Abstract
On August 29, 2005, Hurricane Katrina made landfall resulting in catastrophic damage and flooding to New Orleans, LA, and the Gulf Coast, which may have had significant mental health effects on the population. To determine rates and predictors of symptoms consistent with a diagnosis of posttraumatic stress disorder (PTSD) in New Orleans residents following Hurricane Katrina, we conducted a web-based survey 6 months after Hurricane Katrina made landfall. Participants included 1,542 employees from the largest employer in New Orleans. The prevalence of PTSD symptoms was 19.2%. Predictors of PTSD symptoms in a multivariate-adjusted regression model included female sex, non-black race, knowing someone who died in the storm, not having property insurance, having had a longer evacuation, a much longer work commute compared to before Hurricane Katrina, and currently living in a newly purchased or rented house or in a temporary trailer. Despite universal health coverage and the benefits of an employee assistance program for all employees, only 28.5% of those with PTSD symptoms had talked to a health professional about the events of Hurricane Katrina or issues encountered since the storm. A significant burden of PTSD symptoms was present 6 months following Hurricane Katrina among a large group of adults who had returned to work in New Orleans. Given their key role in the economic redevelopment of the region, there is a tremendous need to identify those in the workforce with symptoms consistent with PTSD and to enhance treatment options. The strong relationship between displacement from ones’ pre-Katrina residence and symptoms of PTSD suggests a need to focus resource utilization and interventions on individuals living in temporary housing.
Keywords: Hurricane Katrina, Natural disaster, Posttraumatic stress disorder, Risk factors.
INTRODUCTION
Hurricane Katrina made landfall just southeast of New Orleans, LA, on August 29, 2005, resulting in one of the worst natural disasters in US history.1, 2 A series of levee breaks in New Orleans associated with the hurricane led to widespread flooding covering 80% of the city, an area of approximately 120 square miles. As a result of the storm, over one million people in the New Orleans metropolitan area were displaced, and all residents of New Orleans proper, an estimated 455,000 people, lived under a mandatory evacuation for 33 days.3
Natural disasters of the magnitude of Hurricane Katrina are known to exert significant mental health effects, with posttraumatic stress disorder (PTSD) being the most studied and reported consequence.4–6 Those able to return and work after the evacuation and long displacement caused by Hurricane Katrina are thought of as having the best resources, both financially and socially. However, ensuring a healthy and productive workforce is an essential component in the economic recovery of the city. Broadly classifying employees who return to work as resilient survivors may result in a missed opportunity to identify and interrupt the mental health sequelae of Hurricane Katrina. To help inform workplace supervisors, policymakers and health professionals, we conducted a cross-sectional survey to determine the prevalence and predictors of symptoms consistent with a diagnosis of PTSD among Hurricane Katrina survivors who have returned to New Orleans and resumed work.
METHODS
Data Collection and Sample
The sampling frame included all faculty, staff, and administrators who were employed at Tulane University during the week of August 23–27, 2005, and remained employed as of February 1, 2006. Tulane University is a private, nonprofit institution of higher education and was the largest employer in the city of New Orleans at the time of the survey. The University maintains several satellite campuses in New Orleans and Covington, LA and Gulfport, MS. At the time of the survey, they also maintained a temporary medical campus in Houston, TX as a result of storm damage to facilities in New Orleans.
Potential participants from all Tulane University offices and campuses received an e-mail from the study investigators requesting their voluntary participation through completion of a web-based questionnaire. This introductory e-mail and three follow-up e-mail messages were sent between February 17 and March 13, 2006, with survey responses accepted on the web site through March 31, 2006. The approximately 200 employees without a University-administered e-mail account were not included in the sample. Overall, 3,553 employees were sent an e-mail invitation to participate. Of the 1,801 potential participants who acknowledged receipt of the e-mail by visiting the study web site, 1,542 completed the study survey for a cooperation rate of 86% and a participation rate among all employees of 43%. Among employees who visited the web site but did not complete the survey, 33 declined participation, 147 visited the web site but did not complete the online consent form, and 79 completed the consent form but did not submit the survey.
Study Instrument
The study instrument was comprised of 50 items assessing several domains, including socioeconomic and demographic characteristics, evacuation and displacement due to Hurricane Katrina, and symptoms consistent with a diagnosis of PTSD in the aftermath of the storm. Information about evacuation and displacement due to Hurricane Katrina was assessed through questions developed specifically for the study. We also determined the type of residence participants inhabited before Hurricane Katrina, whether they had property or renter’s insurance, changes in the duration of their work commute from before to after Hurricane Katrina, and whether they had returned to their pre-Katrina residence or remained displaced.
Symptoms of PTSD were assessed using the validated 17-item PTSD checklist (PCL-17).7–9 This scale allows for the identification of a specific stressor, identified in the current study as “Hurricane Katrina and the aftermath of the storm.” Response options to each item on the PCL-17 are recorded on a five-point Likert scale ranging from 1 (not at all) to 5 (extremely) indicating the degree to which a respondent has been bothered by a particular symptom over the previous month. A symptom was deemed present when a respondent reported an item as being experienced moderately, quite a bit, or extremely (3, 4, or 5, respectively) in the past month.9 In the current study, PTSD was defined using the Diagnostic and Statistical Manual IV criteria.7 To be categorized as having symptoms consistent with a diagnosis of PTSD, a respondent had to report at least one criterion B symptom (reexperiencing), three criterion C symptoms (avoidance/numbing), and two criterion D symptoms (hyperarousal). This definition has demonstrated convergent validity with several other measures.9 In sensitivity analyses, scores were summed with a final range of 17 to 85. In accord with previous studies, a score of 50 or higher was considered consistent with symptoms of PTSD.9
The Institutional Review Board of Tulane University approved all aspects of the study. A web-based informed consent document required participants to select check boxes acknowledging their understanding of the study, voluntary participation, and rights and responsibilities of study participants prior to the initiation of the study questionnaire.
Statistical Analysis
The prevalence of PTSD symptoms was calculated for the overall population and after stratification by sociodemographic and hurricane-related characteristics. Chi-square tests were employed to quantify the significance of differences in the prevalence of PTSD symptoms across these characteristics. We calculated the percentage of participants with PTSD symptoms who had “talked to a health professional about the events of Hurricane Katrina or issues encountered since Hurricane Katrina.” Multivariate-adjusted logistic regression models were used to calculate odds ratios for PTSD symptoms. This model included age, race, sex, and variables that were statistically significant (P < 0.05) in age-, race-, and sex-adjusted logistic regression models (data not shown). All analyses were conducted using Stata 8.2 (Stata, College Station, TX, USA).
RESULTS
Respondent Characteristics
The mean age of respondents was 44 years (range 22–82 years) and the majority were female (64.9%) and non-black (89.9%; Table 1). All respondents had at least a high school diploma and 20.3% had an annual household income <$40,000. A majority of respondents lived with a spouse or partner (65.7%) before Hurricane Katrina made landfall and 80.2% had property insurance (Table 2). Overall, 32.8% of respondents were displaced from their homes for more than 3 months, 43.2% of respondents knew someone who died due to reasons related to Hurricane Katrina, and 18.8% reported a much longer work commute compared to that before Hurricane Katrina. At the time of the survey, 65.9% of respondents had returned to the same dwelling they inhabited before the hurricane, whereas 20.2% were living in a newly purchased or rented residence, 8.2% were living with a friend or relative, and 4.8% were living in a temporary trailer.
TABLE 1.
Prevalence of symptoms consistent with a diagnosis of PTSD 6 months after Hurricane Katrina according to demographic and socioeconomic factors
| Variable | % of the Population | % with PTSD symptoms | P valuea |
|---|---|---|---|
| Age group, years | |||
| 22–34 | 25.6 | 18.3 | 0.934 |
| 35–44 | 25.6 | 19.5 | |
| 45–54 | 27.2 | 19.1 | |
| 55–82 | 21.6 | 20.2 | |
| Sex | |||
| Male | 35.1 | 14.7 | 0.001 |
| Female | 64.9 | 21.9 | |
| Race | |||
| Non-black | 89.9 | 19.3 | 0.858 |
| Black | 10.1 | 18.7 | |
| Education level | |||
| Less than college degree | 15.3 | 28.0 | <0.001 |
| College degree | 19.8 | 22.0 | |
| Graduate work/degree | 64.8 | 16.4 | |
| Annual household income | |||
| <$40,000 | 20.3 | 23.3 | 0.006 |
| $40,000–$79,999 | 38.6 | 21.7 | |
| ≥$80,000 | 41.1 | 15.7 | |
aThe chi-square test was used for comparison; P values are two-tailed
TABLE 2.
Prevalence of symptoms consistent with a diagnosis of PTSD 6 months after Hurricane Katrina according to evacuation, displacement, and relocation characteristics of the study sample
| % of the Population | % with PTSD symptoms | P valuea | |
|---|---|---|---|
| Pre-Katrina cohabitation | |||
| Alone | 20.9 | 22.1 | Ref |
| Spouse/partner | 65.7 | 17.8 | 0.081 |
| Other family (e.g., children/parents) | 27.8 | 18.5 | 0.213 |
| Roommate | 3.1 | 16.7 | 0.390 |
| Had property insurance | |||
| Yes | 80.2 | 17.8 | 0.006 |
| No | 19.8 | 24.8 | |
| Evacuated | |||
| Yes | 90.2 | 19.7 | Ref |
| No | 4.0 | 17.7 | 0.711 |
| Not on Gulf Coast | 5.7 | 14.8 | 0.261 |
| Date of evacuation | |||
| Before or on August 27th | 37.9 | 20.6 | 0.269 |
| August 28th | 51.9 | 18.2 | |
| August 29th or after | 10.2 | 23.5 | |
| Primary residence during evacuation | |||
| Shelter | 0.6 | N/A | N/A |
| Relative’s house | 44.8 | 16.6 | Ref |
| Friend’s house | 17.9 | 24.1 | 0.009 |
| Hotel | 10.7 | 22.7 | 0.075 |
| Other | 26.0 | 20.9 | 0.091 |
| Length of evacuation | |||
| Less than 1 month | 25.1 | 13.8 | 0.004 |
| 1 to <2 months | 25.3 | 20.4 | |
| 2 to <3 months | 16.8 | 25.0 | |
| ≥3 months | 32.8 | 20.9 | |
| Know someone who died | |||
| No | 56.8 | 15.2 | <0.001 |
| Yes | 43.2 | 24.6 | |
| Current work commute, compared to before Hurricane Katrina | |||
| Same | 41.5 | 17.6 | Ref |
| Shorter | 11.7 | 21.4 | 0.250 |
| A little longer | 28.0 | 16.2 | 0.551 |
| Much longer | 18.8 | 26.6 | 0.002 |
| Current dwelling | |||
| Same as before the storm | 65.9 | 16.2 | Ref |
| Newly purchased/rented residence | 20.2 | 24.5 | 0.001 |
| With a friend/relative | 8.2 | 24.0 | 0.030 |
| Temporary trailer | 4.8 | 32.9 | <0.001 |
N/A denotes a sample size too small to permit valid estimation
Ref = reference category
aThe chi-square test was used for all comparisons; P values are two-tailed
Prevalence of PTSD Symptoms
The prevalence of symptoms consistent with a diagnosis of PTSD was 19.2% at the time of the survey. Only 28.5% of those with PTSD symptoms had talked with a health professional about Hurricane Katrina or issues encountered since the storm. Of those without symptoms consistent with a diagnosis of PTSD, 13.4% had talked with a health professional about the hurricane and its aftermath.
Predictors of PTSD Symptoms
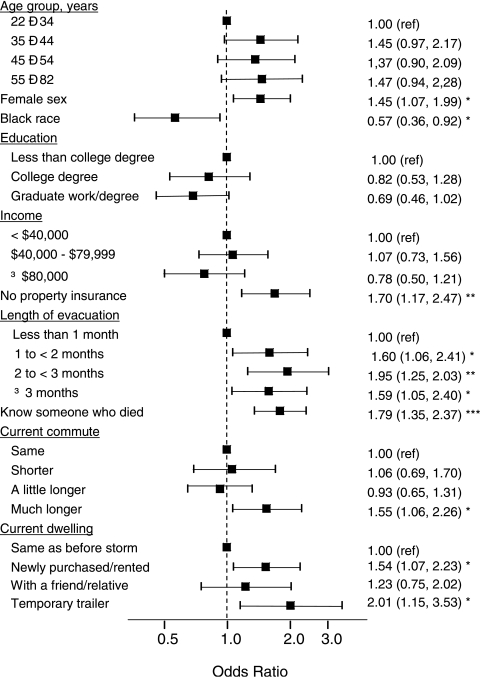
The prevalence of symptoms consistent with a diagnosis of PTSD was higher among females compared to males and at lower levels of education and income (Table 1). Although not statistically significant, non-blacks were more likely to have these symptoms. PTSD symptoms were also more common among respondents who did not have property insurance, were displaced from New Orleans for a longer period of time, knew someone who died due to Hurricane Katrina, had a much longer work commute at the time of the survey compared to before Hurricane Katrina, and were not living in their pre-Katrina residence (Table 2). Most of these associations remained present after multivariate adjustment (Figure 1). Of note, a strong multivariate-adjusted increased risk for symptoms consistent with a diagnosis of PTSD was present for respondents who were female, knew someone who died in the aftermath of Hurricane Katrina, had a much longer work commute compared to before the storm, and those who had not returned to their prestorm residence, especially those currently living in a temporary trailer.
FIGURE 1.
Multivariate adjusted odds ratios and 95% confidence intervals of symptoms consistent with a diagnosis of PTSD associated with demographic, socioeconomic, evacuation, displacement, and relocation characteristics 6 months after Hurricane Katrina.
Sensitivity Analyses
The prevalence of PTSD symptoms, when defined as a score on the PCL-17 score ≥50, was 10.3%. Among participants meeting this alternative definition of PTSD symptoms, 34.2% had talked with a health professional about Hurricane Katrina or issues encountered since the storm. The factors associated with PTSD symptoms were identical, when using a PCL-17 score ≥50, to those identified in the primary analyses (data not shown).
DISCUSSION
We found a significant burden of symptoms consistent with a diagnosis of PTSD in the largest New Orleans workforce 6 months after Hurricane Katrina. Risk factors for PTSD symptoms included female sex, a longer displacement from New Orleans, knowing someone who died due to Hurricane Katrina, and having a much longer work commute compared to that before the storm. Exceptionally high rates of PTSD symptoms were present among respondents who continued to be displaced from their prestorm residence at the time of the survey and were living in temporary trailers. Particularly worrisome was the finding that a majority of those experiencing symptoms consistent with a diagnosis of PTSD had not sought the aid of a health professional.
The current study was based on a population that lived in New Orleans when Hurricane Katrina made landfall and who have returned to work in New Orleans. The choice of study population (i.e., limiting the current study to a returning workforce) deserves special attention. First, it should be recognized that the mental health recovery from Hurricane Katrina is not complete when a person returns to work. Second, workplace supervisors can utilize the results from the current study to understand the burden of PTSD that may be present and plan appropriately for their employees’ mental health needs. If not addressed, PTSD and other mental health problems may reduce productivity and result in a negative workplace environment. With only 28.5% of persons with symptoms consistent with a diagnosis of PTSD talking to a health care professional about Hurricane Katrina and its aftermath, an opportunity to mitigate the mental health effects of the storm is being missed.
The 1-year period prevalence of PTSD in US adults has been reported to be 3.6%.10 In previous studies of natural disaster survivors, the point prevalence of PTSD has been reported to be as low as 5% and as high as 60%.11–13 The prevalence rate of 19.2% for symptoms consistent with a diagnosis of PTSD in the population we studied was slightly lower than the 25% reported 6 months after Hurricane Andrew.6 This is not entirely unexpected given that the current study population may be better off than other post-Katrina New Orleans residents with respect to employment, income, and access to health care. Therefore, our findings may underestimate the prevalence of PTSD symptoms in the general population currently living in New Orleans and the surrounding area.
PTSD can last from several months to years after a natural disaster, during which time persons experience a reduced quality of life and decreased productivity.14, 15 Although symptoms of intrusion and arousal lessened from 6 to 30 months after Hurricane Andrew, the prevalence of PTSD symptoms did not decline.6 Whereas the initial traumatic experience of Hurricane Katrina may be considered a point-source exposure, the difficulties incurred in the aftermath of Hurricane Katrina may be on-going for the residents of the New Orleans metropolitan area and the Mississippi Gulf Coast.16–18 Specifically, even among residents who have been able to return to the area, many roadblocks exist that prevent their ability to return to normal routines. These include waiting for revised Federal Emergency Management Agency’s flood maps that dictate residents’ rights to rebuild their houses, negotiating with insurance companies, the limited availability of public transportation, and the 2006 hurricane season. Throughout New Orleans, buildings that remain boarded up, nonfunctional traffic lights, and dead trees and storm debris are unavoidable, daily reminders of the storm. Whereas PTSD symptoms may resolve themselves in some persons, there is a tremendous need to identify populations prone to poor long-term outcomes subsequent to natural disasters including Hurricane Katrina.
Consistent with previous research, a small percentage of those with PTSD symptoms (28.5%) in the aftermath of Hurricane Katrina had sought care from a health professional.19, 20 The low rate of care-seeking behavior among respondents with symptoms consistent with a diagnosis of PTSD may have resulted from a lack of respondent awareness of stress-related psychopathology and the availability of mental health treatment options, the refusal on the part of respondents to seek care, and the perceived lack of time or low prioritization of mental health care while trying to put their lives back together. Also, the stigma of having a mental health disorder may have been a barrier that prevented respondents from pursuing professional attention.21, 22 Additionally, the health system in the New Orleans metropolitan area sustained substantial losses, with many physicians displaced and/or having relocated due to Hurricane Katrina. In fact, many health facilities remain closed nearly 1 year after Hurricane Katrina. Nonetheless, this finding is especially disconcerting given that all respondents in the current study were employed and had health insurance. Furthermore, all respondents had access to an Employee Assistance Program that was promoted extensively and included counseling sessions at no cost to the employee.
In the current study, one in three respondents was not living in the same dwelling as before the storm. Even after adjustment for several potential confounders, those who had not returned home were more likely to be experiencing PTSD symptoms, regardless of whether they were living in a newly purchased or rented residence, with a friend or relative, or in a temporary trailer. It is worth noting that the risk of symptoms consistent with a diagnosis of PTSD was especially high among respondents living in temporary trailers. Based on government estimates, more than 50,000 residents of the New Orleans metropolitan area and the Mississippi Gulf Coast are currently living in temporary trailers provided by the Federal Emergency Management Agency. It was not feasible to delineate the relative contributions of Hurricane Katrina’s destruction, the subsequent flooding, and living in a temporary trailer to the development of PTSD symptoms in the current study. Nonetheless, the association between living in a trailer and symptoms consistent with a diagnosis of PTSD is striking and warrants further investigation. Living in a 20-by-9-ft temporary trailer is likely to be emotionally difficult and may limit an individual’s ability to recover from the psychological impact of Hurricane Katrina. Although some of these trailers are located in newly created trailer parks, others are placed on the personal property of those whose homes are uninhabitable. These trailers are often located in desolate neighborhoods with limited services. It is also possible that living in a trailer is a proxy for lack of local social support (e.g., no friends or family to stay with in the immediate area), the logistics of securing a trailer (e.g., bureaucratic processes, time to get the trailer, etc.), or the extent of personal property damage.
Our findings need to be interpreted in the context of possible study limitations. The sample is by no means representative of New Orleans as a whole. However, because of the massive displacement of New Orleans residents and the subsequent dispersion of individuals across the USA, a survey of a representative sample of pre-Hurricane Katrina New Orleans residents is difficult at best. This sample was drawn from a single employer in the city of New Orleans. Tulane University was the largest employer in New Orleans at the time of the study and the study participants may reasonably represent a segment of individuals living in the affected area. Because the study population may be better off than other post-Katrina New Orleans residents with respect to employment, income, and access to health care, our findings may underestimate the prevalence of PTSD symptoms in the general population of New Orleans. However, it is important to recognize the high burden of PTSD symptoms among adults who have survived Hurricane Katrina and returned to work in New Orleans. This group may be overlooked and seen as not needing mental health counseling. Data from the current study demonstrates a need for mental health treatment among this group of people. Another possible limitation resulted from the use of a brief survey instrument. This strategic decision was made to limit respondent burden and increase the participation rate. Nonetheless, the use of a brief questionnaire prevented the assessment of additional potential mental health sequelae of Hurricane Katrina, such as depression or substance abuse, and other important covariates (e.g., whether families were able to stay together, extent and cost of property damage, etc.). Finally, although we had a robust response rate of 86% among those who visited the web site, this represents only 43% of Tulane University employees, presenting the possibility of selection bias. However, many employees may not routinely check their e-mail accounts, meaning that this response rate may be a severe underestimate. Additionally, this rate is consistent with prior posttraumatic event survey work.4, 23
Despite these limitations, the current study maintains several strengths. Most importantly, this study provides an estimate of the burden of symptoms consistent with a diagnosis of PTSD in a clearly defined population using a validated tool.8, 9 Furthermore, the large number of respondents permitted the assessment of predictors of these symptoms by important covariates and after multivariate adjustment.
In conclusion, a substantial burden of symptoms consistent with a diagnosis of PTSD was present among respondents in the current study. It is striking that, in this employed cohort, of all of whom had health insurance and access to an Employee Assistance Program, only approximately one-quarter of participants with PTSD symptoms had talked with a health professional about Hurricane Katrina and the storm’s aftermath. These results suggest an unanswered need for mental health care and counseling for the hundreds of thousands of New Orleans and Mississippi Gulf Coast residents affected by Hurricane Katrina. The strong relationship between female sex, knowing someone who died as a result of the storm, and displacement from pre-Katrina residences and living in temporary trailers with symptoms consistent with a diagnosis of PTSD highlights specific groups in need of immediate targeted interventions, counseling, and resource investment.
Acknowledgements
We would like to thank the employees of Tulane University for their time in participating in this study, particularly in the face of their many ongoing challenges. We would also like to acknowledge the assistance of the Disaster Research Education and Mentoring Center (http://www.disasterresearch.org/).
Footnotes
DeSalvo, Tynes, and Muntner are with the Section of General Internal Medicine and Geriatrics, Tulane University School of Medicine, New Orleans, LA, USA; DeSalvo, Hyre, Menke, and Muntner are with the Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA; Ompad is with the Center of Urban Epidemiologic Studies, New York Academy of Medicine, New York, NY, USA; Tynes is with the Department of Psychiatry, Tulane University School of Medicine, New Orleans, LA, USA; Tynes is with the Jefferson Parish Human Services Authority, Metairie, LA, USA.
References
- 1.NOAA National Climatic Data Center. Climate of 2005. Summary of Hurricane Katrina. Available at: http://www.ncdc.noaa.gov/oa/climate/research/2005/katrina.html. Accessed December 5, 2006.
- 2.DeSalvo KB, Muntner P, Fox CE. Community-based health care for “the city that care forgot.” J Urban Health. 2005;82:520–523. [DOI] [PMC free article] [PubMed]
- 3.Census Bureau Quick Facts Page. US Census Bureau. Available at: http://quickfacts.census.gov/qfd/states/22/22071.html. Accessed December 5, 2006.
- 4.Galea S, Ahern J, Resnick H, et al. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 2002;346:982–987. [DOI] [PubMed]
- 5.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. [DOI] [PubMed]
- 6.Norris FH, Perilla J, Riad J. Stability and change in stress, resources, and psychological distress following natural disaster: findings from Hurricane Andrew. Anxiety Stress Coping. 1999;12:363–396. [DOI] [PubMed]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV TR). Washington, DC: American Psychiatric Association Ed; 2000.
- 8.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34:669–673. [DOI] [PubMed]
- 9.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist: reliability, validity, and diagnostic utility. Abstract presented at the Annual Meeting of the International Society for Traumatic Stress Studies. 1993.
- 10.National Institute of Mental Health. “Facts about Post-Traumatic Stress Disorder.” OM-99 4157 (Revised). 2002. Available at: http://www.nimh.nih.gov/publicat/ptsdfacts.cfm. Accessed December 5, 2006.
- 11.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–632. [DOI] [PubMed]
- 12.Canino G, Bravo M, Rubio-Stipec M. The impact of disaster on mental health: prospective and retrospective analyses. Int J Ment Health. 1990;19:51–69.
- 13.Madakasira S, O’Brien KF. Acute posttraumatic stress disorder in victims of a natural disaster. J Nerv Ment Dis. 1987;175:286–290. [DOI] [PubMed]
- 14.Carr VJ, Lewin TJ, Webster RA, Kenardy JA, Hazell PL, Carter GL. Psychosocial sequelae of the 1989 Newcastle earthquake: II. Exposure and morbidity profiles during the first 2 years post-disaster. Psychol Med. 1997;27:167–178. [DOI] [PubMed]
- 15.McFarlane AC. The longitudinal course of posttraumatic morbidity. The range of outcomes and their predictors. J Nerv Ment Dis. 1988;176:30–39. [DOI] [PubMed]
- 16.Burnett K, Ironson G, Benight C, et al. Measurement of perceived disruption during rebuilding following Hurricane Andrew. J Trauma Stress. 1997;10:673–681. [DOI] [PubMed]
- 17.Fukuda S, Morimoto K, Mure K, Maruyama S. Posttraumatic stress and change in lifestyle among the Hanshin-Awaji earthquake victims. Prev Med. 1999;29:147–151. [DOI] [PubMed]
- 18.Koopman C, Classen C, Spiegel D. Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif., firestorm. Am J Psychiatry. 1994;151:888–894. [DOI] [PubMed]
- 19.Carr VJ, Lewin TJ, Carter GL, Webster RA. Patterns of service utilisation following the 1989 Newcastle earthquake: findings from phase 1 of the Quake Impact Study. Aust J Public Health. 1992;16:360–369. [DOI] [PubMed]
- 20.Boscarino JA, Adams RE, Figley CR. Mental health service use 1-year after the World Trade Center disaster: implications for mental health care. Gen Hosp Psychiatry. 2004;26:346–358. [DOI] [PMC free article] [PubMed]
- 21.Mann CE, Himelein MJ. Factors associated with stigmatization of persons with mental illness. Psychiatr Serv. 2004;55:185–187. [DOI] [PubMed]
- 22.Carlos OJ, Njenga FG. Lessons in posttraumatic stress disorder from the past: Venezuela floods and Nairobi bombing. J Clin Psychiatry. 2006;67(Suppl 2):56–63. [PubMed]
- 23.Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to terrorist attacks: findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288:581–588. [DOI] [PubMed]