Abstract
The New York State Department of Health (NYSDOH) AIDS Institute (AI) began an initiative in 1990 in collaboration with the Office of Alcoholism and Substance Abuse Services (OASAS) to colocate HIV prevention and clinical services at drug treatment clinics. In 1990, the initiative began funding drug treatment programs to provide HIV counseling, testing, and prevention services. HIV primary care was added the following year. Program implementation and development are described. An analysis is included of HIV counseling and testing data for the period 1990–2002 and quality of care data for five standardized quality measures with comparisons to data from other clinical settings. In the first 13 years of the initiative 168,340 HIV-antibody tests were conducted including 52,562 tests of injection drug users (IDUs) identifying 14,612 HIV-infected persons; the seroprevalence was 8.68%. By the end of 2000, the HIV primary care caseload peaked at 3,815 patients. Quality of primary medical care services among participating drug treatment programs has consistently matched or exceeded that provided in more conventional health care settings such as the hospitals and community health centers that were used as a basis for comparison. Colocating HIV primary care within substance use treatment is an effective strategy for providing accessible high-quality HIV prevention and primary care services.
Keywords: Colocated, Drug treatment, Injection drug use, Substance abuse
INTRODUCTION
From 1988 through the decade of the 1990s, injection drug use (IDU) has been the leading route of transmission for new HIV infection in New York State, surpassing transmission among men who have sex with men (MSM).1 In the late 1980s, it was estimated based on seroprevalence studies that as many as 50% of injection drug users in New York were already infected with HIV.2 In addition, sexual risk behaviors associated with crack and cocaine use such as exchanging sex for drugs and money placed noninjecting substance users and their partners at elevated risk for HIV.1
Interventions to provide HIV prevention, counseling, testing, and health care service to IDUs and other substance users were complicated by the difficulty these groups have in accessing regular health care and by the traditional mistrust many substance users felt with conventional health care providers (e.g., complaining of poor treatment and lack of respect). Medical providers also complained of the difficulty in providing medical treatment to substance users. They viewed the population as uncooperative, noncompliant, and belligerent.3 As a result, the health care utilization patterns of substance users were often irregular, with a heavy emphasis on emergency room services.
New York State has the largest drug treatment system in the U.S. According to the federal Substance Abuse and Mental Health Services Administration (SAMHSA), in 2003 there were 306,857 admissions to New York State substance use treatment programs.4 As a basis for comparison, the next largest state program (California) had 192,838 admissions or about a third less than New York. In 2002, New York’s OASAS licensed substance use treatment providers served an average daily census of more than 115,000 clients, with approximately 39% of this census in methadone treatment on any given day.5
To improve HIV prevention and health care services for IDUs and other substance users in the late 1980s, the New York State Department of Health AIDS Institute collaborated with OASAS (previously the Division of Substance Use Services) to develop HIV prevention and health care services colocated within drug treatment programs. This strategy was designed to exploit the unique access these facilities had to large numbers of persons who had used injection drugs and other substances, as well as the expertise of the substance use treatment staff in serving this target population.
Schlenger, Kroutil, and Roland report on a 3-year demonstration project, in which the Health Resources and Services Administration collaborated with the Alcohol, Drug Abuse and Mental Health Administration (later to become the Substance Abuse and Mental Health Services Agency) to fund innovative models for enhancing linkages between primary care and substance abuse treatment. The impetus for the study that began in 1989 was the growing concern about HIV among substance users. There were 21 participating projects from 15 states that used either a “centralized” model that colocated both services or a decentralized model that relied on linkages and case management to connect drug treatment and primary care. Unlike the initiative described in this paper, most of the participating projects were either county health departments, city health departments, or community health centers. Only one drug treatment program participated. The results of this demonstration project supported the centralized model as having “substantial advantages” for clients identified in primary care settings; as twice as many were able to access drug treatment as primary care clients identified in a decentralized setting. The study also found clients in drug treatment had a variety of health care needs and suggested a potential advantage of centralized approaches to the delivery of medical care.6
In a 1993 article that appeared in the AIDS and Public Policy Journal, Yedidia and Hanson reported on the results of a survey of 45 executive directors of drug treatment programs, located in New York State, on integrating HIV and primary care services in their facilities. Survey responses identify inadequate funding and the difference in clinical philosophies between drug treatment and medicine as prime obstacles to integrating HIV and primary care services in drug treatment. Broadening the mission of nonresidential drug treatment to include HIV services is recommended. The authors acknowledge the critical role of drug treatment programs in containment of HIV through prevention and primary care services; calling for drug treatment programs to maximize HIV-related services depending on their modality and location (New York City or upstate). The article cites evidence of on-site testing being more effective than referral to outside agencies and recommends integrating HIV testing as “the essential first element.” The article also recommends integrating primary care as the foundation for expanding HIV services.7
Selwyn, Budner, Wasserman, and Arno report on a 16-month prospective study (11/89–2/91), integrating primary care services in a New York City methadone clinic. Medical care was provided to 212 seropositive and 264 seronegative drug injectors. The authors found that “on-site primary medical care services were readily and frequently used by patients at the methadone program” with 81% of the injectors receiving their care on site. The report suggested that methadone treatment programs might have a “strategically important” role in the delivery of HIV services to IDUs. The authors argue for a comprehensive model integrating primary care, and AIDS prevention and treatment services within substance abuse treatment. It also recommended that on-site medical care include the capacity to treat a range of acute and chronic diseases and medical sequelae associated with drug abuse.8
In a 1996 paper, Selwyn examines the impact of HIV infection on medical services in drug treatment programs. The article suggests that the HIV epidemic forced us to examine long-standing fissures between the medical and addiction treatment communities, and develop a treatment philosophy that incorporates clients’ recovery and medical needs. The virtues of colocated drug treatment and HIV services are discussed, and successful models in San Francisco and the Montefiore Medical Center’s methadone treatment clinics are cited. Selwyn addresses the economic aspects of colocation, asserting that system-wide it reduces costs by reducing emergency room admissions and hospital in-patient stays. The article cites the lack of dedicated resources for primary care as an obstacle and describes how the NYS Medicaid program provided income for Montefiore’s methadone treatment program to support the needed staffing levels. The article also discusses the need for systems to provide ongoing training and support of medical personnel.9
This paper describes the successful development of HIV prevention and primary care programs colocated at substance use treatment programs in New York. It reviews the steps taken to design and implement these innovative programs and discussion of the barriers encountered. Individual client level data and aggregate data submitted to AI by providers participating in the project are discussed and analyzed. The data describe client characteristics, HIV counseling and testing rates, primary care activity, and quality of HIV-related health care performance measures for HIV positive clients in colocated primary care programs.
METHODS
Program Implementation
HIV Prevention
The implementation of the colocated HIV prevention and primary care/substance use treatment initiative (“HIV/Substance Use Treatment Initiative”) began in 1989 with a grant from the Centers for Disease Control and Prevention (CDC) to fund a pilot HIV prevention program at selected drug treatment facilities. The initial program included HIV education, HIV counseling and testing, referrals, and group and individual supportive counseling. In collaboration with OASAS, the AI reviewed applications and selected 12 providers to receive grant funding. Funded sites employed a variety of substance use treatment models including seven methadone programs, one therapeutic community, one community-based outreach program (CBO) serving the clients of several smaller drug treatment programs, one CBO conducting street outreach to female sex workers, one 28-day residential program, and one municipality (the city of Buffalo), which managed several drug-free ambulatory clinics. Providers were selected in part based on the presence of the twin epidemics of HIV and substance use in their communities: nine programs were located in NYC, one in the Mid-Hudson region, and two in Buffalo. Currently, 28 contractors or programs with more than 90 sites provide colocated HIV education and counseling and testing in the initiative.
The HIV prevention service model was designed to be integrated within the drug treatment milieu, to educate clients about HIV and to identify persons with HIV and refer them to care. The service components include risk reduction education for all substance use treatment clients, HIV counseling and testing and partner notification, group and individual supportive counseling and referral and follow-up, and linkage agreements and joint planning with HIV service providers in the community. Whereas most of the providers participating in the initiative targeted substance users in treatment, two providers focused their activities on outreach to substance users not in treatment.
HIV Primary Care
In 1991, the AI and OASAS secured both State and Federal Substance Use and Mental Health Services Agency (SAMHSA) grants to support the implementation of HIV primary care services in substance use treatment settings. Initial funding was directed to 11 drug treatment facilities: eight NYC methadone providers and three NYC drug-free providers offering ambulatory and residential modalities. Six of these providers were previously funded for HIV prevention services and had identified a large number of clients with HIV. The new funding was intended to complete the integration of comprehensive HIV services within the drug treatment clinic. The services offered in this model include: HIV primary medical care; prevention services such as education and training, counseling and testing where it was not otherwise being provided, and medical case management. Adherence counseling was also included in the model with several providers electing to directly observe clients taking at least some doses of their antiretroviral medications. Substance use treatment providers were required to establish linkages with hospitals for subspecialty services, with community-based organizations for social services not available on site, and with local government agencies responsible for administering entitlement programs like Medicaid and welfare programs. When a client receiving HIV primary care graduated or left drug treatment, the provider was responsible for transitioning the client to a hospital outpatient clinic, community health center, or a provider of the client’s choosing to continue their HIV medical care. The outcome of the referral was to be confirmed and documented. Currently, 17 providers with more than 50 sites provide colocated HIV primary care and substance use treatment services in the initiative.
The program model was originally designed to be a discreet limited ambulatory care unit to provide high-quality care in an accepting environment for persons in drug treatment. Acknowledging that this population often had serious life issues in addition to their health, the model incorporated case management and counseling services. Since counseling and case management services are the cornerstone of drug treatment, these positions were often recruited from within the program. Case management services emphasized keeping appointments and accessing specialty care off site.
Recruitment of qualified HIV physicians was critical to the development and success of the colocated initiative. Historically, physicians working in drug treatment programs did not provide primary health care. The HIV epidemic changed the paradigm. The colocated clinic offered an opportunity to work in the forefront of the epidemic. Grant funding, which allowed competitive salaries, and favorable work schedules, (daytime hours Monday through Friday) resulted in participating sites being able to attract a cadre of dedicated physicians.
Technical Assistance and Support for the Substance Use Initiative
The AI has provided technical assistance and support since the inception of the HIV/Substance Use Treatment Initiative. Technical support for the medical providers was the responsibility of the AI’s Office of the Medical Director (OMD). Quarterly meetings of providers were convened to address new developments in the field and to respond to issues that arose. In addition, early in the initiative medical consultants were employed by AI’s OMD that would participate on site visits, reviewing charts and assisting providers on an individual basis. The AI implemented a multifaceted education and training program specifically targeted to providers’ needs. Technical assistance is provided by AI staff through site visits, consultants, provider meetings, conferences, and by subcontracting with regional medical centers. Training has covered a broad array of administrative and programmatic issues including: integration of HIV services within drug treatment, fiscal management, and Management Information Systems development.
At the same time, AI designed and implemented a Clinical Education Initiative (CEI) to support the development of HIV clinical expertise among community-based providers including the substance use treatment programs.10 Under the program, 13 medical centers around the State recognized for their expertise in the care and treatment of HIV provide access to community providers to additional HIV clinical expertise. Education is provided through preceptorships, case conferences, and lectures, often on-site at the clinic.
Barriers
Before 1990, the prevailing philosophy within the drug treatment community in New York was to limit services in substance use treatment settings exclusively to the rehabilitation from substance use and addiction. It was argued that the rehabilitation process was so emotionally demanding that introducing other concerns as stressful as HIV would distract clients from the primary purpose of treatment and undermine recovery. At that time, HIV was seen as a terminal illness with a rapid and irreversible downward course. In addition, medical staff at many substance use treatment programs were not knowledgeable about HIV or prepared to treat persons with HIV.
Consequently, most substance use treatment providers were slow to implement the colocated HIV/Substance Use Treatment Initiative. There was a need to overcome resistance from clinic directors and counseling staff of substance use treatment programs, many of who were themselves in recovery and had been treated in programs that adhered to the single-focus-treatment model. They were uncomfortable with the addition of these new services, and program executives were reluctant to compel staff to cooperate. To overcome these barriers, AI staff worked with executive staff at facilities to broaden the mission of their treatment programs from a single-focus substance use treatment model to that of a public health service provider. This change would have a widespread impact not only on how substance use treatment programs operated but also on how the community viewed them. With the high risk and prevalence of HIV among their clients and staff, agencies would fulfill their drug treatment mission more effectively if they were also able to address their clients’ HIV service needs. In addition, financial incentives including enhanced Medicaid HIV rates motivated some programs to accept the new model.
Evaluation and Data Collection
Demographics and Program Data
At HIV/Substance Use Treatment Initiative sites, client-level demographics, risk behavior, and prior testing history data are recorded for all clients that are pretest-counseled, using standard data collection instruments required by the CDC. Demographic and risk behavior data are recorded for all HIV primary care patients at the time of their initial comprehensive exam. In addition, contracted agencies are required to submit monthly activity reports to the AI containing aggregate data for all HIV prevention, support, and primary care activities.
Quality of Care Initiative
The AI established a HIV quality of care program that focuses on working with providers in a collaborative manner to help improve services and management.11 AI’s OMD developed a Quality of Care Committee consisting of HIV ambulatory care providers that included several physicians from the Substance Abuse Initiative. The Committee developed and promulgated standards of care that were used for development of the key indicators for quality management and review. The Committee then constructed algorithms for all the quality indicators that are described in this section. At each participating site a work plan is developed that details program objectives and activities. Feedback is obtained through data collection and visits to all sites that include both medical record chart reviews and interviews with staff and clients.
The clinical algorithms for HIV quality of care examined in this study are as follows:11
HIV staging: CD4 cell count measured—Percentage of patients diagnosed with HIV who have had their CD4 cell count measured within 6 months of the date of the review.
HIV staging: Viral load level measured—Percentage of patients diagnosed with HIV who have had their viral load level measured within 6 months of the date of the review. (These data are available only since 1997.)
PCP prophylaxis—Percentage of patients diagnosed with AIDS (as defined by CDC) who are receiving PCP prophylaxis at the time of the review.
Tuberculosis (TB) purified protein derivative (PPD) screening—Percentage of patients diagnosed with HIV who were screened for TB with a PPD within 12 months of the date of the review.
Pelvic examination—Percentage of female patients diagnosed with HIV who have had a pelvic exam performed within 12 months of the date of the review.
The AI also contracts with an independent review agency, the Island Peer Review Organization (IPRO), for quality reviews of medical records to assess quality of care. IPRO abstracts data annually from medical records and conducts on-site reviews of the medical charts of all participating providers. Chart selection and sample size is based on each provider’s primary care caseload with an over-sampling of records for females to ensure an adequate sample to assess pelvic examination rates. Bayesian estimation techniques are used to determine sample size based on the probability that a randomly chosen chart documents the quality indicator in question. Finite population corrections are made to develop more precise measurement estimates with narrower confidence intervals.12 Data are presented using Bayesian Estimate methodology to reduce variance with smaller sample sizes.13
RESULTS
HIV Prevention Services
The first component of the HIV/Substance Use Initiative to become fully operational was the HIV prevention services program model, which began in July 1990.
Demographics
The demographics and risk factors for persons testing positive for HIV through the initiative was compared to those testing positive throughout the State for 2002 (Table 1). Overall, persons testing HIV-positive through the initiative were more likely than all persons newly reported in New York with HIV to be Hispanic, less likely to be Black non-Hispanic or White non-Hispanic, and more likely to report having injected drugs. Specifically, 46.7% of persons testing positive in the initiative were Hispanic compared to 24.4% of all newly reported persons with HIV in New York, whereas the pattern was reversed for Black non-Hispanic and White non-Hispanic. A total of 527 of the 946 HIV-positive persons identified in the project were from NYC MMTPs where 49.7% of the clients were Hispanic, 26.3% Black, and 23.4% White. Overall, 47.8% of persons testing HIV-positive through the initiative report having injected drugs, as would be expected in a substance use treatment setting, compared with 11.8% of newly reported HIV cases statewide.
TABLE 1.
Comparison of demographic and risk-factor data for HIV infection for persons receiving HIV counseling and testing at colocated HIV primary care and substance use treatment sites and newly reported HIV cases in New York state, 2002
| On-site HIV C&T | On-site HIV test positive | Newly reported HIV for NYS | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Sex | ||||||
| Male | 6,292 | 63.7 | 347 | 65.6 | 2,483 | 63.3 |
| Female | 3,572 | 36.2 | 182 | 34.4 | 1,442 | 36.7 |
| Unknown | 9 | 0.1 | 0 | 0.0 | 0 | 0.0 |
| Total | 9,873 | 100.0 | 529 | 100.0 | 3,925 | 100.0 |
| Race/Ethnicity | ||||||
| Black, Non Hispanic | 3,263 | 33.0 | 204 | 38.6 | 2,104 | 53.6 |
| Hispanic | 4,072 | 41.2 | 247 | 46.7 | 958 | 24.4 |
| White, Non Hispanic | 1,745 | 17.7 | 58 | 11.0 | 778 | 19.8 |
| Asian Pacific Islander, Native American | 76 | 0.8 | 1 | 0.2 | 66 | 1.7 |
| Other/Unknown | 717 | 7.3 | 19 | 3.6 | 19 | 0.5 |
| Total | 9,873 | 100.0 | 529 | 100.0 | 3,925 | 100.0 |
| Age | ||||||
| <13 | 27 | 0.3 | 0 | 0.0 | 28 | 0.7 |
| 13–19 | 493 | 5.0 | 2 | 0.4 | 104 | 2.6 |
| 20–29 | 1,926 | 19.5 | 38 | 7.2 | 770 | 19.6 |
| 30–49 | 6,006 | 60.8 | 396 | 74.9 | 2,500 | 63.7 |
| 50+ | 1,413 | 14.3 | 90 | 17.0 | 522 | 13.3 |
| Unknown | 8 | 0.1 | 3 | 0.6 | 1 | 0.0 |
| Total | 9,873 | 100.0 | 529 | 100.0 | 3,925 | 100.0 |
| HIV Risk | ||||||
| Injection drug user | 2,271 | 23.0 | 253 | 47.8 | 462 | 11.8 |
| Other HIV risk | 7,602 | 77.0 | 276 | 52.2 | 3,463 | 88.2 |
| Total | 9,873 | 100.0 | 529 | 100.0 | 3,925 | 100.0 |
HIV Counseling and Testing Trends
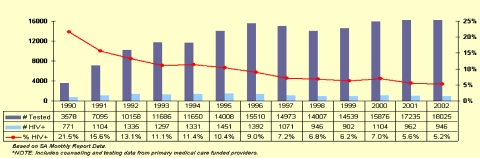
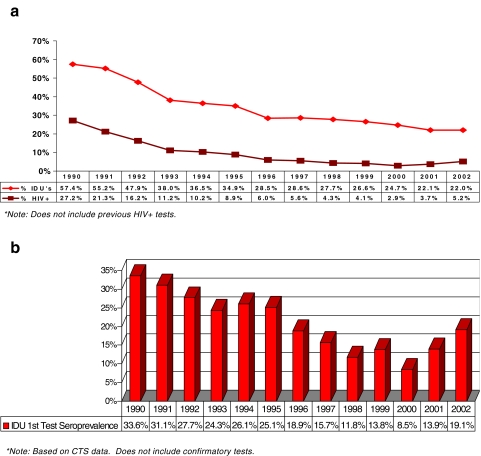
Figure 1 shows the trends in HIV counseling and testing, and the number and percent who were HIV-positive over the first 13 years of the initiative. By the end of 1990, 3,578 persons had been tested for HIV, 771 (21.5%) of whom were infected. Seroprevalence was highest among injection drug users testing for the first time (Figure 2b). Of the 660 in this category, 222 or 33.6% tested positive. The following year the numbers grew significantly as 7,095 persons tested, identifying 1,104 positives (15.6%), including 1,428 IDUs testing for the first time revealing 444 positives (31.1%). By the end of December 2002, the Initiative had conducted 168,340 HIV tests (including 52,562 tests on IDUs) and identified 14,612 infected persons, a seroprevalence rate of 8.68% (cumulative data from Figures 1 and 2a).
FIGURE 1.
HIV counseling and testing 1990–2002 colocated project.
FIGURE 2.
(a) Testing and seroprevalence of injection drug users (IDUs) over time colocated project. (b) Seroprevalence among IDU first-time testers colocated project.
From the beginning of the Initiative, transmission through injection drug use was responsible for the majority of HIV infections among substance users. In 1990, 57.4% of those tested for HIV in drug treatment settings reported having injected drugs; by 2002 that figure had declined to 22% (Figure 2a). In addition, there were substantial declines in seroprevalence among IDUs tested (Figure 2a). This decline occurred even among injection drug users being tested for the first time through 2000 (Figure 2b). However, seroprevalence among IDUs testing for the first time increased in 2001 and again in 2002. Because the overall numbers are small, this increase can be accounted for by two providers that test active IDUs as part of their outreach activities. Together these two providers identified 18 of 32 positives among those IDUs testing for the first time in 2001 and 32 of the 51 positives identified from this group in 2002.
There is extensive data that support this pattern of declining seroprevalence among IDUs. CDC’s National Serosurveillance report for the period 1993–1997 showed declining seroprevalence among IDUs entering drug treatment for the nation as a whole and specifically for the northeast, which included NYC, Boston, and Newark.14 CDC’s 2004 Commentary on Cases of HIV Infection and AIDS in the United States notes that for the period 2001–2004, the estimated number of HIV/AIDS cases and deaths declined among IDUs.15
Contributing to declining seroprevalence among IDUs in New York State is the availability of clean syringes. Under emergency public health regulations promulgated in May 1992, New York State authorized community-based organizations and government entities to operate syringe exchanges. Based on data collected by AI, approximately 3 million syringes are exchanged annually. In addition, effective January 2001, the Expanded Syringe Access Demonstration program legalized the sale or furnishing of up to 10 syringes to persons age 18 or older without a prescription by pharmacists, health care facilities, and health care providers who have registered with the NYSDOH.16
HIV Primary Care Services
Demographics and Trends in Caseload
Table 2 shows the demographics and IDU risk data of persons entering primary care at the colocated drug treatment sites compared with new AIDS cases in New York State for the period 1998–2002. (It should be noted that these two groups are not precisely similar as some of the clients entering the primary care caseload have HIV infection but not AIDS). The comparison for this 5-year time period reveals that the Initiative’s new primary care clients are more likely than newly reported AIDS cases in New York to be female (38.3% versus 33%), Hispanic (41.5% versus 29%), in the 30–49 age group (81.6% versus 70.5%) and an injection drug user (57.8% versus 26.9%). The relatively high percent of Hispanics entering HIV primary care is consistent with the demographics of the drug treatment programs where colocated services are provided. Of the 3,250 clients in HIV primary care at the end of 2002, 2,280 clients or 70.15% are from New York City-based MMTPs where 49.7% of the census is Hispanic.17
TABLE 2.
Comparison of demographic and risk data of persons added to the primary care caseload at colocated HIV primary care and substance use treatment sites with new AIDS cases in New York state for the period 1998–2002
| On site, new primary care caseload | New AIDS cases for NYS | |||
|---|---|---|---|---|
| N | % | N | % | |
| Sex | ||||
| Male | 3,587 | 61.7 | 20,591 | 67.0 |
| Female | 2,225 | 38.3 | 10,119 | 33.0 |
| Total | 5,812 | 100.0 | 30,710 | 100.0 |
| Race/Ethnicity | ||||
| Black, Non-Hispanic | 2,359 | 40.6 | 15,812 | 51.5 |
| Hispanic | 2,413 | 41.5 | 8,919 | 29.0 |
| White, Non-Hispanic | 910 | 15.7 | 5,513 | 18.0 |
| Asian Pacific Islander, Native American | N/A | 0.0 | 309 | 1.0 |
| Other/Unknown | 130 | 2.2 | 157 | 0.5 |
| Total | 5,812 | 100.0 | 30,710 | 100.0 |
| Age | ||||
| 12 and under | N/A | 0.0 | 106 | 0.3 |
| 13–19 | 12 | 0.2 | 323 | 1.1 |
| 20–29 | 417 | 7.2 | 2,814 | 9.2 |
| 30–49 | 4,741 | 81.6 | 21,637 | 70.5 |
| 50 and over | 642 | 11.0 | 5,830 | 19.0 |
| Total | 5,812 | 100.0 | 30,710 | 100.0 |
| HIV risk | ||||
| Injection drug user | 3,361 | 57.8 | 8261 | 26.9 |
| Other HIV risk | 2,451 | 42.2 | 22,449 | 73.1 |
| Total | 5,812 | 100.0 | 30,710 | 100.0 |
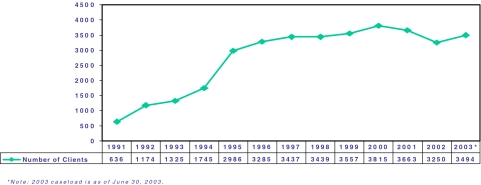
The presence of HIV positive clients identified by the counseling and testing program pushed the development of HIV primary care services at these sites. HIV testing data also supported subsequent applications for funds to expand HIV primary medical care. Because the HIV counseling and testing programs were able to overcome the most serious obstacles to implementing HIV services in drug treatment settings, HIV primary care programs started up more quickly and were able to establish a combined caseload of 636 patients by the end of 1991. Thereafter, the caseload grew rapidly, increasing by 85% to 1,174 the following year (Figure 3). Most of the clients testing positive elected to receive their primary care on site. The initiative has continued to grow by reducing grant funds for existing contracts as third-party Medicaid revenue was generated. The grant savings were used to fund additional drug treatment providers to take part in the initiative.
FIGURE 3.
Primary care caseload colocated.
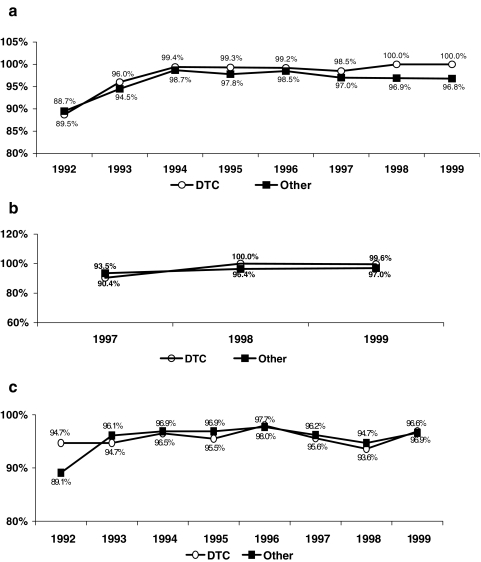
Quality of Primary Care
Quality review results from HIV/Substance Use Initiative sites demonstrate that drug treatment programs are competent providers of HIV prevention and primary care services. Quality evaluation results for every year from 1992 to 1999 reveal colocated drug treatment programs have matched or outperformed other ambulatory care providers, hospitals, and community health centers for adult HIV care on the algorithms previously described (Figure 4a–e). For CD 4 cell count monitoring, drug treatment providers’ performance ranged from 88.7% success in 1992 to 100% in 1998 and 1999 compared to a performance range of 89.5 to 96.8% for all other providers. Viral Load monitoring first became a quality indicator in 1997, and for the period 1997–1999, drug treatment providers’ performance ranged from 90.4% in 1997 to 100% in 1998 and 99.6% in 1999 compared to a performance range of 93.5 to 97% for all other providers. Drug treatment PCP prophylaxis rates for patients diagnosed with AIDS remained consistently above 93% for the period 1992–1999, which was similar to the performance level for all other providers. Drug treatment programs’ performance on PPD screens ranging from 82.6 to 91.1% exceeded the performance for other providers that ranged from 55.1 to 70.1%. Similarly, the 8-year performance range on pelvic exams was 80.4 to 94.3% for drug treatment providers, consistently above performance levels for other providers that ranged from 66.7 to 80.9%.
FIGURE 4.
(a) Quality result: CD4 cell count measured within 6 months of chart review. (b) Quality result: Percentage of patients whose viral load was measured within 6 months of review. (c) Quality result: Percentage of patients diagnosed with AIDS receiving PCP prophylaxis at time of review. (d) Quality result: Percentage of HIV+ patients who had a PPD screen within 12 months of review. (e) Quality result: Percentage of females receiving a pelvic exam within 12 months of chart review.
DISCUSSION
The original purpose of colocating HIV prevention and primary care services was to increase access to HIV testing and care for the highest risk populations who have historically had difficulty accessing health-related services through the conventional provider community. Based on 13 years of utilization data and the results of independent quality reviews, drug treatment programs in New York have demonstrated that they are well situated to and capable of delivering HIV services and health care. Participating drug treatment programs report that their clients readily accept health care services on site at the treatment facilities.
This is different from the experience with trying to provide care in separate settings. For example, in 1997, Guderman et al. found that extensive medical screening at a methadone clinic in Los Angeles was without merit because clients did not follow through with referrals for off-site medical care. It was further found that clients only sought medical care when their conditions had reached a “more advanced state.”18 Another study conducted by Umbricht-Schneiter et al. found that 92% of IDUs will follow through with medical care offered on site at the methadone treatment clinic, whereas only 34% followed through with similar medical services a few blocks away (walking distance).19
Counseling and Testing and Risk Behavior Trends
We found that injection drug use declined as a reported risk factor in participants at initiative sites from 57.4% in 1990 to 22% in 2002. This is consistent with data from other sources. For example, Desjarlais et al. found declining seroprevalance in drug users in general in New York City.2 From 1988 through June of 1998 OASAS reports that the percentage of injectors dropped from 71% to 39% for all admissions to treatment for heroin addiction in New York State.17 Among all race/ethnicity groups in New York, intranasal use has replaced injection as the primary mode of administration among heroin users. Surveys of active users conducted by OASAS’ Field Research Unit reveal that this is attributed to effective prevention messages about HIV, illness, and death due to AIDS among friends and acquaintances and the increased purity of heroin.17 Because addiction is a chronic recurring condition, a large number of active heroin users have at some time been in treatment and, therefore, were probably exposed to intensive risk reduction education, which may or may not have been at drug treatment programs that participated in this initiative. In addition, many clients reported having contact with outreach educators presenting HIV risk reduction information.
Funding Strategies
Adequacy of grant and Medicaid funding has been critical to the development and success of the initiative. Historically, Medicaid provided reimbursement for several types of drug treatment services including; methadone, enhanced chemical dependency outpatient, inpatient detoxification, and 28-day residential (rehab). However, since drug treatment providers had limited responsibilities for health care beyond annual physical exams that were supported through drug treatment funding from OASAS, very few drug treatment providers had grants or were able to access Medicaid reimbursement for medical services.
This initiative incorporates a combination of grant funding and Medicaid reimbursement. Grant funds are used to pay start-up costs, facility renovations, equipment purchases, and to help support expanded staffing structures that include case managers, counselors and nurses. Enhanced Medicaid reimbursement rates for a limited number of HIV-related visits were created for all ambulatory care providers that submitted applications to participate in the Provider Service Agreement for HIV care. Specifically, the enhanced rates covered pre- and posttest counseling, HIV disease monitoring, which in most instances occurred twice a year, and annual HIV comprehensive exams. These enhanced rates proved helpful, especially to encourage HIV counseling and testing, but because on average they only reimbursed for three medical visits a year, it was not sufficient to support ongoing care for their HIV patients. In 1994, in collaboration with NYSDOH, drug treatment providers began applying to become certified as diagnostic and treatment centers, which would allow them to access Medicaid reimbursement for all medical (clinic) visits. The clinic rate was based on the provider’s staffing and costs. Whereas it was not an “enhanced” reimbursement for most drug treatment programs with HIV primary caseloads of 100 patients or more, it produced enough revenue to support expansion and enhancement of HIV medical services.
In summary, grant funding was essential to stimulate interest in establishing HIV services, the enhanced Medicaid rates helped initiate and increase counseling and testing services and to stimulate interest in HIV primary care. However, the general clinic rate for primary care visits is the single most utilized reimbursement category, providing the majority of reimbursement for ongoing HIV health care.
Study Limitations
Adequacy of financial support is a critical element to the success of the initiative and must be considered in assessing the generalizability of this model. As previously noted, provider participation and expansion of the colocation model throughout NYS’ drug treatment community was supported by Medicaid reimbursement through conventional and enhanced reimbursement systems. Grants plus enhanced Medicaid reimbursement for counseling and testing provided the funding needed for prevention services. The addition of Medicaid reimbursement for medical clinic visits was needed to sustain HIV primary care services. Because this Medicaid reimbursement is fee for service, it is important to have sufficient client participation to generate the needed revenue. The providers participating in NYS’ colocation initiative had a census of at least 500 clients receiving drug treatment services. Those that successfully incorporated HIV primary care were able to establish a caseload of at least 100 clients.
The data reflect active client participation in both counseling and testing and primary care services. Counseling and testing was well utilized before implementation of primary care and primary care rapidly developed substantial caseloads consisting of most of the known HIV+ clients attending participating drug treatment programs. Case management services are also widely utilized as every client in primary care also receives a case management needs assessments and has a treatment plan developed. However, the role and success of ancillary services such as education, support groups, crisis intervention, and outreach is less clear. There is not as much data available for these services, and it is not possible to determine the extent to which these services encouraged and supported participation in counseling, testing, and primary care. Feedback from providers indicates that the service culture of the drug treatment provider is critical in how some of these services should be delivered and in part is determined by modality (i.e., methadone, chemical dependency outpatient or residential). Most of the methadone treatment providers were not accustomed to using the group format for addiction or supportive counseling and found the individual counseling model a better fit for their HIV programs. In contrast, participating chemical dependency outpatient and residential treatment providers had both widely utilized group interventions for drug treatment counseling and found groups an effective vehicle for HIV education and support.
Expanding the Model
The success of having substance use treatment programs provide HIV primary medical care has raised the question of whether these providers should expand to provide general health care. Several providers reported that focusing solely on HIV health care was limiting. These providers found that many of their uninfected clients were frustrated at not being able to access care on site. Becoming certified as diagnostic and treatment centers allowed these providers to expand health care to their uninfected clients. By the end of 2002, 10 free-standing drug treatment programs with a combined census of 18,400 clients had become certified. This change enabled the programs to provide and bill Medicaid for non-HIV medical care and qualified them to participate in managed care plans as primary care providers capable of providing general ambulatory care to IDUs and other drug users.
CONCLUSIONS
Through the successful implementation of the “one stop shopping” model for HIV services, the HIV/Substance Use Treatment Initiative was able to bring HIV prevention education, testing and medical care to the venue serving the highest concentration of persons at risk for and infected with HIV due to injection and other drug use. This proved to be an efficient and effective approach to getting persons in substance use treatment tested for HIV and those who are HIV infected into care. The commitment of management and staff at the drug treatment clinics was critical in the implementation and successful promotion of the service protocol. Acceptance of the service model by drug treatment counselors, the staff with the most client contact, was essential for client access.
The service delivery design utilized in the HIV/Substance Use Treatment Initiative was developed specifically to meet the needs of substance users and the facilities that provide drug treatment so that it would be self-sustaining. The high utilization of these services demonstrates the motivation of substance users to care for their health when services are provided in a sensitive and respectful manner.
This model is effective in reaching high-risk individuals who may not otherwise be engaged in continuous medical care. The unique access afforded by this model for hard to reach populations includes substantial fixed costs to support the requisite staffing team required to provide high-quality HIV care. Settings such as alcohol and mental health treatment may consider integrating HIV services in a similar manner if the conditions are favorable. The facility must be able to generate third-party revenue from funding sources such as Medicaid. It is also important that the patient population is large enough to generate sufficient income to support ongoing operations. There is critical information prospective providers need to know about the population they are serving, including type and severity of risk factors and whether they are already receiving continuous health care. In addition, providers must be able to attract qualified and knowledgeable staff sensitive to the needs of the target population.
The effectiveness of New York State’s model of colocating drug abuse treatment with HIV counseling, testing, and primary medical care supports the conclusions and recommendations reached by the research cited in this paper. Based on the capacity of New York State’s substance abuse treatment network, level of need and financial resources available through grant funding and conventional and enhanced Medicaid reimbursement, the colocation model made sense. However, as the research suggests, New York State’s experience is that diverging philosophies of the health care and drug treatment fields and availability of ongoing training for clinicians are challenges that require planning and government leadership. In designing a system that coordinates delivery of drug treatment services with HIV prevention and primary care, states and municipalities need to consider their service provider landscape, availability of resources, and level of need to decide whether colocation is a viable option or one of the other models cited in the research such as enhanced case management and linkages are a better fit.
Acknowledgments
The authors wish to express their gratitude to, Humberto Cruz, Alma Candelas, Daniel O’Connell, Roberta Glaros, Mona Scully, and Megan Tesoriero for their contributions in the creation, development, and implementation of the HIV and drug treatment Colocated Initiative.
Footnotes
Rothman is with the Bureau of HIV Ambulatory Care, AIDS Institute, New York State Department of Health, Albany, New York, USA; Rudnick and Slifer are with the Substance Abuse Unit, AIDS Institute, New York, NY, USA; Agins is with the Office of the Medical Director, AIDS Institute, New York, NY, USA; Heiner is with the Karl Heiner Statistical Consulting, Ltd., Schenectady, New York, USA; Birkhead is with the AIDS Institute, Albany, New York, USA.
References
- 1.AIDS In New York State; 2001–2002. New York State Department of Health. Available at: http://www.nyhealth.gov/diseases/aids/reports/homeaids.htm. Accessed on: September 26, 2006.
- 2.Des Jarlais DC, Perlis T, Friedman SR, et al. Declining seroprevalence in a very large HIV epidemic: injecting drug users in NYC, 1991–1996. Am J Public Health. 1998;88:1801–1806. [DOI] [PMC free article] [PubMed]
- 3.Stone VE, Weissman JS, Cleary PD. Satisfaction with ambulatory care of persons with AIDS: predictions of patient ratings of quality. JGIM. 1995:10;239–245. [DOI] [PubMed]
- 4.Substance Abuse and Mental Health Services Administration (SAMHSA). Available at: http://oas.samhsa.gov/tx.htm, click on “State Data”. Accessed on: September 26, 2006.
- 5.OASAS-Certified Treatment System. Available at: http://www.oasas.state.ny.us. Accessed on: September 26, 2006.
- 6.Schlenger WE, Kroutil LA, Roland EJ. Case management as a mechanism for linking drug abuse treatment and primary care: preliminary evidence from the ADAMHA/HRSA linkage demonstration. NIDA Research Monograph. 1992;(127). [PubMed]
- 7.Yedidia MJ, Hanson KL. Integrating HIV-Related Primary Care and Drug Treatment: Lessons from New York State. APPJ. Fall 2003;7(3).
- 8.Selwyn PA, Budner NS, Wasserman WC, Arno PS. Utilization of On-Site Primary Care Services by HIV-Seropositive and Seronegative Drug Users in a Methadone Maintenance Program. Public Health Rep. July–August 1993;108(4):492–500. [PMC free article] [PubMed]
- 9.Selwyn PA. The impact of HIV infection on medical services in drug abuse treatment programs. JSAT. 1996;13(5):397–410. [DOI] [PubMed]
- 10.AIDS Institute Clinical Education Initiative. Available at: http://www.hivguidelines.org. Accessed on: September 26, 2006.
- 11.HIV Quality of Care Initiative. Available at: http://www.hivguidelines.org. Accessed on: September 26, 2006.
- 12.Heiner KW, Walshaw D. “Inferences on Healthcare Indicators for the Treatment of HIV/AIDS”. Eurostat. 2001;213–222.
- 13.Heiner KW, Laws D, Walshaw D. “Simulation in Models of Health Care Quality”. Computing Science and Statistics. 2000;32.
- 14.Centers for Disease Control and Prevention. HIV Prevalence Trends in Selected Populations in the United States: Results from National Serosurveillance, 1993-1997. Atlanta: Centers for Disease Control and Prevention;2001:1–51. Available at: http://www.cdc.gov/hiv/pubs/hivprevalence/hivprevalence.htm. Accessed on: October 5, 2006.
- 15.Department of Health and Human Services Cases of HIV Infection and AIDS in the United States, 2004. Commentary Section. February 28, 2006.
- 16.Report on Syringe Access in New York State; January 2005. New York State AIDS Advisory Council. Available at: http://www.health.state.ny.us/diseases/aids/workgroups/aac/docs/syringeaccess.pdf Accessed on: October 6, 2006.
- 17.Data reports produced by The New York State Office of Alcoholism and Substance Abuse Services (OASAS) Research Division. June 1, 2006.
- 18.Guderman DM, Carter WC, Charuvastra VC, Ling W. Clinical Utility of Screening Laboratories in the Initiation of Methadone Treatment. 28th Annual Medical Scientific Conference. April, 1997.
- 19.Umbrecht-Schneiter A, Ginn D. Providing medical care to methadone clinic patients: referral va on-site care. Am J Public Health. 1994;84(2):207–210. [DOI] [PMC free article] [PubMed]