Abstract
Context:
Assessment tools should identify functional limitations associated with functional ankle instability (FAI) by discriminating unstable from stable ankles.
Objective:
To identify assessment tools that discriminated FAI from stable ankles and determine the most accurate assessment tool for discriminating between FAI and stable ankles.
Design:
Case-control study.
Setting:
Research laboratory.
Patients or Other Participants:
Fifteen individuals with FAI and 15 healthy individuals; participants with unilateral FAI reported “giving-way” sensations and ankle sprains, whereas healthy participants did not.
Intervention(s):
Participants answered 12 questions on the Ankle Joint Functional Assessment Tool (AJFAT). They also performed a single-leg jump landing, which required them to jump to half their maximum jump height, land on a single leg, and stabilize quickly on a force plate.
Main Outcome Measure(s):
Receiver operating characteristic curves determined cutoff scores for discriminating between ankle groups for AJFAT total score and resultant vector (RV) time to stabilization. Accuracy values for discriminating between groups were determined by calculating the area under the receiver operating characteristic curves.
Results:
The cutoff score for discriminating between FAI and stable ankles was ≥26 (sensitivity = 1, specificity = 1) and ≥1.58 seconds (sensitivity = 0.67, specificity = 0.73) for the AJFAT total score and RV time to stabilization, respectively. The area under the curve for the AJFAT was 1.0 (asymptotic significance <.05), whereas the RV time to stabilization had an area under the curve of 0.72 (asymptotic significance <.05).
Conclusions:
The AJFAT was an excellent assessment tool for discriminating between ankle groups, whereas RV time to stabilization was a fair assessment tool. Although both assessments discriminated between ankle groups, the AJFAT more accurately discriminated between groups than the RV time to stabilization did. Future researchers should confirm these findings using a prospective research design.
Keywords: balance, ankle sprains, time to stabilization, Ankle Joint Functional Assessment Tool
Key Points
For discriminating between stable ankles and those with functional instability, the Ankle Joint Functional Assessment Tool was excellent, whereas the resultant vector time to stabilization was fair.
The Ankle Joint Functional Assessment Tool more accurately discriminated between groups than the resultant vector time to stabilization did.
The Ankle Joint Functional Assessment Tool and resultant vector time to stabilization might be used as clinical assessments to identify functional limitations associated with functional ankle instability.
Ankle sprains are common injuries that occur during physical activity, especially activities that involve landing from a jump.1–3 Residual ankle instability can exist after sprains, and recurrent ankle sprains might continue to occur during physical activity.4–12. In addition to recurrent sprains, physically active individuals commonly report “giving-way” sensations at the ankle joint with weight-bearing activity.6–13 Individuals who experience these residual ankle sprain symptoms have a condition known as functional ankle instability (FAI), and giving way is common among individuals who have suffered an ankle sprain.1–6,13,14 Clinicians typically assess FAI by obtaining a history of the frequency of recurrent ankle sprains and giving-way sensations occurring with activity.4–6,11–21
In addition to assessing frequency of sprains and giving-way sensations, we use several tests clinically and in research to assess FAI. Single-leg balance tests (instrumented and non-instrumented),11–13,21,22 Star Excursion Balance Test,23 functional performance deficits,19 strength tests,11–12 and orthopaedic laxity tests11–24 are employed to assess ankle instability. Some individuals with FAI have deficits on these aforementioned tests compared with those with healthy ankles,11–13,19,21–24 whereas others may not demonstrate deficits and only report feelings of giving way in the ankle during activity.11,25–29
Recently, single-leg jump-landing tests have been used to assess the effects of FAI on dynamic postural stability 15–18 and improvements in dynamic postural stability associated with coordination training in participants with FAI.25 Functional ankle instability has been correlated with increases in frontal and sagittal stabilization times of single-leg jump landings, and researchers have contended that causal factors of FAI might be responsible for these landing impairments.15–17 Time-to-stabilization calculations provide clinicians and researchers with separate measures of dynamic postural stability in the frontal and sagittal planes of motion. However, a time-to-stabilization measure that is calculated from the resultant vector (RV) of the frontal and sagittal ground reaction forces might provide clinicians and researchers with a single stability assessment that accounts for both planes of motion. We have recently developed this RV time-to-stabilization measure, and one purpose of our study was to examine the ability of RV time to stabilization to discriminate between participants with FAI and participants with stable ankles.
Although evaluating stabilization times of physically active individuals with FAI provides relevant information on the effects of ankle instability on dynamic postural stability, stabilization times must be calculated from ground reaction forces. Clinicians typically do not have access to instrumented force plates. As an alternative, clinicians can use questionnaires to quantify self-reported functional limitations in individuals with FAI and to assess improvements associated with coordination training in participants with FAI.16,17,19–21,25,30 One functional instability questionnaire that has been used to quantify functional limitations is the Ankle Joint Functional Assessment Tool (AJFAT)16,17,21,25 We have recently used this questionnaire to assess functional limitations in participants with FAI and participants with stable ankles.16,17,25 We have not, however, examined potential differences between these ankle groups. Therefore, another purpose of our study was to examine the ability of this questionnaire to discriminate between FAI and stable ankles.
Clinicians can use a variety of tools to evaluate FAI, and assessment tools should be able to identify functional limitations associated with FAI by discriminating unstable ankles from stable ankles. In this investigation, we chose to use RV time to stabilization and the AJFAT to assess dynamic stability or functional limitations associated with FAI. However, which of these assessment tools is sensitive for discriminating between FAI and stable ankles is currently unknown. The tools that best discriminate between stable and unstable ankles could be used as preparticipation screening assessment tools to identify functional limitations associated with FAI or to evaluate improvements associated with coordination training. Identifying and correcting deficits associated with FAI before participation in physical activity could have implications for preventing ankle sprains.
Therefore, our overall purpose was to determine the most accurate assessment tool for discriminating between FAI and stable ankles. To analyze the accuracy of each assessment, we determined the following for the AJFAT and RV time to stabilization: (1) sensitivity and specificity, (2) positive predictive and negative predictive scores, (3) the probability of identifying participants correctly, and (4) the “best” cutoff score for discriminating between FAI and stable ankles using the AJFAT and RV time to stabilization. The best cutoff score was defined as the score with the greatest sensitivity and the lowest false-positive score (ie, 1–specificity).
Methods
Participants
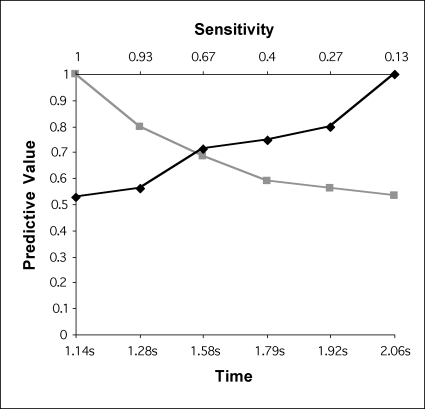
Fifteen participants with stable ankles were matched by age, height, mass, sex, and leg tested with 15 participants with unilateral FAI (Table 1). The same leg as the match was tested in participants with stable ankles. Participants were matched by dominant (leg used to kick a ball) or nondominant (leg used to stand on while kicking a ball) leg. Inclusion criteria for FAI used in this study have been described in our previous reports.16,17,25 In summary, participants with FAI reported a history of 1 sprain followed by at least 3 days of immobilization. They also reported a minimum of 2 ankle sprains and 2 episodes of giving-way sensations during physical activity after the initial sprain. Participants retrospectively reported their frequency of sprain and giving way during an interview. We recorded the frequency of ankle sprains and giving-way sensations within 1 year of their participation in this study. Participants did not require immobilization with these subsequent ankle sprains but had to report signs and symptoms of an acute ankle sprain (pain, swelling, mild point tenderness, abnormal movement). Additionally, we assessed ankle joint laxity with the anterior drawer and talar tilt special tests. Laxity was quantified using a grading scale reported by Ryan.11 Potential participants were excluded if they reported an ankle sprain within 6 weeks of this study. All participants read and signed a consent form approved by the Committee for the Protection of the Rights of Human Subjects, which also approved the study.
Table 1.
Characteristics of Participants With or Without Functional Ankle Instability (Mean ± SD)
Ankle Joint Functional Assessment Tool
All participants completed the AJFAT.21 Those with FAI compared the unstable ankle with the stable ankle; those with stable ankles compared the test ankle with the non-test ankle. Participants chose the answers that best described the ankle using the following scale: much less than the other ankle, slightly less than the other ankle, equal in amount to the other ankle, slightly more than the other ankle, or much more than the other ankle. Each answer was assigned a point value between 0 and 4. However, these point values were unknown to the participants. Higher point values represented greater levels of symptoms or greater functional instability associated with functional limitations. Question scores were then added to provide a total score on the AJFAT. The maximum score on this assessment tool was 48. The tool had 12 questions that rated (1) ankle pain, (2) ankle swelling, (3) ability to walk on uneven surfaces, (4) overall feeling of stability, (5) overall ankle strength, (6) ability to descend stairs, (7) ability to jog, (8) ability to change direction when running, (9) overall activity level, (10) ability to sense a “rollover” event, (11) ability to respond to a “rollover” event, and (12) ability to return to activity after a “rollover” event. Our pilot data indicated that the AJFAT has high test-retest reliability (intraclass correlation coefficient 2,1 = 0.94) and precision (standard error of measurement = 1.5 points).
Single-leg Jump-landing Test
Participants were tested on a single-leg jump-landing test, which we have previously described.16,17,25,31 In summary, participants stood 70 cm away from the center of a force plate and performed a jump using a bilateral-foot take-off technique. Participants jumped to 50% to 55% of their maximum jump height and then attempted to land on a single leg. They were instructed to stabilize as quickly as possible and remain as motionless as possible in a single-leg stance for 20 seconds. Three practice trials and 7 testing trials were performed, with 30 seconds of rest between trials. Trials were repeated if participants failed to jump within the 50% to 55% range, hopped on the test leg, or touched down with the non–weight-bearing leg.
Data Collection and Reduction
A Bertec force plate (model 4060-08A; Bertec Corp, Columbus, OH) collected ground reaction force data at a sampling rate of 180 Hz. Analog signals were amplified by a factor of 2 with a Bertec amplifier (model AM-6701). Signals were then passed through a BNC adapter chassis (model PCI-MIO-16E-1; National Instruments Corp, Austin, TX) that was interfaced with an analog-to-digital board within a personal computer. MotionSoft Balance Assessment computer software (version 2.0; MotionSoft Inc, Chapel Hill, NC) converted digital data to ground reaction force vectors and moments. Data were filtered using a 2nd-order, recursive low-pass Butterworth digital filter with an estimated optimum cutoff frequency of 12.53 Hz.15–17,25,31 Anterior-posterior (AP) and medial-lateral (ML) ground reaction forces were combined to form a resultant vector
Time to stabilization for the RV was then calculated using a normalization method that we have previously described for anterior-posterior and medial-lateral time to stabilization.17 Resultant vector time to stabilization essentially determined the time point when the beginning ground reaction force resembled the ground reaction force of stabilized single-leg stance of participants with stable ankles.16,17,25,31 The average RV time to stabilization value of 7 trials for each participant was used for data analysis. Our pilot data indicated that the RV time to stabilization had moderate test-retest reliability (intraclass correlation coefficient 2,7 = 0.70) and high precision (standard error of measurement = 0.26 seconds).
Statistical Analysis
We calculated sensitivity and specificity values for each dependent measure across the range of possible scores to compute receiver operating characteristic (ROC) curves. Sensitivity referred to the probability that participants with FAI were correctly identified as having FAI. Specificity referred to the probability that participants with stable ankles were correctly identified as not having FAI. Additionally, positive predictive and negative predictive scores were calculated for each dependent measure across the range of possible scores to compute ROC curves. Positive predictive score referred to the proportion of participants with positive test results who were correctly assessed as having FAI. Conversely, negative predictive score referred to the proportion of participants with negative test results who were correctly assessed as having stable ankles. An ROC curve and the area under the curve (AUC) were computed for AJFAT total score and RV time to stabilization. The best cutoff score was calculated for AJFAT total score and RV time to stabilization by determining the score with the greatest sensitivity and the lowest false-positive score (ie, 1–specificity). We used SPSS software (version 13.0; SPSS Inc, Chicago, IL) for statistical analyses. Asymptotic significance level for the AUC was set at P < .05.
Results
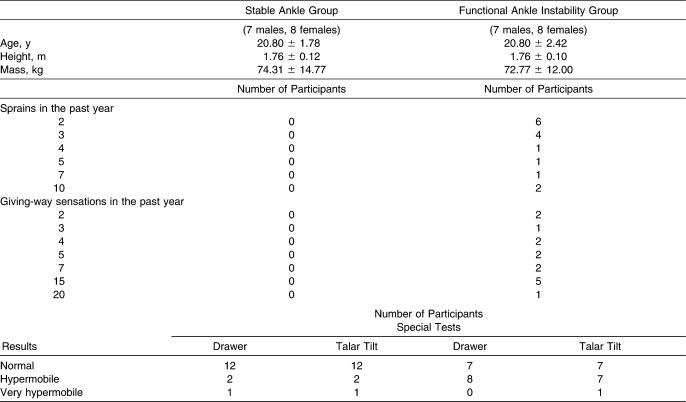
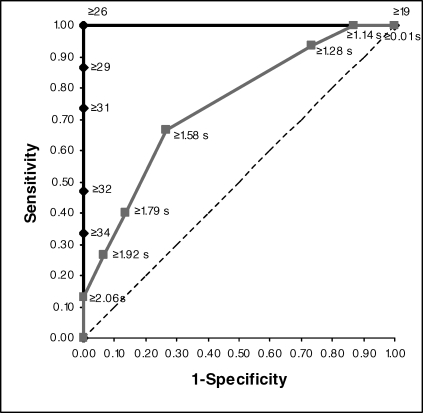
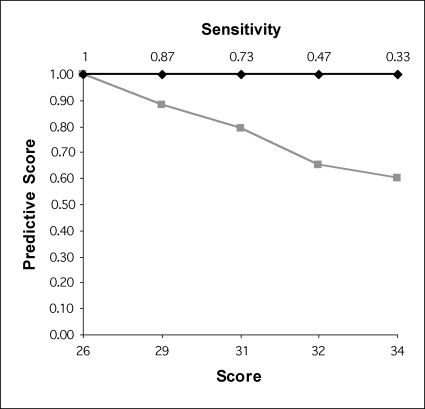
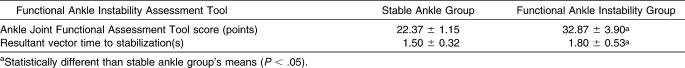
The AJFAT ROC curve had an AUC of 1.0 (asymptotic significance <.05), while the RV time to stabilization ROC curve had an AUC of 0.72 (asymptotic significance <.05) (Figure 1). Positive and negative predictive scores are presented in Figures 2 and 3 for the AJFAT total score and RV time to stabilization, respectively. The best cutoff score for discriminating between FAI and stable ankles was ≥26 and ≥1.58 seconds for the AJFAT total score and RV time to stabilization, respectively (Table 2).
Figure 1. Receiver operating characteristic (ROC) curve. The ROC curve for the Ankle Joint Functional Assessment Tool is the black line running vertically from points 0,0 to 0,1 and then horizontally from points 0,1 to 1,1. The ROC curve for resultant vector time to stabilization is the grey line.
Figure 2. Positive and negative predictive scores with associated sensitivity scores for the Ankle Joint Functional Assessment Tool. The black line represents positive predictive scores, and the grey line represents negative predictive scores. The score ≥26 and sensitivity of 1.00 represents the best cutoff score that minimizes the sum of false-positive and false-negative scores.
Figure 3. Positive and negative predictive scores with associated sensitivity scores for the resultant vector time to stabilization. The black line represents positive predictive scores, and the grey line represents negative predictive scores. The score ≥1.58 seconds and sensitivity of 0.67 represents the best cutoff score that minimizes the sum of false-positive and false-negative scores.
Table 2.
Functional Ankle Instability Assessments (Mean ± SD)
Discussion
The most important finding of our investigation was that total score on the AJFAT accurately identified functional limitations in 100% of participants with FAI. Clinicians might use AJFAT scores to identify functional limitations associated with FAI, as individuals with FAI and predictor scores ≥26 on the AJFAT likely have some degree of functional limitations. Although not as accurate, RV time to stabilization still identified functional limitations associated with FAI. These assessments could be used as preparticipation screening assessment tools to identify functional limitations in individuals with FAI. Coordination exercises might then be recommended to increase ankle stability in individuals who have impaired scores.21,25 Correctly identifying and rehabilitating FAI in physically active individuals is paramount for improving feelings of ankle stability21,22 and preventing ankle sprain injuries.22, 32–35.
The best cutoff score for discriminating between ankle groups is the score with the greatest accuracy.36,37 This cutoff score is represented graphically as the most “northwest” point on an ROC curve (Figure 1).36 The ROC curves plot sensitivity versus false-positive scores to determine the best cutoff score that discriminates between groups. Typically, the best cutoff score maximizes positive predictive and negative predictive scores by minimizing the sum of false-positive (individuals with stable ankles identified as having FAI) and false-negative (individuals with FAI identified as having stable ankles) scores.36 Thus, a clinical test that makes few mistakes misclassifying individuals will be accurate in discriminating between groups.
This concept is demonstrated clearly for data associated with the AJFAT, as this test has perfect accuracy. Perfect accuracy is graphically defined as the ROC curve running vertically from points 0,0 to 0,1 along the ordinate axis and then running horizontally from points 0,1 to 1,1.37 The cutoff score ≥26 is associated with positive and negative predictive scores of 1 (Figure 1). With a cutoff score ≥26, the sum of false-positive and false-negative scores is 0. As cutoff scores increase, positive predictive scores remain at 1 because no individuals with stable ankles are identified as having FAI (Figure 2). However, negative predictive scores begin to decline as cutoff scores increase, mainly due to the number of false-negative scores increasing (Figure 2). Consequently, the sum of false-positive and false-negative scores increases, indicating that greater cutoff scores are not optimal in discriminating between groups. Thus, a cutoff score ≥26 is the most accurate score for discriminating between ankle groups.
Identifying a clinically appropriate cutoff score for identifying functional limitations is more difficult with RV time to stabilization. A score ≥1.58 seconds is the best cutoff score (based on our definition of a best cutoff score) for discriminating between ankle groups. A score ≥1.58 seconds minimizes the sum of false-positive and false-negative scores, yet 5 individuals with FAI were identified as having stable ankles and 4 individuals with stable ankles were identified as having FAI (Figure 3). With certain clinical scenarios, clinicians might choose a cutoff score with high sensitivity and a high false-positive score to capture their target clinical population.36 For example, a clinical goal might be to recommend coordination rehabilitation to prevent ankle sprains in individuals with FAI who have functional limitations as measured by time to stabilization. Clinicians might place more importance on correctly identifying functional limitations in a greater number of individuals with FAI, thereby misclassifying a fair number of individuals with stable ankles as having FAI. As a result, a better cutoff score might be ≥1.14 seconds, even though the sum of false-positive and false-negative scores is not minimized. Identifying individuals with FAI and a cutoff score ≥1.14 seconds for the purpose of injury prevention rehabilitation would be achieved to a greater extent than with a cutoff score ≥1.58 seconds, as the number of individuals with FAI excluded from rehabilitation would be minimized. Because coordination rehabilitation has prevented ankle sprains in individuals with or without a history of ankle sprains,32–35 individuals with stable ankles who are misclassified as having functional limitations associated with FAI might actually benefit from injury prevention rehabilitation.
Our overall purpose was to determine the assessment tool that best discriminated between individuals with FAI and individuals with stable ankles. The AUC is an indicator of the discrimination performance of an assessment, as the probability that randomly chosen individuals will be correctly identified is equivalent to the value of the AUC.37,38 The AJFAT outperformed the RV time to stabilization in discriminating between ankle groups, because the AJFAT had an AUC of 1.0 and RV time to stabilization had an AUC of 0.72. Traditionally, an academic point scale is used to classify the accuracy, or performance, of a test based on the AUC (.90 to 1.00 = excellent, .80 to .89 = good, .70 to .79 = fair, .60 to .69 = poor, .50 to .59 = fail).37–39 This point scale indicates that the AJFAT is an excellent tool for discriminating between ankle groups, whereas RV time to stabilization is a fair discrimination test. Furthermore, a test performs better than another test when one ROC curve lies above and to the left of another ROC curve.37,39 The ROC curve of the AJFAT lies above and to the left of the RV time to stabilization ROC curve, so we conclude that the AJFAT performs better than the RV time to stabilization in discriminating between ankle groups.
In our current investigation, the cutoff score ≥26 identified functional limitations in participants with FAI. Currently, specific cutoff scores for identifying functional limitations associated with FAI using AJFAT total score have not been reported in the literature. Our cutoff score, however, would identify functional limitations associated with FAI as measured by total score on the AJFAT in published investigations.16,17,21,25 We converted mean AJFAT total scores from previous reports to our scale (greater point values indicate greater functional limitations) to compare published scores with our cutoff score.16,17,21,25 Converted AJFAT total scores reported in the literature for FAI were 30.89,21 30.70,16 31,17 and 31.5525 for participants with FAI and 25.08,21 23.30,25 and 2217 for participants with stable ankles. All values for FAI groups reported in literature were above 26,16,17,21,25 and AJFAT total scores for stable ankle groups were lower than 26.21,25 Interestingly, researchers have reported that participants with FAI who performed coordination training improved posttest AJFAT total score over baseline scores by 51%21 and 25%,25 whereas participants with stable ankles have improved posttest scores over baseline scores by 27%21 after coordination training. Although authors have reported that the AJFAT total score for participants with FAI dropped below a cutoff score of 26 after coordination training,21,25 no evidence indicates that lowering these cutoff scores decreases the frequency of giving way or the incidence of ankle sprain. Scores below a cutoff score of 26 suggest, however, that functional ability assessed with the AJFAT improves after coordination training.
Our study has limitations that affect the interpretation of our results. We identified individuals with FAI and stable ankles before their participation in this study by using frequency of giving way and frequency of ankle sprain as criteria. Retrospective collection of data could have introduced variability, as participants might not have accurately recalled frequency data and functional limitations on the AJFAT. Furthermore, our results are spectrum biased, as no participants in this investigation had an ankle injury similar to FAI, such as an acute lateral ankle sprain or tendinitis. Our assessments might help clinicians to identify impaired individuals with FAI, but the assessments really evaluate functional limitations of the ankle. Functional limitations associated with FAI could be similar to functional limitations associated with other ankle injuries. Therefore, clinicians should continue to take a history of frequency of giving way and frequency of ankle sprain to assess FAI and not limit their diagnosis to total score on the AJFAT or RV time to stabilization.
Conclusions
The AJFAT was an excellent assessment tool for discriminating between FAI and stable ankles, whereas RV time to stabilization was a fair assessment tool. The AJFAT, however, more accurately discriminated between groups than RV time to stabilization. These results are clinically relevant, as clinicians might be able to prevent ankle sprains by rehabilitating individuals with FAI who are assessed correctly as having functional limitations. However, clinicians should rule out other ankle injuries before designing a rehabilitation protocol, as misclassification of an individual with an ankle injury other than FAI might result in an ineffective rehabilitation. Future researchers should cross-validate our findings in a prospective study by examining patients with FAI, as well as patients with other conditions of the ankle.
References
- 1.Bahr R, Karlsen R, Lian O, Ovrebø R.V. Incidence and mechanisms of acute ankle inversion injuries in volleyball: a retrospective cohort study. Am J Sports Med. 1994;22(5):595–600. doi: 10.1177/036354659402200505. [DOI] [PubMed] [Google Scholar]
- 2.McKay G.D, Goldie P.A, Payne W.R, Oakes B.W. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yeung M.S, Chan K.M, So C.H, Yuan W.Y. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyle J, Negus V. Joint position sense in the recurrently sprained ankle. Aust J Physiother. 1998;44(3):159–163. doi: 10.1016/s0004-9514(14)60375-5. [DOI] [PubMed] [Google Scholar]
- 5.Forkin D.M, Koczur C, Battle R, Newton R.A. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23(4):245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- 6.Freeman M.A. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669–677. [PubMed] [Google Scholar]
- 7.Fridén T, Zätterström R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17(1):118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- 8.Garn S.N, Newton R.A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1988;68(11):1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- 9.Glick J.M, Gordon R.B, Nishimoto D. The prevention and treatment of ankle injuries. Am J Sports Med. 1976;4(4):136–141. doi: 10.1177/036354657600400402. [DOI] [PubMed] [Google Scholar]
- 10.Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21(4):206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- 11.Ryan L. Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Aust Physiother. 1994;40(1):41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- 12.Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7(5):291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- 13.Freeman M.A, Dean M.R, Hanham I.W. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 14.Goldie P.A, Evans O.M, Bach T.M. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75(9):969–975. [PubMed] [Google Scholar]
- 15.Brown C, Ross S.E, Mynark R, Guskiewicz K.M. Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J Sport Rehabil. 2004;13(2):122–134. [Google Scholar]
- 16.Ross S.E, Guskiewicz K.M. Examination of static and dynamic postural stability in individuals with functionally stable and unstable ankles. Clin J Sport Med. 2004;14(6):332–338. doi: 10.1097/00042752-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Ross S.E, Guskiewicz K.M, Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J Athl Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 18.Wikstrom E.A, Tillman M.D, Borsa P.A. Detection of dynamic stability deficits in participants with functional ankle instability. Med Sci Sports Exerc. 2005;37(2):169–175. doi: 10.1249/01.mss.0000149887.84238.6c. [DOI] [PubMed] [Google Scholar]
- 19.Docherty C.L, Arnold B.L, Gansneder B.M, Hurwitz S, Gieck J. Functional-performance deficits in volunteers with functional ankle instability. J Athl Train. 2005;40(1):30–34. [PMC free article] [PubMed] [Google Scholar]
- 20.Hale S.A, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 21.Rozzi S.L, Lephart S.M, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29(8):478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 22.Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33(12):1991–1998. doi: 10.1097/00005768-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Gribble P.A, Hertel J, Denegar C.R, Buckley W.E. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PMC free article] [PubMed] [Google Scholar]
- 24.Hubbard T.J, Kaminski T.W, Vander Griend R.A, Kovaleski J.E. Quantitative assessment of mechanical laxity in the functionally unstable ankle. Med Sci Sports Exerc. 2004;36(5):760–766. doi: 10.1249/01.mss.0000126604.85429.29. [DOI] [PubMed] [Google Scholar]
- 25.Ross S.E, Guskiewicz K.M. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med. 2006;16(4):323–328. doi: 10.1097/00042752-200607000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16(1):64–66. [PubMed] [Google Scholar]
- 27.Bernier J.N, Perrin D.H, Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32(3):226–232. [PMC free article] [PubMed] [Google Scholar]
- 28.Kaminski T.W, Perrin D.H, Gansneder B.M. Eversion strength analysis of uninjured and functionally unstable ankles. J Athl Train. 1999;34(3):239–245. [PMC free article] [PubMed] [Google Scholar]
- 29.Demeritt K.M, Shultz S.J, Docherty C.L, Gansneder B.M, Perrin D.H. Chronic ankle instability does not affect lower extremity functional performance. J Athl Train. 2002;37(4):507–511. [PMC free article] [PubMed] [Google Scholar]
- 30.Munn J, Beard D.J, Refshauge K.M, Lee R.Y. Do functional-performance tests detect impairment in subjects with ankle instability? J Sport Rehabil. 2002;11(1):40–50. [Google Scholar]
- 31.Ross S.E, Guskiewicz K.M. Time to stabilization: a method for analyzing dynamic postural stability. Athl Ther Today. 2003;8(3):37–39. [Google Scholar]
- 32.Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13(4):259–262. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- 33.Wester J.U, Jespersen S.M, Nielsen K.D, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23(5):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 34.Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32(6):1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 35.McGuine T.A, Keene J.S. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 36.Sackett D.L, Haynes R.B, Guyatt G.H, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1991. pp. 83–118. [Google Scholar]
- 37.Lasko T.A, Bhagwat J.G, Zou K.H, Ohno-Machado L. The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform. 2005;38(5):404–415. doi: 10.1016/j.jbi.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 38.Hanley J.A, McNeil B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 39.Sung M.M, Kim H.J, Kim E.K, Kwak J.Y, Yoo J.K, Yoo H.S. Clinical evaluation of JPEG2000 compression for digital mammography. IEEE Trans Nucl Sci. 2002;49(3):827–832. [Google Scholar]