Abstract
Exogenous application of agonists at the kainate subtype of glutamate receptors has been shown to depress evoked monosynaptic inhibition by γ-aminobutyric acid (GABA)ergic interneurons in the hippocampus. This observation has led to the hypothesis that synaptic release of endogenous glutamate might have a disinhibitory effect on neuronal circuits, in addition to depolarizing neurons via postsynaptic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), kainate, and N-methyl-d-aspartic acid (NMDA) receptors. It is not known, however, if glutamate released from excitatory neurons has the same kainate receptor-mediated effect on monosynaptic inhibitory transmission as exogenous agonist application. Indeed, the recent demonstration that excitatory synaptic signals elicited in interneurons are partly mediated by kainate receptors suggests that these receptors may have a pro- rather than disinhibitory role. Here, we examine the effect of synaptically released glutamate on monosynaptic inhibitory signaling. In the presence of antagonists to AMPA and NMDA receptors, brief bursts of activity in glutamatergic afferent fibers reduce GABAergic transmission. This depression of inhibition is reversibly abolished by blocking kainate receptors. It persists when GABAB receptors are blocked and is enhanced by blocking metabotropic glutamate receptors, possibly explained by presynaptic regulation of glutamate release from excitatory afferents by metabotropic autoreceptors. We conclude that the net kainate receptor-mediated effect of synaptically released glutamate is to reduce monosynaptic inhibition. Since this form of disinhibition may contribute to seizure initiation, kainate receptors may constitute an important target for anticonvulsant drug development.
Keywords: disinhibition, guinea pigs
Exogenous application of kainate to rodent hippocampal slices reduces the amplitude of evoked monosynaptic inhibitory postsynaptic potentials or currents (PSCs) (1–3). The phenomenon is blocked by kainate receptor antagonists and is mimicked by applying a selective agonist of the GluR5 subtype of kainate-preferring receptors (2). Kainate application has also been reported to reduce the frequency of action potential-independent “miniature” inhibitory PSCs (3). Because the endogenous agonist at kainate receptors is the ubiquitous excitatory transmitter glutamate, these observations have prompted the suggestion that kainate receptors play a disinhibitory role in neuronal networks: synaptic glutamate release might decrease inhibition via an effect at presynaptic kainate receptors in addition to its conventional excitatory effects mediated by postsynaptic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), kainate, and N-methyl-d-aspartic acid (NMDA) receptors (4). This disinhibition hypothesis has, however, recently been challenged on three lines of evidence. First, although kainate receptor agonists attenuate evoked inhibitory PSCs, there is some disagreement as to whether they reduce the frequency of miniature inhibitory PSCs (5–7), raising a question over their purported presynaptic site of action. Second, kainate receptor agonists have been shown to depolarize interneurons, greatly enhancing their spontaneous firing rate (5–7). Finally, the synaptic excitation of interneurons is partly mediated by kainate receptors (5,6). These observations raise the possibility that the net role of kainate receptors may be pro- rather than disinhibitory (8).
None of the above studies has addressed the effect of glutamate release from excitatory synapses (as opposed to exogenous agonist application) on monosynaptic inhibition. Any inference about the physiological role of kainate receptors on interneurons is therefore based indirectly on predicting the consequences of the different subcellular phenomena listed above. The purpose of the present study is to examine the interaction between kainate receptors and γ-aminobutyric acid (GABA)ergic inhibition in a physiological “network” context and to ask whether synaptic glutamate release onto kainate receptors, on balance, enhances or depresses monosynaptic inhibition. Briefly, we find that activity in excitatory afferent fibers depresses GABAergic inhibition in a kainate receptor-dependent manner. This phenomenon is a unique instance of glutamatergic disinhibition, which, if it occurs in vivo, could contribute to seizure initiation.
METHODS
Transverse hippocampal slices (450 μm thick) were obtained from 4- to 5-week-old guinea pigs and stored in an interface chamber before transfer to a submersion-type recording chamber. The storage and perfusion solution contained 119 mM NaCl, 2.5 mM KCl, 1.3 mM MgSO4, 2.5 mM CaCl2, 26.2 mM NaHCO3, 1 mM NaH2PO4, and 11 mM glucose and was gassed with 95% O2/5% CO2. Bipolar stainless steel stimulating electrodes were positioned in stratum radiatum of the CA1 subfield, although in some cases, one electrode was in stratum oriens (see below). The stimulus duration was 20 μs. Whole-cell recordings were made from CA1 pyramidal neurons, with pipettes containing 145 mM KCl, 10 mM Hepes, 2 mM 1,2-bis(2-aminophenoxy)ethane-N,N,N′,N′-tetraacetic acid (BAPTA), 0.2 mM CaCl2, 1 mM MgCl2, 2 mM MgATP, 0.3 mM GTP, and 5 mM QX314 Br (pH 7.2, osmolarity 295 mOsm). In some cells, CsCl was substituted for KCl, with identical results. Neurons were voltage-clamped at −60 mV (Axopatch 1D amplifier, Axon Instruments), and records were filtered at 1 kHz, digitized at 2–5 kHz, and stored on a personal computer. The access resistance was monitored with a voltage step, and was <20 MΩ.
The goal of the experiments was to determine whether release of glutamate from excitatory nerve terminals could reduce monosynaptic GABAA receptor-mediated inhibition. We encountered two obstacles. First, extracellular stimuli designed to elicit monosynaptic GABAergic inhibitory PSCs also recruit glutamatergic afferent fibers, principally Schaffer collateral axons from CA3 pyramidal neurons. Second, kainate receptor activation by synaptic release of glutamate is normally accompanied by recruitment of AMPA and NMDA receptors (5, 6, 9, 10). Extracellular stimulation of Schaffer collateral axons therefore elicits depolarizing currents in postsynaptic neurons, mediated by AMPA and NMDA receptors. These actions result in monosynaptic excitatory PSCs in pyramidal neurons as well as disynaptic inhibitory PSCs if GABAergic interneurons are brought to threshold for firing.
We adopted the following experimental design. To isolate effects of synaptically released glutamate mediated by kainate receptors, we routinely blocked NMDA receptors with d,l-2-amino-5-phosphonovalerate (APV, 100 μM) and AMPA receptors with the noncompetitive blocker GYKI52466 (11) (100 μM). Any residual actions of glutamate should be mediated by kainate and metabotropic receptors (12). To separate glutamatergic and GABAergic inputs, we took advantage of the anatomy of the transverse hippocampal slice. Compared with glutamatergic Schaffer collateral axons, some of which run the entire transverse length of the CA1 subfield, the axonal projections of GABAergic interneurons are much more restricted (13–15). We therefore recorded from a pyramidal neuron at one end of the CA1 field (either at the CA1–CA2 junction or close to the subiculum), and positioned a “proximal” stimulating electrode within 300 μm in stratum radiatum or oriens (Fig. 1A). Stimuli delivered via this electrode directly activated GABAergic interneurons in monosynaptic contact with the postsynaptic cell as well as Schaffer collateral axons. We also positioned a distal stimulating electrode at the other end of the CA1 subfield in stratum radiatum. Stimulation via this electrode was designed to recruit Schaffer collateral axons. Synaptic recruitment of interneurons by this electrode was reduced, if not prevented, by the AMPA and NMDA receptor blockers, whereas direct electrical activation of monosynaptically coupled interneurons was minimized because of the limited extent of their arborizations.
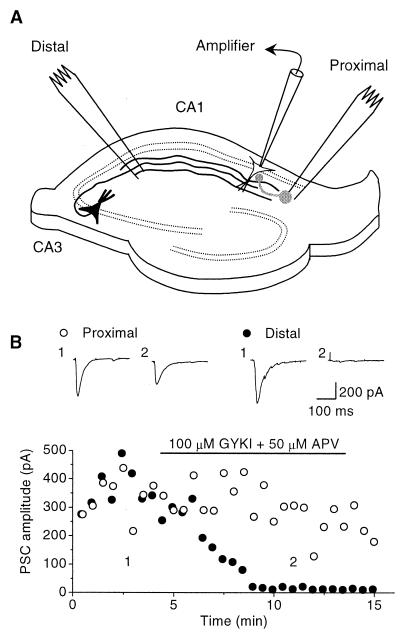
Figure 1.
Experimental design. (A) Schematic illustration of the hippocampal slice showing the positioning of the recording pipette and stimulating electrodes. Schaffer collateral axons are shown in black, and a local inhibitory interneuron is shown in gray. (B) Effect of blocking AMPA and NMDA receptors with GYKI52466 and APV, respectively. The response to the distal stimulus (●) was completely blocked. The proximal stimulus (○), however, continued to elicit a monosynaptic response. Insets show averages of five successive traces obtained at the times indicated.
The experimental results reported here were obtained at room temperature (23–25°C). Measurements obtained at 35–37°C were obscured by a high frequency of spontaneous PSCs. Data are given as mean ± SE, and the effects of experimental manipulations were analyzed with Student’s paired t test. Drugs were purchased from Sigma, except for QX314 Br (Alomone Laboratories) and APV, 6,7-dinitroquinoxaline-2,3-dione (DNQX), (S)-α-methyl-4-carboxyphenylglycine (MCPG), α-methylserine-O-phosphate (MSOP), and l-trans-pyrrolidine-2,4-dicarboxylic acid (PDC) (Tocris Cookson, Bristol, U.K.). CGP35348 was obtained from CIBAGeigy. Part of the GYKI52466 supply was a gift from I. Tarnawa (Institute for Drug Research, Budapest, Hungary), and part was purchased from Research Biochemicals, Natick, MA. Stimulation was interrupted for 5–10 minutes during solution exchange to test the effects of the different antagonists. GYKI52466 and DNQX were dissolved in DMSO, and MCPG and PDC were dissolved in NaOH. Application of either vehicle alone was without effect on PSCs or evoked field potentials.
RESULTS
Fig. 1B shows the effect of applying APV and GYKI52466 on the PSCs elicited by alternately stimulating via the proximal or the distal electrode. The response to distal stimulation disappeared, as expected if monosynaptic excitatory PSCs and disynaptic inhibitory PSCs were abolished. The response to proximal stimulation, on the other hand, was only partially reduced, as expected if a monosynaptic inhibitory PSC remained. We routinely verified that the residual PSC was completely blocked by picrotoxin (100 μM) at the end of the experiment, confirming that it was mediated by GABAA receptors. Experiments were discontinued if a PSC remained after single stimuli delivered to the distal electrode in the presence of GYKI52466 and APV.
Although stimulation via the distal electrode elicited no PSC, it should still cause release of glutamate. What effect does synaptically released glutamate have on the amplitude of the GABAergic PSC elicited by proximal stimulation? We examined the effect of a brief high-frequency train of distal stimuli, designed to release a large pulse of glutamate, on the response to proximal stimulation. Fig. 2A shows a comparison of interleaved trials where the GABAergic PSC was either elicited on its own or within 100 ms of the end of a five-pulse, 100-Hz tetanus delivered via the distal electrode. We observed a 23% depression of the test PSC, which was completely abolished by subsequent addition of the nonselective AMPA/kainate receptor blocker DNQX (16) (50 μM). Because AMPA receptors were already blocked by GYKI52466, the effect of DNQX implies that the depression of inhibition was mediated by kainate receptors.
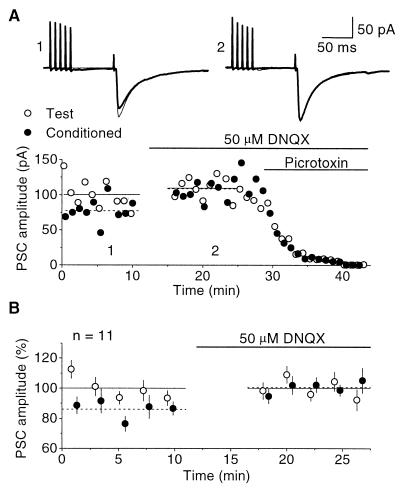
Figure 2.
Depression of GABAergic transmission. (A) Upper, Superimposed traces showing the monosynaptic GABAergic PSC elicited on its own (thin line) or after a high-frequency burst delivered via the distal electrode (thick line). The depression (1) is abolished by addition of DNQX to the perfusion solution (2). Lower, Proximal PSC amplitude plotted against time for the same experiment. APV and GYKI52466 were present throughout, to block NMDA and AMPA receptors. The traces in A were obtained by averaging 10 records under each condition, at the times indicated. Horizontal lines indicate the average amplitudes of the test and conditioned PSC before and during DNQX perfusion. Picrotoxin (100 μM) abolished the PSC, indicating that it was mediated by GABAA receptors. (B) Average of 11 experiments. The PSC amplitudes were normalized to set the average amplitude of the unconditioned response to 100%. Each point shows the average of 2–4 successive trials. DNQX completely abolished the depression of inhibition.
Fig. 2B shows a summary of 11 experiments in which the same procedure was followed. The depression averaged 13% ± 2% and was completely abolished by DNQX (P < 0.0001; see also Fig. 4B). Although these results argue strongly for a kainate receptor-mediated depression of GABAergic inhibition, a more compelling demonstration would require that the effect of blocking kainate receptors be reversed by washing out the antagonist. Since the effect of DNQX is very slow to wash out, we applied instead the reversible nonselective ionotropic glutamate receptor antagonist kynurenic acid (17) (2.5–10 mM). Fig. 3A shows the results obtained in one experiment. In the continued presence of APV and GYKI52466, kynurenic acid perfusion was accompanied by a reduction in depression from 24% to 1%. After washout of kynurenic acid, the depression recovered to 17%. This effect of kynurenic acid was consistent across eight identical experiments (see also Fig. 4B), further supporting a role for kainate receptors in mediating the depression of inhibitory transmission.
Figure 4.
Summary of results indicating that kainate receptors mediate the depression of monosynaptic inhibition. The depression was abolished by 50 μM DNQX (A) and reversibly reduced by 2.5–10 mM kynurenic acid (B) or 10 μM Gd3+ (C). The depression was nonsignificantly reduced by 100 μM CGP35348 (D) but in the same neurons was abolished by the subsequent addition of DNQX. Blockade of metabotropic receptors with 250 μM MCPG and 200 μM MSOP increased the depression (E). PDC (100–200 μM) had no significant effect on the depression (F). The distal tetanus was 5 pulses at 100 Hz except for the experiments in D, where it consisted of 10 pulses at 200 Hz.
Figure 3.
Blockade of kainate receptors reversibly reduces disinhibition. (A) Effect of kynurenic acid (2.5 mM) in one cell. Upper, superimposed averages of conditioned (thick lines) and unconditioned PSCs (thin lines) recorded before (1), during (2), and after (3) perfusion with kynurenic acid. Lower, proximal PSC amplitude plotted against time. The averaged traces were obtained at the times indicated (numbers in brackets indicate % decrease in PSC amplitude produced by the conditioning train). The depression of inhibition was abolished by kynurenic acid and partially recovered following washout. (B) Effect of gadolinium studied in another cell. The averaged PSCs were obtained before (1), during (2), and after (3) perfusion with 10 μM Gd3+. (C) Averaged results obtained in 11 cells (washout data was obtained in 8 cells). Each point shows the average of three successive trials. The depression of the PSC by the conditioning train disappeared in the presence of Gd3+ and recovered after washout. APV and GYKI52466 were present throughout all of the illustrated experiments.
A potential weakness of the above experiments is that DNQX and kynurenic acid act on AMPA as well as kainate receptors. If AMPA receptors were incompletely blocked by GYKI52466, they might have contributed to the depression of GABAergic inhibition caused by the conditioning train. We therefore examined the effect of gadolinium, which, at 10 μM, blocks kainate receptors without significant effect on AMPA receptors (18). Perfusion of 10 μM Gd3+ completely and reversibly abolished the depression of inhibition in 11 cells (Figs. 3 B and C and 4C). Gd3+ had no effect on the unconditioned GABAergic PSC, or (in separate control experiments) on the amplitude of AMPA receptor-mediated field potentials. Three different kainate receptor antagonists (DNQX, kynurenic acid, and Gd3+) thus completely abolished the depression of inhibition.
The insets in Fig. 3A show that a small current sometimes followed the high-frequency trains delivered via the distal stimulus, even though single stimuli were without effect. This small current (<15% of the test PSC elicited by the proximal stimulus) was unaffected by the kainate receptor antagonists (P > 0.5, DNQX experiments; P > 0.4, Gd3+ experiments), but was uniformly abolished by adding picrotoxin at the end of the experiments, indicating that it was mediated by GABAA receptors. We conclude that, despite the remote position of the distal electrode, high-frequency trains of stimuli could occasionally recruit monosynaptically coupled interneurons. We found no evidence that tetanic afferent fiber stimulation could directly activate postsynaptic kainate receptors on pyramidal neurons in CA1 [in contrast to the effect of mossy fiber stimulation on CA3 pyramidal neurons (9, 10)]. The observation that the distal high-frequency stimuli could occasionally elicit GABA release at synapses on the pyramidal neuron raises the possibility that this transmitter may also activate presynaptic GABAB receptors on interneuron terminals (19–21), potentially contributing to the depression of inhibition. We therefore tested the effect of the GABAB receptor blocker CGP35348 (22) on the disinhibition. We used 100 μM CGP35348, a concentration that abolishes monosynaptic GABAB receptor-mediated signals and reduces GABAB receptor-mediated paired-pulse depression (20). In these experiments, we deliberately increased the frequency and number of pulses in the conditioning train (200 Hz, 10 pulses) to enhance the likelihood of detecting a contribution of GABAB receptors. CGP35348 produced a small, nonsignificant reduction in the depression in nine cells (P = 0.36). Subsequent addition of DNQX, however, abolished the depression (Fig. 4D). Thus, although we cannot exclude a small contribution of GABAB receptors to the depression of inhibition with 200 Hz tetani, the major effect is still mediated by kainate receptors.
We also tested the involvement of metabotropic glutamate receptors by adding the group I/II antagonist MCPG (250 μM) together with the group III antagonist MSOP (200 μM) (23, 24). If presynaptic metabotropic receptors on interneuron terminals contribute to the action of glutamate on GABAergic transmission, these drugs should attenuate the depression of inhibition. Instead, we observed a reversible increase in depression (Fig. 4E). These results therefore lend no support to the hypothesis that activation of metabotropic receptors on inhibitory axon terminals by synaptically released glutamate depresses transmission. Although they could be explained by a facilitatory action of metabotropic receptor activation on GABA release, an alternative explanation is that metabotropic receptors on Schaffer collateral terminals mediate autoinhibition of glutamate release during the high-frequency stimulus train (24). Removing this feedback inhibition would then enhance glutamate release, potentiating the depression of GABAergic transmission.
Finally, we asked whether glutamate transporters play a role in regulating the kainate receptor-mediated depression of GABAergic PSCs. Adding the transportable analog PDC (100–200 μM) to the perfusion solution produced a nonsignificant enhancement of the depression (Fig. 4F).
DISCUSSION
The present results indicate that synaptic glutamate release attenuates monosynaptic GABAergic inhibition via an action at kainate receptors. Neither GABAB nor metabotropic glutamate receptors appear to contribute significantly to the phenomenon.
The subcellular mechanism of the disinhibition is unclear. One possible explanation is that glutamate release from excitatory terminals depresses GABA release via an action at presynaptic kainate receptors. A similar presynaptic effect of kainate on glutamate release has been reported (25–27). The hypothesis that kainate reduces GABA release by a presynaptic action is supported by a recent report of quantal analysis of the action of exogenous kainate on inhibitory transmission (3). Because axo-axonic synapses have not been demonstrated in the hippocampus (28), such a mechanism would require that glutamate acted extrasynaptically, as has been demonstrated in other systems (29–31). However, the evidence that kainate acts presynaptically at inhibitory interneurons is not unanimous (5–7). It is also unclear whether kainate receptors are located at GABAergic axon terminals (32–34) as would be required for a presynaptic locus of action. An alternative explanation for the disinhibition is that glutamate acts at dendritic and/or somatic receptors on interneurons (5, 6). Activation of these receptors depolarizes interneurons, which at first sight should lower the threshold for their recruitment by the proximal stimulus and therefore lead to an increase, rather than a decrease, in the size of the GABAergic signal. The fact that synaptic release of glutamate attenuates GABAergic signaling is therefore unexpected but could be explained by activation of a slow subthreshold conductance, which might lower excitability or reduce axonal action potential propagation (6). Another alternative is that the distal stimulus recruits a population of interneurons that, in turn, inhibits GABA release. This is less likely because the small PSC occasionally seen after the distal tetanus (Fig. 3A), which presumably reflects interneuron recruitment, was unaffected by blocking kainate receptors.
A surprising aspect of the results is that inhibitory PSCs were attenuated for up to 100 ms after the end of the conditioning train in the glutamatergic afferent fibers (see, for instance, Fig. 2A). Over this interval, extracellular glutamate concentrations would be expected to have returned to resting levels (35), making it unlikely that kainate receptors were continuously exposed to agonist. The duration of disinhibition is, however, compatible with the prolonged time course of the kainate receptor-mediated component of synaptic PSCs in interneurons (5, 6) and CA3 pyramidal neurons (9, 10). This time course remains unexplained, because kainate receptors in cultured hippocampal neurons exposed to glutamate show rapid deactivation kinetics (36). An alternative explanation is that kainate receptor activation triggers a metabolic cascade, which has been implicated in the reduction of inhibitory PSC amplitude by exogenous kainate application (37).
Perfusion of PDC did not lead to a significant enhancement of the depression of GABAergic signaling. This result does not distinguish between the alternative possible sites of action of glutamate on inhibitory interneurons, because blockade of transport leads to a buildup of extracellular glutamate (38). This phenomenon may desensitize kainate receptors (36) and therefore mask the consequences of enhancing the spatial extent of glutamate diffusion after release.
The present study shows that activity-dependent kainate receptor recruitment has a disinhibitory effect on monosynaptic GABAergic signaling, as was originally proposed on the basis of exogenous kainate receptor agonist application (1–4). It would be premature, however, to conclude that kainate receptors have, on balance, a net disinhibitory effect in vivo, because the interneurons were activated by electrical stimulation with AMPA and NMDA receptors blocked. Indeed, synaptic kainate receptor activation has been shown to bring interneurons to action potential threshold, implying that they may enhance feed-forward inhibition (5). We saw no evidence of disynaptic inhibitory PSCs in the present study: the occasional small PSCs after the conditioning train were unaffected by blocking kainate receptors, implying a monosynaptic origin. More intense activity in the excitatory afferent fibers may be necessary to elicit feed-forward inhibition than was achieved here. Under physiological conditions, however, where AMPA and NMDA receptors are available to depolarize interneurons synaptically, kainate receptors might contribute to their recruitment. Ultimately, whether kainate receptors play, on balance, a pro- or disinhibitory role will be determined by the relative magnitude of kainate receptor-dependent interneuron recruitment and attenuation of monosynaptic inhibition.
The physiological role of kainate receptor-mediated attenuation of monosynaptic inhibition is unclear. The phenomenon could facilitate the transmission of information through the hippocampal formation under conditions of intense afferent fiber firing. On the other hand, it may also contribute to the initiation of epileptic seizures, because excessive excitatory signaling could be accompanied by a reduction in inhibition, providing a positive feedback loop. Notwithstanding the unresolved question whether kainate receptor-mediated recruitment of interneurons outweighs the attenuation of inhibition, kainate receptors may be an important target for anticonvulsant drug development.
Acknowledgments
We are indebted to D. A. Rusakov and F. Asztely for help with some experiments and to A. Spauschus and R. A. Nicoll for comments on the manuscript. We are very grateful to Dr. Tarnawa for the gift of GYKI52466, and to Drs. Kaufmann, Maître, and Olpe for the gift of CGP35348. This research was supported by the Medical Research Council. Z.M. is a Royal Society Postdoctoral Fellow, sponsored by the North Atlantic Treaty Organization and the Foreign and Commonwealth Office.
ABBREVIATIONS
- AMPA
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- NMDA
N-methyl-d-aspartic acid
- GABA
γ-amino butyric acid
- PSC
postsynaptic current
- APV
d,l-2-amino-5-phosphonovalerate
- DNQX
6,7-dinitroquinoxaline-2,3-dione
- MSOP
α-methylserine-O-phosphate
- MCPG
(S)-α-methyl-4-carboxyphenylglycine
Footnotes
This paper was submitted directly (Track II) to the Proceedings Office.
References
- 1.Fisher R S, Alger B E. J Neurosci. 1984;4:1312–1323. doi: 10.1523/JNEUROSCI.04-05-01312.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clarke V R, Ballyk B A, Hoo K H, Mandelzys A, Pellizzari A, Bath C P, Thomas J, Sharpe E F, Davies C H, Ornstein P L, et al. Nature (London) 1997;389:599–603. doi: 10.1038/39315. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez-Moreno A, Herreras O, Lerma J. Neuron. 1997;19:893–901. doi: 10.1016/s0896-6273(00)80970-8. [DOI] [PubMed] [Google Scholar]
- 4.Lerma J. Neuron. 1997;19:1155–1158. doi: 10.1016/s0896-6273(00)80407-9. [DOI] [PubMed] [Google Scholar]
- 5.Cossart R, Esclapez M, Hirsch J C, Bernard C, Ben-Ari Y. Nat Neurosci. 1998;1:470–478. doi: 10.1038/2185. [DOI] [PubMed] [Google Scholar]
- 6.Frerking M, Malenka R C, Nicoll R A. Nat Neurosci. 1998;1:479–486. doi: 10.1038/2194. [DOI] [PubMed] [Google Scholar]
- 7.Bureau I, Bischoff S, Heinemann S F, Mulle C. J Neurosci. 1999;19:653–663. doi: 10.1523/JNEUROSCI.19-02-00653.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mody I. Nat Neurosci. 1998;1:434–436. doi: 10.1038/2151. [DOI] [PubMed] [Google Scholar]
- 9.Vignes M, Collingridge G L. Nature (London) 1997;388:179–182. doi: 10.1038/40639. [DOI] [PubMed] [Google Scholar]
- 10.Castillo P E, Malenka R C, Nicoll R A. Nature (London) 1997;388:182–186. doi: 10.1038/40645. [DOI] [PubMed] [Google Scholar]
- 11.Paternain A V, Morales M, Lerma J. Neuron. 1995;14:185–189. doi: 10.1016/0896-6273(95)90253-8. [DOI] [PubMed] [Google Scholar]
- 12.Lerma J, Morales M, Vicente M A, Herreras O. Trends Neurosci. 1997;20:9–12. doi: 10.1016/S0166-2236(96)20055-4. [DOI] [PubMed] [Google Scholar]
- 13.Ramon y Cajal S. Histologie du Système Nerveux de l’Homme et des Vertébrés. Paris: Maloine; 1909. [Google Scholar]
- 14.Freund T F, Buzsaki G. Hippocampus. 1996;6:347–470. doi: 10.1002/(SICI)1098-1063(1996)6:4<347::AID-HIPO1>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 15.Buhl E H, Halasy K, Somogyi P. Nature (London) 1994;368:823–828. doi: 10.1038/368823a0. [DOI] [PubMed] [Google Scholar]
- 16.Honoré T, Davies S N, Drejer J, Fletcher E J, Jacobsen P, Lodge D, Nielsen F E. Science. 1988;241:701–703. doi: 10.1126/science.2899909. [DOI] [PubMed] [Google Scholar]
- 17.Ganong A H, Lanthorn T H, Cotman C W. Brain Res. 1984;273:170–174. doi: 10.1016/0006-8993(83)91108-3. [DOI] [PubMed] [Google Scholar]
- 18.Huettner J E, Stack E, Wilding T J. Neuropharmacology. 1998;37:1239–1247. doi: 10.1016/s0028-3908(98)00082-3. [DOI] [PubMed] [Google Scholar]
- 19.Harrison N L. J Physiol (London) 1990;422:433–446. doi: 10.1113/jphysiol.1990.sp017993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davies C H, Starkey S J, Pozza M F, Collingridge G L. Nature (London) 1991;349:609–611. doi: 10.1038/349609a0. [DOI] [PubMed] [Google Scholar]
- 21.Isaacson J S, Solis J M, Nicoll R A. Neuron. 1993;10:165–175. doi: 10.1016/0896-6273(93)90308-e. [DOI] [PubMed] [Google Scholar]
- 22.Olpe H R, Karlsson G, Pozza M F, Brugger F, Steinmann M, Van Riezen H, Fagg G, Hall R G, Froestl W, Bittiger H. Eur J Pharmacol. 1990;187:27–38. doi: 10.1016/0014-2999(90)90337-6. [DOI] [PubMed] [Google Scholar]
- 23.Watkins J, Collingridge G. Trends Pharmacol Sci. 1994;15:333–342. doi: 10.1016/0165-6147(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 24.Pin J-P, Duvoisin R. Neuropharmacology. 1995;34:1–16. doi: 10.1016/0028-3908(94)00129-g. [DOI] [PubMed] [Google Scholar]
- 25.Represa A, Tremblay E, Ben Ari Y. Neuroscience. 1987;20:739–748. doi: 10.1016/0306-4522(87)90237-5. [DOI] [PubMed] [Google Scholar]
- 26.Chittajallu R, Vignes M, Dev K K, Barnes J J, Collingridge G L, Henley J M. Nature (London) 1996;379:78–81. doi: 10.1038/379078a0. [DOI] [PubMed] [Google Scholar]
- 27.Kamiya H, Ozawa S. J Physiol (London) 1998;509:833–846. doi: 10.1111/j.1469-7793.1998.833bm.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters A, Palay S L, Webster H F. The Fine Structure of the Nervous System: Neurons and Their Supporting Cells. New York: Oxford Univ. Press; 1991. [Google Scholar]
- 29.Scanziani M, Salin P A, Vogt K E, Malenka R C, Nicoll R A. Nature (London) 1997;385:630–634. doi: 10.1038/385630a0. [DOI] [PubMed] [Google Scholar]
- 30.Min M-Y, Rusakov D A, Kullmann D M. Neuron. 1998;21:561–570. doi: 10.1016/s0896-6273(00)80566-8. [DOI] [PubMed] [Google Scholar]
- 31.Kullmann D M, Asztely F. Trends Neurosci. 1998;21:8–14. doi: 10.1016/s0166-2236(97)01150-8. [DOI] [PubMed] [Google Scholar]
- 32.Bettler B, Egebjerg J, Sharma G, Pecht G, Hermans-Borgmeyer I, Moll C, Stevens C F, Heinemann S. Neuron. 1992;8:257–265. doi: 10.1016/0896-6273(92)90292-l. [DOI] [PubMed] [Google Scholar]
- 33.Egebjerg J, Bettler B, Hermans-Borgmeyer I, Heinemann S. Nature (London) 1991;351:745–748. doi: 10.1038/351745a0. [DOI] [PubMed] [Google Scholar]
- 34.Bettler B, Mulle C. Neuropharmacology. 1995;34:123–139. doi: 10.1016/0028-3908(94)00141-e. [DOI] [PubMed] [Google Scholar]
- 35.Rusakov D A, Kullmann D M. J Neurosci. 1999;18:3158–3170. doi: 10.1523/JNEUROSCI.18-09-03158.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lerma J, Paternain A V, Naranjo J R, Mellstrom B. Proc Natl Acad Sci USA. 1993;90:11688–11692. doi: 10.1073/pnas.90.24.11688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodriguez-Moreno A, Lerma J. Neuron. 1998;20:1211–1218. doi: 10.1016/s0896-6273(00)80501-2. [DOI] [PubMed] [Google Scholar]
- 38.Isaacson J S, Nicoll R A. J Neurophysiol. 1993;70:2187–2191. doi: 10.1152/jn.1993.70.5.2187. [DOI] [PubMed] [Google Scholar]