In 1995, Gass and Stern1 described a case of acute annular outer retinopathy (AAOR) in a patient with rapid-onset, large, dense scotoma associated with a gray intraretinal ring. Recently, Fekrat et al2 presented 4 patients with presumed AAOR and hypothesized an immune-mediated role in the pathogenesis. Concrete evidence for autoimmunity and effective therapy are needed. We report 2 patients with classic AAOR.
Report of Patients
Patient 1
A 43-year-old Japanese woman arrived at Kyorin University Hospital complaining of 1 week of painless blurry vision accompanied by a whirlpool-like pattern of light in her right eye. Her visual acuity was 20/50 OD and 20/16 OS with a relative afferent pupillary defect in her right eye. Anterior segment examination results were normal. Ophthalmoscopy revealed a whitish ring around the optic disc and a larger ring centered over the macula in the right eye (Figure 1A). The left fundus appeared normal (Figure 1B). There were no vitreous cells in either eye and fluorescein angiography results were unremarkable. Goldmann visual fields demonstrated a central scotoma in the right eye and small arcuate scotoma in the left eye (Figure 1, C and D).
Figure 1.
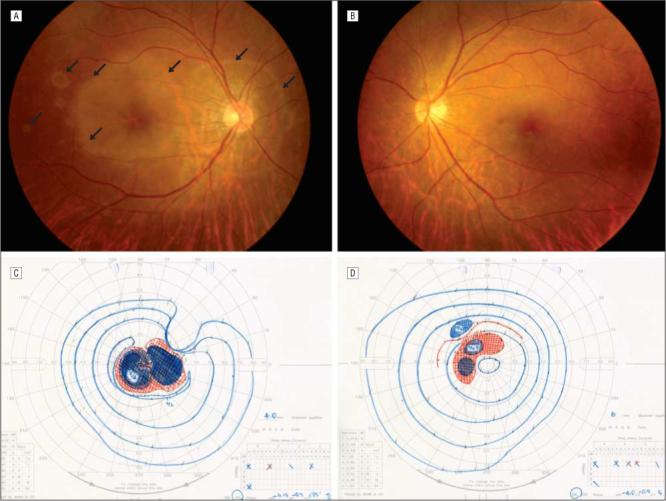
A, Fundus photograph of patient 1 at admission showing subretinal whitish-gray rings centered over the macula and the optic disc in the right eye (arrows). B, The left eye appeared normal. Goldman visual field of the patient's right (C) and left (D) eye during initial evaluation demonstrating the striking visual field deficits.
The whitish rings in the right eye faded during 2 weeks; however, the Goldmann visual fields remained unchanged. Multifocal electroretinography revealed depression of macular function in both eyes. The patient had no systemic symptoms. Results from the medical workup, which included chest radiography, Mantoux skin testing, and complete blood count, were unremarkable. Herpes viruses (simplex, varicella-zoster), Cytomegalovirus, Epstein-Barr virus, and human immunodeficiency virus serum titers were negative. Brain magnetic resonance imaging, abdominal ultrasound, and breast and gynecological examination results were also unremarkable. Treatment with 40 mg of prednisone daily was initiated 2 weeks after initial examination and tapered off during 6 months. The multifocal electroretinography appeared to improve in the left eye with therapy; however, bilateral visions, fields, and fundi appearances remained unchanged. No further deterioration was detected 18 months since halting treatment.
Serum was obtained 1 month after stopping corticosteroid treatment. Using indirect immunohistochemistry with confocal microscopy, positive reactivity was detected along the inner nuclear layers and nerve fiber layers (Figure 2). Very faint staining was also noted along the outer nuclear layers (Figure 2). In contrast, no reactivity was seen in controls with normal serum.
Figure 2.
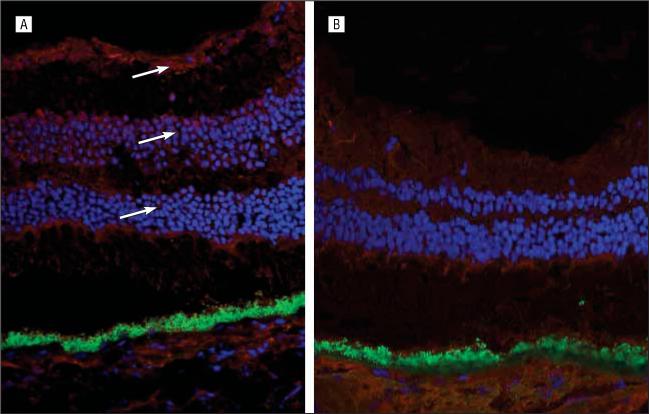
A, Indirect immunohistochemistry with confocal microscopy–enhanced imaging illustrates the positive staining (arrows) localized along the inner nuclear and nerve fiber layers. Very faint staining was also noted along the outer nuclear layers. This reaction was obtained using serum from patient 1 as the primary antibody and goat antihuman Cy3 red color as the secondary antibody on a healthy, unfixed, frozen human retina. B, There was no reaction using serum from a healthy control as the primary antibody and goat antihuman Cy3 red color as the secondary antibody on a healthy unfixed, frozen human retina (blue, 4′,6-diamidino-2-phenylindole dihydrochloride staining for nuclei; green, autofluorescent staining for retinal pigment epithelium lipofuscin; original magnification × 150).
Patient 2
A 35-year-old Japanese/African American man without significant medical history complained of several days of painless haziness and a shimmering water-droplet pattern of light in the peripheral field of his left eye. Visual acuity was 20/15 OD and 20/20 OS. A relative afferent pupillary defect was found in his left eye. Confrontational visual field showed loss of most superior and temporal fields with sparing of far temporal field in the left eye; visual field was normal in the right. Anterior segments and vitreous were normal in both eyes. Funduscopy revealed a whitish intraretinal patch along the temporal retina in the right eye and an intraretinal whitish-gray ring that traversed 360° of the midperiphery in the left eye (Figure 3). Retinal necrosis syndrome was an initial impression. Treatment with oral valacyclovir (100 mg 3 times/d) was started. Results of medical workup, including neurology consultation, brain magnetic resonance imaging, and serologies for human immunodeficiency virus 1 and 2, Cytomegalovirus, herpes simplex virus 1 and 2, hepatitis, and toxoplasmosis, were normal. The patient was then treated with 40 mg of prednisone daily. During the next 2 months, the whitish patch in his right eye became hyperpigmented. Centrally, a subretinal whitish-gray ring, which also became hyperpigmented, appeared surrounding the optic nerve and an area inferior to the fovea in the right eye. He progressed with multifocal scotomata in his right eye and an enlarging ring scotoma with preservation of a small central and 2 small peripheral islands in the left eye.
Figure 3.
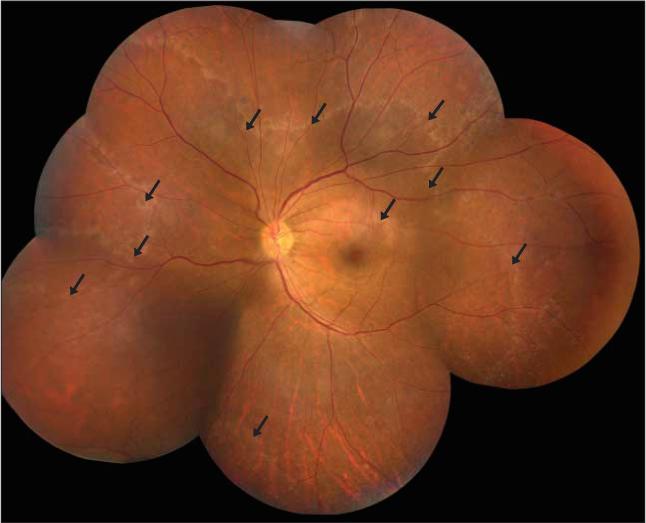
Montage of retinal photographs of the left eye of patient 2 during initial admission demonstrating a 360° subretinal whitish-gray ring along the retinal midperiphery (arrows).
The patient was referred to the National Eye Institute 3 months after initial examination. His visual acuity was 20/12.5 OD and 20/16 OS; everything else was unchanged. Fluorescein angiogram demonstrated prominent granularity of the retinal pigment epithelium in both eyes. Electroretinogram showed normal rod-mediated response in the right eye but abnormal response in the left and borderline cone-mediated response in the right eye with abnormal response in the left, which is indicative of a diffuse unilateral or markedly asymmetrical retinopathy. Both A and B waves also reduced. With indirect immunohistochemistry and confocal microscopy, strong positive reactivities were detected in the inner and outer nuclear layers with faint staining along the inner segments of the photoreceptors (Figure 4).
Figure 4.
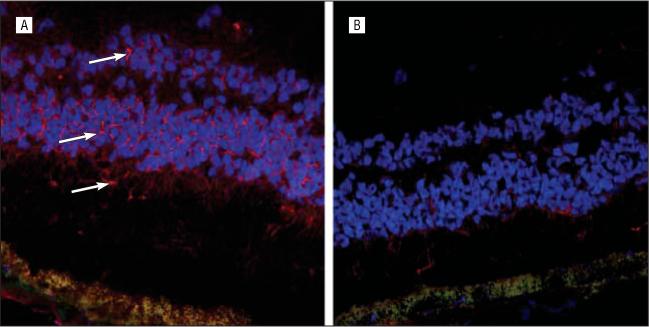
A, Using the same technique as for patient 1, indirect immunohistochemistry with confocal microscopy–enhanced imaging was performed in patient 2 and showed positive staining (arrows) with serum localized to the inner and outer nuclear layers, with faint staining along the inner segments of the photoreceptors. B, There was no definite reaction using serum from a healthy control as the primary antibody and goat antihuman Cy3 red color as the secondary antibody on a normal unfixed, frozen human retina (blue, 4′,6-diamidino-2-phenylindole dihydrochloride staining for nuclei; green, autofluorescent staining for retinal pigment epithelium lipofuscin; original magnification × 250).
Two months later, he developed a new scotoma in the right superior field and enlargement of preexisting scotomata. The small central field disappeared in the left eye and vision decreased to hand motions. Treatment with plasmapheresis was started (total of 3 cycles with 6 runs per cycle), followed by oral cyclophosphamide (150 mg daily for 9 months then tapered). In an effort to monitor preplasmapheresis and postplasmapheresis, the patient's serum reactivity against normal mouse retinal tissues was evaluated using serial 1:320 and 1:80 diluted serums (range, 1:40−1:640) preplasmapheresis and postplasmapheresis, respectively. This antibody was in the IgG class. Two years later, he was stable but without improvement on electroretinogram and without additional therapy.
Comment
In 2000, Gass3 reclassified AAOR as part of the acute zonal outer retinopathies, which are characterized by scotomata, photopsia, and absence of the appearance of fundus abnormalities, and suggested that the two may represent different manifestations of the same disease entity. Because the intraretinal ring observed in AAOR is evanescent or becomes hyperpigmented, it is possible that AAOR patients may be diagnosed with acute zonal occult outer retinopathy.2,4 Viral infection and autoimmune etiological processes have been suggested.
We detected antiretinal autoantibodies in the serum of 2 patients with AAOR and propose that autoimmunity could play a predominant role in triggering the disease. Although immune response to an occult viral or microbial infection may initiate AAOR, antimicrobial treatment would not be effective once the disease has begun. In our patients, immunosuppression seemed to stabilize their retinal function. Furthermore, our second patient benefited from plasmapheresis, which lowered antiretinal antibody levels.
Whether the serum antiretinal antibodies detected were primarily or secondarily involved in pathogenesis is not clear.5 We suspect that antiretinal antibodies could contribute to the progressive deterioration of retinal function. It is interesting that both individuals have Japanese ancestry. With the small sample size, we cannot make any generalized conclusions. Although most of the population may have circulating autoantibodies against various tissues, including retina, titer levels are low and usually do not induce disease. Further investigation to characterize specific antiretinal autoantibodies and the possible regulatory interactions between autoimmunity and zonal outer retinopathy will expand our understanding of AAOR.
Footnotes
Financial Disclosure: None reported.
References
- 1.Gass JD, Stern C. Acute annular outer retinopathy as a variant of acute zonal occult outer retinopathy. Ophthalmology. 1995;119(3):330–334. doi: 10.1016/s0002-9394(14)71176-6. [DOI] [PubMed] [Google Scholar]
- 2.Fekrat S, Wilkinson CP, Chang B, et al. Acute annular outer retinopathy: report of four cases. Am J Ophthalmol. 2000;130(5):636–644. doi: 10.1016/s0002-9394(00)00560-2. [DOI] [PubMed] [Google Scholar]
- 3.Gass JDM. Editorial: the acute zonal outer retinopathies. Am J Ophthalmol. 2000;130(5):655–657. doi: 10.1016/s0002-9394(00)00738-8. [DOI] [PubMed] [Google Scholar]
- 4.Cheung CMG, Kumar V, Saeed T, et al. Acute annular outer retinopathy. Arch Ophthalmol. 2002;120(7):993. doi: 10.1001/archopht.120.7.993. [DOI] [PubMed] [Google Scholar]
- 5.Hooks JJ, Tso MO, Detrick B. Retinopathies associated with antiretinal antibodies. Clin Diagn Lab Immunol. 2001;8(5):853–858. doi: 10.1128/CDLI.8.5.853-858.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]


