Abstract
This article explores trends and correlates of Chicago’s opiate-related overdose (OD) deaths. We manually examined data from every death certificate filed between 1999 and 2003 to identify all Chicago residents’ accidental deaths involving acute intoxication with illicit opiates, OD, or opiate poisoning. The analysis includes an examination of contextual characteristics in 77 Chicago neighborhoods. Negative binomial regression analysis permits the calculation of incidence rate ratios (IRR) associated with time trends. OD incidence peaked in 2000 and then declined markedly by 2003 [year 2000–2003 IRR = 0.65, 95% confidence interval (CI) (0.54, 0.78)]. Over the 2000–2003 period, overall incidence of fatal OD declined by 34%. Over this period, the sharpest observed declines occurred among African-Americans [IRR = 0.64, 95% CI (0.51, 0.81)] and Hispanics/Latinos [IRR = 0.53, 95% CI (0.32, 0.88)]. The opiate-related fatality incidence also declined among non-Hispanic whites [IRR = 0.743, 95% CI (0.52, 1.06)]. Even at the end of the study period, illicit opiate-related OD accounted for 35% of all accidental deaths to Chicago adults aged 18–64, with 45% of OD deaths occurring among African-American men. In summary, illicit opiate OD in Chicago peaked in 2000 and markedly declined by 2003. Opiate OD continues to pose a major threat of mortality to Chicago adults.
Keywords: Drug abuse, Heroin, Incidence, Overdose, Trends.
INTRODUCTION
Illicit opiate-related overdose (OD) is a leading cause of premature death among injection drug users (IDUs) in industrial democracies,1–3 rivaling both HIV/AIDS4–6 and hepatitis C7–11 in mortality attribution. Heroin—an opioid, or partly synthetic opium derivative—is the most commonly injected illicit opiate, accounting for the vast proportion of opiate-related OD deaths. Although OD incidence varies across settings, annual mortality rates among untreated opiate addicts range from 1 to 2% with higher mortality incidence in some populations.12–16 International OD death rates among opiate users range from six to 20 times greater than the norm for their drug-free peers, with accidental OD accounting for up to 45% of their deaths.17,18 Intravenous heroin use—as opposed to less lethal routes of administration such as intranasal ingestion—accounts for the vast majority of opiate-related ODs.19,20 The nationwide incidence of opiate OD deaths has shown long-term escalation, growing by 56% between 1990 and 1997.12,13,21,22 In some localities, OD death rates doubled over the same time period that death rates attributable to HIV and hepatitis C virus dropped.13
OD-related morbidity and mortality have proved especially problematic in Chicago, the third largest city in the United States. Estimates derived from the work of Holmberg (1996)23 and Friedman et al. (2004),24 combined with local publicly available data, indicate that roughly 45,000 IDUs live in Chicago,25,26 making the city home to one of the largest IDU populations in the country.1 In addition, Chicago has ranked first among major U.S. metropolitan areas in the absolute number and population rate of emergency department mentions of heroin use.27 Also, Chicago ranks second only to New York City in the absolute number of fatalities directly attributable to opiate misuse. Inmates in Chicago’s correctional facilities rank first in the nation in positive toxicology screens for opiate use.27
This article marshals death certificate data concerning Chicago residents who suffered a fatal opiate-related2 OD over a 5-year period (1999–2003). We offer a snapshot of a major public health issue affecting a marginalized and stigmatized population. Our principal research aim is to analyze these data to ascertain trends in the descriptive epidemiology of OD fatalities attributable to the use of illicit opiates. We focus on opiates and opioids because, relative to other psychoactive substances, they contribute to more accidental OD deaths.28,29
This endeavor is a first step toward achieving rational public health programming and policy decision-making, as well as more methodologically integrated research on this often overlooked cause of premature death.
BACKGROUND AND SIGNIFICANCE
Firsthand experience with OD pervades the lives of IDUs. Even when nonfatal, opiate OD can cause significant morbidity. Because IDUs constitute a “hidden” population, nonfatal OD incidence data remain sparse, although the phenomenon seems common if not “normal” among IDUs. Opiate-related emergency department visits in Chicago increased more than 95% from 1988 to 1995; more than a third of these visits involved OD.30 An even more rapid increase in reported opiate-related visits occurred between 1995 and 2002.27
Most OD deaths occur in metropolitan areas; some cities report OD death rates 65% higher than the U.S. average.22 OD deaths typically exhibit spatial clustering.22 Davidson and colleagues, for instance, report that 47% of San Francisco opiate-related OD deaths between 1997 and 2000 transpired in single-room occupancy hotels (SROs) and 36% materialized within a small central-city radius.31 Moreover, OD fatality is differentially distributed across population segments. OD fatalities affect men and women and all ethnic groups, but population fatal OD incidence is more than twice as high among men, and OD disproportionately affects non-Hispanic African-Americans as compared with non-Hispanic whites.3,12,13
Fatal opiate OD results from cardiac arrest, apnea, or circulatory collapse following excessive opiate ingestion.32–34 Fatal OD episodes usually unfold over 1 to 3 h, a period long enough to accommodate the pursuit of OD reversal methods.1,2,18 Studies indicate that most IDUs know the main physiological signals associated with imminent OD, and up to 85% of opiate ODs occur in the presence of others.18 Although studies indicate that lone IDUs face elevated risk, companions’ suboptimal response poses a key risk-factor for fatal OD.3
DATA AND METHODOLOGY
Manually screened Chicago death certificates furnish the data source for all opiate-related OD deaths considered here. Inconsistencies in the filing and coding process for death certificates3 led us to develop a case definition for opiate-OD-related death. This process yields a more sensitive case-finding process than does relying solely on coding from the 10th edition of the International Classification of Disease (ICD-10).
Case Definition
An opiate death case satisfies all of the following criteria: (1) decedent resided in the city of Chicago; (2) part 1 or part 2 of the death certificate specifically mentions acute intoxication, OD, or poisoning with opiate; (3) the Cook County Medical Examiner’s Office ruled the death accidental; (4) no physical injury causes (e.g., motor vehicle accident) appear on the certificate; and (5) the OD fatality occurred within city limits.
Case Finding
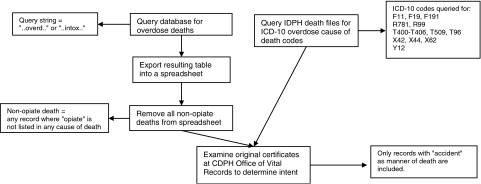
Figure 1 summarizes our data extraction process. Candidate certificates were identified in two different but linked locations: (1) the Illinois Department of Public Health (IDPH) master death files, 1999–2003, and (2) the Chicago Real Time Death Surveillance System (CRTDSS) 2003.
FIGURE 1.
Diagram of data extraction process.
The IDPH files contain demographic and cause-of-death data for Chicago residents dying anywhere in the United States. All cause-of-death and nature-of-injury data for the study period were coded to the ICD-10 standard. Underlying and contributing cause-of-death and nature-of-injury fields were queried for the values presented in Table 1. Case definition criteria were then applied to paper copies of queried candidate certificates. Eligible certificates were entered into a database. The research team supplemented this master file information with address data (i.e., residence, death scene). “Dead-on-arrival” cases were considered to have died at the location where emergency medical service professionals found them.
TABLE 1.
Values queried in cause-of-death analysis
| Category | Description |
|---|---|
| X42 | Accidental poisoning by/exposure to narcotics/psychodysleptics not elsewhere classified |
| X62 | Intentional self-poisoning by narcotics/psychodysleptics not elsewhere classified |
| Y12 | Poisoning by/exposure to narcotics/psychodysleptics not elsewhere classified, undetermined intent |
| F11 | Mental/behavior disorder due to use of opiates |
| F19 | Mental/behavior disorder due to use of multiple drugs |
| R781 | Finding of opiate in blood |
| T400 | Poisoning by opium |
| T401 | Poisoning by opiate |
| T402 | Poisoning by other opioids |
| T403 | Poisoning by methadone |
| T404 | Poisoning by other synthetic narcotic |
| T509 | Poisoning by other and unspecified drugs, medicaments, and biological substances |
By working with the CRTDSS described below, we determined that Illinois medical examiners’ certificates were often classified as R99—“other ill-defined and unspecified causes of mortality”—when, in fact, a specified cause of death was established. We therefore queried the cause-of-death and nature-of-injury fields for the R99 code and screened the relevant certificates; additional cases were then added to the database.
Our second data location is the CRTDSS. Under CRTDSS, every death certificate filed in the city (Chicago occurrence deaths) is entered into a locally maintained database containing demographic information, location of death, residential address, and verbatim text from the cause-of-death fields. A senior physician epidemiologist reviews all illegible or questionable certificates to determine final status.
To account for misspelled entries, and because the CRTDSS files are not ICD-coded, we queried the cause-of-death fields using the text string “..op..” (truncation of “opiate”). Candidate certificates were identified and screened as noted above. Data from all eligible certificates were ported into the database. To identify inconsistencies, we checked the CRTDSS file against the IDPH master file. This audit revealed two findings that led us to modify our case finding: (1) the existence of opiate-OD-related deaths classified as R99, which prompted us to modify our file query for the relevant span of years, and (2) the presence of locally filed certificates in the RTDSS that were not entered into the IDPH master file.
Throughout the case-finding process, two independent certificate reviewers worked in tandem. A senior reviewer compared their respective findings to each other and to master data sources. Inconsistencies prompted necessary changes to the data collection and entry protocols. We imported the final, cleaned database into ArcGIS and generated a point file pinned to the Chicago street grid. ArcGIS 9 facilitated our map generation (see below) and identification of incidence clusters.
Additional Data Resources
We used the IDPH master death files to obtain frequency counts of other causes of death. Population data for 2000–2003 were examined from the Census 2000 SF-1 file and the American Community Survey for 2002 and 2003. For Hispanics, non-Hispanic blacks, and non-Hispanic whites, the population changes between the 2002 and 2003 American Community Surveys and the 2000 Census were similar to or smaller than the confidence interval for the 2003 American Community Survey population estimates. We therefore used the Census 2000 SF-1 file to calculate rates for 2000–2003. All persons of Hispanic race, regardless of national origin, were assigned to the Hispanic denominator. For non-Hispanics, persons reporting single race were used as denominators for rate calculation. Two percent of Chicago non-Hispanic adults reported multiple races in the census.
Statistical Analysis
Myriad individual and community forces and conditions affect OD fatality, a relatively rare event. Existing surveillance systems observe some contributing factors, but they fail to monitor other critical determinants of OD incidence, such as local injection practices, changing demographic parameters of opiate users, drug market fluctuations, and the effects of newly introduced accelerants/enhancers (e.g., Fentanyl, a narcotic analgesic whose role in fatal OD has recently attracted widespread attention).35 To minimize the impact of unobserved heterogeneity, we use a random-effect binomial regression specification where the dependent variable is the absolute number of OD fatalities in each neighborhood and year. Such models have been widely used in health services research, such as analyses of emergency department use.36–38
The number of fatal OD events in a given neighborhood is modeled as a count variable with potential values of 0, 1, 2, etc. We use neighborhood population as a proxy for “exposure” to OD risk. We assume that, within each neighborhood, OD incidence follows a Poisson distribution. Each neighborhood acts as its “own control” in examining temporal patterns of OD mortality. This specification accounts for the rare, episodic nature of OD mortality. It also facilitates subgroup analysis on populations of special clinical or policy significance.
We assume overdispersion across neighborhoods, reflecting important unobserved heterogeneity at the neighborhood level. One important source of overdispersion arises because we cannot directly observe each neighborhood’s number of illicit opiate users. As described in detail elsewhere,34,39,40 we model this heterogeneity (and the heterogeneity that emanates from other sources) by presuming that each neighborhood carries a time invariant, although unobserved, neighborhood effect, which randomly manifests across locations according to a gamma distribution, thus allowing for local variation in OD incidence. This framework leads to the increasingly standard random effects negative binomial regression specification.
We estimated all parameters using STATA 9.0 and report all results in terms of incidence rate ratios (IRR). The interpretation of IRR is analogous to the adjusted odds ratios typically reported from binary logistic regression. For dummy variables, an IRR below 1.0 corresponds to reduced OD incidence. An IRR exceeding 1.0 indicates heightened OD mortality incidence.
RESULTS
Over the 5-year period (1999–2003), 1,260 Chicago residents suffered an accidental, fatal opiate OD. If 80% of decedents were intravenous users of opiates (most likely heroin), approximately 2% of Chicago’s estimated 45,000 IDUs died of OD in this period. Hence, the annual IDU mortality incidence in Chicago was approximately 0.4%. Ninety-five percent of these decedents expired in the city; most of the remaining 5% died in contiguous suburbs. In addition, 185 nonresidents suffered a fatal OD within the city. Most of the nonresidents died in neighborhoods exhibiting high rates of fatal OD among residents. These OD death clusters may reflect the city’s distribution of illicit drug markets.
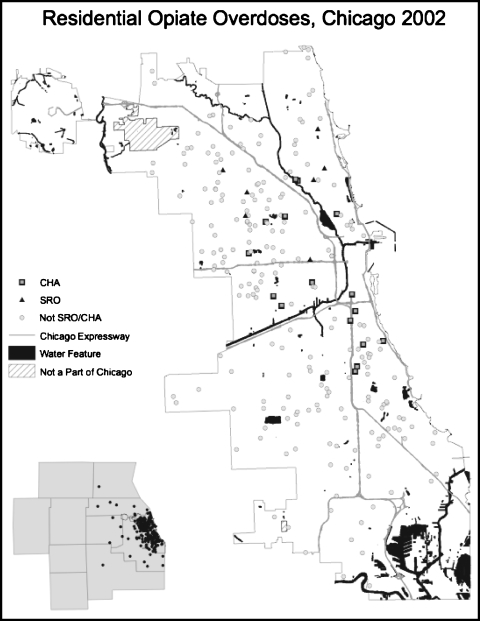
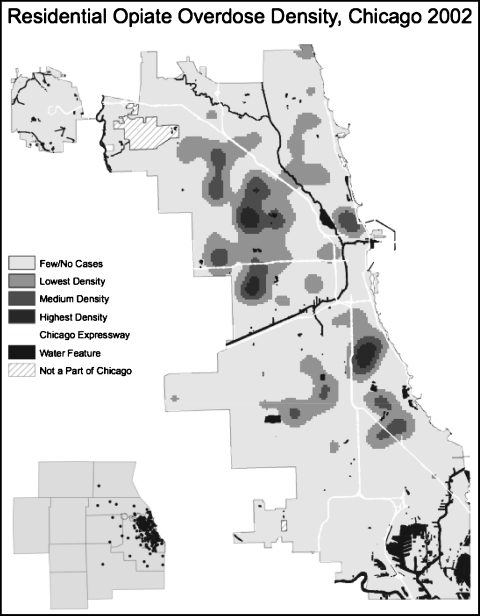
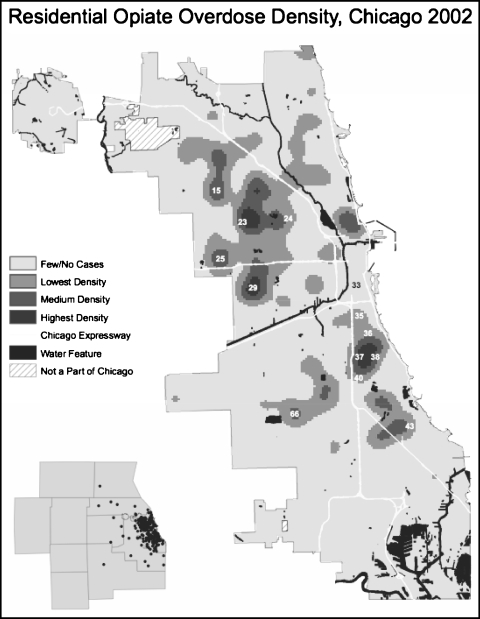
Performing sophisticated cluster analyses lies outside of our current scope. It is worthwhile, however, to characterize the neighborhoods, or “community areas” (CAs),4 as exhibiting the highest densities in 2002, our “benchmark” year. Figures 2 and 3 display the spatial distribution of OD deaths in 2002 by location and density respectively. Figure 4 illustrates opiate OD density by CA. The CA numbers indicate the areas highest in OD fatalities, both in absolute numbers and in deaths per 100,000 population. Although fatal OD risk varies markedly by race/ethnicity, some neighborhoods experience tighter OD death groupings than do others, a pattern that remains relatively constant over time. Unlike previous studies of OD fatality in San Francisco,31 we found that a small proportion of IDU deaths accrued to residents of SROs. Table 2 presents OD fatality by sex and race over the period 1999–2003.
FIGURE 2.
Opiate ODs in Chicago, 2002.
FIGURE 3.
Opiate OD density in Chicago, 2002.
FIGURE 4.
Opiate OD density by CA in Chicago, 2002.
TABLE 2.
Opiate-related OD as a percentage of all accidental deaths in Chicago 1999–2003
| Gender and ethnicity | Opiate-related deaths | All accidental deaths | Percent |
|---|---|---|---|
| Hispanic female | 15 | 84 | 17.9 |
| Hispanic male | 116 | 487 | 23.8 |
| Non-Hispanic black female | 146 | 420 | 34.8 |
| Non-Hispanic black male | 473 | 1,122 | 42.1 |
| Non-Hispanic white female | 45 | 182 | 24.7 |
| Non-Hispanic white male | 261 | 728 | 35.9 |
| Total | 1,056 | 3,056 | 34.9 |
In terms of the absolute number of OD fatalities, the following communities make up the top eight CAs of risk (listed in descending order): 25 (Austin), 29 (North Lawndale), 24 (West Town), 38 (Grand Boulevard), 66 (Chicago Lawn), 23 (Humboldt Park), 43 (South Shore), and 15 (Portage Park). Except for CA 15 (discussed below), these CAs exhibit a poverty rate higher than that of Chicago as a whole (19.6%). In fact, the poverty rates are more than twice that of the city’s rate in CA 38 (46.9%) and CA 29 (45.2%). These communities’ average proportion of nonwhite residents is 76%, nearly twice that of Chicago. The top two ranking CAs (25 and 29) have an average poverty rate of 46%, with an average of 98% nonwhite residents. These demographic trends support—but do not confirm—findings concerning Chicago’s “hypersegregation,” whereby poverty, race, social inequality, and health disparities converge lethally in particular spaces.41
As stated above, CA 15 represents an exception to these trends. In this CA, the poverty rate is 8%, with only 19% of the residents being nonwhite. The absence of additional data prevents us from drawing firm conclusions about this anomalous situation. One hypothesis, however, is that this CA stands close to the drug markets operating in CAs 23 and 24.
Analyzing these clusters in terms of OD fatalities per 100,000 population yields slightly different insights. Using rate calculations, the following communities comprise the highest OD death risk areas (listed in descending order): 33 (Near South Side), 38 (Grand Boulevard), 29 (North Lawndale), 36 (Oakland), 37 (Fuller Park), 40 (Washington Park), and 35 (Douglas).
A few insights emerge straight away. First, these communities’ average poverty rate is 43%, twice that of the city and nearly twice that of the top-ranking communities described above (i.e., CAs ranked in terms of the absolute number of fatal ODs). Also, these communities’ share of nonwhites averages 94%, considerably higher than that of the communities analyzed from an absolute number perspective.
Finally, these CAs historically have hosted the single largest concentration of high-rise public housing in the country. Other researchers have documented the confluence of social problems in these areas.42 One glaring exception to this trend arises with CA 33, whose poverty rate is 32% and whose residents in 2002 were 74% nonwhite. One possible explanation for this aberration is the area’s rapid and widespread gentrification and population displacement, which began in 2000 and accelerated remarkably in 2003. This CA, as with CA 15 in the previous discussion, also may have been experiencing a “spillover” effect because of its proximity to drug markets.
Although fatal OD among youths attracts attention from the mass media, the community, and harm reduction programs, only three fatal ODs occurred among minors in this period. Ninety-nine percent of the decedents were between the ages of 18 and 64, and the median age at death was 39 years. Five percent of the fatal ODs occurred among people aged 55 and over. Ninety-two percent were either found dead at the scene of their OD or had expired by the time they reached a hospital. In other words, nearly every OD decedent expired in the same location where they consumed the culpable substance.
For Chicago adults aged 18–64, accidents are the third leading cause of death. Table 2 displays fatal opiate-related OD as a proportion of all accidental deaths in this age group between 1999 and 2003. In the year 2003, OD accounted for 34% of all accidental deaths in this age group. The impact of opiate OD on accidental death varies by race and gender. Opiate OD clearly exerts a disproportionate impact on accidental deaths among non-Hispanic black males. Non-Hispanic black females and non-Hispanic white males exhibit nearly identical rates of opiate-OD-related deaths in relation to all accidental deaths combined.
African-American men comprise the most populous category of OD death victims, accounting for almost half of OD fatalities (see Table 3). This proportion remains steady throughout the study period, ranging from 47.1% of all deaths in 1999 to 45.4% of deaths in 2003. Among non-Hispanic white males, OD mortality declined by a slightly greater proportion (from 27.5 to 21.5%) over the same period, with a small accompanying increase among Hispanic/Latino males. Virtually the entire recorded mortality decline occurred among males. Expressed in terms of relative risk in the overall Chicago population, non-Hispanic blacks bear the highest risk of fatal OD, with a relative risk of 1.9 to 2.5 compared to the second highest risk group. For each year, the highest risk group had a rate 13–30 times higher than the lowest risk group. Table 4 shows the results of our multivariate models in terms of IRR and associated 95% confidence intervals.
TABLE 3.
Reported Chicago opiate OD deaths 1999–2003
| 1999 | 2000 | 2001 | 2002 | 2003 | Total | |
|---|---|---|---|---|---|---|
| All men | 228 | 252 | 177 | 184 | 158 | 999 |
| African-American men | 130 | 148 | 92 | 99 | 93 | 562 |
| Non-Hispanic white men | 76 | 64 | 58 | 58 | 44 | 300 |
| Hispanic/Latino men | 22 | 40 | 27 | 27 | 19 | 135 |
| Men in other race/ethnic categories | 0 | 0 | 0 | 0 | 2 | 2 |
| All women | 48 | 58 | 44 | 54 | 47 | 251 |
| African-American women | 38 | 46 | 26 | 35 | 32 | 177 |
| Non-Hispanic white women | 10 | 6 | 14 | 14 | 8 | 52 |
| Hispanic/Latino women | 0 | 6 | 4 | 5 | 6 | 21 |
| Women in other race/ethnic categories | 0 | 0 | 0 | 0 | 1 | 1 |
| All cases | 276 | 310 | 221 | 238 | 205 | 1,250 |
TABLE 4.
Random-effects negative binomial model of OD deaths
| All deaths IRR [95% CI] | African-American IRR [95% CI] | Non-Hispanic white IRR [95% CI] | Hispanic/Latino IRR [95% CI] | |
|---|---|---|---|---|
| 1999 | 0.89 [0.76, 1.05] | 0.86 [0.70, 1.06] | 1.24 [0.90, 1.70] | 0.47*** [0.28, 0.79] |
| 2000 | Reference year | Reference year | Reference year | Reference year |
| 2001 | 0.71**** [0.60, 0.84] | 0.60**** [0.48, 0.76] | 1.02 [0.74, 1.42] | 0.66* [0.42, 1.05] |
| 2002 | 0.77*** [0.65, 0.91] | 0.69**** [0.55, 0.86] | 1.04 [0.75, 1.45] | 0.68 [0.42, 1.09] |
| 2003 | 0.65**** [0.54, 0.78] | 0.64**** [0.51, 0.81] | 0.74 [0.52, 1.06] | 0.53** [0.32, 0.88] |
CI = confidence interval
*p < 0.10; **p < 0.05; ***p < 0.01; ****p < 0.001
OD mortality overall and within each population subgroup declined from a peak in 2000 to lower incidence in the year 2003. Non-Hispanic blacks and Hispanics displayed the largest and most statistically significant declines. Striking declines—although below standard significance levels—occurred among non-Hispanic whites between 2002 and 2003 (Table 4).
DISCUSSION
Our findings support the acknowledged link between age and the likelihood of OD death1,12,13,15 in the U.S. and other wealthy societies. Chicago’s mean age of death—39 years—resonates with the findings.55 Researchers must continue to explore the complex pathways linking age and accidental death from opiate OD. Current theory suggests a cumulative physiological effect: The gradual accretion of physical risk factors, including the degradation of the body’s ability to tolerate the drug’s impact due to impaired metabolic function of the liver and other organs, may contribute to OD.34,43 Other physiological mechanisms may include polydrug misuse (e.g., combining opiates with alcohol or benzodiazepines such as Klonopin® or Xanax®).32–34 Combined central nervous system depressants could act synergistically with the cumulative damage mechanism.
Unfortunately, social and behavioral research in this area lags far behind the incidence and prevalence of OD-related mortality. Moving beyond physiological explanations, we emphasize that OD fatality—while a seemingly “natural” adverse event occurring within the human organism—is best understood as a socially and economically shaped phenomenon. Our data suggest a disproportionate impact of OD on non-Hispanic blacks, who experience a much higher mortality rate even while non-Hispanic whites experience a greater number of nonfatal ODs; African-American IDUs OD less frequently than do white IDUs, but African-Americans appear much more likely to die from their ODs than whites.3 Also, males (who make up approximately 75% of the IDU population in the USA) are more likely to die from an accidental OD than are females. This community- and population-level analysis, though, leaves individual behavioral questions underexplored and unanswered.
The risk of lethal OD may be influenced by factors whose effects have been noted but which have garnered less systematic investigation. One important factor is heightened systemic vulnerability following release from detoxification programs and/or incarceration,44–46 a time period in which the “protective factor” of abstinence can become a risk factor for fatal OD.
From a medical perspective, OD mortality is readily preventable even among the most active and high-risk IDUs. As mentioned above, our own study finds that 92% of OD victims were found dead at the scene. Moreover, ODs transpire over a period of up to 3 h and typically occur in the presence of others.18 Yet, a major contributor to fatal OD is the inadequacy of companions’ responses.1 Some studies indicate that most bystanders employ ineffectual means when attempting to counter a peer OD (e.g., physical agitation, cold showering, placement of ice on the genitalia).25
In 2000, Chicago’s largest sterile syringe exchange program—The Chicago Recovery Alliance (CRA)—responded to these “social facts” and mounted an OD-reduction intervention: providing opiate users with “take-home” naloxone,5 an opiate antagonist used by emergency medical personnel to reverse opiate OD, and extensive training on resuscitating an opiate OD victim.47 CRA expects participants to convey this training and a supply of naloxone to the people in whose presence the participants most often inject.
The 5-year period we examine in this article encompasses the CRA’s operation of the take-home naloxone program. To date, CRA staff have prescribed naloxone and provided training to approximately 7,500 clients, and recorded more than 500 unsolicited reports of successful naloxone-facilitated OD reversals. Whether or not active engagement in naloxone-facilitated OD resuscitation can reduce (or has reduced) the city’s OD mortality rate remains to be seen.
The present analysis merely suggests that OD incidence may have peaked and that OD reversal interventions unfolded during a period of OD mortality reduction. However, researchers have yet to convincingly establish the impact of OD preventative interventions in Chicago or other locales where programs have mounted similar efforts.48,49 An evaluation of such programs and their multilevel and multifactorial effects would be an important public health enterprise.
Study Limitations
IDUs comprise a hidden, dynamic population. Observed declines in OD mortality may reflect compositional changes in the underlying population of opiate users, their drug-using activities, their utilization of health services, and/or in the drug market itself.
Confounding trends may include significant heroin shortages with accompanying declines in street heroin purity and in the incidence of OD death. For example, in early 2001 Australia experienced a large, unexpected reduction in heroin availability and an attendant drug purity degradation, two variables that interacted to produce a precipitous decline in OD deaths.40,50 At the same time, a similar pattern materialized in Canada.51
The limitations of our data prevent the scrutiny of these concerns, although data collected and summarized by the Community Epidemiology Working Group suggest that Chicago experienced rather stable underlying patterns of heroin consumption and behavioral risk (i.e., exhibits 2–5) over the study period. Data from the Drug Abuse Warning Network (DAWN) indicate that the rate of heroin-related emergency department mentions per 100,000 population increased from 162 in 1999 to 220 in 2002 (exhibit 2)52 (later DAWN data are not directly comparable to 1995–2002 reported figures52). Another data source—the Arrestee Drug Abuse Monitoring Program—indicates that the proportion of male arrestees in Chicago testing positive for opiates also remained stable over our study period (exhibit 5).52
Chicago heroin price and purity data present interpretive challenges. In the year 2000, the price per milligram, according to the Domestic Monitoring Program, was $0.48, reached a peak of $0.71 in 2001, and then remained below $0.50 in the remaining 2 years. Although no clear price trend emerged, observed street heroin purity peaked in 1997 and gradually declined over the study period, reaching 16.6% in 2003 (exhibit 8).53
Finally, our study is based upon death certificate data and is thus confined to sociodemographic and cause-of-death information. Our future work will explore toxicology data to clarify the role of polysubstance misuse, and primary behavioral data collected from OD survivors and witnesses to fatal OD, and data regarding community-level OD prevention program activities. Combined, these efforts will advance the cause of rational policy-making and program development.
Conclusions
This article establishes a clear pattern critical to public health and drug policy. Opiate OD poses a significant threat to population health. OD accounted for more than one-third of accidental deaths to Chicago residents aged 18–64 during the study period. If counted as a separate category, OD would account for more deaths than diabetes or suicide in this age group.54
OD mortality declined sharply, especially among African-American and Hispanic IDUs. The number of recorded OD deaths declined by more than one-third between the years 2000 and 2003. This decline’s causes remain unknown despite intriguing—although still unexamined—potential explanations such as naloxone distribution through syringe exchange programs.
Footnotes
For estimation purposes an “injection drug user” is defined as anyone who has injected any illicit substance (e.g., heroin, cocaine, crystal methamphetamine) at least once in the past year.
“Opiate-related” means that the postmortem toxicology report indicated illicit opiate poisoning/intoxication as a primary cause of death.
For example, the coding of multiple drug combination does not reveal the specific drugs involved.
The Social Science Research Committee at the University of Chicago established “community areas” in the late 1920s. A CA consists of an aggregation of census tracts with a collectively shared history and sociocultural public sphere. CA boundaries have remained stable over the past 75 years to allow for cross-time comparisons. The United States Census Bureau has officially sanctioned these areas and organizes Chicago’s census data by tract and by CA.
Naloxone is the generic version of Narcan®.
Scott is with the Department of Sociology, Egan Urban Center, DePaul University, Chicago, IL, USA; Thomas is with the Chicago Department of Public Health, Chicago, IL, USA; Pollack is with the School of Social Service Administration, University of Chicago, Chicago, IL, USA. Ray is with the Department of Sociology and Anthropology, North Carolina State University, Raleigh, NC, USA.
Contributor Information
Greg Scott, Phone: +1-773-3254893, Email: gscott@depaul.edu.
Sandra D. Thomas, Phone: +1-312-7479810, Email: Thomas_Sandra@cdph.org
Harold A. Pollack, Phone: +1-773-7024414, Email: haroldp@uchicago.edu
Bradley Ray, Email: bradray@gmail.com.
References
- 1.Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: I. Prevalence and correlates of non-fatal heroin overdose. Addiction. 1996;91(3):405–411. [DOI] [PubMed]
- 2.Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: II. Responses to overdose. Addiction. 1996;91(3):413–417. [DOI] [PubMed]
- 3.Darke S, Zador D. Fatal heroin ‘overdose’: a review. Addiction. 1996;91(12):1765–1772. [DOI] [PubMed]
- 4.Chiasson M, Berenson L, Li W, et al. Declining HIV/AIDS mortality in New York City. J Acquir Immune Defic Syndr. 1999;21(1):59–64. [DOI] [PubMed]
- 5.Des Jarlais D, Diaz T, Perlis T, et al. Variability in the incidence of human immunodeficiency virus, hepatitis B virus, and hepatitis C virus infection among young injecting drug users in New York City. Am J Epidemiol. 2003;157(5):467–471. [DOI] [PubMed]
- 6.Barkan S, Leonetti A, Hopkins S, Duchin J. Substantial decrease in numbers and rates of AIDS deaths over the last decade [letter to the editor]. J Acquir Immune Defic Syndr. 1999;22(3):312–314. [DOI] [PubMed]
- 7.Edlin B. Prevention and treatment of hepatitis C in injection drug users. Hepatology. 2002;36(5 (S1)):S210–219. [DOI] [PMC free article] [PubMed]
- 8.Lorvick J, Kral A, Seal K, Gee L, Edlin B. Prevalence and duration of hepatitis C among injection drug users in San Francisco, CA. Am J Public Health. 2001;91(1):46–47. [DOI] [PMC free article] [PubMed]
- 9.Hagan H, McGough J, Thiede H, Weiss N, Hopkins S, Alexander E. Syringe exchange and risk of infection with hepatitis B and C viruses. Am J Epidemiol. 1999;149(3):203–213. [DOI] [PubMed]
- 10.Thorpe L, Ouellet L, Levy J, Williams I, Monterroso E. Hepatitis C virus infection: prevalence, risk factors, and prevention opportunities among young injection drug users in Chicago, 1997–1999. J Infect Dis. 2000;182(6):1588–1594. [DOI] [PubMed]
- 11.Thomas D, Vlahov D, Solomon L, et al. Correlates of hepatitis C virus infections among injection drug users. Medicine (Baltimore). 1995;74(4):212–220. [DOI] [PubMed]
- 12.Centers for Disease Control and Prevention. Heroin overdose deaths—Multnomah County, Oregon, 1993–1999. MMWR Morb Mortal Wkly Rep. 2000;49(28):633–636. [PubMed]
- 13.Centers for Disease Control and Prevention. Unintentional opiate overdose deaths—King County, Washington, 1990–1999. MMWR Morb Mortal Wkly Rep. 2000;49(28):636–640. [PubMed]
- 14.Strang J, Darke S, Hall W, Farrell M, Ali R. Heroin overdose: the case for take-home naloxone. Br Med J. 1996;312(7044):1435–1436. [DOI] [PMC free article] [PubMed]
- 15.Oppenheimer E, Tobutt C, Taylor C, Andrew T. Death and survival in a cohort of heroin addicts from London clinics: a 22-year follow-up study. Addiction. 1994;89(10):1299–1308. [DOI] [PubMed]
- 16.Barnett P. The cost-effectiveness of methadone maintenance as a health care intervention. Addiction. 1999;94(4):479–488. [DOI] [PubMed]
- 17.Hulse G, English D, Milne E, Holman C. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94(2):221–229. [DOI] [PubMed]
- 18.Sporer K. Strategies for preventing heroin overdose. Br Med J. 2003;326(7386):442–444. [DOI] [PMC free article] [PubMed]
- 19.ACMD. Reducing Drug-related Deaths. London: Advisory Council on the Misuse of Drugs, Stationery Office; 2000.
- 20.Donoghoe M. Opioid Overdose. Trends, Risk Factors and Priorities for Action. Geneva: World Health Organization; 1998.
- 21.Sporer K. Acute heroin overdose. Ann Intern Med. 1999;130(7):584–590. [DOI] [PubMed]
- 22.Garfield J, Drucker E. Fatal overdose trends in major U.S. cities: 1990–1997. Addict Res Theory. 2001;9(5):425–436.
- 23.Holmberg S. The estimated prevalence and incidence of HIV in 96 large U.S. metropolitan areas. Am J Public Health. 1996;86(5):642–654. [DOI] [PMC free article] [PubMed]
- 24.Friedman S, Tempalski B, Cooper H, et al. Estimating numbers of injection drug users in metropolitan areas for structural analysis of community vulnerability and for assessing relative degrees of service provision for injection drug users. J Urban Health. 2004;81(3):377–400. [DOI] [PMC free article] [PubMed]
- 25.Scott G. Estimating Injection Drug User Population Parameters in Chicago: A Review and Synthesis of Secondary Data for the National HIV Behavioral Surveillance Effort; October 2004. Atlanta: Centers for Disease Control and Prevention; 2005.
- 26.Scott G. Ethnographic Assessment of Injection Drug Use in Chicago: A Foundation for Behavioral Surveillance; January 2005. Atlanta: Centers for Disease Control and Prevention; 2005.
- 27.Kane-Willis K, Schmitz-Bechteler S. A Multiple Indicator Analysis of Heroin Use in the Chicago Metropolitan Area: 1995 to 2002. Chicago, IL: Roosevelt University; 2004.
- 28.Steentoft A, Teige B, Holmgren P, et al. Fatal poisonings in young drug addicts in the Nordic countries: a comparison between 1984–1985 and 1991. Forensic Sci Int. 1996;78(1):29–37. [DOI] [PubMed]
- 29.EMCDDA. 2000 Annual Report on the State of the Drugs Problem in the European Union. Madrid: European Monitoring Centre for Drugs and Drug Addiction; 2000.
- 30.NIDA. NIDA Annual Emergency Room Data 1995: Data from the Drug Abuse Warning Network (DAWN). Washington, DC: Department of Health and Human Services; 1995.
- 31.Davidson P, McLean R, Kral A, Gleghorn A, Edlin B, Moss A. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urban Health. 2003;80(2):261–273. [DOI] [PMC free article] [PubMed]
- 32.Goldberger B, Cone E, Grant T, Caplan T, Levine B, Smialek J. Disposition of heroin and its metabolites in heroin related deaths. J Anal Toxicol. 1994;18(1):22–28. [DOI] [PubMed]
- 33.Ruttenberger A, Luke J. Heroin-related deaths: a new epidemiological insights. Science. 1984;226(4670):14–20. [DOI] [PubMed]
- 34.Warner-Smith M, Darke S, Lynskey M, Hall W. Heroin overdose: causes and consequences. Addiction. 2001;96(8):1113–1125. [DOI] [PubMed]
- 35.Heinzmann D, DSadovi C, Maxwell T. Deadly Heroin Mix Tightens Grip on City. Chicago Tribune. June 7, 2006;A:1.
- 36.Cameron A, Trivedi P. Regression Analysis of Count Data. Cambridge, UK: Cambridge University Press; 1998.
- 37.Pollack H, Dombkowski K, Zimmerman J, et al. Emergency department use among Michigan children with special health care needs: an introductory study. Health Serv Res. 2004;39(3):665–692. [DOI] [PMC free article] [PubMed]
- 38.Pollack H, Khoshnood K, Blankenship K, Altice F. The impact of needle exchange-based health services on emergency department use. J Gen Intern Med. 2002;17(5):341–348. [DOI] [PMC free article] [PubMed]
- 39.Louria D, Hensle R, Rose J. The major medical complications of heroine addiction. Ann Intern Med. 1967;67(1):1–22. [DOI] [PubMed]
- 40.Degenhardt L, Day C, Gilmour S, Hall W. The “lessons” of the Australian “heroin shortage”. Subst Abuse Treat Prev Policy. 2006;1:11. [DOI] [PMC free article] [PubMed]
- 41.Massey DS, Denton NA. American Apartheid: Segregation and the Making of the American Underclass. Cambridge, MA: Harvard University Press; 1993.
- 42.Venkatesh SA. American Project: The Rise and Fall of a Modern Ghetto. Cambridge, MA: Harvard University Press; 2000.
- 43.Darke S, Sims J, McDonald S, Wickes W. Cognitive impairment among methadone maintenance patients. Addiction. 2000;95(5):687–695. [DOI] [PubMed]
- 44.Drucker E. Harm reduction: a public health strategy. Curr Issues Public Health. 1995;1:64–70.
- 45.Strang J, Best D, Man L, Noble A, Gossop M. Peer-initiated overdose resuscitation: fellow drug users could be mobilised to implement resuscitation. Int J Drug Policy. 2000;11(6):437–445. [DOI] [PubMed]
- 46.Collins E, Kleber H, Whittington R, Heitler N. Anesthesia-assisted vs buprenorphine- or clonidine-assisted heroin detoxification and naltrexone induction: a randomized trial. J Am Med Assoc. 2005;294(8):903–913. [DOI] [PubMed]
- 47.Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively-injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis. 2006;25(3):89–96. [DOI] [PubMed]
- 48.MacGillis A. City Seeks Expanded Anti-OD Training. Sun. September 27, 2005.
- 49.Bennett G, Higgins D. Accidental overdose among injecting drug users in Dorset, UK. Addiction. 1999;94(8):1179–1190. [DOI] [PubMed]
- 50.Caulkins J, Reuter P. Heroin supply in the long-term and short-term perspectives: comments on Wood et al. 2006. Addiction. 2006;101(5):621–622. [DOI] [PubMed]
- 51.Wood E, Stoltz J, Li K, Montaner J, Kerr T. Changes in Canadian heroin supply coinciding with the Australian heroin shortage. Addiction. 2006;101(5):689–695. [DOI] [PubMed]
- 52.Community Epidemiology Working Group. Proceedings of the Community Epidemiology Work Group, volume II; June 2005. Community Epidemiology Work Group; 2005.
- 53.Community Epidemiology Working Group, Proceedings of the Community Epidemiology Working Group, Volume II, January 2006.
- 54.CDPH. Special Calculation, Chicago OD Mortality. Chicago: Chicago Department of Public Health; 2005.
- 55.Darke S, Hall W, Weatherburn D, Lind B. Fluctuations in heroin purity and the incidence of fatal heroin overdose. Drug Alcohol Depend. 1999;54(2):155–161. [DOI] [PubMed]