Abstract
Context:
Athletic trainers must have sound evidence for the best practices in treating and preventing heat-related emergencies and potentially catastrophic events.
Objective:
To examine the effectiveness of a superficial cooling vest on core body temperature (Tc) and skin temperature (Tsk) in hypohydrated hyperthermic male participants.
Design:
A randomized control design with 2 experimental groups.
Setting:
Participants exercised by completing the heat-stress trial in a hot, humid environment (ambient temperature = 33.1 ± 3.1°C, relative humidity = 55.1 ± 8.9%, wind speed = 2.1 ± 1.1 km/hr) until a Tc of 38.7 ± 0.3°C and a body mass loss of 3.27 ± 0.1% were achieved.
Patients or Other Participants:
Ten healthy males (age = 25.6 ± 1.6 years, mass = 80.3 ± 13.7 kg).
Intervention(s):
Recovery in a thermoneutral environment wearing a cooling vest or without wearing a cooling vest until Tc returned to baseline.
Main Outcome Measure(s):
Rectal Tc, arm Tsk, time to return to baseline Tc, and cooling rate.
Results:
During the heat-stress trial, Tc significantly increased (3.6%) and, at 30 minutes of recovery, Tc had decreased significantly (2.6%) for both groups. Although not significant, the time for return to baseline Tc was 22.6% faster for the vest group (43.8 ± 15.1 minutes) than for the no-vest group (56.6 ± 18.0 minutes), and the cooling rate for the vest group (0.0298 ± 0.0072°C/min) was not significantly different from the cooling rate for the no-vest group (0.0280 ± 0.0074°C/min). The Tsk during recovery was significantly higher (2.1%) in the vest group than in the no-vest group and was significantly lower (7.1%) at 30 minutes than at 0 minutes for both groups.
Conclusions:
We do not recommend using the cooling vest to rapidly reduce elevated Tc. Ice-water immersion should remain the standard of care for rapidly cooling severely hyperthermic individuals.
Keywords: hyperthermia, hypohydration, heatstroke
Key Points
Applying a cooling vest to a hyperthermic individual did not increase the cooling rate.
A cooling vest did not rapidly reduce an elevated core body temperature.
Ice-water immersion remains the best method of rapidly cooling severely hyperthermic individuals.
An inherent risk of dehydration and hyperthermia leading to exertional heat illness exists when healthy individuals are physically active in hot, humid environments.1 An athletic trainer's ability to recognize and manage heat-related emergencies is crucial in preventing catastrophe. Exertional heatstroke, which is the most serious exertional heat illness, is a life-threatening medical emergency characterized by progressive weakness, fatigue, and hyperthermia.2 Hyperthermia, or elevated core body temperature, is common in individuals exercising in hot, humid environments. However, when core body temperature (Tc) is elevated above thermoregulatory capacity, it has a severe effect on the central nervous system and can be fatal.3 Researchers1,3–32 have investigated methods of rapidly cooling Tc to determine the most effective method that athletic trainers and other health care professionals can use to cool hyperthermic individuals.
Ice-water immersion is the standard of care for rapidly reducing Tc in hyperthermic individuals.1–3,8,9,13 However, an array of adjunctive cooling methods have emerged in sports medicine. Some of these cooling methods include water spray,6,23,28 warm-air spray,6 face fanning,16,20,23,28 helicopter rotary-blade downdraft,29 whole-body liquid cooling garments,4,11,12 ice towels,20 head-cooling units,7,10,14,24 and cooling vests.17,21,25,26,30–34 These adjunctive cooling methods often are marketed as, and mistaken for, effective ways to rapidly reduce Tc.
Microclimate cooling systems are cooling methods designed to remove heat from the skin using cooled air, circulating cooled liquid, or gel or ice-pack vests.4 These commercially available systems have been developed and marketed to athletes and athletic trainers as products that “reduce the risk of heat stress and heat related injuries and illnesses by reducing core body temperature and heart rate either during or following work in hot environments.”33 Insufficient research is available on the effects that microclimate cooling garments have on the evaporative cooling and thermoregulatory effectiveness. The testing that researchers33 have conducted has been task specific (primarily military-operation specific), making generalization of findings to athletic applications difficult.
More evidence of the effectiveness of microclimate cooling products in rapidly cooling hyperthermic individuals is needed to provide practitioners with information on the best evidence-based clinical practice for cooling individuals experiencing dangerously elevated Tc. The purpose of our study was to determine the effectiveness of a cooling vest on Tc and skin temperature (Tsk) after dehydration and hyperthermia induced by exercise in a hot, humid environment.
Methods
Participants
We recruited 10 healthy male volunteers (age = 25.6 ± 1.6 years, mass = 80.3 ± 13.7 kg) from the surrounding community. Height data for the participants was not obtained. They completed a health and injury questionnaire during a familiarization session. Potential participants were excluded if they had a history of heat-induced illness; chronic health problems; orthopaedic limitations; or diagnosis of cardiovascular, metabolic, or respiratory disease within the past year. Female participants were excluded because of the body temperature and fluid balance fluctuations associated with the physiology of the menstrual cycle. Participants read and signed informed consent forms. The investigation was approved by the Florida International University institutional review board.
Research Design
We conducted a randomized control pretest-posttest investigation with 2 experimental groups. We measured the dependent variables before and after the heat-stress trial and at recovery. All participants performed a heat-stress trial designed to produce a dehydrated and hyperthermic condition. Upon completion of the heat-stress trial, participants were assigned randomly to either rest for a minimum of 30 minutes while wearing a cooling vest (vest group, n = 5) or rest in a controlled condition without wearing a cooling vest (no-vest group, n = 5) until baseline Tc was reached. Dependent variables were Tc before, during, and after the heat-stress trial and at recovery; Tsk; time to return to baseline Tc; and core body cooling rate during the recovery period. Descriptive variables were percentage of body mass lost, urine color, specific gravity of urine, and environmental conditions (ambient temperature and relative humidity).
Instruments
Microclimate Cooling Vests
Participants assigned to the vest group were fitted with HeatShield cooling vests (ClimaTech Safety, Inc, White Stone, VA) during the recovery period immediately after the heat-stress trial (Figure 1). This microclimate superficial cooling garment consists of an outer shell made of INDURA Ultra Soft (Westex, Inc, Chicago, IL) fireproof, cotton-blend fabric. Beneath this outer shell lie a radiant heat-reflective material, a layer of insulation, the patented synthetic ice core, and a hydrophobic quilted layer next to the body. The cooling vest is designed for firefighters, hazardous materials teams, and mobile personnel exposed to extreme heat conditions. For athletes, the cooling vest is designed to be worn continuously during recovery and not during exercise. Following the manufacturer's instructions, we charged the cooling vest by placing it in a standard household freezer at its lowest setting for 5 to 6 hours. After it was charged, the cooling vest was fitted over a T-shirt; was adjusted for comfort; and was fastened with self-adhesive straps for a snug fit, overlapping straps as necessary. According to the manufacturer, the cooling vest can maintain a comfortable 21.1°C (70°F) environment in 37.8°C (100°F) conditions for approximately 3.5 hours.33
Figure 1. The HeatShield cooling vest.33.

Thermoregulatory Responses
The Tc and Tsk were measured to identify the hyperthermic condition and to monitor the participants during the recovery period. The Tc was measured using a rectal probe (YSI 401 series; Yellow Springs Instruments, Inc, Dayton, OH). The Tsk was determined using a skin thermistor (model 408/708; Yellow Springs Instruments, Inc) placed on the lateral aspect of the upper arm at the mid-humerus and secured with elastic tape. The reusable temperature probes were calibrated using standards traceable to the US National Institute of Standards and Technology and carried the CE mark (certified to the Medical Device Directive [MDD] 93/42/EEC).35 The cooling rate was calculated as the difference in Tc from 0 to 30 minutes of the recovery period.
Hydration Status
Dehydration was determined by measuring body mass, urine color, and specific gravity of urine. Body mass was measured using a digital medical platform scale (model BWB-800S; Tanita, Inc, Brooklyn, NY) and was calibrated with certified weights before each data-collection session. Nude body mass was determined after participants entered a private room, disrobed, and stood on the scale while the investigator read the remote display attached to a cord placed under the door. Clothed body mass was determined with participants wearing running clothes, a heart-rate monitor (model S210; Polar Electro, Inc, Woodbury, NY), and skin thermistors. Participants wore nylon mesh shorts, socks, and running shoes to minimize the amount of sweat trapped in the clothing. Percentage of body mass lost was calculated from the nude pre-exercise and postexercise body mass measurements.
Specific gravity of urine was measured using a clinical refractometer (model 300CL; ATAGO Co, Inc, Tokyo, Japan). Calibration of the clinical refractometer was performed before the first sample following the manufacturer's instructions. We determined urine concentration by matching the participant's urine color with the closest shade recorded on a urine color chart.2 Specific gravity and color of urine are considered valid and reliable indicators of urine concentration.2
Environmental Conditions
Environmental conditions were monitored throughout the heat-stress trial and recovery periods. We used a digital environmental monitoring device (thermohygrometer model PTH8709K; Mannix Testing & Measurement, Inc, Lynnbrook, NY) similar to those devices readily available to athletic trainers in the field to measure ambient temperature and humidity. Before each data-collection session, we calibrated the monitor by using the calibration salts according to the manufacturer's instructions. The digital monitoring device has a temperature range of −10°C to 50°C and is accurate to ±1°C, and it has a relative humidity range of 5% to 95% and is accurate to ±5%. Wind speed was measured using an electronic anemometer (Kestrel 3000; Richard Paul Russell Limited, Lymington, United Kingdom).
Experimental Procedures
Familiarization Session
Potential participants reported to the research laboratory for a familiarization session the day before testing. We recorded demographic information and baseline nude body mass for those chosen during this session for participation in the study. Participants received several instructions: (1) return to the laboratory at 9:30 am the following day wearing an athletic supporter, mesh shorts, a cotton T-shirt, sweat socks, and running shoes; (2) consume a light breakfast of a bagel or toast and a small glass of juice; and (3) abstain from ingestion of alcohol, caffeine, and nonprescription medication and dehydrating behaviors (sauna, diuretics, sweat suits, etc) for the duration of the study.
Heat-stress Trial
Upon arrival at the laboratory for testing, participants completely voided urine, and we recorded nude body mass, urine color, and specific gravity of urine. A euhydrated (normally hydrated) body mass was confirmed as less than ±1% of body mass recorded during the familiarization session. Participants performed the heat-stress trial (mean = 67.0 ± 10.6 minutes, range = 55 to 85 minutes) in a hot, humid environment until they achieved the criterion dehydration of 3.0% (actual = 3.27 ± 0.1%) loss of body mass and hyperthermia (Table 1). The heat-stress trial consisted of exercise on a motor-driven treadmill (Proform model PFTL38580; ICON Health & Fitness, Logan, UT) located outdoors under the sun in a hot, humid, subtropical climate (ambient temperature = 33.1 ± 3.1°C, relative humidity = 55.1 ± 8.9%, wind speed = 2.1 ± 1.1 km/h). The trial commenced with a 5-minute warm-up at 40% of each participant's age-predicted heart rate range (target heart rate = 131 ± 27 beats/min). Treadmill speed then was increased, and participants exercised at 60% of the age-predicted heart rate range (target heart rate = 145.7 ± 5.9 beats/min). A 60-second rest was administered after every 15 minutes of exercise. As safety precautions, we monitored heart rate and mean arterial pressure after every 15 minutes of exercise, and we monitored Tc every 5 minutes during exercise. Following the protocol of our institutional review board, if Tc were to exceed 39.0°C, we were prepared to terminate the heat-stress trial and immediately implement the emergency protocol, including cold-water immersion and activation of emergency medical systems. However, none of our participants experienced this elevated Tc. We used Tc (Table 1) and Tsk (Table 2) for the first (0 minutes) and last complete data point (60 minutes) of the heat-stress trial for data analysis.
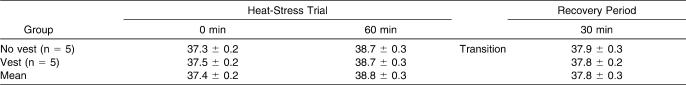
Table 1.
Mean Core Body Temperature (± SD) During the Heat-Stress Trial and Recovery Period for Vest and No-Vest Groups (°C)
Table 2.
Mean Skin Temperature (± SD) During the Heat-Stress Trial and Recovery Period for Vest and No-Vest Groups (°C)
Transition and Recovery Period
After the heat-stress trial, participants transitioned to recovery as quickly as possible by removing all clothing, toweling dry, and voiding urine, and we confirmed the criterion body mass loss of at least 3% with color and specific gravity of urine. The recovery period consisted of dehydrated and hyperthermic participants resting supine or seated in a thermoneutral environment (ambient conditions = 26.6 ± 2.2°C, relative humidity = 55.4 ± 5.8%) until baseline Tc was reached (mean time to baseline = 50 ± 17 minutes, range = 30 to 80 minutes). During recovery, participants assigned to the cooling-vest group rested with the vest over a dry T-shirt, while the no-vest group rested in their exercise clothes. We used Tc (Table 1) and Tsk (Table 2) from the transition from the heat-stress trial for the first data point (0 minutes) and the last complete data point (30 minutes) of recovery for data analysis. At the conclusion of the data-collection session, normothermic dehydrated participants were required to orally rehydrate with cool water until they returned to within 2% of their pre-exercise body mass.
Statistical Analysis
We used a 2 (vest and no-vest conditions) × 3 (0 minutes, transition after 60 minutes of the heat-stress trial, and at 30 minutes of recovery) analysis of variance with repeated measures on the second factor on Tc and Tsk. Bonferroni adjustments for repeated measures were used to prevent inflation of the alpha. We performed independent t tests to identify significant differences between groups on the time to return to baseline Tc and cooling rate during the recovery period. Descriptive statistics were calculated for the hydration status and environmental conditions measures. Data were analyzed using SPSS (version 13.0 for Windows; SPSS Inc, Chicago, IL), and significance was set at P ≤ .05 for all analyses.
Results
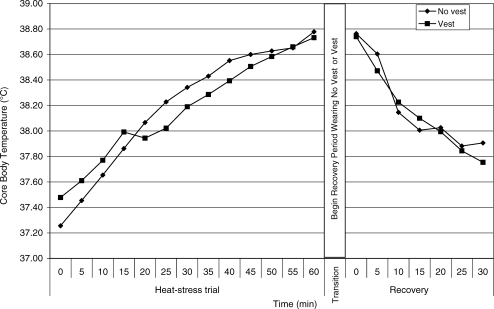
Mean Tc comparisons were performed for the vest and no-vest groups for the heat-stress trial, transition, and recovery periods (Figure 2). During the heat-stress trial, Tc was not significantly different between groups (F1,8 = 0.018, P = .897, power = .052) but was significantly different (F2,16 = 140.998, P ≤ .001) over time. Compared with 0 minutes, Tc had increased by 3.6% at 60 minutes of the heat-stress trial and had decreased by 1.2% at 30 minutes of recovery. The Tc after 30 minutes of recovery was also 2.6% lower than after 60 minutes of the heat-stress trial for both groups. Although not significant (t8 = 1.219, P = .258), the time for return to baseline Tc during the recovery period was 22.6% faster for the vest group (43.8 ± 15.1 minutes) than for the no-vest group (56.6 ± 18.0 minutes). Likewise, the cooling rate (rate of Tc decrease) during the recovery period was not significantly different (t8 = .830, P = .830) for the vest group (0.0298 ± 0.0072°C/min) than for the no-vest group (0.0280 ± 0.0074°C/min).
Figure 2. Core body temperature of participants during the heat-stress trial and recovery while wearing no vest or vest.
Mean Tsk comparisons were performed for the vest and no-vest groups for the heat-stress trial, transition, and recovery periods (Figure 3). The Tsk during the heat-stress trial was not significantly different between groups (F1,8 = 0.075, P = .791, power = .057) but was significantly increased (F2,16 = 30.507, P ≤ .001) across time. From 0 minutes to 60 minutes of the heat-stress trial, Tsk increased 5.0%. From 60 minutes of the heat-stress trial to 30 minutes of recovery, Tsk decreased 8.4%.
Figure 3. Skin temperature of participants during the heat-stress trial and recovery while wearing no vest or vest.
Discussion
By examining the efficiency of a microclimate cooling vest on reducing Tc after active dehydration and hyperthermia induced by exercising in a hot, humid environment, we determined the thermophysiologic effect and clinical application of this vest on the prevention and treatment of mild hyperthermia. Because various adjunctive cooling therapies are available, athletic trainers should be knowledgeable of the best clinical practice for rapidly cooling hyperthermic athletes experiencing exertional heat illnesses.
Our findings do not support the use of the microclimate cooling vest for the rapid reduction of Tc in mildly hyperthermic individuals. Participants in the vest group had reduced Tc in a shorter period than participants in the no-vest group, but the findings were not significant. In addition, the time to recovery recorded for the vest group would not be efficient for treating an athlete with dangerously high Tc; a rapid cooling method, such as cold-water immersion, would be most effective in preventing death.1–3,8,9,11,13,36–38 The duration and intensity of the exercise-induced hyperthermia determine the severity of physiologic damage that may occur. Therefore, faster reduction of the Tc to normothermic levels results in a decreased chance of the individual incurring damage to vital organs, such as the heart, brain, liver, or muscles.37
The Tsk increased as a result of the heat-stress trial and decreased to below baseline values during recovery. Reactive hyperemia during the continuous cooling of the recovery period may have occurred when participants wore the vest. The Tsk maintained between 33°C and 53°C has been associated with greater cutaneous vasodilatation and a larger heat flux from the core to the skin.4 The cooling vest provided a convective heat gradient that cooled the skin, but increased blood flow in the skin may have warmed the thin layer of the vest closest to the skin. Unlike liquid cooling garments in which re-chilled coolant is continuously perfused against the skin, the cooling vest absorbing the heat from the skin may have prevented effective cooling during the recovery period.
The Tsk decreased during the recovery period; however, it paradoxically continued to decrease beyond baseline values after 30 minutes of recovery for both groups, most likely as a result of continued whole-body evaporative cooling. According to Armstrong,2 the means by which the body regulates its temperature depends on the environment. Evaporation is the focal means of heat dissipation in a hot, dry environment, but radiation and convection account for most of the heat loss in a hot, wet environment because evaporation is hindered.2 However, in our study, the means by which Tsk was regulated was dependent on the air temperature as well as surface temperature. In addition, the ambient environment during recovery consisted of a mean temperature of 26.6 ± 2.2°C with a relative humidity of 55.4 ± 5.8%. The amount of heat that the body loses via convection increases as the air temperature decreases. Therefore, the body loses heat when Tsk is higher than the environmental temperature. One must also consider surface temperature because the temperature of surfaces in contact with the body, in this case a cooling vest, determines the body's conductive heat exchange.39 The mechanism of continued heat loss from the skin in both groups could be attributed to a combination of several factors, such as ceasing exercise; moving the participants from a hot, humid environment to a thermoneutral environment; and evaporative skin cooling.
Our evidence suggests that the cooling vest was no more effective for rapidly reducing Tc than resting in a thermoneutral environment was. Our findings support the results of other researchers4,26,31 who found that a cooling garment was not successful in rapidly decreasing elevated Tc. Based on the body of evidence that other authors1–3,5,8,9,11,13,36–38 have provided, ice-water immersion is clearly the fastest and most effective method of reducing Tc in hyperthermic individuals.
However, other researchers12,14,17,21,25 have found that some microclimate cooling garments are effective in decreasing thermal strain. For instance, Godek et al17 rapidly cooled a hyperthermic football player with ice-water-soaked vests, neck collars, and caps after his Tc rose to 40.9°C. In this case study,17 the cooling vest most likely was effective because it was soaked in ice water and ice-water-soaked garments also covered the head and neck, which is a technique very similar to that of the ice-water immersion.
Binkley et al1 stated that cooling over vital superficial blood vessels, such as those in the head and neck regions, is another means of decreasing elevated Tc when ice-water or cold-water immersion is not available. Hasegawa and associates25 found that a cooling jacket with ice packs inserted anteriorly and posteriorly effectively decreased thermal and cardiovascular strain while participants cycled in an environmental chamber. In their study, however, the cooling garment was worn during exercise, and the garment was tight fitting to the participant. In our investigation, the cooling garment was worn over a dry T-shirt, following the manufacturer's instructions, and was placed on the participant after the Tc was already elevated.
Although the use of superficial microclimate cooling garments to rapidly cool hyperthermic individuals may not be appropriate, some justification may exist in practical application. Although they did not record data on the psychological effects of cooling, researchers7,26 reported the positive psychological effects of wearing cooling garments after exercise in a hot, humid environment. The cooling vest that we used could be employed as an adjunctive cooling method when Tc levels remain normal. A proper hydration protocol should always be implemented with any cooling method to ensure athletes are hydrating properly and are not mistaking the sensation of coolness with proper fluid replacement, as the first author (R.M.L.) and colleagues26 reported. A false sense of coolness also could cause athletes to exert themselves to dangerous limits. Researchers should investigate the psychological effects that cooling may have on athletes exercising in the heat. Based upon our findings, we do not recommend using the cooling vest for an athlete experiencing signs of exertional heatstroke when elevated Tc must be reduced rapidly, and we assert that the cooling garment should not be considered a viable treatment for hyperthermia or exertional heat illness.
Conclusions
Despite our small sample size, we conclude that the cooling vest did not rapidly cool Tc. For ethical and safety concerns, the extent of this heat-stress trial was limited to elicit only mild hyperthermia of Tc less than 39.0°C. The hyperthermia achieved in our investigation was mild, was similar to that of Clapp et al3 and Clements et al,8 and did not reflect the extreme conditions in which many athletes compete. In addition, the induced hyperthermia was not as extreme as that normally found in athletes with exertional heatstroke (rectal temperatures exceeding 41.0°C).3 Based on our findings, we recommend that a cooling vest should not be used in the treatment of heatstroke. Ice-water immersion rapidly reduces Tc and should continue to be considered the best cooling method to treat an athlete who presents with hyperthermia.
Acknowledgments
ClimaTech Safety, Inc, a subsidiary of SummitStone Corporation, White Stone, VA, provided supplies and equipment to support our investigation.
References
- 1.Binkley H.M, Beckett J, Casa D.J, Kleiner D.M, Plummer P.E. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2002;37(3):329–343. [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong L.E. Performing in Extreme Environments. Champaign, IL: Human Kinetics; 2000. pp. 15–70. [Google Scholar]
- 3.Clapp A.J, Bishop P.A, Muir I, Walker J.L. Rapid cooling techniques in joggers experiencing heat strain. J Sci Med Sport. 2001;4(2):160–167. doi: 10.1016/s1440-2440(01)80026-8. [DOI] [PubMed] [Google Scholar]
- 4.Cheuvront S.N, Kolka M.A, Cadarette B.S, Montain S.J, Sawka M.N. Efficacy of intermittent, regional microclimate cooling. J Appl Physiol. 2003;94(5):1841–1848. doi: 10.1152/japplphysiol.00912.2002. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong L.E, Crago A.E, Adams R, Roberts W.O, Maresh C.M. Whole-body cooling of hyperthermic runners: comparison of two field therapies. Am J Emerg Med. 1996;14(4):355–358. doi: 10.1016/S0735-6757(96)90048-0. [DOI] [PubMed] [Google Scholar]
- 6.Weiner J.S, Khogali M. A physiological body-cooling unit for treatment of heat stroke. Lancet. 1980;1(8167):507–509. doi: 10.1016/s0140-6736(80)92764-6. [DOI] [PubMed] [Google Scholar]
- 7.Greenleaf J.E, Van Beaumont W, Brock P.J, et al. Fluid-electrolyte shifts and thermoregulation: rest and work in heat with head cooling. Aviat Space Environ Med. 1980;51(8):747–753. [PubMed] [Google Scholar]
- 8.Clements J.M, Casa D.J, Knight J.C, et al. Ice-water immersion and cold-water immersion provide similar cooling rates in runners with exercise-induced hyperthermia. J Athl Train. 2002;37(2):146–150. [PMC free article] [PubMed] [Google Scholar]
- 9.Sandor R.P. Heat illness: on-site diagnosis and cooling treatment. Physician Sportsmed. 1997;25(6):35–40. doi: 10.3810/psm.1997.06.1400. [DOI] [PubMed] [Google Scholar]
- 10.Rasch W, Cabanac M. Selective brain cooling is affected by wearing headgear during exercise. J Appl Physiol. 1993;74(3):1229–1233. doi: 10.1152/jappl.1993.74.3.1229. [DOI] [PubMed] [Google Scholar]
- 11.Costrini A. Emergency treatment of exertional heatstroke and comparison of whole body cooling techniques. Med Sci Sports Exerc. 1990;22(1):15–18. [PubMed] [Google Scholar]
- 12.Hexamer M, Werner J. Control of liquid cooling garments: technical control of body heat storage. Appl Human Sci. 1996;15(4):177–185. doi: 10.2114/jpa.15.177. [DOI] [PubMed] [Google Scholar]
- 13.Roberts W.O. Tub cooling for exertional heatstroke. Physician Sportsmed. 1998;26(5):111–112. doi: 10.3810/psm.1998.05.1669. [DOI] [PubMed] [Google Scholar]
- 14.Desruelle A.V, Candas V. Thermoregulatory effects of three different types of head cooling in humans during a mild hyperthermia. Eur J Appl Physiol. 2000;81(1–2):33–39. doi: 10.1007/PL00013794. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro Y, Seidman D.S. Field and clinical observations of exertional heat stroke patients. Med Sci Sports Exerc. 1990;22(1):6–14. [PubMed] [Google Scholar]
- 16.Germain M, Jobin M, Cabanac M. The effect of face fanning during recovery from exercise hyperthermia. Can J Physiol Pharmacol. 1987;65(1):87–91. doi: 10.1139/y87-017. [DOI] [PubMed] [Google Scholar]
- 17.Godek S.F, Bartolozzi A.R, Burkholder R, Sugarman E. Rapid cooling of an NFL defensive lineman with a core temperature of 40.9°C during a full padded practice [abstract] Med Sci Sports Exerc. 2005;37(suppl 5):S280. [Google Scholar]
- 18.Cotter J.D, Bradford C.D. Ice-based cooling does not hasten recovery or prevent heat loss activity in hot humans [abstract] Med Sci Sports Exerc. 2003;35(suppl 5):S28. [Google Scholar]
- 19.Schiller E.R, Mitchell J.B, Miller J.R, Dugas J.P, Pizza F.X. Effect of different cooling methods on thermoregulation following intermittent anaerobic exercise in the heat [abstract] Med Sci Sports Exerc. 1997;29(suppl 5):S97. [Google Scholar]
- 20.Walker S.M, Horodyski M.B, Powers M, White L.J. A comparison of three cooling methods on core body temperature [abstract] J Athl Train. 2004;39(suppl 2):S-60–S-61. [Google Scholar]
- 21.Smith J.E.W, Kovacs M.S, Strecker E, Pascoe D.D. Efficacy of aluminum weave cooling capes in reducing thermal load following exercise [abstract] Med Sci Sports Exerc. 2004;36(suppl 5):S313. [Google Scholar]
- 22.Proulx C.I, Ducharme M.B, Kenny G.P. Effect of water temperature on efficiency during hyperthermia in humans. J Appl Physiol. 2003;94(4):1317–1323. doi: 10.1152/japplphysiol.00541.2002. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell J.B, Schiller E.R, Miller J.R, Dugas J.P. The influence of different external cooling methods on thermoregulatory responses before and after intense intermittent exercise in the heat. J Strength Cond Res. 2001;15(2):247–254. [PubMed] [Google Scholar]
- 24.Bulbulian R, Shapiro R, Murphy M, Levenhagen D. Effectiveness of a commercial head-neck cooling device. J Strength Cond Res. 1999;13(3):198–205. [Google Scholar]
- 25.Hasegawa H, Takatori T, Komura T, Yamasaki M. Wearing a cooling jacket during exercise reduces thermal strain and improves endurance exercise performance in a warm environment. J Strength Cond Res. 2005;19(1):122–128. doi: 10.1519/14503.1. [DOI] [PubMed] [Google Scholar]
- 26.Lopez R.M, Eberman L.E, Cleary M.A, LaMarche B.H, Line S.M. Superficial cooling does not decrease core body temperature before, during, or after exercise in an American football uniform [abstract] J Athl Train. 2005;40(suppl 2):S-44. doi: 10.1519/JSC.0b013e3182736e5b. [DOI] [PubMed] [Google Scholar]
- 27.Dugas J.P, Mitchell J.B, McFarlin B.K, Dewalch D, McBroom M. The effect of twenty minutes of pre-exercise cooling on high-intensity running performance [abstract] Med Sci Sports Exerc. 1999;31(suppl 5):S306. [Google Scholar]
- 28.Mitchell J.B, McFarlin B.K, Dugas J.P. The effect of pre-exercise cooling on high intensity running performance in the heat. Int J Sports Med. 2003;24(2):118–124. doi: 10.1055/s-2003-38203. [DOI] [PubMed] [Google Scholar]
- 29.Poulton T.J, Walker R.A. Helicopter cooling of heatstroke victims. Aviat Space Environ Med. 1987;58(4):358–361. [PubMed] [Google Scholar]
- 30.Dale R.B, Bishop P.A, Smith J.F, et al. The effects of extrinsic cooling during intermittent exercise in the heat with American football gear [abstract] Med Sci Sports Exer. 2002;34(suppl 5):S220. [Google Scholar]
- 31.Johnson B.M, Somarriba G.A, Rhaman K.Z, Asfour S, Olvey S, Jacobs P.L. Ineffectiveness of torso cooling vests in reducing uncompensable heat stress [abstract] Med Sci Sports Exerc. 2005;37(suppl 5):S404. [Google Scholar]
- 32.Johnson E.A, Sleivert G, Cheung S.S, Wenger H. Pre-cooling decreases psychophysical strain during steady-state rowing and enhances self-paced performance in elite rowers [abstract] Med Sci Sports Exerc. 2005;37(suppl 5):S170. [Google Scholar]
- 33.ClimaTech Safety, Inc. http://www.climatechsafety.com. Accessed October 17, 2003.
- 34.Corcoran S. Why some workers boil over wearing cooling garments. Occup Health Saf. 2002;71(5):104–106. [PubMed] [Google Scholar]
- 35.YSI, Inc. http://www.ysi.com. Accessed November 10, 2005.
- 36.Casa D.J, Armstrong L.E. Exertional heatstroke: a medical emergency. In: Armstrong L.E, editor. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003. pp. 47–51. [Google Scholar]
- 37.Casa D.J, Almiquist J, Anderson S, Cleary M.A. Inter-Association Task Force on Exertional Heat Illness consensus statement. 2003. http://www.nata.org/statements/consensus/heatillness.pdf. Accessed July 15, 2007.
- 38.Casa D.J, Armstrong L.E, Ganio M.S, Yeargin S.W. Exertional heat stroke in competitive athletes. Curr Sports Med Reports. 2005;4(6):309–317. doi: 10.1097/01.csmr.0000306292.64954.da. [DOI] [PubMed] [Google Scholar]
- 39.Havenith G. Interaction of clothing and thermoregulation. Exog Dermatol. 2002;1(5):221–230. [Google Scholar]