 1985 Dec 19;313(25):1557–1563. doi: 10.1056/NEJM198512193132501. [DOI] [PubMed] [Google Scholar]
- Hanss M., Collen D. Secretion of tissue-type plasminogen activator and plasminogen activator inhibitor by cultured human endothelial cells: modulation by thrombin, endotoxin, and histamine. J Lab Clin Med. 1987 Jan;109(1):97–104. [PubMed] [Google Scholar]
- Kristensen P., Larsson L. I., Nielsen L. S., Grøndahl-Hansen J., Andreasen P. A., Danø K. Human endothelial cells contain one type of plasminogen activator. FEBS Lett. 1984 Mar 12;168(1):33–37. doi: 10.1016/0014-5793(84)80201-x. [DOI] [PubMed] [Google Scholar]
- Labarrere C. A., Pitts D., Nelson D. R., Faulk W. P. Vascular tissue plasminogen activator and the development of coronary artery disease in heart-transplant recipients. N Engl J Med. 1995 Oct 26;333(17):1111–1116. doi: 10.1056/NEJM199510263331704. [DOI] [PubMed] [Google Scholar]
- Lawson J. H., Daniels L. J., Platt J. L. The evaluation of thrombomodulin activity in porcine to human xenotransplantation. Transplant Proc. 1997 Feb-Mar;29(1-2):884–885. doi: 10.1016/s0041-1345(96)00192-3. [DOI] [PubMed] [Google Scholar]
- Lawson J. H., Platt J. L. Molecular barriers to xenotransplantation. Transplantation. 1996 Aug 15;62(3):303–310. doi: 10.1097/00007890-199608150-00001. [DOI] [PubMed] [Google Scholar]
- Leventhal J. R., Dalmasso A. P., Cromwell J. W., Platt J. L., Manivel C. J., Bolman R. M., 3rd, Matas A. J. Prolongation of cardiac xenograft survival by depletion of complement. Transplantation. 1993 Apr;55(4):857–866. doi: 10.1097/00007890-199304000-00033. [DOI] [PubMed] [Google Scholar]
- Leventhal J. R., Matas A. J., Sun L. H., Reif S., Bolman R. M., 3rd, Dalmasso A. P., Platt J. L. The immunopathology of cardiac xenograft rejection in the guinea pig-to-rat model. Transplantation. 1993 Jul;56(1):1–8. doi: 10.1097/00007890-199307000-00001. [DOI] [PubMed] [Google Scholar]
- Levin E. G., Loskutoff D. J. Cultured bovine endothelial cells produce both urokinase and tissue-type plasminogen activators. J Cell Biol. 1982 Sep;94(3):631–636. doi: 10.1083/jcb.94.3.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin E. G., Marzec U., Anderson J., Harker L. A. Thrombin stimulates tissue plasminogen activator release from cultured human endothelial cells. J Clin Invest. 1984 Dec;74(6):1988–1995. doi: 10.1172/JCI111620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lijnen H. R., Collen D. Endothelium in hemostasis and thrombosis. Prog Cardiovasc Dis. 1997 Jan-Feb;39(4):343–350. doi: 10.1016/s0033-0620(97)80032-1. [DOI] [PubMed] [Google Scholar]
- Lin S. S., Kooyman D. L., Daniels L. J., Daggett C. W., Parker W., Lawson J. H., Hoopes C. W., Gullotto C., Li L., Birch P. The role of natural anti-Gal alpha 1-3Gal antibodies in hyperacute rejection of pig-to-baboon cardiac xenotransplants. Transpl Immunol. 1997 Sep;5(3):212–218. doi: 10.1016/s0966-3274(97)80040-8. [DOI] [PubMed] [Google Scholar]
- Magee J. C., Collins B. H., Harland R. C., Lindman B. J., Bollinger R. R., Frank M. M., Platt J. L. Immunoglobulin prevents complement-mediated hyperacute rejection in swine-to-primate xenotransplantation. J Clin Invest. 1995 Nov;96(5):2404–2412. doi: 10.1172/JCI118297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurry K. R., Kooyman D. L., Alvarado C. G., Cotterell A. H., Martin M. J., Logan J. S., Platt J. L. Human complement regulatory proteins protect swine-to-primate cardiac xenografts from humoral injury. Nat Med. 1995 May;1(5):423–427. doi: 10.1038/nm0595-423. [DOI] [PubMed] [Google Scholar]
- Moore K. L., Andreoli S. P., Esmon N. L., Esmon C. T., Bang N. U. Endotoxin enhances tissue factor and suppresses thrombomodulin expression of human vascular endothelium in vitro. J Clin Invest. 1987 Jan;79(1):124–130. doi: 10.1172/JCI112772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson I. M., Ljungnér H., Tengborn L. Two different mechanisms in patients with venous thrombosis and defective fibrinolysis: low concentration of plasminogen activator or increased concentration of plasminogen activator inhibitor. Br Med J (Clin Res Ed) 1985 May 18;290(6480):1453–1456. doi: 10.1136/bmj.290.6480.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker W., Saadi S., Lin S. S., Holzknecht Z. E., Bustos M., Platt J. L. Transplantation of discordant xenografts: a challenge revisited. Immunol Today. 1996 Aug;17(8):373–378. doi: 10.1016/0167-5699(96)10028-1. [DOI] [PubMed] [Google Scholar]
- Platt J. L., Fischel R. J., Matas A. J., Reif S. A., Bolman R. M., Bach F. H. Immunopathology of hyperacute xenograft rejection in a swine-to-primate model. Transplantation. 1991 Aug;52(2):214–220. doi: 10.1097/00007890-199108000-00006. [DOI] [PubMed] [Google Scholar]
- Platt J. L., LeBien T. W., Michael A. F. Interstitial mononuclear cell populations in renal graft rejection. Identification by monoclonal antibodies in tissue sections. J Exp Med. 1982 Jan 1;155(1):17–30. doi: 10.1084/jem.155.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt J. L., Vercellotti G. M., Dalmasso A. P., Matas A. J., Bolman R. M., Najarian J. S., Bach F. H. Transplantation of discordant xenografts: a review of progress. Immunol Today. 1990 Dec;11(12):450–457. doi: 10.1016/0167-5699(90)90174-8. [DOI] [PubMed] [Google Scholar]
- Platt J. L., Vercellotti G. M., Lindman B. J., Oegema T. R., Jr, Bach F. H., Dalmasso A. P. Release of heparan sulfate from endothelial cells. Implications for pathogenesis of hyperacute rejection. J Exp Med. 1990 Apr 1;171(4):1363–1368. doi: 10.1084/jem.171.4.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruitt S. K., Kirk A. D., Bollinger R. R., Marsh H. C., Jr, Collins B. H., Levin J. L., Mault J. R., Heinle J. S., Ibrahim S., Rudolph A. R. The effect of soluble complement receptor type 1 on hyperacute rejection of porcine xenografts. Transplantation. 1994 Feb;57(3):363–370. doi: 10.1097/00007890-199402150-00009. [DOI] [PubMed] [Google Scholar]
- Saadi S., Holzknecht R. A., Patte C. P., Stern D. M., Platt J. L. Complement-mediated regulation of tissue factor activity in endothelium. J Exp Med. 1995 Dec 1;182(6):1807–1814. doi: 10.1084/jem.182.6.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleef R. R., Bevilacqua M. P., Sawdey M., Gimbrone M. A., Jr, Loskutoff D. J. Cytokine activation of vascular endothelium. Effects on tissue-type plasminogen activator and type 1 plasminogen activator inhibitor. J Biol Chem. 1988 Apr 25;263(12):5797–5803. [PubMed] [Google Scholar]
- Schleef R. R., Loskutoff D. J. Fibrinolytic system of vascular endothelial cells. Role of plasminogen activator inhibitors. Haemostasis. 1988;18(4-6):328–341. doi: 10.1159/000215815. [DOI] [PubMed] [Google Scholar]
- Soeda S., Kakiki M., Shimeno H., Nagamatsu A. Rapid and high-yield purification of porcine heart tissue-type plasminogen activator by heparin-sepharose choromatography. Life Sci. 1986 Oct 13;39(15):1317–1324. doi: 10.1016/0024-3205(86)90329-2. [DOI] [PubMed] [Google Scholar]
- Sprengers E. D., Kluft C. Plasminogen activator inhibitors. Blood. 1987 Feb;69(2):381–387. [PubMed] [Google Scholar]
- Wiman B., Ljungberg B., Chmielewska J., Urdén G., Blombäck M., Johnsson H. The role of the fibrinolytic system in deep vein thrombosis. J Lab Clin Med. 1985 Feb;105(2):265–270. [PubMed] [Google Scholar]
- van Hinsbergh V. W., Kooistra T., Emeis J. J., Koolwijk P. Regulation of plasminogen activator production by endothelial cells: role in fibrinolysis and local proteolysis. Int J Radiat Biol. 1991 Jul-Aug;60(1-2):261–272. doi: 10.1080/09553009114551981. [DOI] [PubMed] [Google Scholar]