Abstract
We carried out a retrospective review of 32 consecutive patients (30 adults and two children) with total or partial lesions of the brachial plexus who had surgical repair using nerve grafting, neurotisation, and neurolysis between January 1991 and December 2003. The outcome measures of muscular strength were correlated with the type of lesion, age, preoperative time, length and number of grafts, and time to reinnervation of the biceps. The function of the upper limb was also evaluated. There was a significant correlation between muscular strength after surgical repair and both the preoperative time and the length of the nerve graft. There was also a significant correlation between muscular strength and the number of grafts. Muscular strength was better when the neurolysis was done before six months. When neurosurgical repair and reconstructive procedures were performed, the function of the upper limb was improved.
Résumé
Nous avons fait une étude rétrospective de 32 malades consécutifs (30 adultes et 2 enfants) avec une atteinte totale ou partielles du plexus brachial, après réparation chirurgicale utilisant une greffe nerveuse, une neurotization et une neurolyse entre janvier 1991 et décembre 2003. La mesure de la force musculaire a été correlée avec le type de lésion, l'âge, le délai opératoire, la longueur et le nombre des greffes, et le temps de reinervation du biceps. La fonction du membre supérieur a aussi été évaluée. Il y avait une corrélation négative significative entre la force musculaire après réparation chirurgicale et d'une part, le délai préopératoire et, d'autre part la longueur de la greffe du nerf. Il y avait aussi une corrélation positive significative entre la force musculaire et le nombre de greffes. La force musculaire était meilleure quand la neurolyse a été faite avant six mois. Quand la réparation neurochirurgicale et les procédés de reconstruction ont été exécutés, la fonction du membre supérieur était améliorée.
Introduction
Over the years, opinions concerning the treatment of lesions of the brachial plexus have changed. The last three decades nave witnessed a resurgence of interest in the pathology of the brachial plexus. The works of Seddon [14] and other authors [2, 3, 6, 7, 9–13] have demonstrated that continuity of the neural substance can be obtained with grafts, and surgeons were stimulated to consider reconstruction of traction lesions of the brachial plexus.
The development of microsurgery and the associated technology renewed interest in surgical reconstruction, and has given rise to more favourable results in comparison to earlier studies: Millesi [9], Narakas[11], and others [10–13, 16]. A careful analysis of the published literature, however, fails to offer a clear panorama of the functional results of reconstruction. The goals of the present study were to evaluate the results of surgical treatment of traumatic lesions of the brachial plexus and to identify variables with prognostic value for the outcome of surgical repair.
Materials and methods
We carried out a retrospective review of 32 consecutive patients with total or partial lesions of the brachial plexus and without spontaneous recovery of biceps after 3–6 months. The patients, with a mean age of 27.3 years (range 16–44) were treated by surgical repair from January 1991 to December 2003. The study also included 20 patients in whom various reconstructive procedures were done.
At a mean follow-up of 6.7 years, the patients underwent further independent neurological and functional evaluation that included sensibility, muscular strength, and pain, although sensibility was not included in this study. Muscular strength was recorded on the international scale of grades 0–5. The overall results were classified as functional (M5-M3), not functional (M2-M1), and not reinnervated (M0). Pain was described in terms of its time of onset, site, radiation, and relief with medication [3]; degree 0 indicated no pain, degree 1 indicated intermittent pain that was often related to the weather or to the patient's emotional state, degree 2 indicated severe pain, and degree 3 indicated intolerable pain that was sufficient to awaken the patient from sleep and could not be relieved by major analgesics [4]. The types of lesions were classified as follows: type I (C5-C6 paralysis, 11 patients), type II (C5-C6-C7 paralysis, nine patients), and type III (C5–T1 or complete paralysis, 12 patients).
The data were collected on the chart proposed by Kendall et al. [8]. The outcome measures of muscular strength were correlated with the type of lesion, age, preoperative time, length of the graft, number of grafts, and time to reinnervation of the biceps. The extent of the correlation of variables was estimated using the Spearman rank correlation method (Rs). The linear regression method was used to investigate the interactions between these variables and muscular strength. For all analyses, a p-value <0.05 for a type-1 error was considered significant. Finally, upper limb function was evaluated using the scale proposed by Narakas [11].
Results
Three types of surgical procedures were carried out: nerve grafting, neurotisation, and neurolysis. Nerve grafting was carried out in 13 cases: six between the ends of the superior trunk and seven from the C5 spinal nerve toward the suprascapular nerve. Neurotisation (with the phrenic nerve, II-III intercostal nerves, or XI cranial nerve) was carried out in 25 cases toward the musculocutaneous nerve or the musculocutaneous portion of the lateral cord. Neurolysis was carried out 15 times: six on the C7 spinal nerve, six on the C5-C6-C7 spinal nerves, two on the superior trunk, and one on the lateral cord.
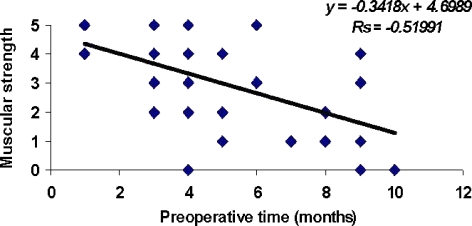
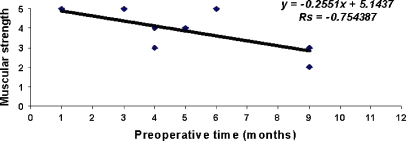
Preoperative time
To analyse the relationship between preoperative time and muscular motor recovery, we evaluated a total of 53 muscles. The average preoperative time in all cases was 5.2 months: 4.3 months for the functional group (M5-M3), 6.9 months for the non-functional group (M2-M1), and 8.4 months for the patients in whom reinnervation was not obtained (M0). There was a significant negative correlation between preoperative time and muscular strength after surgical repair (Fig. 1).
Fig. 1.
Correlation between preoperative delay and muscular strength
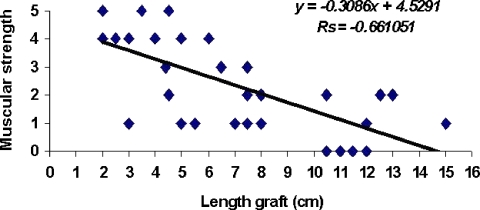
Length of the nerve grafts
We included all patients in whom we used nerve grafts to restore neural defects (simple nerve graft and nerve graft associated with neurotisation). The muscular strength of 38 muscles was evaluated: 28 biceps muscles and ten external rotators of the shoulder.
The overall average graft length was 4.5 cm. In the group with functional results (M5-M3), the average length was 3.9 cm; in the non-functional (M2-M1) group it was 6.6 cm; and in the group without reinnervation (M0), it was 9.6 cm. There was a significant negative correlation between the length of the nerve graft and muscular strength after surgical repair (Fig. 2).
Fig. 2.
Correlation between length of nerve graft and muscular strength
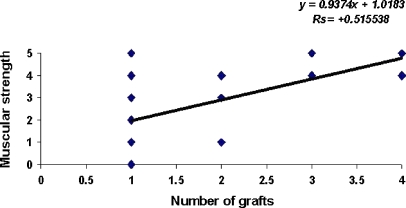
Number of implanted grafts
The average number of grafts was 1.6: in the group with functional results it was 2.4, in the not-functional group it was 1.1, and in those with no reinnervation it was 1.0. A significant positive correlation was found between the number of grafts and muscular strength (Fig. 3).
Fig. 3.
Correlation between number of nerve grafts and muscular strength
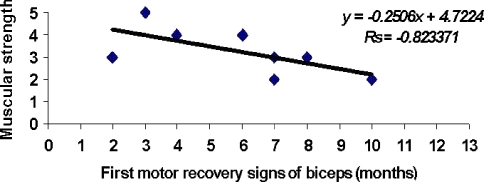
First signs of motor recovery
There was a significant negative correlation (Fig. 4) between the time of appearance of the first signs of reinnervation and the muscular strength of the biceps after surgical repair. We found no significant relationship between muscular strength and age or between muscular strength and type of lesion.
Fig. 4.
Correlation between biceps recovery (time) and muscular strength
Neurolysis
Muscular strength was better when neurolysis was done before six months. There was a negative correlation between the preoperative time and functional results (M5-M3; Rs=−0.75; Fig. 5).
Fig. 5.
Correlation between preoperative delay in neurolysis and muscular strength
Pain
Surgery modified the intensity and distribution of the pain. In nine patients the pain disappeared, 15 patients had pain of degree 1, six had pain of degree 2, and only two patients had pain of degree 3. These differences represent a significant (p=0.002) improvement and suggest that the surgical procedure has an analgesic effect [4].
Reconstructive procedures
In 20 patients we carried out the following palliative surgical procedures: flexorplasty of the elbow (11), transfer toward the shoulder (seven), arthrodesis of the shoulder (two), arthrodesis of the wrist (five), transfer of the flexor carpi ulnaris (two), and rotational transfer of the biceps for supination contracture of the forearm (one).
Functional evaluation of the upper limb
The functional results of the upper limb after neurosurgical repair were rated as follows: good in eight patients, fair in eight patients, and poor in 16 patients. When upper limb function was evaluated after further reconstructive procedures following the neurosurgical repair, the outcomes were as follows: good in 11 patients, fair in 13 patients, and poor in only eight patients.
Discussion
Evaluating outcomes of reconstructive surgery for lesions of the brachial plexus is extremely complex. The time between accident and surgical intervention is one of the more important factors and may be an important predictor of the final outcome. Kanaya et al. [7] noted that a delay of more than eight months implied a bad prognosis for functional recovery. This was the first time this had been reported for patients treated surgically for closed lesions of the brachial plexus. The authors recommended that patients be treated surgically within the first three months in order to gain a satisfactory functional recovery.
Narakas and Hentz [12] studied 114 patients treated surgically from 1970 to 1982 and found a correlation between preoperative duration and recovery. When reconstruction was delayed for more than 8–12 months, the recovery was minor, but if reconstruction was carried out before the fourth month, the functional outcome was better.
Bentolila et al. [3] pointed out that the delay between the moment of injury and the surgical intervention is one of the most important factors that presages the final outcome. They added that to obtain a satisfactory functional result, the delay should be less than four months, and no surgery using nerve grafts should be carried out after seven months if good functional results are desired.
We found that the preoperative duration inversely influenced the probability of motor recovery. This means that when the duration between the lesion's origin and the surgical intervention is long, the possibility for recovery is diminished.
Narakas and Hentz [12] also compared outcome with the length of the nerve graft. They found that the functional outcome was favourable in cases with grafts less than 5 cm but that it was less favourable in those with grafts longer than 10 cm. This corresponds with our study, in which we found that graft length inversely influenced the motor results after surgical treatment.
Comtet et al. [6] found that the correlation between the number of grafts and the functional outcome was statistically significant. In their series of 31 patients, the average number of grafts was 1.6 in patients with shortcomings and 6.2 in patients with functional results (M3-M5). In our study of 32 patients, we demonstrated a direct relationship between the number of grafts and the motor results. The motor recovery of the biceps stabilised around an average of 14 (range 8–22) months. Narakas and Hentz found that motor recovery stabilised around 18 months [12].
Kanaya et al. [7] found that neurolysis performed before six months implied a good prognosis for functional recovery. We also found that muscular strength was better when neurolysis was carried out before six months.
Pain after lesions of the brachial plexus has not received much attention. Incomplete reports of patterns of lesion and inadequate evaluations have disqualified most of these studies from being included in a comparative study. After surgery was done, we found a significant improvement in pain. This may suggest that the surgical treatment produces an analgesic effect [3, 11].
Repair of the brachial plexus is only one part of the treatment. After the nerve regeneration has been completed, any palliative surgery using all available techniques, such as tendon and muscular transfers, arthrodesis, tenodesis, etc., should be done in order to improve the functional results [1, 5, 15].
In brachial plexus lesions, paralysis of the shoulder girdle muscles is frequently associated with paralysis of the elbow flexors. In such lesions, restoration of elbow flexion depends on the stability of the shoulder and in other centers is frequently resolved by arthrodesis [13]. We only recommend shoulder arthrodesis in those patients who undergo flexorplasty of the elbow using the pectoralis and sternocleidomastoid muscles and in patients with paralysis of the trapezius and of latissimus dorsi at the same time. In other patients, we suggest doing a transfer of the trapezius or the latissimus dorsi.
When we evaluated the function of the whole upper limb, it was possible to demonstrate the value of neurosurgical repair in lesions of the brachial plexus. When reconstructive procedures were performed after the primary neurosurgical repair, the function of the upper limb was generally improved. We were unable to compare our results with other published studies because various different methods of evaluation [7, 9, 12, 14, 16] were used.
Our study has the deficiencies inherent in all retrospective reviews. The studied variables were selected because they are reliable and widely accepted. Selection bias related to surgeon preference, technical difficulty, degree of nerve injury, and number of avulsed roots may have influenced the type of surgical method selected. From the homogeneous preoperative patient population, however, we believe the selection bias to be minimal. We found that the preoperative time and the length and number of nerve grafts have a prognostic value on the outcome of surgical repair and that surgical treatment produces an analgesic effect. This study points out the benefits of surgical reconstruction of traumatic lesions of the brachial plexus.
References
- 1.Alnot JY, Abols Y (1984) Réanimation de la flexion du coude par transfers tendineux dans les paralysies traumatiques du plexus brachial de l'adulte. Rev Chir Orthop 70:313 [PubMed]
- 2.Barnes R (1949) Traction injuries of the brachial plexus in adults. J Bone Joint Surg Br 31:10–12 [PubMed]
- 3.Bentolila V, Nizard R, Bizot P, Sedel L (1999) Complete traumatic brachial plexus palsy. Treatment and outcome after repair. J Bone Joint Surg Am 81:20–28 [DOI] [PubMed]
- 4.Berman J, Anand P, Chen L, Taggart M, Birch R (1996) Pain relief from preganglionic injury to the brachial plexus by late intercostal transfer. J Bone Joint Surg Br 78:986–992 [DOI] [PubMed]
- 5.Brooks D, Seddon H (1959) Pectoral transplantation for paralysis of the flexors of the elbow: a new technique. J Bone Joint Surg Br 41:36–43 [DOI] [PubMed]
- 6.Comtet JJ, Sedel L, Fredenucci JF, Herzberg G (1988) Duchenne-Erb palsy. Experience with direct surgery. Clin Orthop 237:17–23 [PubMed]
- 7.Kanaya F, Gonzalez M, Park CM et al (1990) Improvement in motor function after brachial plexus surgery. J Hand Surg Am 15:30–35 [DOI] [PubMed]
- 8.Kendall HO, Kendall FP, Wadsworth GE (1971) Muscles—testing and function, 2nd edn. Williams & Wilkins, Baltimore
- 9.Millesi H (1977) Surgical management of brachial plexus injuries. J Hand Surg Am 2:367–378 [DOI] [PubMed]
- 10.Monreal R (1997) Nervous transfers in order to reestablish the flexión of the elbow in the lesions of the brachial plexus. Rev Cubana Ortop Traumatol 11:41–45
- 11.Narakas A (1981) The effects on pain of reconstructive neurosurgery in 160 patients with traction and/or crush injury to the brachial plexus. In: Seigfried J, Zimmerman M (eds) Phantom and stump pain. Springer, Berlin Heidelberg New York, p 126
- 12.Narakas A, Hentz V (1988) Neurotization in brachial plexus injuries. Indications and results. Clin Orthop 237:43–56 [PubMed]
- 13.Narakas A (1993) Muscle transposition in the shoulder and upper arm for sequelae of brachial plexus palsy. Clin Neurol Neurosurg 95(Suppl):89–91 [DOI] [PubMed]
- 14.Nagano T, Tsuyama N, Ochiai N et al (1989) Direct nerve crossing with intercostal nerve to treat avulsion of the brachial plexus. J Hand Surg Am 14:980–985 [DOI] [PubMed]
- 15.Seddon HJ (1963) Nerve grafting. J Bone Joint Surg Br 45:447–461 [PubMed]
- 16.Sedel L (1982) The results of surgical repair of brachial plexus injuries. J Bone Joint Surg Br 64:54–66 [DOI] [PubMed]