Abstract
Gustducin, a transducin-like guanine nucleotide-binding regulatory protein (G protein), and transducin are expressed in taste receptor cells where they are thought to mediate taste transduction. Gustducin and transducin are activated in the presence of bovine taste membranes by several compounds that humans perceive to be bitter. We have monitored this activation with an in vitro assay to identify compounds that inhibited taste receptor activation of transducin by bitter tastants: AMP and chemically related compounds inhibited in vitro responses to several bitter compounds (e.g., denatonium, quinine, strychnine, and atropine). AMP also inhibited behavioral and electrophysiological responses of mice to bitter tastants, but not to NaCl, HCl, or sucrose. GMP, although chemically similar to AMP, inhibited neither the bitter-responsive taste receptor activation of transducin nor the gustatory responses of mice to bitter compounds. AMP and certain related compounds may bind to bitter-responsive taste receptors or interfere with receptor-G protein coupling to serve as naturally occurring taste modifiers.
The taste of quinine and denatonium benzoate (perceived by humans as intensely bitter) is thought to be transduced via seven transmembrane-helix receptors coupled to heterotrimeric guanine nucleotide-binding proteins (G proteins) (reviewed in refs. 1 and 2). Gustducin, a transducin-like G protein, and transducin itself are expressed in taste receptor cells (3, 4). Gustducin-null mice and transgenic mice expressing a mutated form of gustducin that disrupts signal transduction have dramatically diminished responsiveness to compounds that humans characterize as bitter or sweet, implicating gustducin in the transduction of these taste qualities (refs. 5, 6; L. Ruiz-Avila, G. T. Wong, and R.F.M., unpublished observations). Gustducin and transducin can be activated in vitro by several bitter tastants in the presence of apparent taste receptor activities present in taste receptor cell membranes (4, 6). We reasoned that this in vitro assay could be used to identify compounds that would function in vivo as bitter antagonists and flavor modifiers. In the present work, we describe our initial results using this assay to identify such compounds.
MATERIALS AND METHODS
G Protein Activation Assays.
Bovine (Bos primigenius) tongues were collected fresh from a local slaughterhouse and transported on ice to the laboratory. Circumvallate papillae were hand dissected, frozen in liquid nitrogen, and stored at −80°C until use. The collected taste tissues were homogenized, particulates removed by centrifugation, and enriched taste cell membranes collected as described (6). The pelleted membranes were rinsed twice, resuspended in homogenization buffer lacking protease inhibitors, and further homogenized by 20 passages through a 25-gauge needle. Aliquots were either flash frozen or stored on ice until use. The concentration of protein in the membrane preparations was determined by the Peterson modification of the micro-Lowry method (7). Activation of transducin was based on the published trypsin sensitivity procedure (6, 8). After the trypsin digestion, samples were diluted with Laemmli buffer (9) and separated by SDS/PAGE by using a 4–20% gel and Tris–glycine buffer. The separated polypeptides were transferred by electro-blotter to a poly(vinylidene difluoride) membrane, which was blocked by the addition of 5% BLOTTO [50 mM Tris⋅HCl, pH 7.4/100 mM NaCl/5% nonfat dry milk], (30 min), then transducin peptides were visualized by binding of transducin antiserum and horseradish peroxidase-labeled goat anti-rabbit secondary antibody, followed by developing with bicinchoninic acid staining reagents from Bio-Rad and exposure to x-ray film.
All bitter tastant and buffer chemicals were of the highest purity available and were purchased either from Sigma or Boehringer Mannheim, unless otherwise noted. Rhodopsin was purified in the light as 6 M urea-washed bovine rod outer segments by using published procedures (10). Bovine transducin heterotrimer was purified by standard procedures (11). The rabbit polyclonal antitransducin antibody was a kind gift of Mel Simon and John Watson (California Institute of Technology, Pasadena, CA).
Behavioral Assays.
Multiple sets of male C57BL/6J mice from the Jackson Laboratory were tested. Each set (n = 10) was tested with tastant ± AMP or GMP. Between tests, mice were provided with acidified water (pH 4.5) for about 2 wk. Tested mice ranged in age from 8 to 20 wk. Mice were individually housed, provided with food ad libitum (Pico Lab Mouse Diet 20 no. 5058; PMI Feeds, St. Louis, MO) and presented with distilled water in two sipper bottles for 48 h before testing. During each 48-h test period, a given concentration of tastant was provided in one sipper bottle, whereas the other had distilled water. After 24 h, volumes consumed were recorded, the bottles refilled, and positions reversed (to control for positional cues). Tastants were presented in ascending concentration. Preference ratios were calculated as the fraction of tastant consumed as a percentage of the total volume of liquid consumed. Mean preference ratios and Student’s t tests were calculated from total collected data.
Nerve Recording.
Glossopharyngeal nerve responses were recorded from male C57BL/6J mice as previously described (12). Each mouse was anesthetized with intraperitoneal injection of sodium pentobarbital (40–50 mg/kg) and maintained at a surgical level of anesthesia with supplemental injections of the drug. The trachea was cannulated, and the mouse was then fixed in the supine position with a head holder to allow dissection of the glossopharyngeal nerve. The hypoglossal nerve was transected bilaterally to prevent inadvertent tongue movements. The right glossopharyngeal nerve was exposed by removal of the digastric muscle and posterior horn of the hyoid bone. The glossopharyngeal nerve was then dissected free from underlying tissues and cut near its entrance to the posterior foramen lacerum. The entire nerve was placed on a silver wire electrode for whole nerve recording. An indifferent electrode was positioned nearby in the wound. Neural responses resulting from topical application of tastants to the tongue were fed into an amplifier and displayed on an oscilloscope screen. Whole nerve responses were integrated by using an RMS-DC converter (Hendrick, Tallahassee, FL) with a time constant of 0.5 s. For chemical stimulation of the circumvallate and foliate papillae, an incision was made on each side of the animal’s face from the corner of the mouth to just above the angle of the jaw, the papillae were exposed, and their trenches opened via slight tension applied through a small suture sewn in the tip of the tongue. Tastant solutions were delivered to the tongue by gravity flow, and flowed over the tongue for a controlled period. The stability of each preparation was monitored by the periodic application of 0.1 M NH4Cl. A recording was considered to be stable when the 0.1 M NH4Cl response magnitudes at the beginning and end of each stimulation series deviated by no more than 15%. Only responses from stable recordings were used in the data analysis. In the analysis of whole nerve responses, the magnitudes of the integrated response at 20, 25, 30, 35, and 40 s after stimulus onset were measured and averaged to generate tonic responses: the tonic response represents the sustained nerve response to continuous tastant stimulation of taste receptor cells. The relative tonic response for each stimulus was obtained by normalization to the response from 0.1 M NH4Cl (the tonic response of NH4Cl was defined as 1.0). Student’s t test was used for statistical analysis.
RESULTS
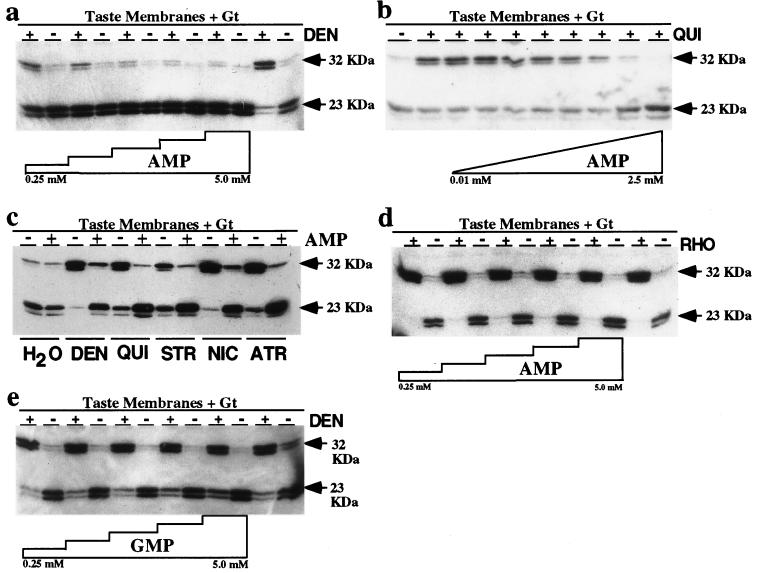
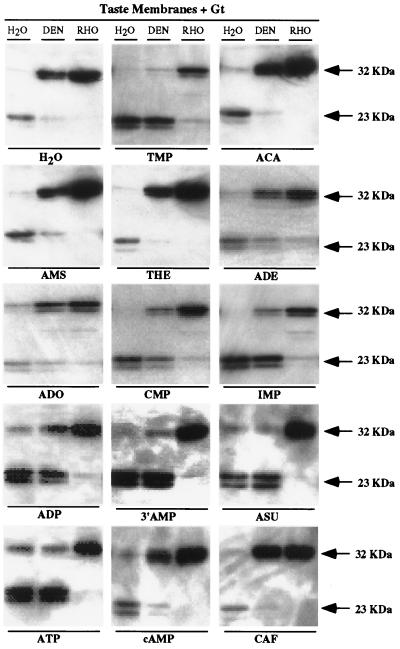
The active (GTP-bound) form of G proteins such as gustducin and transducin can be distinguished from the inactive (GDP-bound) form by limited trypsin digestion (13, 14). Using transducin as a reporter in this in vitro assay, we identified compounds that inhibited gustatory responses to bitter compounds. Taste membrane activation of transducin by the bitter compounds denatonium benzoate (DEN) and quinine hydrochloride (QUI) was inhibited in a dose-dependent fashion by AMP (Fig. 1 a and b). The inhibitory effect of AMP generalized to every bitter compound that activated transducin in the presence of taste membranes: DEN, QUI, strychnine, nicotine, atropine (Fig. 1c), sparteine, naringin, caffeic acid, and quinacrine (data not shown). The inhibitory effect of AMP was specific and required taste receptors, because AMP did not inhibit rhodopsin-mediated activation of transducin (Fig. 1d). GMP did not inhibit taste membrane activation of transducin in response to DEN (Fig. 1e) or other bitter tastants (data not shown), suggesting specificity of binding. Several AMP-related compounds potently inhibited DEN/taste receptor activation of transducin: thymidine 5′-monophosphate, ADP, 3′AMP, adenosine 5′-succinate, ATP (Fig. 2), and adenosine 2′-monophosphate (data not shown). 5′-Cytidylic acid, and inosinic acid partially inhibited DEN/taste membrane activation of transducin (Fig. 2). As with GMP (Fig. 1e), adenosine 5′-carboxylate, adenosine 5′-monosulfate, theophylline, adenine, adenosine, cAMP, and caffeine did not block activation of transducin by DEN-stimulated taste membranes (Fig. 2).
Figure 1.
AMP inhibits activation of transducin by bitter stimuli in the presence of bovine taste receptor cell membranes. (a) Inactive (GDP-bound) transducin (rightmost lane) generates a 23 kDa fragment on digestion with trypsin. Active (GTPγS-bound) transducin (second from right lane) activated by DEN plus taste membranes generates a 32-kDa fragment on treatment with trypsin. Increasing concentrations of AMP (0.25, 0.5, 1.25, 2.5, and 5.0 mM) inhibit activation of transducin by DEN plus bovine taste receptor membranes, as determined by the shift from 32-kDa to 23-kDa fragments. (b) Increasing concentrations of AMP (0.01, 0.05, 0.10, 0.50, 1.0, 1.5, 2.0, and 2.5 mM) inhibit activation of transducin by 1.0 mM QUI plus bovine taste membranes. (c) AMP (2.5 mM) inhibits the taste membrane-dependent activation of transducin by DEN (5.0 mM), QUI (1.0 mM), strychnine hydrochloride (STR, 5.0 mM), nicotine hemisulfate (NIC, 5.0 mM), and atropine hydrochloride (ATR, 5.0 mM). (d) AMP (0.25, 0.5, 1.25, 2.5, and 5.0 mM) does not inhibit activation of transducin by 0.001 mM rhodopsin. (e) GMP (0.25. 0.5, 1.25, 2.5, and 5.0 mM) does not inhibit activation of transducin by DEN (5.0 mM) plus bovine taste membranes.
Figure 2.
Only certain AMP analogues block activation of transducin by DEN plus taste membranes. Taste membrane-dependent activation of transducin by DEN (5.0 mM) is not inhibited by adenosine 5′-carboxylate (ACA, 5.0 mM), adenosine 5′-monosulfate (AMS, 5.0 mM), theophylline (THE, 5.0 mM), adenine hydrochloride (ADE, 5.0 mM), adenosine hydrochloride (ADO, 5.0 mM), cAMP (5.0 mM), or caffeine (CAF, 5.0 mM). DEN/taste membrane activation of transducin is inhibited by thymidine 5′-monophosphate (TMP, 5.0 mM), 5′-cytidylic acid (CMP, 5.0 mM), inosinic acid (IMP, 5.0 mM), ADP (5.0 mM), 3′AMP (5.0 mM), adenosine 5′-succinate (ASU, 5.0 mM) and ATP (5.0 mM). H2O and rhodopsin (RHO) lanes control for nonspecific receptor-independent effects.
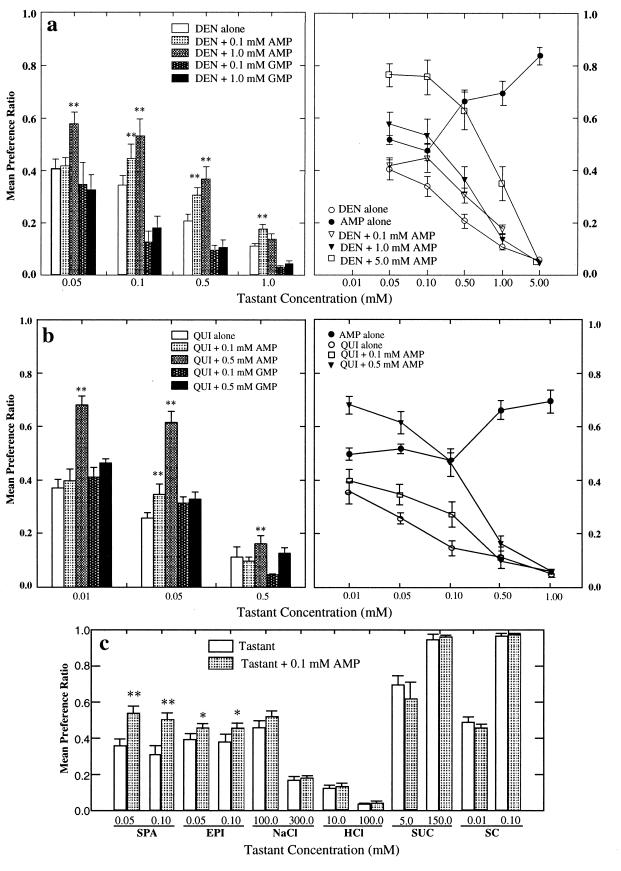
To determine whether AMP, as distinct from GMP, would diminish the gustatory responses to bitter compounds, two-bottle preference tests (15) were carried out on mice presented with various tastants ± AMP or GMP. AMP, but not GMP, inhibited the aversive responses of mice to DEN (Fig. 3a) and QUI (Fig. 3b). The inhibitory effect of AMP gradually decreased as the concentration of bitter tastant increased and was eliminated at the highest concentrations of DEN and QUI tested (5.0 and 1.0 mM, respectively) (Fig. 3 a and b). Several other tastants that humans characterize as bitter [sparteine and (−)-epicatechin (16)], sweet [sucrose and the high-potency artificial sweetener SC45647 (17)], sour (HCl), or salty (NaCl) were also tested ± AMP. AMP inhibited the aversive responses to the two bitter compounds, sparteine and epicatechin, but did not affect the behavioral responses to sucrose, SC45647, NaCl, or HCl (Fig. 3c).
Figure 3.
AMP blocks aversive responses of mice to several bitter compounds. (a) (Left) Forty-eight-hour two-bottle preference responses of C57BL/6J mice (n = 10) to DEN alone, AMP alone, DEN plus AMP (0.1 and 1.0 mM), and DEN plus GMP (0.1 and 1.0 mM). AMP (0.1 and 1.0 mM) inhibited the aversive responses to DEN at 0.05, 0.10, 0.50, and 1.0 mM (P < 0.001). GMP (0.1 and 1.0 mM) did not inhibit the aversive responses to DEN. **P < 0.001. Right: increasing concentrations of AMP (0.1, 1.0, 5.0 mM) shifted the dose-aversiveness curve to the right. AMP alone did not elicit behavioral responses until its concentration reached 0.5 mM. (b) (Left) Preference responses of C57BL/6J mice (n = 10) to QUI alone, AMP alone, QUI plus AMP (0.1 and 0.5 mM), and QUI plus GMP (0.1 and 0.5 mM). AMP (0.1 and 0.5 mM) inhibited the aversive responses to QUI at 0.05, 0.10, and 0.50 mM (P < 0.001). GMP (0.1 and 0.5 mM) did not inhibit the aversive responses to QUI. **P < 0.001. (Right) Increasing concentrations of AMP shifted the dose-aversiveness curve to the right. (c) Preference responses of C57BL/6J mice (n = 10) exposed to two different concentrations of tastants ± 0.1 mM AMP. AMP inhibited the aversive responses to the bitter tastants sparteine (SPA) at 0.05 and 0.10 mM (P < 0.001); and (−)-epicatechin (EPI) at 0.05 mM and 0.10 mM (P < 0.01). AMP did not alter the behavioral responses to NaCl (0.1 and 0.3 M), HCl (0.01 and 0.10 mM), sucrose (SUC) (5.0 and 150 mM), or the high-potency artificial sweetener SC45647 (SC) (0.01 and 0.10 mM). **P < 0.001; *P < 0.01.
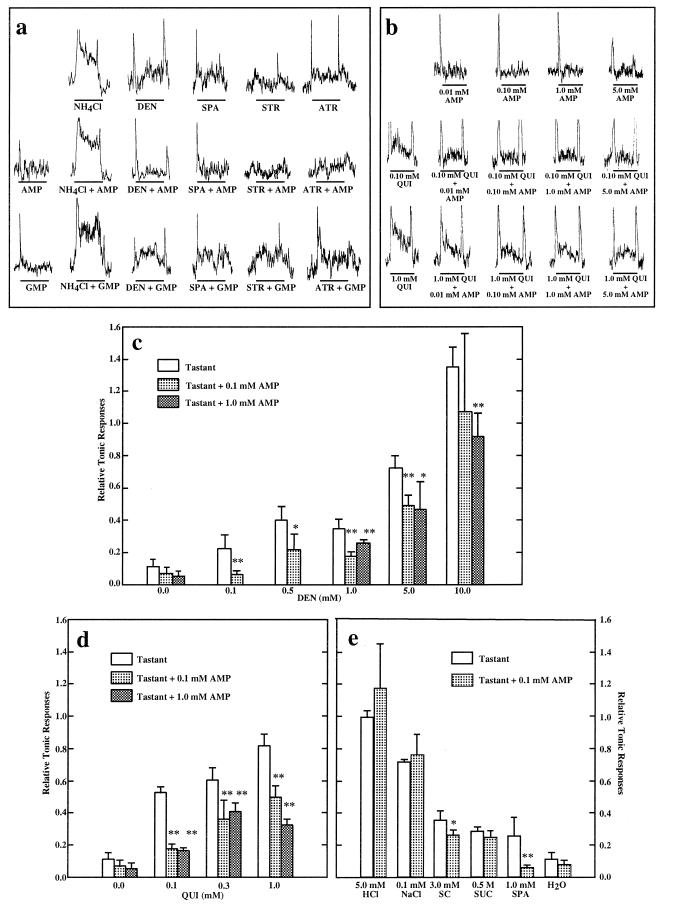
To determine whether the inhibition of aversive responses to bitter compounds by AMP was because of peripheral taste inhibition (as predicted by the biochemical data of Figs. 1 and 2) we recorded summated glossopharyngeal nerve responses of mice (12) to various tastants ± AMP or GMP. The glossopharyngeal nerve innervates taste receptor cells of the posterior tongue and in mice is responsive to salty, sweet, sour, and bitter stimuli (18). AMP (0.1 mM) significantly inhibited the nerve responses to DEN, QUI, sparteine, strychnine, and atropine (Fig. 4 a and b). GMP (0.1 mM) had no effect on the glossopharyngeal responses to any of these bitter compounds (Fig. 4a and data not shown). The glossopharyngeal responses increased as QUI or DEN concentrations were raised: AMP (0.1 and 1.0 mM) significantly inhibited these nerve responses (Fig. 4 b–d). In contrast, AMP did not affect the nerve responses to NH4Cl, HCl, NaCl, or sucrose (Fig. 4e), consistent with the behavioral responses. Interestingly, although AMP inhibited slightly the glossopharyngeal responses to the artificial sweetener SC45647 (Fig. 4e), it did not diminish the behavioral responses to this compound (Fig. 3c).
Figure 4.
AMP diminishes the glossopharyngeal nerve responses of mice to lingual stimulation with bitter tastants. (a) (Top) Glossopharyngeal responses to 0.1 M NH4Cl, 5.0 mM DEN, 1.0 mM sparteine (SPA), 1.0 mM strychnine (STR), and 1.0 mM atropine (ATR). (Middle) Glossopharyngeal responses to the above compounds mixed with 0.1 mM AMP. (Bottom) Glossopharyngeal responses to the above compounds mixed with 0.1 mM GMP. (b) Glossopharyngeal responses to a series of concentrations of AMP (0.01, 0.1, 1.0, 5.0 mM) alone (Top), and in combination with QUI (0.1 mM and 1.0 mM) (Middle and Bottom, respectively). (c) Relative tonic responses recorded from glossopharyngeal nerves of mice (n = 5 to 7) stimulated by lingual application of DEN (0.1, 0.5, 1.0, 5.0, and 10.0 mM) ± AMP (0.1 and 1.0 mM). **P < 0.001; *P < 0.01. (d) Relative tonic responses recorded from glossopharyngeal nerves of mice (n = 6 to 8) stimulated by lingual application of QUI (0.1, 0.3, and 1.0 mM) and its mixtures with AMP (0.1 and 1.0 mM). **P < 0.001. (e) Relative tonic responses recorded from glossopharyngeal nerves of mice (n = 4 to 7) stimulated by lingual application of 5.0 mM HCl, 0.1 M NaCl, 3.0 mM SC45647, 0.5 M sucrose (SUC), 1.0 mM SPA, or water with or without 0.1 mM AMP. AMP inhibits the relative tonic responses of 1.0 mM SPA (P < 0.001) and 3.0 mM SC45647 (P < 0.01), but not of the other compounds. **P < 0.001; *P < 0.01.
DISCUSSION
AMP and closely related compounds inhibited in vitro activation of transducin by taste membranes plus DEN, QUI, and several other bitter compounds. This effect was specific to the bitter-responsive heptahelical receptors presumably present in taste membranes and was not caused by nonspecific or general activation of rhodopsin-like receptors. AMP and like compounds also blocked behavioral and gustatory nerve responses to DEN, QUI, and other bitter compounds, but did not affect responses to NaCl, HCl, or sucrose. AMP did diminish glossopharyngeal responses to the high-potency sweetener SC45647, although it did not affect behavioral responses to this compound. AMP, ADP, ATP, thymidine 5′-monophosphate, 5′-cytidylic acid, and inosinic acid all inhibited in vitro taste receptor responses, whereas GMP did not, indicating selectivity in the binding of these compounds; more refined structure–activity relationship analysis may aid in determining the basis for these differences and the structure of the target’s binding pocket. The rapidity of AMP’s actions in the electrophysiological assays argues against an intracellular site of action and suggests that AMP is probably acting at a cell-surface receptor. However, the present data do not distinguish between competitive or noncompetitive modes of action of AMP at the receptor.
High concentrations of DEN, QUI, and other bitter tastants overcame AMP’s inhibition of aversive responses, suggesting either that AMP is acting as a competitive inhibitor or that the bitter tastants activated other AMP-resistant bitter transduction pathways in addition to gustducin/transducin-mediated pathways, consistent with residual responsiveness to bitter compounds in gustducin knockout and transgenic mice expressing a mutated form of gustducin that disrupts signal transduction (refs. 5 and 6; L. Ruiz-Avila, G. T. Wong, and R.F.M., unpublished observations). The existence of multiple bitter transduction pathways is also supported by the observation that inhibition by AMP of glossopharyngeal responses to increasing concentrations of QUI reached a plateau at which glossopharyngeal responses to QUI could not be reduced further.
In recent studies (D.M. and R.F.M., unpublished work), we have determined that certain artificial sweeteners inhibit in vitro activation of taste receptors by DEN, QUI, and other bitter compounds; these sweeteners also inhibited behavioral and gustatory nerve responses to these gustducin/transducin coupled bitter compounds. This phenomenon of sweet-bitter “mixture suppression” (19, 20) may be explained in part by antagonistic binding of sweeteners to the same receptor targets that bind bitter compounds and may relate to previous observations of chemical similarities of high-potency sweeteners and high-potency bitter compounds (21–23).
Multiple lines of evidence implicate gustducin/transducin, their coupled receptors, and effector enzymes (e.g., phosphodiesterases and phospholipase C) in bitter transduction (reviewed in refs. 1 and 2). In addition to gustducin and transducin, the G proteins Gs, Gi3, and G14 are also present in taste receptor cells (1, 3) and may be involved in taste transduction. Biochemical and electrophysiological studies implicate cyclic nucleotides, inositol trisphosphate, diacyl glycerol, and Ca2+ as second messengers in bitter and/or sweet taste transduction (24–28). Biochemical and genetic data clearly implicate gustducin in the transduction of both bitter and sweet taste qualities: (i) gustducin null mice have markedly diminished behavioral and gustatory nerve responses to both bitter and sweet compounds (5); (ii) a mutated form of gustducin disrupted in its interactions with receptors acts as a dominant negative to block both bitter and sweet responsiveness in vivo (L. Ruiz-Avila, G. T. Wong, and R.F.M., unpublished observations); (iii) in vitro studies demonstrate that bovine taste receptor-containing membranes and solubilized taste receptors activate gustducin/transducin in the presence of DEN, QUI, and several other bitter compounds (6); (iv) although sweet compounds do not activate gustducin/transducin in this assay, our recent data (D.M. and R.F.M., unpublished work) demonstrate that certain sweeteners block in vitro activation of gustducin/transducin and thereby lead to sweet-bitter “mixture suppression.”
Although biochemical and genetic studies of taste G proteins have provided new insights into the molecular nature of the sweet and bitter transduction cascades, physical studies of the taste receptors involved in bitter and sweet transduction (29, 30) have been of limited utility because of the scarcity of material and the lack of high-affinity ligands. Typical naturally occurring bitter and sweet tastants are active in the range of 10–500 mM, whereas the most potent sweet or bitter tastants have thresholds for detection of 10–100 nM. The likelihood of receptor families and multiple independent pathways further compounds the difficulties of characterizing taste receptors. Structure-activity relationship analyses of high-potency sweeteners have led to working models of the physical nature of the receptor’s binding pocket (reviewed in refs. 31, 32); however, these approaches are severely limited by the possibility of receptor heterogeneity and multiple independent pathways for sweetener function. The approach we have presented may have utility for identifying specific subtypes of bitter receptors and naturally occurring and synthetic compounds that act as selective blockers of bitter taste.
Acknowledgments
R.F.M. is an Associate Investigator of the Howard Hughes Medical Institute. This research was supported by National Institutes of Health Grants RO1DC03055 and RO1DC3155 (R.F.M.).
ABBREVIATIONS
- DEN
denatonium benzoate
- QUI
quinine hydrochloride
References
- 1.Kinnamon S C, Margolskee R F. Curr Opin Neurobiol. 1996;6:506–513. doi: 10.1016/s0959-4388(96)80057-2. [DOI] [PubMed] [Google Scholar]
- 2.Lindemann B. Physiol Rev. 1996;76:719–766. doi: 10.1152/physrev.1996.76.3.719. [DOI] [PubMed] [Google Scholar]
- 3.McLaughlin S K, McKinnon P J, Margolskee R F. Nature (London) 1992;357:563–569. doi: 10.1038/357563a0. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Avila L, McLaughlin S K, Wildman D, McKinnon P J, Robichon A, Spickofsky N, Margolskee R F. Nature (London) 1995;376:80–85. doi: 10.1038/376080a0. [DOI] [PubMed] [Google Scholar]
- 5.Wong G T, Gannon K S, Margolskee R F. Nature (London) 1996;381:796–800. doi: 10.1038/381796a0. [DOI] [PubMed] [Google Scholar]
- 6.Ming D, Ruiz-Avila L, Margolskee R F. Proc Natl Acad Sci USA. 1998;95:8933–8938. doi: 10.1073/pnas.95.15.8933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peterson G L. Anal Biochem. 1977;83:346–356. doi: 10.1016/0003-2697(77)90043-4. [DOI] [PubMed] [Google Scholar]
- 8.Neer E J, Denker B M, Thomas T C, Schmidt C J. Methods Enzymol. 1994;237:226–239. doi: 10.1016/s0076-6879(94)37065-6. [DOI] [PubMed] [Google Scholar]
- 9.Laemmli U K. Nature (London) 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 10.Mazzoni M R, Malinski J A, Hamm H E. J Biol Chem. 1991;266:14072–14081. [PubMed] [Google Scholar]
- 11.Fung B K-K, Hurley J B, Stryer L. Proc Natl Acad Sci USA. 1981;78:152–156. doi: 10.1073/pnas.78.1.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ninomiya Y, Inoue M, Imoto T, Nakashima K. Am J Physiol (London) 1997;272:R1002–R1006. doi: 10.1152/ajpregu.1997.272.3.R1002. [DOI] [PubMed] [Google Scholar]
- 13.Fung B K-K, Nash C R. J Biol Chem. 1983;258:10503–10510. [PubMed] [Google Scholar]
- 14.Halliday K R, Stein P J, Chernoff N, Wheeler G L, Bitensky M W. J Biol Chem. 1984;259:516–525. [PubMed] [Google Scholar]
- 15.Harder D B, Maggio J C, Whitney G. Chem Senses. 1989;14:547–564. [Google Scholar]
- 16.Glendinning J I. Physiol Behav. 1994;56:1217–1227. doi: 10.1016/0031-9384(94)90369-7. [DOI] [PubMed] [Google Scholar]
- 17.Nofre, C., Tinti, J. M. & Ouar-Chatzopoulos, E., inventors; Université Claude Bernard, Lyon 1, France, assignee. Sweetening agents. U.S. patent 4,921,939. May 1, 1990.
- 18.Ninomiya Y, Mizukoshi T, Higashi T, Katsukawa H, Funakoshi M. Brain Res. 1984;302:305–314. doi: 10.1016/0006-8993(84)90244-0. [DOI] [PubMed] [Google Scholar]
- 19.Bartoshuk L M. Physiol Behav. 1975;14:643–649. doi: 10.1016/0031-9384(75)90193-6. [DOI] [PubMed] [Google Scholar]
- 20.Formaker B K, Frank M E. Brain Res. 1996;727:79–90. doi: 10.1016/0006-8993(96)00356-3. [DOI] [PubMed] [Google Scholar]
- 21.Lee C K. Adv Carbohydr Chem Biochem. 1987;45:199–351. doi: 10.1016/s0065-2318(08)60140-7. [DOI] [PubMed] [Google Scholar]
- 22.Benedetti E, Gavuzzo E, Santini A, Kent D R, Zhu Y F, Zhu Q, Mahr C, Goodman M. J Pept Sci. 1995;1:349–359. doi: 10.1002/psc.310010602. [DOI] [PubMed] [Google Scholar]
- 23.Shin W, Kim S J, Shin J M, Kim S H. J Med Chem. 1995;38:4325–4331. doi: 10.1021/jm00021a022. [DOI] [PubMed] [Google Scholar]
- 24.Tonosaki K, Funakoshi M. Nature (London) 1988;331:354–356. doi: 10.1038/331354a0. [DOI] [PubMed] [Google Scholar]
- 25.Behe P, DeSimone J A, Avenet P, Lindemann B. J Gen Physiol. 1990;96:1061–1084. doi: 10.1085/jgp.96.5.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernhardt S J, Naim M, Zehavi U, Lindemann B. J Physiol (London) 1996;490:325–336. doi: 10.1113/jphysiol.1996.sp021147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cummings T A, Daniels C, Kinnamon S C. J Neurophysiol. 1996;75:1256–1263. doi: 10.1152/jn.1996.75.3.1256. [DOI] [PubMed] [Google Scholar]
- 28.Spielman A I, Nagai H, Sunavala G, Dasso M, Breer H, Boekhoff I, Huque T, Whitney G, Brand J G. Am J Physiol. 1996;270:C926–C931. doi: 10.1152/ajpcell.1996.270.3.C926. [DOI] [PubMed] [Google Scholar]
- 29.Cagan R H, Morris R W. Proc Natl Acad Sci USA. 1979;76:1692–1696. doi: 10.1073/pnas.76.4.1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shimazaki K, Sato M, Nakao M. Biochim Biophys Acta. 1986;884:291–298. doi: 10.1016/0304-4165(86)90176-5. [DOI] [PubMed] [Google Scholar]
- 31.Roy G. Crit Rev Food Sci Nutr. 1992;31:59–77. doi: 10.1080/10408399209527561. [DOI] [PubMed] [Google Scholar]
- 32.Schiffman S S, Gatlin C A. Neurosci Biobehav Rev. 1993;17:313–345. doi: 10.1016/s0149-7634(05)80015-6. [DOI] [PubMed] [Google Scholar]