Abstract
Households and workplaces are the predominant location for exposure to secondhand smoke. The purpose of this study is to examine the association between health status and smoking restrictions at home and work and to compare the relative effect of household and workplace smoking restrictions on health status. This study uses data from a cross sectional representative probability sample of 2,537 Chinese American adults aged 18–74 living in New York City. The analysis was limited to 1,472 respondents who work indoors for wages. Forty-three percent of respondents reported a total smoking ban at home and the workplace, 20% at work only, 22% home only, and 15% reported no smoking restriction at home or work. Smokers who live under a total household smoking ban only or both a total household and total workplace ban were respectively 1.90 and 2.61 times more likely to report better health status compared with those who reported no smoking ban at work or home. Before the NYC Clean Indoor Air Act second-hand smoke (SHS) exposure among this immigrant Chinese population at home and work was high. This study finds that household smoking restrictions are more strongly associated with better health status than workplace smoking restrictions. However, better health status was most strongly associated with both a ban at work and home. Public health efforts should include a focus on promoting total household smoking bans to reduce the well-documented health risks of SHS exposure.
Keywords: Adults, Chinese Americans, Health status, Smoking restrictions, Tobacco.
INTRODUCTION
According to the 2006 Surgeon General Report “Health Consequences of Involuntary Exposure to Tobacco Smoke” there is no safe level of exposure to secondhand smoke (SHS).”1 The report also confirmed that homes and workplaces remain the predominant locations for exposure.1 Driven by scientific evidence of the harmful effects of exposure to SHS, clean indoor air legislation in the U.S. and internationally continues to expand. Surveillance data indicate that protection in the home has followed the trend of increased protection at work.2–4 These trends have been observed across ethnic and racial groups in the U.S.
An analysis of data from the 1991 NHIS reported that current, former, and never smokers exposed to SHS at home or work were more likely to report poorer health status than were people without such exposure.5 In a recent study among nonsmoking hospitality workers, the prevalence of respiratory symptoms was higher among those working in premises where smoking was permitted.6 The March 2006 smoking ban in Scotland was also associated with significant early improvements in respiratory symptoms among nonsmoking bar workers. Asthmatic bar workers also reported improved quality of life.7
Remarkably, the 2006 U.S. Surgeon General report on SHS did not present information with regard to the Asian American Pacific Islander (AAPI) population.1 Yet AAPIs constitute the fastest growing minority group in the U.S., representing 4% of the population at 10.6 million people, with a projected representation of 12% by 2050.8,9 Chinese Americans in particular constitute the largest Asian subgroup (2.43 million people) and, according to the 2000 Census, have grown by almost 50% since 1990.10,11 Moreover, regional surveys conducted in Asian languages indicate that Chinese Americans are at high risk for excess tobacco-related morbidity and mortality with smoking prevalence rates for men ranging from 28 to 36%.12–14 Despite the magnitude of this population growth, there is lack of information on health measures and more specifically the impact of tobacco related policies on health status among Chinese Americans. Furthermore, there are no studies examining the relative effects of household and workplace smoking on health status among the native or foreign-born U.S. population.
With the continued spread of workplace smoking bans the home will increasingly become the most common location for exposure to SHS for adults and children who live with a smoker. The current study is the first to compare the relative effect of workplace and household smoking restriction on health status using data from a large sample of Chinese Americans living in New York City.
METHODS
Data Sources
This study uses baseline data from a representative probability sample of 2,537 Chinese American adults aged 18–74 residing in two communities in New York City. This analysis was limited to 1,472 respondents (1,071 nonsmokers and 401 current smokers) who work indoors in NYC for wages. The survey was conducted from November 2002 to August 2003. These neighborhoods encompass seven zip codes and were chosen based on their high concentration of Chinese Americans.17 From 1990 to 2000, the population of Chinese residents in both communities increased from 47,408 to 108,960.18
Eligible households were obtained from the white pages of these two communities, using a list of 867 unique spellings from 622 native surnames identified in consultation with Chinese linguists. A stratified systematic sampling procedure was applied by zip code to all listed households, resulting in a sample frame of households representative of each Chinese American community. Details of the sampling procedure are provided in a previous study.14 Sample data were weighted to account for unequal probabilities of sample selection and nonresponse. The final individual-level weight used for data analysis was a product of two weight components: a household-level (screener) weight component and a within-household person weight component. The base weights for the screener response rate are the original probabilities of selection. The base weights for the extended interview response rate are the screener-nonresponse-adjusted household weights multiplied by the probability of adult selection within the household.
The survey used for this study was informed by focus groups, and gathered information on health status, chronic conditions, and other health indicators including tobacco use, alcohol consumption, physical activity, height, and weight. Questions were adapted from validated national health survey instruments, translated into Chinese, back-translated, and pilot-tested.19–21 After informed consent, interviews were conducted in English and various Chinese dialects such as Mandarin, Cantonese, and Fukinese. Seventy-seven percent of the surveys were completed as in-person interviews and 23% by telephone. The change in mode from in-person to telephone survey, necessary because of budget constraints, was tested as a fixed effect in the analysis and had an insignificant effect on the statistical models reported in this paper.
Measures
Respondents were identified as smokers if they reported having smoked 100 cigarettes in their lifetime and currently smoke either everyday or some days. Household smoking restrictions were measured with the following question, “Some households have rules about when and where people may smoke. Which statement best describes the rules about smoking inside your home?” Response choices were: Smoking is not allowed anywhere, smoking is allowed in some places or at sometimes, or smoking is allowed everywhere inside the home. Those reporting that smoking was not allowed anywhere were assumed to have a total household smoking ban. Workplace smoking restrictions were measured with the question: “Which best describes the smoking policy at your primary place of work?” Response choices were: Smoking is not allowed anywhere, smoking is allowed in smoke work areas, smoking is allowed everywhere except no smoking areas, and smoking is allowed in all work areas. In the analysis, a total workplace ban was defined as “smoking not allowed anywhere.” Partial smoking ban effects were not analyzed because of consistent reports of the reduced effect of less comprehensive smoking restrictions on exposure to SHS and tobacco use behaviors compared with total bans.14,22,23
Health status was measured using the standardized question “Would you say your health in general is excellent, very good, good, fair, or poor?” Chronic conditions were measured by whether the respondent had ever been told by a physician that they had the following: diabetes, bronchitis, emphysema, asthma, heart disease, high blood pressure, or cancer. Linguistic acculturation was measured by a composite of two categorical variables: speaks English in the home and/or reads English newspapers most or every day. Last, sociodemographic variables such as gender, age, household income, and education were measured and included for analysis.
Analysis
Data were analyzed using the weighted survey procedure in STATA 8.0. Standard descriptive statistics were used to summarize data collected for demographics, smoking-related characteristics, health-related characteristics, and workplace and household smoking policies. The χ2 test for independence was used to examine the relationship between the dependent variable of smoking restrictions (household and workplace) and significant differences by demographics, health status, smoking status, and other variables (Table 1). The χ2 test was also used to examine the relationship between the main dependent variable in this study, health status, and significant differences by smoking restrictions and sociodemographic variables among nonsmokers (Figure 1, Table 2).
TABLE 1.
Smoking restrictions by demographics and tobacco-related variables among nonsmokers and current smokers
| Demographic characteristics | Ban at work and home | Ban at home only | Ban at work only | No ban at work and home |
|---|---|---|---|---|
| n = 638 (43.0%) | n = 276 (21.6%) | n = 311 (20.3%) | n = 247 (15.1%) | |
| Gender** | ||||
| Male | 39.7 | 25.9 | 16.4 | 18.0 |
| Female | 47.6 | 15.8 | 25.5 | 11.1 |
| Age | ||||
| 18–34 | 43.7 | 21.6 | 23.1 | 11.6 |
| 35–44 | 41.6 | 21.0 | 18.3 | 19.1 |
| 45–54 | 40.9 | 22.5 | 21.6 | 15.0 |
| ≥ 55 | 47.7 | 22.9 | 15.3 | 14.1 |
| Education** | ||||
| < 12 | 37.5 | 25.1 | 19.3 | 18.1 |
| HS graduate | 44.9 | 21.4 | 16.4 | 17.3 |
| > 12 | 47.6 | 18.2 | 23.7 | 10.5 |
| Marital Status** | ||||
| Not Married | 44.9 | 11.5 | 30.1 | 13.5 |
| Married | 42.6 | 23.9 | 18.1 | 15.5 |
| Income | ||||
| <$10,000 | 36.6 | 19.0 | 20.6 | 23.7 |
| $10,000–20,000 | 39.8 | 22.3 | 20.2 | 17.8 |
| $21,000–40,000 | 42.1 | 23.5 | 19.3 | 16.1 |
| >$40,000 | 51.3 | 20.2 | 19.4 | 9.0 |
| Insurance** | ||||
| Uninsured | 24.7 | 34.0 | 29.1 | 41.4 |
| Insured | 75.3 | 66.0 | 70.9 | 58.6 |
| Years in US | ||||
| ≤ 5 | 36.9 | 23.2 | 20.5 | 19.4 |
| 6 to 15 | 43.1 | 20.2 | 21.2 | 15.5 |
| ≥ 16 | 44.6 | 24.4 | 18.2 | 12.8 |
| Acculturation** | ||||
| Not acculturated | 40.8 | 22.1 | 19.8 | 17.3 |
| Acculturated | 50.1 | 20.0 | 21.6 | 8.3 |
| Attitude toward smoking in public spaces* | ||||
| Agree | 43.8 | 21.9 | 19.7 | 14.6 |
| Disagree | 30.4 | 8.0 | 32.3 | 29.4 |
| Smoking Status** | ||||
| Current | 19.5 | 19.2 | 28.1 | 33.1 |
| Former | 40.2 | 37.0 | 13.7 | 9.1 |
| Never | 50.3 | 19.5 | 19.2 | 11.0 |
*p < .05
**p < .01
FIGURE 1.
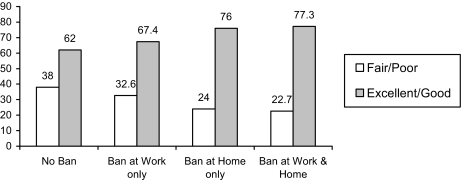
Self-reported health status (%) under home and workplace smoking restrictions for nonsmokers only; χ2 = 23.4, p < .01.
TABLE 2.
Bivariate analysis of demographic variables, smoking restrictions and health status among nonsmokers
| Variables (N = 1071) | Health status | |
|---|---|---|
| Fair/poor | Excellent | |
| Age** | ||
| 18–34 | 17.1 | 33.2 |
| 35–44 | 29.4 | 29.3 |
| 45–54 | 39.7 | 25.7 |
| > = 55 | 13.9 | 11.8 |
| Education | ||
| <HS | 41.1 | 35.2 |
| HS grad | 26.9 | 22.2 |
| >HS | 32.1 | 42.6 |
| Marital status*** | ||
| Not married | 9.6 | 20.6 |
| Married | 90.4 | 79.4 |
| Income** | ||
| < 20,000 | 49.75 | 34.5 |
| 21,000–39,999 | 26.43 | 31.9 |
| ≥40,000 | 23.8 | 33.6 |
| Chronic diseases** | ||
| No | 78.4 | 87.6 |
| Yes | 21.6 | 12.4 |
| Saw a MD in the past 12 months* | ||
| No | 14.1 | 26.0 |
| Yes | 85.9 | 74.0 |
| Acculturated ** | 18.6 | 29.2 |
| Not acculturated | 81.4 | 70.8 |
*p ≤ .05
**p ≤ .01
***p ≤ .001
Logistic regression analyses were used to estimate the association between health status and smoking restrictions at home and work. Analyses were stratified by smoking status. Among current smokers there was no significant association between smoking restrictions and health status; therefore, we present the final regression among nonsmokers (current and former) only. The main independent variables in the model were smoking restrictions at home and/or work. “No smoking restrictions at work and home” was the reference category. Additionally, the model was adjusted for age, gender, marital status, educational attainment, and income. Other independent variables were included if they were significant at p ≤ .05 on bivariate analysis and/or if they have been empirically shown to be associated with health status.24 These included acculturation, whether the participants saw a medical doctor in the past year, and if they had at least one chronic health condition.
A NYC smoking ban, which included bars and restaurants, went into effect March 30, 2003 during data collection. Data collection ended 3 months after the smoking ban. Of the 1,472 subjects included in this analysis, 724 were interviewed in the 3-month period after the policy was implemented. Based on a survey question asking if there was a change in one’s workplace ban policy within the last 12 months, 136 (78 nonsmokers and 58 current smokers) of the 724 reported new workplace smoking restrictions. However, we categorized these 136 respondents as having no workplace ban. This approach was based on an assumption that the health effect of the workplace ban was not measurable in the short time frame after passages of the ban legislation.25,26 To test our assumption, the regression analysis was also conducted with respondents categorized according to their actual response (i.e., reported a workplace ban). The results in the regression analysis remained the same.
RESULTS
Table 1 describes and compares the study population by smoking restriction policy. Categories included: 1) a total ban at work and home, 2) a total ban at work only, 3) a total ban at home only, and 4) no smoking ban. Forty-three percent of respondents reported a total smoking ban at home and the workplace, 20% at work only, 22% home only, and 15% reported no smoking restriction at home or work. Exposure to various smoking restriction policies differed significantly by gender (p < .01). A general pattern of distribution was observed in which men reported greater exposure to a ban at home only and no ban at all, compared to patterns observed among women. Smoking restriction policies also varied by education (p < .01), with a general pattern of lowest educated respondents reporting greatest exposure to both no ban and a total ban at home only. Other significant differences were observed with marital status (p < .01), acculturation (p < .01), smoking status (p < .01), health insurance status (p < .01), and attitude toward smoking in public spaces (p < .01). Those who agreed with the statement that smoking should be restricted in public spaces were more likely to report smoking restrictions at home and in the workplace.
Table 2 describes the relationship between health status and sociodemographics among nonsmokers. Self-reported health status of fair/poor versus excellent varied significantly across sociodemographic characteristics including age group (p < .01), marital status (p < .001), and household income (p < .01). Health status also differed significantly across levels of acculturation (p < .01) and according to whether a respondent had a chronic disease (p < 0.01). Participants with higher levels of acculturation and no reported chronic illness were more likely to report excellent health compared to those with a lower level of acculturation and at least one chronic illness.
Figure 1 illustrates the relationship between health status and ban policy. Self-reported health status differed according to ban policy (χ2 = 23.4, p < .01) with a general trend of improving health with increasing restrictions on smoking.
Table 3 presents logistic regression results among nonsmokers for self-reported health status as the dependent variable. Smoking restrictions were positively associated with better health status. Compared to the reference group of no smoking restrictions, respondents who were exposed to a total smoking ban at home and work were more than two times as likely to report excellent or good health status (OR=2.61, p < .01). In addition, respondents who had a ban at home only were more likely to report excellent/good health status (OR = 1.90, p < .05). In contrast, females (OR = 0.61, p < .05), and those who saw a health professional in the past 12 months (OR = 0.42, p < .001), were significantly more likely to have fair or poor health status.
TABLE 3.
Correlates of health status among nonsmokers (former and never)
| Smoking restrictions and socio-demographic variables | OR (95% CI) |
|---|---|
| Smoking restrictions | |
| No restrictions | 1.0 |
| Restrictions at work only | 1.13 (0.56, 2.3) |
| Restrictions at home only | 1.90 * (0.99, 3.67) |
| Restrictions at both home and work | 2.61 ** (1.22, 4.08) |
| Gender | |
| Male | 1.0 |
| Female | 0.61* (0.47, 1.00) |
| Marriage | |
| Not Married | 1.0 |
| Married | 0.61 (0.31, 1.19) |
| Acculturation | |
| Not Acculturated | 1.0 |
| Acculturated | 1.48 (0.89, 2.45) |
| Saw health Professional in last 12 months | |
| No | 1.0 |
| Yes | 0.42 *** (0.26, 0.68) |
| Chronic Condition | |
| No | 1.0 |
| Yes | 0.64 (0.38, 1.07) |
Odds ratios and 95% confidence intervals based on a multiple logistic regression analysis. (N = 1071)
*p < .05,
**p < .01
***p < .001
aReference—no smoking restrictions at work and home
*Odds ratios adjusted for marital status, education, age, and income
DISCUSSION
This study demonstrates that a large proportion of Chinese immigrants living and working in NYC were not protected from SHS by workplace and home bans before the 2003 NYC Clean Indoor Air Act. Only 43% of study participants reported both a total ban in both the home and workplace. A recent survey of Asian Americans living in the Delaware Valley similarly found high rates of exposure to SHS at home and in the workplace (38 and 40% respectively).27
We also demonstrate a significant positive effect of household smoking bans on health status relative to workplace bans. Household bans alone were a more robust predictor of better self-reported health status than workplace bans alone. When reported together, however, workplace and household bans both contributed to better health status than household bans alone. The reasons for this finding may be explained by the fact that household exposure to cigarettes smoke constitutes a greater percentage of total exposure than workplace exposure.1 Additionally, a U.S. study in Massachusetts found that exposure at home came from a closer source compared with workplace exposure.28
This is the first study to examine the relative effect of household and workplace smoking restrictions on health status. The findings provide evidence for a cumulative benefit to the overall health status of smoking restrictions in both the home and workplace, but in particular the home. Smoking restrictions have a dual goal: to protect the health of nonsmokers and to increase smoking cessation among smokers. Numerous studies have demonstrated that workplace bans are associated with reduced consumption and smoking prevalence.22,23,26,29 Although less studied, there is consistent evidence of a similar association between household bans and higher rates of reduced consumption, cessation attempts, and smoking cessation.4,23,30–32 Moreover, previous analyses suggest that household bans are even more effective than workplace bans in reducing tobacco use.23 This study builds on this literature by highlighting potential health benefits of promoting both workplace legislation and voluntary household smoking restrictions and provides additional rationale for more aggressively promoting voluntary household smoking bans.
In this immigrant population, it is worth noting the relationship between linguistic acculturation and health status. Data from the National Health Interview Survey demonstrate a health advantage among Asian American immigrants compared with U.S.-born. This advantage, referred to as the healthy migrant effect, appears to diminish with increasing length of residence, a measure used as a proxy for acculturation.14,32–34 In contrast, this study finds a positive association between acculturation and health status on bivariate analysis, although not when controlled for other demographic variables. Reports of better health among the acculturated in this study population are in part explained by the fact that more acculturated respondents also had higher education and income levels, factors that are associated with better health status.35,36 Of note, this analysis also demonstrated that acculturated individuals were more likely to be protected from SHS at work and home compared to less acculturated individuals. Similarly, Ma et al37 found that among Asian Americans acculturation, measured as a composite variable including native language used, food preference, and time living in the U.S. was associated with less smoking in the home.
As this and other immigrant populations grow, studies of their health status and the link between acculturation and tobacco-related health outcomes are increasingly important. Research that elucidates relevant social and cultural influences on tobacco use and household smoking restrictions is needed to inform the design of effective interventions to increase adoption of these polices nationally and internationally. Previous studies suggest that educating smokers and nonsmokers about the health dangers of SHS will increase adoption of household smoking restrictions.9,11,21,38 However, we lack data regarding what cultural concepts influence the decision to create smoke-free homes, what type of social marketing messages would resonate with this population, and what barriers may impede adoption of smoking restrictions among immigrant populations. Particular attention must be paid to influencing smokers who are most likely to benefit from these policies but who are less likely to have smoke-free homes and whose families are most at risk. Our data and others’ suggest that among Asian Americans the most at risk are the least acculturated non-English speaking immigrants.27,37 Finally, research is still needed on the full range of health benefits that result from reducing or eliminating exposure to SHS in both the home and workplace.
The findings in this study are subject to several limitations. First, the cross-sectional design is not sufficient to establish whether a causal relation exists between smoking restrictions in the workplace and household, and health status. Moreover, the direction of this relationship cannot be conclusively determined. For example, poor health status may lead to implementing a household ban. Household and workplace bans are associated with reduced consumption among smokers, which may lead to improved self-reported health status among smokers.23,25 A longitudinal follow-up survey of this cohort conducted after the 2003 NYC Clean Indoor Air Act will provide insights into the impact of smoking in public places on household smoking restrictions and health outcomes.
Second, we do not know when the workplace or household bans were implemented relative to the time of the survey. As described in the analysis section, in the case of workplace bans we account for this by assuming that those surveyed after the NYC Clean Indoor Air Act (n = 136) did not have a workplace ban, despite their reports of having experienced a change in workplace policy. A similar adjustment was not possible for household bans. Therefore, our study findings, although consistent with findings in the recent Surgeon Generals report, require confirmation.1 Third, the study is conducted among a specific Asian American subgroup in NYC, therefore we cannot conclude that the associations found between health status and ban policy are generalizable. In terms of exposure to SHS at home and work and prevalence of household smoking bans, however, there is remarkable consistency in reports among Asian Americans, and Chinese Americans specifically, living in different locations across the U.S.2,27,37 Finally, smoking restrictions were established through self reports. However, reports of smoking restrictions correlated with separate measures of SHS exposure at home and work, thus supporting the validity of self reports for key study variables.
CONCLUSION
Involuntary exposure to second-hand smoke remains a serious public health hazard.1 With smoking rates among Chinese American men higher than that of the general U.S. population, workplace and households bans, in particular, have the potential to significantly impact the health of this population. Smoke-free public places appear to facilitate the adoption of smoke-free homes.4 Therefore, as smoke-free air legislation spreads, we can expect a rise in protection from SHS at home. This does not, however, preclude the need to take a proactive approach to increasing adoption of household bans. As the policy environment continues to move toward comprehensive protection at the workplace, the household will increasingly become the main and perhaps the only significant source of exposure among nonsmoking adults as it is among children. We cannot legislate household smoking bans, but governmental agencies can increase their efforts in developing and testing effective interventions to promote household smoking policies. Household smoking restrictions benefit smokers and nonsmokers: they protect the health of both and they encourage smokers to quit.
Acknowledgments
This work was supported by grant R01-CA93788-01 from the State and Community Tobacco Control Interventions Program, Tobacco Control Research Branch, National Cancer Institute, National Institutes of Health.
We are grateful for the contributions of the New York City Department of Health and Mental Hygiene, Asian Americans for Equality, American Cancer Society, and Westat, Inc.
This study was approved by the Hunter College and Columbia University Institutional Review Boards.
Footnotes
Shelley and Hung are with the Department of Sociomedical Sciences, Columbia University Mailman School of Public Health, New York, NY, USA; Yerneni and Fahs are with the Brookdale Center on Aging, Hunter College, City University of New York, New York, NY, USA. Fahs and Das are with the Economics Program Graduate Center, City University of New York, New York, USA.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11524-007-9204-4
References
- 1.U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General-Executive Summary. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2006.
- 2.Gilpin EA, Farkas AJ, Emery SL, Ake CF, Pierce JP. Clean indoor air advances in California, 1990–1999. Am J Public Health. 2002;92:785–791. [DOI] [PMC free article] [PubMed]
- 3.Koh HK, Judge CM, Robbins H, Celebucki CC, Walker DK, Connolly GN. The first decade of the Massachusetts Tobacco Control Program. Public Health Rep. 2005;120(5):482–495. [DOI] [PMC free article] [PubMed]
- 4.Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15 Suppl 3:iii42–iii50 Jun [DOI] [PMC free article] [PubMed]
- 5.Mannino DM, Siegel M, Rose D, Nkuchia J, Etzel R. Environmental tobacco smoke exposure in the home and worksite and health effects in adults: results from the 1991 National Health Interview Survey. Tob Control. 1997;6(4):296–305. [DOI] [PMC free article] [PubMed]
- 6.Dimich-Ward H, Lawson J, Hingston A, Chan-Yeung M. Impact of smoking policy on the respiratory health of food and beverage servers. Scand J Work Environ Health. 2005;31(1):75–81. [DOI] [PubMed]
- 7.Menzies D, Nair A, Williamson PA, et al. Respiratory symptoms, pulmonary function, and markers of inflammation among bar workers before and after a legislative ban on smoking in public places. JAMA. 2006;296:1742–1748. [DOI] [PubMed]
- 8.Schmidley DA. Profile of the foreign-born population in the United States: 2000, Series P23-206. Washington, D.C.: U.S. Census Bureau; 2000.
- 9.Ghosh C. Healthy People 2010 and Asian Americans/Pacific Islanders: defining a baseline of information. Am J Public Health. 2003;93:2093–2098. [DOI] [PMC free article] [PubMed]
- 10.US Bureau of the Census. Profiles of general demographic characteristics 2000: 2000 Census of population and housing. Washington, D.C.: U.S. Department of Commerce; 2001.
- 11.Barnes JS, Bennett CE. The Asian population: 2000. Washington, D.C.: U.S. Department of Commerce; 2002.
- 12.Yu E, Chen E, Kim K, Abdulrahim S. Smoking among Chinese American: behavior, knowledge and beliefs. Am J Public Health. 2002;92(6):1007–1012. [DOI] [PMC free article] [PubMed]
- 13.Ma GX, Shive S, Tan, Y, Toubbeh J. Prevalence and predictors of tobacco use among Asian Americans in the Delaware Valley region. Am J Public Health. 2002;92(6):1013–1020. [DOI] [PMC free article] [PubMed]
- 14.Shelley D, Fahs M, Nguyen N, Yerneni R. Correlates of household smoking restrictions. Nic Tob Res. 2006;8(1):103–112. [DOI] [PMC free article] [PubMed]
- 15.Frisbie WP, Cho Y, Hummer RA. Immigration and health of Asian and Pacific Islander adults in the United States. Am J Epidemiol. 2001;153(4):372–380. [DOI] [PubMed]
- 16.Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Public Health. 2004;25:357–376. [DOI] [PubMed]
- 17.Mosisa AT. The role of foreign-born workers in the U.S. economy: U.S. Department of Labor; 2002.
- 18.Community Studies of New York Inc. US Census by Zip Code and Race. Available at: http://www.infoshare.org. Accessed July 27, 2006.
- 19.Centers for Disease Control and Prevention. Cigarette smoking among adults—United States. Morb Mort Wkly Rep. 1997;48(43):993–996. [PubMed]
- 20.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Available at: http://www.cdc.gov/brfss/. Accessed July 27, 2006.
- 21.National Center for Health Statistics. National Health Interview Survey Data. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed July 27, 2006.
- 22.Farrelly MC, Evans WN, Sfekas ES. The impact of workplace smoking bans: results from a national survey. Tob Control. 1999; 8:272–277. [DOI] [PMC free article] [PubMed]
- 23.Farkas AJ, Gilpin, EA, Distefan JM, Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviors. Tob Control. 1999;8:261–265. [DOI] [PMC free article] [PubMed]
- 24.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national databases. Hum Biol. 2002;74(1):83–109. [DOI] [PubMed]
- 25.Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325(7357):188. [DOI] [PMC free article] [PubMed]
- 26.Bauer JE, Hyland A, Li Q, Steger C, Cummings KM. A longitudinal assessment of the impact of smoke-free worksite policies on tobacco use. Am J Public Health. 2005;95(6):1024–1029. [DOI] [PMC free article] [PubMed]
- 27.Ma GX, Tan Y, Fang CY, Toubbeh JI, Shive S. Knowledge, attitudes and behavior regarding secondhand smoke among Asian Americans. Prev Med. 2005;41:446–453. [DOI] [PubMed]
- 28.Emmons KM, Abrams DB. Exposure to environmental tobacco smoke in naturalistic settings. Am J Public Health. 1992;82(1):24–24. [DOI] [PMC free article] [PubMed]
- 29.Levy DT, Friend KB. The effects of clean indoor air laws: what do we know and what do we need to know? Health Edu Res. 2003:18(5):592–609. [DOI] [PubMed]
- 30.Gilpin EA, White MM, Farkas AA, Pierce JP. Home smoking restrictions: which smokers have them and how they are associated with smoking behavior. Nic Tob Res. 1999;1:153–162. [DOI] [PubMed]
- 31.Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. A prospective study of household smoking bans and subsequent cessation related behavior: the role of stage of change. Tob Control. 2004;13:23–28. [DOI] [PMC free article] [PubMed]
- 32.Norman GJ, Ribisl KM, Howard-Pitney B, Howard KA. Smoking bans in the home and car: Do those who really need them have them? Prev Med. 1999;29(6 Pt 1):581–589. [DOI] [PubMed]
- 33.Dey AN, Lucas JW. Physical and mental health characteristics of U.S.- and foreign-born adults: United States, 1998–2003. Adv Data Vital Health Stat Natl Cent Health Stat. 2006;1(369):1–19. [PubMed]
- 34.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74(1):83–109. [DOI] [PubMed]
- 35.Yu SM, Huang ZJ, Singh GK. Health status and health servicesutilization among US Chinese, Asian Indian, Filipino, and otherAsian/Pacific Islander children. Pediatrics. 2004;113:101–107. [DOI] [PubMed]
- 36.Franks P, Clancy CM, Gold MR, Nutting PA. Health insurance andsubjective health status: data from the 1987 National MedicalExpenditure survey. Am J Pub Health. 1993;83:1295–1299. [DOI] [PMC free article] [PubMed]
- 37.Ma GX, Shive SE, Yin T, Feeley RM. The impact of acculturation on smoking in Asian American homes. Journal of Health Care for the Poor & Underserved. 2004;15:267–280. [DOI] [PubMed]
- 38.Rohrbach LA, Howard-Pitney B, Unger JB, et al. Independent evaluation of the California Tobacco Control Program: relationships between program exposure and outcomes, 1996–1998. Am J Pub Health. 2002;92(6):975–983. [DOI] [PMC free article] [PubMed]
- 39.Gilpin EA, Lee L, Pierce JP. Changes in population attitudes about where smoking should not be allowed: California versus the rest of the USA. Tob Control. 2004;13:38–44. [DOI] [PMC free article] [PubMed]