SYNOPSIS
Objective
This article maps the program requirements of the University of Michigan preventive medicine residency (PMR) to the newly established Centers for Disease Control and Prevention/Council of State and Territorial Epidemiologists Competencies for Applied Epidemiologists in Governmental Public Health Agencies (AECs) to determine the feasibility and utility of using these competencies to assess the training of physician epidemiologists.
Methods
The academic and practicum requirements of the PMR are mapped against the 38 AECs for Tier 2, or mid-level epidemiologists. The process of mapping was done by reviewing academic course syllabi/content and practicum tasks to determine how closely they aligned with the AECs. This process allowed us to identify competencies that are relative training strengths and weaknesses of the residency.
Results
Overall, the current program requirements of the PMR generally satisfy the AECs, although one competency was not met in either the academic or practicum year, and another was only met in a single, required academic course. The areas in which AECs were fulfilled by many activities in the residency were in domain 1 (assessment and analysis) and domain 2 (basic public health sciences). The areas in which competencies were met by few activities were primarily in domain 6 (financial and operational planning and management) and domain 7 (leadership and systems thinking).
Conclusion
We found that the process of mapping an academically rigorous epidemiology training program (the PMR) to the AEC was feasible and useful. It permitted us to identify training strengths and gaps in our program and consider modifications that will strengthen the level of competency of our physician graduates.
The field of epidemiology is an important area of focus in public health and preventive medicine residencies (PMRs). Epidemiology has lagged behind other areas of public health as infrastructure has been enhanced through availability of bioterrorism-related funding. A national survey by the Council of State and Territorial Epidemiologists (CSTE) revealed that 29% of all epidemiologists, including physician epidemiologists, in the nation's public health system have had no academic training in epidemiology.1,2 The survey also revealed that there are only one-quarter as many physician epidemiologists as the perceived need, and the number of these individuals working in public health has actually decreased over the last 10 years. Yet, epidemiologists are considered central to our nation's capacity to detect, respond to, and control bioterrorism-related events, other catastrophic health events, and epidemics of acute and chronic diseases.
A medical residency in general preventive medicine/public health is offered at 40 institutions across the U.S.3 These two-year residencies differ fundamentally from clinical residencies in that they include an academic year of coursework leading to award of a Master of Public Health (MPH) degree, followed by a practicum year spent working in the field—typically focusing on public health practice and clinical preventive medicine. PMRs require a minimum of one clinical year of residency training for eligibility, although it is not uncommon for admitted residents to have completed more clinical training or be board certified in a clinical specialty. Graduates of accredited PMRs are eligible to sit for the American Board of Preventive Medicine (ABPM) examination.
The American College of Preventive Medicine (ACPM) estimates that 10,500 preventive medicine physicians are needed nationwide, while currently there are only 7,518 living diplomates who are board certified in preventive medicine.4 In October 2006, 109 physicians took the ABPM exam; 75% passed and are now board certified.5 Lack of a stable funding stream to support PMR programs has resulted in a decrease in the number of residents trained in preventive medicine at a time when the preventive medicine pipeline should be expanding, rather than contracting.4
The University of Michigan School of Public Health (UMSPH) PMR has a special interest in training public health physicians who will remain in the state's public health system. In Michigan, ACPM estimates that eight preventive medicine physicians are needed in the Michigan Department of Community Health, while only three are currently employed there.4 This shortage is typical throughout Michigan, as less than one-quarter of the current medical directors serving in local health departments have graduate training in epidemiology or are board certified in general preventive medicine.6 To help fill this gap, the UMSPH PMR program has focused on physician training and education in general epidemiology.
The residency in general preventive medicine and public health at UMSPH was originally established in 1969. A main focus of the residency is general epidemiology; this program received full accreditation from the Accreditation Council of Graduate Medical Education in 2004. Residents are required to complete a 42-credit program over one year, resulting in award of an MPH in general epidemiology. The academic year meets all curricular requirements of the UMSPH and the Department of Epidemiology and is highly prescribed with residents limited to selecting no more than four hours of elective credit. The academic year is followed by a 12-month practicum year comprising four, three-month rotations at a variety of established field sites within and outside of Michigan. The residency has a 100% completion rate and 80% of graduates have passed the board certification exam in general preventive medicine and public health.
The UMSPH PMR is a well-established, accredited applied epidemiology training program. This article maps the program requirements to the newly established Centers for Disease Control and Prevention (CDC)/CSTE Competencies for Applied Epidemiologists in Governmental Public Health Agencies (AECs)7 to determine the feasibility and utility of using these competencies to assess our training for these physician epidemiologists.
METHODS
As an outgrowth of its epidemiology workforce initiative, CSTE worked with the CDC Office of Workforce and Career Development to convene an expert panel comprising local, state, and federal health representatives, schools of public health, and private-sector professionals to develop the AECs.7 The intent of the AECs was to define the skills a competent epidemiologist working in public health practice would need to possess to effectively carry out their job duties. The eight skill domains utilized in the Core Competencies for Public Health Professionals, developed by the Council on Linkages Between Academia and Public Health Practice (COL),8 were used as a starting point by the panel in developing the AECs.
The panel identified four different levels of practicing epidemiologists, whose desired competencies were felt to differ in significant ways, and developed four corresponding tiers of AECs: basic or entry-level (Tier 1), mid-level (Tier 2), senior-level supervisor or manager (Tier 3a), and senior-level scientist (Tier 3b) competencies. Eight skill domains cut across these tiers:
Assessment and analysis
Basic public health sciences
Communication
Community dimensions of practice
Cultural competency
Financial and operational planning and management
Leadership and systems thinking
Policy development
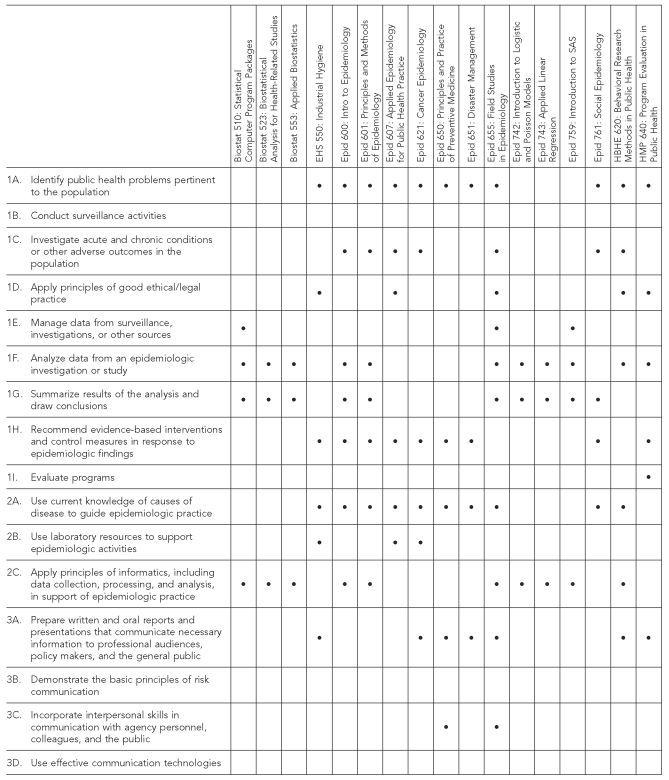
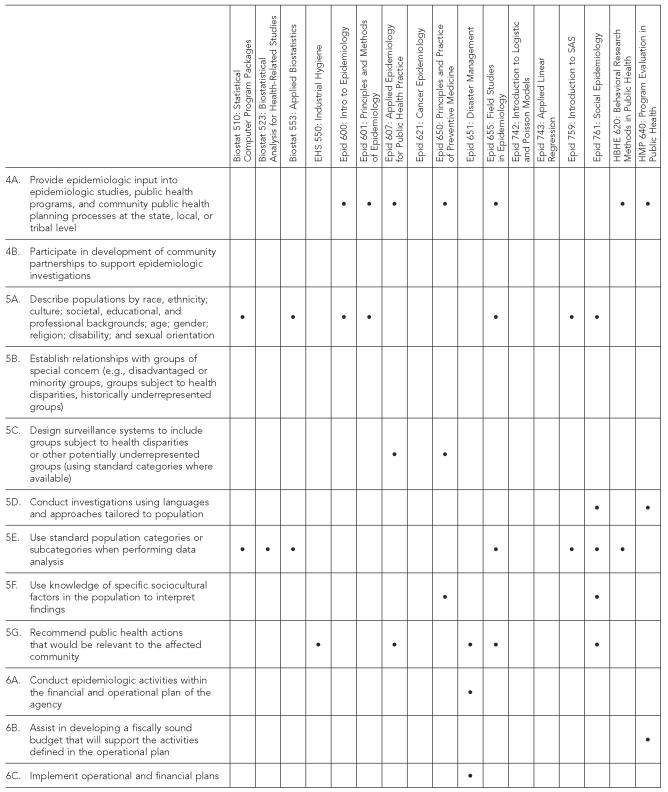
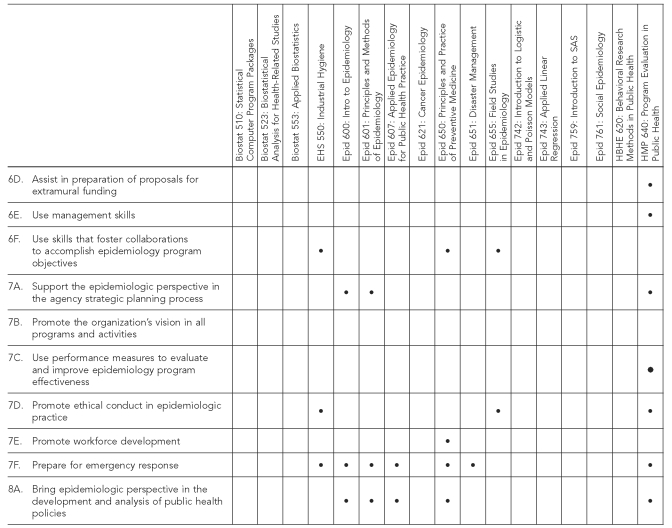
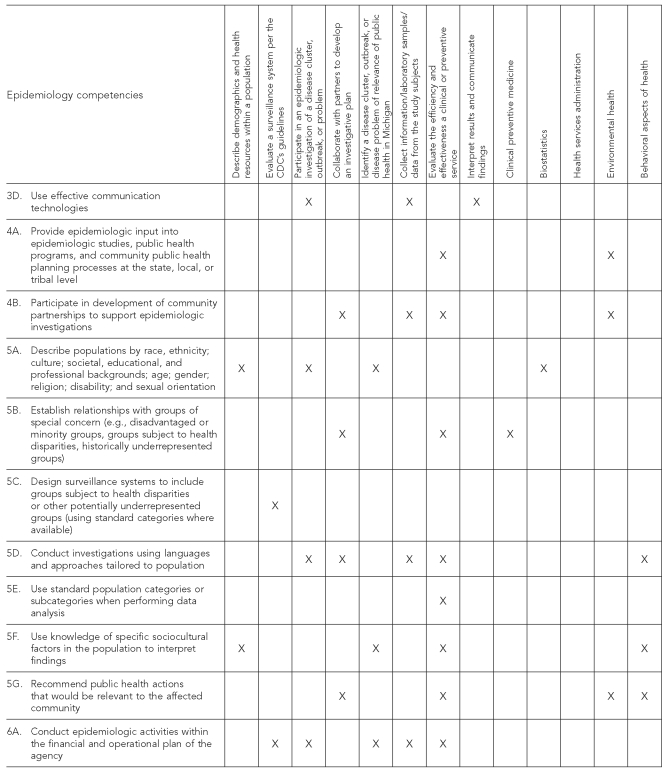
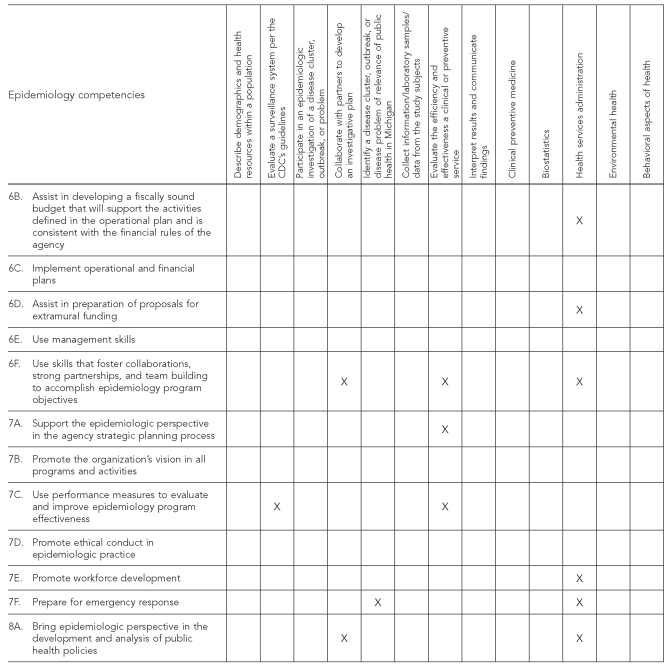
Additionally, 38 competencies, as shown in Figures 1 and 2 and the Table, and multiple subcompetencies further describe the components of the skill domains.
Figure 1.
Preventive medicine residency courses mapped to AECs
AECs = Competencies for Applied Epidemiologists in Governmental Public Health Agencies
Figure 2.
Preventive medicine residency tasks mapped to AECs
AECs = Competencies for Applied Epidemiologists in Governmental Public Health Agencies
CDC = Centers for Disease Control and Prevention
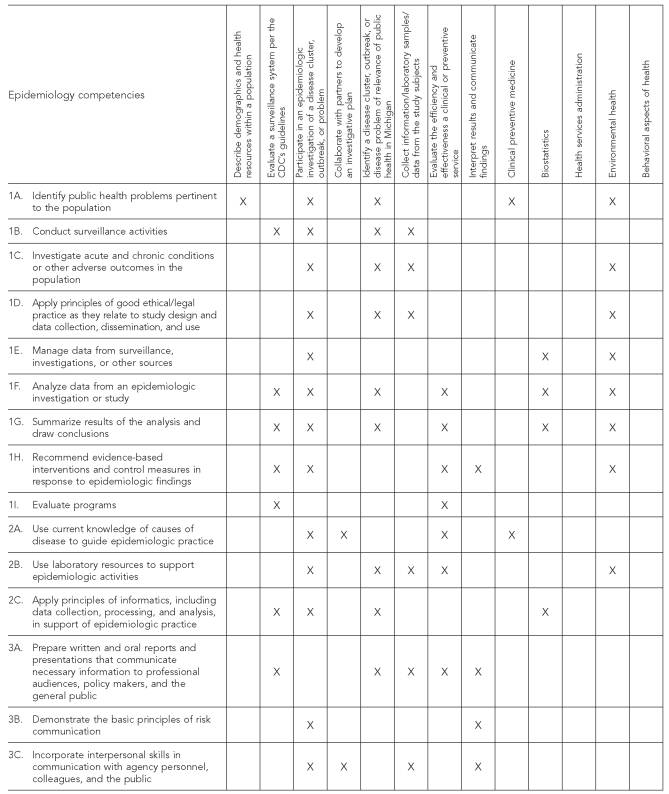
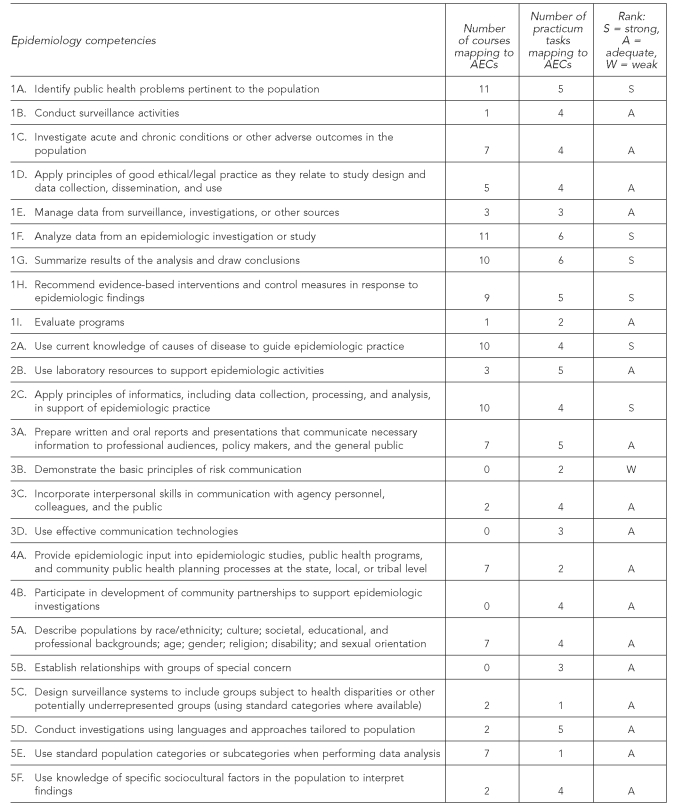
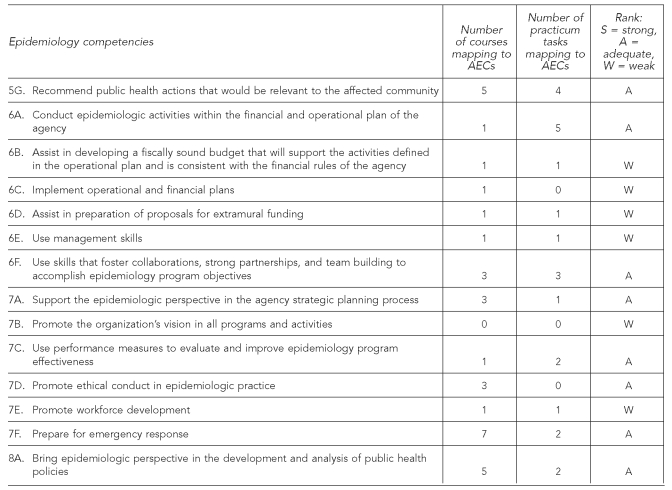
Table.
Summary of competency mapping results
AECs = Competencies for Applied Epidemiologists in Governmental Public Health Agencies
We employed established mapping techniques9 to compare the academic and field requirements of this program to the AECs10 for a Tier 2, or mid-level epidemiologist. This permitted us to assess how well a fully accredited PMR program focusing on epidemiology training meets this comprehensive set of applied competencies, and to ascertain whether it is useful to qualitatively measure PMR training against competencies other than those put forth by the Accreditation Council for Graduate Medical Education (ACGME). We selected Tier 2 because we viewed the competency tiers as having a progressive linear development, expecting epidemiologists to move from Tier 1 (entry level) to Tier 2 (mid-level) and then to Tier 3 (senior manager [3a] or senior scientist [3b]). While most graduates of the PMR program are likely to work in Tier 3 positions, we determined that Tier 2 competency was a minimum level of achievement for graduation from the program.
The academic coursework consists of 42 semester credit hours and identifies 17 classes in which residents enroll, comprising 10 courses in the department of epidemiology, three courses in the department of biostatistics, one in the department of health behavior/health education, and one in the department of health management and policy. This recommended PMR curriculum was used to map the coursework to the AECs.
The practicum year consists of 26 tasks conducted at four rotation sites that were developed based on the ACGME competencies.11 The practicum tasks are inherently more variable than the academic coursework because not every resident completes all tasks at all practicum sites, and tasks tend to vary by the residents' interests and the availability of projects at the host site. However, each resident is required to complete a set of tasks that were developed to specifically provide an experiential complement to the academic coursework and to meet ACGME-specified competencies. The tasks were grouped based on similarity of activities and categorized into the six ACGME content areas of epidemiology, clinical preventive medicine, biostatistics, health services administration, environmental health, and behavioral aspects of health. Tasks directly related to epidemiology were condensed and mapped individually, while tasks related to other categories were mapped in aggregate.
The process of mapping was done by reviewing academic course syllabi and content, as well as practicum tasks to determine how closely aligned they were with the AECs. A group of three individuals—two department of epidemiology faculty and one staff member, all with extensive experience in public health training and education and all associated with PMR—individually mapped the AECs to the academic course learning objectives and practicum tasks. We then compared the results and more fully discussed any competencies that did not have consensus results. In those few cases, a mapping decision was reached based on the majority opinion. This process allowed us to clearly identify competencies that are well-developed in program graduates vs. those that are not.
RESULTS
We examined the 17 courses and 13 task categories that comprise the two-year PMR in epidemiology at UMSPH and mapped them to the 38 CDC/CSTE AECs version 1 (Figures 1 and 2) for Tier 2 epidemiologists.7 These maps illustrate how closely an existing applied epidemiology training program prepares epidemiologists to function as competent Tier 2 epidemiologists. Additionally, these tables include the skill domain and competency letter within that domain. For example, the first competency in skill domain 1 (Assessment and Analysis) states “Identify public health problems pertinent to the population.” This competency is notated as competency 1A and is used to simplify the reporting of the results detailed next.
Through the mapping process, we found that the number of learning opportunities that addressed each competency varied significantly (Figures 1 and 2 the Table). Competencies that mapped to the largest number of learning opportunities differed based on whether the learning activity was coursework or a practicum task. Through coursework, five of the competencies were addressed by at least one of the 17 courses. These included competencies 1A, 1F, 1G, 2A, and 2C. The competencies that mapped to at least five of their 13 practicum task categories included three of the same competencies (1A, 1F, and 1G) and five additional competencies (1H, 2B, 3A, 5D, and 6A).
By contrast, several competencies were determined to not be the focus of coursework, with zero or one course contributing to their overall competency in each area. These include competencies 1B, 1I, 3B, 3D, 4B, 5B, 6A, 6B, 6C, 6D, 6E, 7B, 7C, and 7E. Additionally, several competencies through the practicum year had only zero or one of their 13 task categories contributing to the overall competency. These included competencies 5C, 5E, 6B, 6C, 6D, 6E, 7A, 7B, 7D, and 7E.
To make the results more meaningful, we examined the combined learning experience of coursework and practicum. Each AEC was assigned a qualitative rank of “strong,” “adequate,” or “weak” based on the total number of residency courses and practicum tasks that mapped to it (Table 3). Competencies that only mapped to any combination of 0–2 courses and/or practicum tasks were assigned a weak ranking based on the relative infrequency of exposure to that competency in the residency. Competencies that mapped to any combination of 14 or more courses and/or practicum tasks were classified as strong based on the residents' repeated experience with those competencies in the classroom and in the field. All other competencies were considered adequate.
Of the 38 competencies, 66% (25) were classified as adequate based on the number of activities that contributed to the competency or the significance of that activity. Six competencies (16%) were classified as strong (1A, 1F, 1G, 1H, 2A, and 2C) and seven competencies were classified as weak (3B, 6B, 6C, 6D, 6E, 7B, and 7E) based on the combined contributions of courses and task categories to each competency. The strong competencies focused on data use and application, while the weak competencies clustered around financial and management skills, risk communication, grant writing, agency vision, and workforce development.
DISCUSSION
The UM PMR was specifically intended to train physicians in public health with a strong focus on general epidemiology. The program has been designed to accomplish this through provision of rigorous academic coursework leading to an MPH in general epidemiology followed by an intensive field year with structured tasks that reinforce those principles learned in the classroom through experiential learning in the field. Together, the coursework and practicum training provided during the two-year program meet all of the ACGME competencies for PMRs, and in several cases exceed them. However, given this program's special emphasis on training physician epidemiologists who will work in public health practice settings, it seems appropriate to assess it in the context of how well it meets these newly developed AECs both to identify potential training gaps and to assess the usefulness of the new competencies in doing so.
The mapping of the practicum tasks and required academic coursework against the AECs revealed that almost all were satisfied, albeit sometimes minimally, despite the current program being structured on a different set of ACGME competencies. The majority of the AECs appear to be adequately covered by a combination of coursework in the academic year and tasks performed in the practicum year. Only one AEC, 7B—“Promote the organization's vision in all programs and activities”—was not met in either the practicum or academic year of training, and only one other competency, 6C—“Implement operational and financial plans”—was met in a single required course and not in the practicum year at all. This is perhaps not surprising given that neither of these are ACGME competencies for PMRs, nor would these typically be taught in an epidemiology MPH program.
Beyond these obvious deficiencies, other areas in which the residency minimally met the AECs (the Table) and we deemed weak tended to be those found in domain 6 (financial and operational planning and management) and domain 7 (leadership and systems thinking). Again, the competencies in these two domains are largely not taught in the standard MPH epidemiology curriculum and most are not covered in the ACGME competencies, although they could be considered reasonable competencies for practicing epidemiologists.
The areas of training strength were clearly in domain 1 (assessment and analysis) and domain 2 (basic public health sciences). The UM Department of Epidemiology has a strong focus on methods, analysis, statistical software use, and pathophysiology of disease in its MPH epidemiology program. Not surprisingly, this was reflected in the program meeting virtually all of the competencies belonging to one of these two domains. In general, competencies' strengths seemed to correlate much better with those provided through academic coursework rather than practicum training. The converse was largely true in that AECs that would probably be thought of as more experiential, and therefore covered in the practicum year, were more likely to be training weaknesses. For example, risk communication as a competency was relatively weak in UM's residency even though this could reasonably be expected to be a component of practicum training in a PMR.
There is no doubt that the practicum year of PMRs is more variable in content as individual residents' interest, rotation availability and selection, and variability in site supervisors all collectively impact which rotations, with their associated tasks, are completed. This makes it more difficult to reliably depend on a predetermined set of competencies being satisfied in the practicum year relative to an academic year comprised of classes that tend to be more standardized and less variable over time. By the same token, many of the AECs were significantly augmented or completely fulfilled by the training experiences of our program's practicum year. In that light, it seems problematic to expect MPH graduate programs in epidemiology to meet these same competencies without the experiential component of training that preventive medicine residents receive in the practicum year.
We had never gone through the exercise of formally mapping the academic coursework and practicum tasks in this residency to any competencies, although the program was specifically designed to meet ACGME competencies. We found using the AECs to do so both feasible and useful. It especially permitted us to identify our training strengths and also several training gaps in our program, mostly in the practicum year. This is fortunate in that as a small training program in a large school of public health, it would be much more difficult to alter the required MPH curriculum based on our residency needs than it would be for us to change the tasks in our practicum year to better meet these competencies. We mostly found these AECs reasonable, although we felt that a few of the experiential ones might be considered more appropriate to a senior-level manager than to a mid-level epidemiologist.
The most time-consuming aspect of the mapping was obtaining the individual course syllabi and associated learning objectives and also grouping the many practicum tasks into categories. We did not find the actual exercise of mapping particularly difficult, but we mapped only to the 38 main competencies. The entire AECs document includes a very large number of subcompetencies and sub-subcompetencies, and using all of those would be correspondingly more complex.
REFERENCES
- 1.Council of State and Territorial Epidemiologists. Atlanta: CSTE; 2004. 2004 national assessment of epidemiologic capacity: findings and recommendations. [Google Scholar]
- 2.Assessment of epidemiologic capacity in state and territorial health departments—United States, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(18):457–9. [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. List of ACGME accredited programs and sponsoring institutions. [cited 2007 Jan 28]. Available from: URL: http://www.acgme.org/adspublic.
- 4.American College of Preventive Medicine. Estimating the need for preventive medicine physicians. Testimony of Dr. Michael Parkinson before the Institute of Medicine Committee on Training Physicians for Careers in Public Health. 2006 Oct 5.
- 5.American Board of Preventive Medicine. Examination pass rates. [cited 2007 Jan 28]. Available from: URL: http://www.abprevmed.org/pass_rates.cfm.
- 6.Michigan Department of Community Health. The epidemiology initiative. Bureau of Epidemiology. 2000. Fall. MDCH. Epi-Insight.
- 7.Council of State and Territorial Epidemiologists. Competencies for applied epidemiologists in governmental public health agencies (AECs) [cited 2007 Jan 29]. Available from: URL: http://www.cdc.gov/od/owcd/cdd/aec or http://www.cste.org/competencies.asp.
- 8.Council on Linkages Between Academia and Public Health Practice. Core competencies for public health professionals. [cited 2007 Jan 27]. Available from: URL: http://www.phf.org/Link.htm.
- 9.Calhoun JG, Rowney R, Eng E, Hoffman Y. Competency mapping and analysis for public health preparedness training initiatives. Public Health Rep. 2005;120(Suppl 1):91–9. doi: 10.1177/00333549051200S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (US) and Council of State and Territorial Epidemiologists. Competencies for applied epidemiologists in governmental public health agencies (AECs): Tier 2: mid-level epidemiologist. [cited 2007 Oct 9]. Available from: URL: http://www.cste.org/Assessment/competencies/pdffiles/AEC521SummaryTier2.pdf.
- 11.Accreditation Council for Graduate Medical Education. Preventive medicine competencies (linkages) [cited 2007 Jan 29]. Available from: URL: http://www.acgme.org/acWebsite/RRC_380/380_pmComp.asp.