Abstract
OBJECTIVE
To evaluate the effect of rooming-in (rather than standard nursery care) on the incidence and severity of neonatal abstinence syndrome among opioid-exposed newborns and on the proportion of mothers who retain custody of their babies at hospital discharge.
DESIGN
Retrospective cohort study.
SETTING
Lower mainland in southwestern British Columbia.
PARTICIPANTS
We selected 32 women in the city of Vancouver known to have used heroin or methadone during pregnancy between October 2001 and December 2002. Comparison groups were a historical cohort of 38 women in Vancouver and a concurrent cohort of 36 women cared for in a neighbouring community hospital.
MAIN OUTCOME MEASURES
Need for treatment with morphine, number of days of treatment with morphine, and whether babies were discharged in the custody of their mothers.
RESULTS
Rooming-in was associated with a significant decrease in need for treatment of neonatal abstinence syndrome compared with the historical cohort (adjusted relative risk [RR] 0.40, 95% confidence interval [CI] 0.20 to 0.78) and the concurrent cohort (adjusted RR 0.39, 95% CI 0.20 to 0.75). Rooming-in was also associated with shorter newborn length of stay in hospital compared with both comparison groups. Newborns who roomed in at BC Women’s Hospital were significantly more likely to be discharged in the custody of their mothers than babies in the historical cohort (RR 2.23, 95% CI 1.43 to 3.98) or the concurrent cohort (RR 1.52, 95% CI 1.15 to 2.53) were.
CONCLUSION
Rooming-in might ease opioid-exposed newborns’ transition to extrauterine life and promote more effective mothering.
RÉSUMÉ
OBJECTIF
Évaluer les effets de la cohabitation mère-nouveau-né à l’hôpital (plutôt que les soins standards en pouponnière) sur l’incidence et la sévérité du syndrome de privation néonatal chez les nouveaux-nés exposés aux opiacés et sur la proportion des mères qui conservent la garde de leur bébé au sortir de l’hôpital.
TYPE D’ÉTUDE
Étude de cohorte rétrospective.
CONTEXTE
Basses terres du sud-ouest de la Colombie-Britannique.
PARTICIPANTS
On a choisi 32 femmes de la ville de Vancouver qui avaient consommé de l’héroïne ou de la méthadone durant la grossesse, entre octobre 2001 et décembre 2002. Les groupes de comparaison étaient une cohorte antérieure de 38 femmes de Vancouver et une cohorte concomitante de 36 femmes traitées dans un hôpital communautaire du voisinage.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Le besoin d’un traitement à la morphine, la durée en jours de ce traitement et si le bébé avait quitté l’hôpital sous la garde de sa mère.
RÉSULTATS
La cohabitation s’accompagnait d’une diminution significative du besoin de traitement pour syndrome de privation néonatale par rapport au groupe traditionnel (risque relatif [RR] ajusté: 0,40, intervalle de confiance [IC] à 95%: 0,20 à 0,78) et par rapport avec la cohorte concomitante (RR ajusté: 0,39, IC à 95%: 0,20 à 0,75). La cohabitation était aussi associée à un séjour hospitalier plus court pour le nouveau-né par rapport aux 2 autres groupes de comparaison. Les bébés ayant partagé la chambre avec leur mère au BC Women’s Hospital avaient une probabilité significativement plus élevée de quitter l’hôpital sous la garde de leur mère en comparaison de la cohorte traditionnelle (RR: 2,23, IC à 95%: 1,43 à 3,98) ou de la cohorte concomitante (RR: 1,52, IC à 95%: 1,15 à 2,53).
CONCLUSION
La cohabitation avec la mère pourrait faciliter la transition du nouveau-né exposé aux opiacés vers la vie extra-utérine et promouvoir un maternage plus efficace.
The usual care provided to newborns of women known to be using methadone or heroin in North America involves admission to an intensive care nursery immediately after birth for observation, and, if needed, treatment for neonatal abstinence syndrome (NAS).1–4 Between 48% and 94% of infants exposed to opiates in utero develop clinical signs of withdrawal that manifest at 1 to 7 days of age, usually within 72 hours.1 Clinical features of neonatal opiate-abstinence syndrome include neurologic excitability, gastrointestinal dysfunction, and autonomic system disregulation.2 Treatment has traditionally had a 2-pronged approach: supportive care, including minimization of sensory stimulation and frequent small feedings of hypercaloric formula2,4; and administration of a narcotic or central nervous system depressant titrated to facilitate gradual withdrawal and management of symptoms.2,4 Physical separation from the mother has been deemed necessary for the purpose of careful observation and of maintaining the newborn in a quiet, dimly lit room. Studies in the non-addicted population have shown that separation of mother-infant dyads during the early postpartum period is detrimental to development of maternal attachment5 and predictive of infant abandonment.6,7 Having difficulty with attachment and abandonment are both hallmark behaviours of substance-using mothers.8
To date, use of sensory deprivation has not been examined as an independent predictor of reduction in severity of symptoms associated with neonatal withdrawal.9 In spite of this, rooming-in, now standard in maternity settings, is not offered to women using illicit drugs or methadone. The goal of this study was to compare the prevalence and severity of neonatal abstinence syndrome and the rates of retention of child custody between opioid-exposed newborns rooming in with their mothers and similar newborns who received standard care in intermediate-level nurseries.
METHODS
Setting
In Vancouver, BC, pregnant women who identify themselves as users of illicit drugs are referred by their primary care physicians, social workers, street nurses, alcohol or drug counselors, or themselves to a community outreach clinic (Sheway) located in the inner-city core. At Sheway, a multidisciplinary team provides routine antenatal care, medical care, advocacy for housing and financial services, and social support. Women are referred by Sheway to BC Women’s Hospital (BCWH) during the antenatal period for treatment of infection, cellulitis, intrauterine growth retardation, and stabilization of methadone dosage, as needed. The BCWH is an obstetric teaching hospital, and for the city of Vancouver, the referral centre for women using illicit drugs. A continuum of care between the clinic and hospital is ensured through close communication among nurses, physicians, and social workers at both settings, including shared-case conferences. This integrated approach to care does not exist elsewhere in Canada.
Rooming-in group
Our study cohort consisted of new mothers at BCWH who disclosed use of heroin or methadone or whose newborns were identified as exhibiting symptoms of opiate withdrawal. Rooming-in became available at BCWH in October 2001 to all women who used illicit drugs. Routine care for these mothers included instruction by nursing staff on how to care for the baby and how to identify symptoms of NAS. Nursing and medical staff assessed the parenting skills of rooming-in mothers and observed babies for symptoms of NAS. Observations were documented daily in medical records. They also consulted with mothers about their observation of NAS symptoms in their newborns. Between October 2001 and December 2002, all 32 women admitted to BCWH who used heroin or methadone roomed in with their newborns, and all their records were reviewed for this study.
Comparison groups
The first comparison group consisted of a historical cohort of all women who gave birth at BCWH between January 1999 and September 2001 before the advent of the rooming-in program (n = 110) and who disclosed use of heroin or methadone or whose babies were admitted to a level II nursery for observation of NAS symptoms. To minimize the resources needed for chart review, every third subject was selected for inclusion in the study. The final cohort consisted of 38 women. The women in this cohort had also been Sheway clients and, as such, had received the same coordinated approach to obstetric care as the study group, but had not had rooming-in.
The second comparison cohort consisted of all women (n = 36) who reported use of heroin or methadone or whose babies were admitted to a level II observation nursery for assessment or treatment of symptoms of NAS between January 1999 and December 2002 at Surrey Memorial Hospital (Surrey), a community hospital about 30 minutes’ drive from BCWH. This period coincided with the observation period of the other 2 study cohorts combined. Surrey has the only level II nursery in the suburban and rural area it serves. In Surrey, women did not have access to specialized addiction services in the community. In both comparison groups, babies were kept in a nursery, separate from their mothers during the first week of life.
Screening urine for drug metabolites was not standard practice in either of the study hospitals. Self-reported drug use has been shown to be highly correlated with positive urine screens.10–12 Women who reported use of cocaine or crack (about one third of drug-dependent women in the lower mainland region) but not opioids were excluded.
Newborns in all 3 cohorts stayed in hospital for at least a week for observation of symptoms of NAS. Pediatricians prescribed morphine if needed and titrated to control symptoms. In the rooming-in group, newborns requiring morphine roomed in with their mothers until they were weaned from morphine and were then discharged. In the comparison groups, babies continuing to exhibit symptoms of NAS after the initial observation week were transferred to a pediatric chronic care facility (Sunny Hill Hospital) where they were cared for in a low-stimulation environment and treated with morphine until symptoms of withdrawal subsided. Length of stay required for weaning from morphine ranged from 2 to 3 months.
Before starting the study, a certificate of ethical approval was obtained from the University of British Columbia Clinical Ethics Board.
Neonatal outcomes
Primary outcomes for this study included need for treatment with morphine, number of days of treatment with morphine, and discharge of babies in the custody of their mothers. Apprehension of babies by social services was based on individual social workers’ assessment of mother’s motivation and demonstrated ability to care for her newborn. Secondary outcomes included prevalence of symptoms of NAS, infants’ length of stay in hospital, weight loss greater than 10% in the first week of life, and need for admission to a level II nursery or chronic care unit.
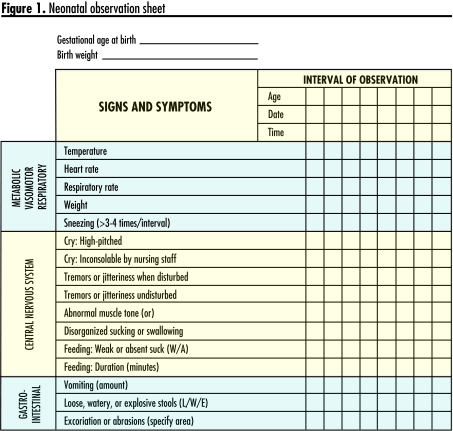
Newborns in all cohorts were monitored daily for symptoms of NAS using a modified version of the Finnigan scale.13 The Finnigan scale has an interrater reliability coefficient of 0.82 among trained nursing staff.13 It was designed to rate the severity of narcotic-withdrawal symptoms for titrating pharmacotherapy. It was validated initially in a sample of 121 physically dependent infants and has been in widespread use since evaluation of NAS symptoms.4,9 We used items measuring soother use, feeding and sucking, jitteriness, diarrhea, muscle tone, vomiting, and inconsolable crying (Figure 1). We eliminated items we thought were susceptible to observer bias, including sleeping time after feeding, disturbed Moro reflex, regurgitation, yawning, nasal stuffiness, sweating, and mottling. Babies were followed until final discharge from hospital, either the primary hospital or the chronic care hospital. Study outcomes were abstracted from hospital charts after discharge.
Figure 1.
Neonatal observation sheet
Analysis
An initial power calculation was not done, as there was no basis in experience or the literature upon which to hypothesize effect sizes in relation to rooming-in. The association between rooming-in and study outcomes was explored initially in bivariate analysis and reported as relative risks (RRs) and 95% confidence intervals (CIs) for categorical outcomes and P values derived from t tests for continuous variables. Unconditional logistic regression models were derived subsequently for each binary outcome variable by adding potential confounders one at a time to the model, retaining the one with the most important contribution as measured by the Wald statistic and then repeating the process with the remaining variables.
Factors entered into the model included ethnicity (white, First Nations, other, or unknown), involvement of birth father, support of family, housing (stable, temporary), income (employed, social assistance, reliance on partner, no source), smoking status, alcohol consumption, methadone dose at delivery (none, 10 to 29, 30 to 59, 60 to 89, and ≥90 mg), gestational age at delivery, mean number of prenatal visits, hospital antenatal admission (yes or no), and parity. Variables were retained in the logistic regression model if their inclusion changed the estimate of the odds ratio (OR) by >10%.14 Using this method, we retained at most 2 variables in each multivariate model.
We then calculated Mantel-Haenszel weighted RRs stratified on the most statistically significant variable from each multivariate analysis. We reported RRs adjusted in this fashion to avoid inflation of the ORs associated with outcomes with a prevalence of >10%.15 Multiple linear regression was used to determine the effect of study group on infant length of stay in hospital while adjusting for relevant variables in a similar fashion. Length of stay was transformed by taking the square root of observed values to approximate more closely a normal distribution. β-coefficients, standard errors, and P values were reported for variables retained in the final linear regression model.
RESULTS
Women in all 3 study cohorts were comparable in age (Table 1). Women in the rooming-in cohort were more likely to be known to be white or First Nations compared with the other cohorts for whom ethnicity was less likely to have been documented. Involvement of birth fathers and family support were more prevalent in the Surrey group. Women in the BCWH historical group were more likely to have had stable housing. More women in the Surrey group had no source of income (30.6%) compared with rooming-in mothers (3.1%) and BCWH historical-group mothers (10.5%).
Table 1.
Maternal characteristics by study cohort:Mean age of women in the BCWH group was 29.2 years (standard deviation [SD] 5.9), in the BCWH historical group was 29.8 years (SD 5.4), and in the Surrey group was 26.6 years (SD 6.7).
| CHARACTERISTICS | BCWH ROOMING IN N = 32 N (%) | BCWH HISTORICAL (NOT ROOMING IN) N = 38 N (%) | SURREY HOSPITAL (NOT ROOMING IN) N = 36 N (%) |
|---|---|---|---|
| Ethnicity | |||
| • White | 15 (46.9) | 13 (34.2) | 8 (22.2) |
| • First Nations | 12 (37.5) | 13 (34.2) | 6 (16.7) |
| • IndoCanadian | 0 | 2 (5.3) | 1 (2.8) |
| • Other | 1 (3.1) | 2 (5.3) | 2 (5.6) |
| • Unknown | 4 (12.5) | 8 (21.1) | 19 (52.8) |
| Birth father involved | 17 (53.1) | 18 (47.4) | 26 (72.2) |
| Family support | 18 (56.3) | 20 (52.6) | 26 (72.2) |
| Custody | |||
| • Custody of at least 1 child | 2 (7.7) | 5 (15.6) | 7 (22.6) |
| • Never retained custody | 18 (69.2) | 19 (59.4) | 15 (48.4) |
| • Custody of previous children unknown | 6 (23.1) | 8 (25.0) | 9 (29.0) |
| Housing | |||
| • Stable | 23 (71.9) | 19 (50.0) | 26 (72.2) |
| • Temporary or homeless | 7 (21.9) | 18 (47.4) | 7 (19.4) |
| • Unknown | 2 (6.3) | 1 (2.6) | 3(8.3) |
| Income | |||
| • Employed* | 2 (6.3) | 4 (10.5) | 4 (11.1) |
| • Social assistance | 22 (68.8) | 16 (42.1) | 21 (53.8) |
| • Reliance on partner | 4 (12.3) | 1 (2.6) | 0 |
| • No source of income | 1 (3.1) | 4 (10.5) | 11 (30.6) |
| •Unknown | 3 (9.4) | 13 (34.2) | 0 |
BCWH—British Columbia Women’s Hospital.
Includes maternity leave, disability pension, and unemployment insurance.
Smoking habits differed somewhat by study group. Women in the Surrey group were more likely to smoke, and, in particular, more likely to smoke more than 1 pack daily. Fewer women in the rooming-in group reported consumption of alcohol (18.8%) compared with women in the BCWH historical (44.7%) and Surrey (27.8%) groups (Table 2). More than 88% of women in all groups reported use of heroin, and about 20% of both the BCWH groups and 50% of the Surrey group reported use of methadone before hospital admission.
Table 2.
Pregnancy characteristics and use of substances by study cohort
| CHARACTERISTICS | BCWH ROOMING IN N = 32 N (%) | BCWH HISTORICAL (NOT ROOMING IN) N = 38 N (%) | SURREY HOSPITAL (NOT ROOMING IN) N = 36 N (%) |
|---|---|---|---|
| Smoking | |||
| • None | 7 (21.9) | 9 (23.7)) | 5 (13.9) |
| • <1 pack/d | 14 (43.8) | 11 (28.9) | 15 (41.7) |
| • ≥1 pack/d | 10 (31.3) | 9 (23.7) | 15 (41.7) |
| • Smoked, amount unknown | 1 (3.1) | 9 (23.7) | 1 (2.8) |
| Alcohol consumption | 6 (18.8) | 17 (44.7) | 10 (27.8) |
| Drug use | |||
| • Heroin | 32 (98.3) | 35 (92.1) | 32 (88.9) |
| • Methadone (before hospital admission) | 6 (18.8) | 8 (21.1) | 18 (50.0) |
| • Other opioid | 8 (25.0) | 8 (21.1) | 16 (44.4) |
| • Cannabis | 4 (12.5) | 6 (15.8) | 15 (41.7) |
| • Cocaine | 15 (46.9) | 30 (78.9) | 16 (72.2) |
| • Crack | 11 (39.3) | 16 (48.5) | 10 (29.4) |
| • Benzodiazepine | 4 (12.5) | 2 (5.3) | 3 (8.3) |
| • Other (crystal meth, ecstasy) | 2 (6.3) | 0 | 2 (5.6) |
| Daily methadone dose at delivery (mg) | |||
| • 0 | 7 (21.9) | 16 (42.1) | 19 (52.8) |
| • 1–29 | 3 (9.4) | 7 (18.4) | 3 (8.3) |
| • 30–59 | 10 (31.3) | 8 (21.1) | 5 (13.9) |
| • 60–89 | 5 (15.6) | 5 (13.2) | 3 (8.3) |
| • >90 | 7 (21.9) | 2 (5.3) | 6 (16.7) |
| Gravidy | |||
| • 1 | 6 (18.8) | 5 (13.5) | 5 (13.9) |
| • 2 | 5 (15.6) | 8 (21.6) | 9 (25.0) |
| • 3 | 3 (9.4) | 4 (10.8) | 8 (22.2) |
| • 4 | 5 (15.6) | 10 (27.6) | 5 (13.9) |
| • 5 or more | 13 (40.6) | 10 (27.0) | 9 (25.0) |
| Nulliparous | 6 (18.7) | 6 (15.8) | 5 (13.9) |
| Antenatal admission to hospital | 20 (62.5) | 22 (57.9) | 4 (11.1) |
| Breastfeeding | 20 (2.5) | 3 (7.9) | 4 (11.1) |
| MEAN (SD) | MEAN (SD) | MEAN (SD) | |
| Gestational age at first prenatal visit | 18.7 (7.0) | 20.2 (9.7) | 22.3 (8.7) |
| No. of prenatal visits | 12.2 (8.0) | 8.8 (7.8) | 5 (4.1) |
BCWH—British Columbia Women’s Hospital, SD—standard deviation
Concurrent use of crack or cocaine was common in all 3 groups, ranging from 46.9% for cocaine use in the rooming-in group to 78.9% in the BCWH comparison group. Mean number of prenatal visits was 5.0 in the Surrey group compared with 8.8 and 12.2 in the BCWH groups, where prenatal care was facilitated by the Sheway program. Also, antenatal admission to hospital was much more common in the BCWH groups. Among women who had had children previously, fewer in the rooming-in group had retained custody of at least 1 child (7.7%) than in the BCWH comparison group (15.6%) or the Surrey group (22.6%). More women in the rooming-in group were breastfeeding (62.5%) than women in the BCWH historical group (7.9%) or the Surrey group (11.1%) were.
In bivariate analysis, rooming-in was associated with substantially reduced rates of newborn treatment with morphine, length of morphine treatment, vomiting, admission to a level II nursery, and length of stay in hospital. Mothers who roomed in were substantially more likely to retain custody of their newborns (Table 3).
Table 3.
Infant outcomes by study cohort
| OUTCOMES | BCWH ROOMING IN N = 32 N (%) | BCWH HISTORICAL (NOT ROOMING IN) N = 38 N (%) | UNADJUSTED RELATIVE RISK (95% CONFIDENCE INTERVAL) | SURREY HOSPITAL (NOT ROOMING IN) N = 36 N (%) | UNADJUSTED RELATIVE RISK (95% CONFIDENCE INTERVAL) |
|---|---|---|---|---|---|
| Treated with morphine | 8 (25.0) | 21 (55.3) | 0.45 (0.23–0.87) | 19 (52.8) | 0.47 (0.24–0.93) |
| Symptoms | |||||
| • Soother use | 10 (31.3) | 9 (23.7) | 1.32 (0.61–2.84) | 5 (13.9) | 2.25 (0.86–5.90) |
| • Jitteriness | 26 (81.3) | 28 (73.7) | 1.10 (0.86–1.42) | 25 (69.4) | 1.17 (0.89–1.54) |
| • Poor sucking | 10 (31.3) | 22 (57.9) | 0.54 (0.30–0.97) | 9 (25.0) | 1.25 (0.58–2.68) |
| • Diarrhea | 3 (9.4) | 5 (13.2) | 0.71 (0.18–2.75) | 9 (25.0) | 0.38 (0.11–1.27) |
| • Vomiting | 0 | 8 (21.1) | 6 (16.7) | ||
| • Inconsolable crying | 4 (12.5) | 16 (42.1) | 0.30 (0.11–0.80) | 2 (5.6) | 2.25 (0.44–11.48) |
| Weight loss ≥10% during first week | 5 (16.6) | 2 (5.2) | 2.96 (0.62–14.28) | 2 (5.3) | 2.81 (0.59–13.5) |
| Admitted to NICU | 12 (37.5) | 34 (89.5) | 0.42 (0.26–0.66) | 30 (83.3) | 0.45 (0.28–0.72) |
| Discharged in custody of mother | 23 (71.9) | 12 (31.6) | 2.28 (1.36–3.81) | 17 (42.5) | 1.52 (1.01–2.29) |
| MEAN (SD) | MEAN (SD) | P | MEAN (SD) | P | |
| No. of days of morphine treatment | 5.9 (14.2) | 18.6 (23.4) | .007* | 18.6 (20.1) | .003* |
| No. of days in hospital | 11.8 (9.1) | 23.5 (24.6) | .014 | 25.9 (19.7) | <.001 |
BCWH—British Columbia Women’s Hospital, NICU—neonatal intensive care unit, SD—standard deviation.
Among those receiving morphine.
The adjusted RRs of requiring morphine treatment associated with rooming-in compared with standard care in a nursery were 0.40 (95% CI, 0.20 to 0.78) for the BCWH historical group and 0.39 (95% CI, 0.20 to 0.75) for the Surrey group, adjusted for maternal methadone dose at delivery (Table 4). The adjusted RRs of admission to a level II or III nursery were markedly lower in the rooming-in group than in the BCWH historical and Surrey groups (RR 0.41, 95% CI 0.25 to 0.65 and 0.45, 95% CI 0.11 to 0.57, respectively), adjusted for antepartum admission of mothers. Newborns cared for by their mothers (rooming-in) at BCWH were significantly more likely to be discharged in the custody of their mothers, adjusted for history of previous child apprehension, compared with those who were cared for in the nursery at BCWH (RR 2.23, 95% CI 1.43 to 3.98) or Surrey (RR 1.52, 95% CI 1.15 to 2.53). Stratified analysis of other binary outcome variables was precluded by small numbers in outcome categories.
Table 4.
Infant outcomes by study cohort and adjusted relative risks
| OUTCOMES | BCWH ROOMING IN N = 32 N (%) | BCWH HISTORICAL (NOT ROOMING IN) N = 38 N (%) | RELATIVE RISK (95% CONFIDENCE INTERVAL) | SURREY HOSPITAL (NOT ROOMING IN) N = 36 N (%) | RELATIVE RISK (95% CONFIDENCE INTERVAL) |
|---|---|---|---|---|---|
| Treated with morphine* | 8 (25.0) | 21 (55.3) | 0.40 (0.20–0.78) | 19 (52.8) | 0.39 (0.20–0.75) |
| Admitted to an NICU† | 12 (37.5) | 34 (89.5) | 0.41 (0.25–0.65) | 30 (83.3) | 0.45 (0.11–0.57) |
| Discharged in custody of mother‡ | 23 (71.9) | 12 (31.6) | 2.23 (1.43–3.98) | 17 (42.5) | 1.52 (1.15–2.53) |
BCWH—British Columbia Women’s Hospital, NICU—neonatal intensive care unit.
Adjusted for methadone dose at delivery.
Adjusted for postpartum admission of mother.
Adjusted for history of apprehension of a child.
Newborn length of stay in hospital (square root) was significantly shorter in the rooming-in group compared with the BCWH comparison group (β-coefficient for cohort membership 1.17, standard error 0.46, P = .01), adjusted for maternal methadone dose at delivery and involvement of the father. Length of stay (square root) was significantly predicted by cohort membership in the comparison between rooming-in and Surrey groups (adjusted β-coefficient for cohort 0.76, standard error 0.21, P = .001).
DISCUSSION
Among opiate-dependent women, rooming-in was associated with a statistically significant decrease in need for newborn treatment of neonatal abstinence syndrome, need for admission to a neonatal intensive care nursery, and mean neonatal length of stay in hospital compared with standard care in a nursery. Infants whose mothers roomed in were significantly more likely to be discharged in the custody of their mothers.
In our study, we could not separate the effects of rooming-in from those of breastfeeding, as more than 60% of women in the rooming-in group breastfed compared with about 10% in each of the comparison groups. Because breastfeeding is a desirable and natural consequence of rooming-in, separation of these effects might be of little clinical interest in most cases. The distinction between rooming-in and breastfeeding might be of interest when breastfeeding is contraindicated because mothers test positive for HIV. In our study, only 5 women (15.6%) in the rooming-in group were HIV positive.
When we restricted our analysis to non-breastfeeding women, significantly fewer of the rooming-in newborns required admission to a level II or III nursery (50%, n = 6) compared with 94.3% (n = 33) in the BCWH comparison group and 87.5% (n = 28) in the Surrey group, P < .001. Although based on small numbers and not statistically significant, observed differences in newborn length of hospital stay for rooming-in compared with the BCWH comparison and the Surrey groups (15.5 days vs 24.2 and 28.8 days, respectively) favoured the rooming-in group as did the presence of diarrhea (8.3% vs 11.4% and 18.8%) and vomiting (0 vs 20.0% and 18.8%). Our study needs to be replicated in a large sample of women who are not breastfeeding to further explore outcomes independently associated with rooming-in.
A potential outcome of breastfeeding in this population might be delayed onset of NAS.16 At BCWH, all women and their newborns discharged from the rooming-in unit are followed for at least 6 months by the medical director of the unit. None of the newborns who roomed in required readmission for symptoms of NAS. While breastfeeding is not contraindicated for mothers maintained on methadone,17 methadone levels in breast milk have not been studied in large samples. A recent study concluded, similar to other small series, that in spite of known variability in the concentration of methadone in breast milk (dependent on fat content of the milk and on sampling time), newborns exposed to the highest reported level of methadone in milk would still be ingesting methadone in the lowest dosage range recommended for neonatal withdrawal.18 Exposure to methadone through breast milk is thought to be at or below the lowest level of physiologic significance.18
Limitations
The non-random allocation of subjects to study groups was a potentially limiting factor in our study design. Subjects, however, did not choose their study groups. The historical control group consisted of a non-biased sample of all eligible women in the city of Vancouver, and the concurrent control group constituted the population of eligible women in a suburban municipality. We cannot exclude the possibility that mothers of newborns who did not exhibit signs of NAS were not included in the study. If their babies exhibited signs of NAS during the first 2 to 3 days of life, however, the mother-infant dyad was included.
Conclusion
Outcomes of pregnancies complicated by addiction are difficult to ascribe to a particular treatment because of the number and importance of potentially confounding lifestyle-related factors. Our reported findings of reduced need for treatment of NAS and retention of custody at discharge among mothers of newborns who roomed in remained statistically significant after adjustment for income, housing, social support, and use of other substances, including tobacco and alcohol. These results should encourage further study in the context of a randomized design with prognostic stratification on breastfeeding. Rooming-in, under the care of supportive nursing and medical staff, might prove to be a safe and potent tool with which to reduce the prevalence and severity of NAS and to promote more effective mothering that might ease opioid-exposed newborns’ transition to extrauterine life.
Acknowledgment
Partial funding for abstraction of data from patient charts was provided by the Department of Family Practice at the University of British Columbia in Vancouver.
EDITOR’S KEY POINTS
When a baby is born to a mother known to be using methadone or heroin, the baby is usually separated from the mother, admitted to an intensive care nursery for observation in a quiet, dimly lit environment, and treated for withdrawal if necessary. The purpose of separation and sensory deprivation, however, has not been studied as an independent predictor of improvement in neonatal withdrawal. Separation might contribute to decreased maternal attachment and neonatal abandonment.
In this retrospective cohort study of newborns of mothers using methadone or heroin, clinically relevant outcomes (treatment for neonatal withdrawal, discharge in the care of the mother) were studied in 2 groups: newborns who roomed in with their mothers or those who received traditional care in the intensive care nursery.
The researchers found that newborns who roomed in with their mothers were less likely to require treatment for neonatal withdrawal and more likely to be discharged home with their mothers. Rooming-in might promote more effective mothering and might reduce the prevalence and severity of neonatal withdrawal.
POINTS DE REPÈRE DU RÉDACTEUR
Lorsqu’un enfant naît d’une femme dont on sait qu’elle consomme de l’héroïne ou de la méthadone, il est habituellement séparé de la mère, transféré dans une pouponnière de soins intensifs pour être observé dans un milieu tranquille avec éclairage réduit et être traité pour sevrage si nécessaire. Le but de la séparation et de la privation sensorielle n’a toutefois pas été étudié comme facteur prédictif indépendant d’une amélioration du syndrome de privation. La séparation pourrait contribuer à une réduction du lien mère-enfant et à l’abandon néo-natal.
Dans cette étude de cohorte rétrospective portant sur des nouveau-nés de mères consommatrices d’hé-roïne ou de méthadone, on a examiné les résultats cliniquement pertinents (traitement pour syndrome de privation et prise en charge par la mère à la sortie de l’hôpital) auprès de 2 groupes: les nouveau-nés qui cohabitent ou ceux qui reçoivent un traitement standard dans une pouponnière de soins intensifs.
Les résultats indiquent que les nouveau-nés qui cohabitaient étaient moins susceptibles de nécessiter un traitement pour syndrome de privation et plus susceptibles de quitter l’hôpital avec leur mère. La cohabitation pourrait favoriser un maternage plus efficace et réduire la prévalence et la sévérité de l’abandon néonatal.
Footnotes
This article has been peer reviewed.
Contributors
Dr Abrahams, Ms Kelly, Ms Payne, Dr Thiessen, Ms Mackintosh, and Dr Janssen contributed to concept and design of the study; data gathering, analysis, and interpretation; and preparing the article for submission.
Competing interests
None declared
References
- 1.American Academy of Pediatrics Committee on Drugs. Neonatal drug withdrawal. Pediatrics. 1998;101:1079–88. [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics. 2001;108:776–89. [PubMed] [Google Scholar]
- 3.Theis J, Selby P, Ikizler Y, Koren G. Current management of the neonatal abstinence syndrome: a critical analysis of the evidence. Biol Neonate. 1997;71:345–56. doi: 10.1159/000244435. [DOI] [PubMed] [Google Scholar]
- 4.Kandall S. Treatment strategies for drug-exposed neonates. Clin Perinatol. 1999;26:231–43. [PubMed] [Google Scholar]
- 5.Norr K, Roberts J, Freese U. Early postpartum rooming-in and maternal attachment behaviors in a group of medically indigent primiparas. J Nurse Midwifery. 1989;34(2):85–91. doi: 10.1016/0091-2182(89)90034-7. [DOI] [PubMed] [Google Scholar]
- 6.Lvoff N, Lvoff V, Klaus M. Effect of the baby-friendly initiative on infant abandonment in a Russian hospital. Arch Pediatr Adolesc Med. 2000;154:474–7. doi: 10.1001/archpedi.154.5.474. [DOI] [PubMed] [Google Scholar]
- 7.Buranasin B. The effects of rooming-in on the success of breastfeeding and the decline in abandonment of children. Asia Pac J Public Health. 1991;5:217–20. doi: 10.1177/101053959100500305. [DOI] [PubMed] [Google Scholar]
- 8.Maza P. Boarder babies and placement in foster care. Clin Perinatol. 1999;26:201–11. [PubMed] [Google Scholar]
- 9.Suresh S, Anand K. Opioid tolerance in neonates: a state-of-the-art review. Paediatr Anaesth. 2001;11:511–21. doi: 10.1046/j.1460-9592.2001.00764.x. [DOI] [PubMed] [Google Scholar]
- 10.Dennis M, Titus J, Diamond G, Donaldson J, Godley SH, Tims FM, et al. The Cannabis Youth Treatment (CYT) experiment: rationale, study design and analysis plans. Addiction. 2002;97(Suppl 1):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- 11.Fals-Stewart W, O’Farrell T, Freitas T, McFarlin S, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patents: psychometric properties. J Consult Clin Psychol. 2000;68:134–44. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 12.Hersh D, Mulgrew C, Van Kirk J, Kranzler H. The validity of self-reported cocaine use in two groups of cocaine abusers. J Consult Clin Psychol. 1999;67:37–42. doi: 10.1037//0022-006x.67.1.37. [DOI] [PubMed] [Google Scholar]
- 13.Finnegan L, Connaughton J, Kron R, Emich J. Neonatal abstinence syndrome: assessment and management. Addict Disord. 1975;2:141–58. [PubMed] [Google Scholar]
- 14.Maldonado G, Greenland S. Simulation study of confounder selection strategies. Am J Epidemiol. 1993;138:923–36. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- 15.Altman D. Practical statistics for medical research. London, Engl: Chapman and Hall; 1991. [Google Scholar]
- 16.Malpas T. Neonatal abstinence syndrome following abrupt cessation of breastfeeding. N Z Med J. 1999;112:12–3. [PubMed] [Google Scholar]
- 17.United States Department of Health and Human Services Centre for Substance Abuse Treatment. Improving treatment for drug-exposed infants. Treatment improvement protocol series. Rockville, Md: United States Department of Health and Human Services; 1993. DHHS publication no. 93–2011. [Google Scholar]
- 18.McCarthy J, Posey B. Methadone levels in human milk. J Hum Lact. 2000;16:115–20. doi: 10.1177/089033440001600206. [DOI] [PubMed] [Google Scholar]