SYNOPSIS
Field epidemiology training programs have been successful models to address a country's needs for a skilled public health workforce, partly due to their responsiveness to the countries' unique needs. The Centers for Disease Control and Prevention has partnered with ministries of health to strengthen their workforce through customized competency-based training programs. While desirable, emphasis on program flexibility can result in redundancy and inconsistency. To address this challenge, the ADDIE model (analysis, design, development, implementation, and evaluation) of instructional design was used by a cross-functional team to guide completion of a standard curriculum based on 15 competencies. The standard curriculum has supported the development and expansion of programs while still allowing for adaptation. This article describes the process that was used to develop the curriculum, which, together with needs assessment and evaluation, is crucial for successful training programs.
As the 2006 World Health Report indicates, the development and maintenance of a trained and motivated workforce is a complex system with unique challenges and solutions facing every country.1 Field epidemiology training programs (FETPs) are highly successful models for addressing this need. FETPs, based on the Centers for Disease Control and Prevention Epidemic Intelligence Service (CDC EIS), are applied epidemiology programs designed to improve and strengthen public health systems and infrastructure. The cornerstone of the FETP is training through service—providing real services to a country's ministry of health while achieving competency in applied epidemiology. Achievement of the program competencies is accomplished in two years by dedicating 30%–40% of a resident's time to the classroom and 60%–70% of the time to fieldwork.2 Program participants are frequently assigned to departments in the ministry of health and are responsible for activities in the department as well as for the FETP.
Over the last 30 years, more than 32 countries have created FETPs in their ministries of health to provide competency-based training for epidemiologists, program managers, and other health workers.3,4 Outside the U.S., there are now more than 1,200 graduates and participants who have trained tens of thousands more.3,5 An outstanding contribution of the programs' participants and graduates is the investigation of epidemics and other public health emergencies. Many epidemiologists involved in controlling the recent outbreaks of severe acute respiratory syndrome were from FETPs and EIS, including the participants of the China FETP in 2003.6 Participants and staff also investigated and helped control many outbreaks of cholera, human immunodeficiency virus, measles, and other infectious diseases; they strengthened surveillance systems (such as those that detected the resurgence of cholera and outbreaks of vaccine-associated polio in the Americas); and designed behavioral risk factor surveillance for chronic diseases and surveys for program targeting and implementation.7 In describing Mexico's dramatic successes in reducing infant mortality rates, Jaime Sepulveda, former Minister of Health, singled out the FETP as one of the critical success factors.8
FETPs have been highly successful in building a workforce and producing high-quality output, based in large part on their response to a country's unique needs and the personal attention of the participants' mentors.2 Programs and curricula have been developed on a case-by-case basis based on country priorities. However, this flexibility and uniqueness of programs can present challenges. FETPs are expensive in terms of technical assistance; an experienced consultant provides apprenticeship-style training to five to 10 participants per year for the first four to 10 years at a typical annual cost of $300,000 to $500,000.2,9 Complacency can form as a program matures and newer challenges capture the attention and funding of ministries and donors. This complacency could result in a decrease in program quality. Concern for program quality has led the Training Programs in Epidemiology and Public Health Interventions Network (TEPHINET) to recommend indicators and processes to evaluate and monitor FETPs.10 Challenges can also arise with program expansion and the need to decentralize training, as human and financial resources are stretched.
To help address these challenges, in 2003, the Division of Global Public Health Capacity Development (DGPHCD) undertook a project to develop a standard FETP curriculum that could serve as a guide for countries as they develop or expand an FETP. This cross-functional project was led by the DGPHCD instructional design staff. Instructional design refers to the systematic process of translating principles of adult learning and instruction into plans for instructional materials and activities.11 This article describes the process of developing and using a standardized curriculum to support the development and expansion of FETPs.
METHODS
The instructional design team in CDC's DGPHCD led the project and began with a comprehensive needs assessment. The process took into consideration key principles of adult learning, an environment that is different from teaching children in school or university students.12 As they mature, adults tend to prefer self-direction, and their experiences provide a rich resource for learning.13 Adults are aware of specific learning needs generated by events such as obtaining a new job. Most importantly for this discussion, adults are competency-based learners: they obtain and apply their knowledge and skills in the work or home environment.14
The instructional design staff introduced the team to a process known as the ADDIE (analysis, design, development, implementation, and evaluation) model.15 This model is commonly used in instructional systems development as a systematic means to achieve the desired results.
To conduct the needs assessment, we set aside past assumptions about what must be taught and began with an analysis of the tasks that a typical epidemiologist must undertake upon completing a two-year program. Based on DGPHCD's experience with prior training programs, we approached the needs analysis phase with the following assumptions:
Target audience participants had a medical background, such as a medical doctor, nurse, or veterinarian. Participants had basic computer literacy, were available full-time for a two-year program, and were committed to learning.
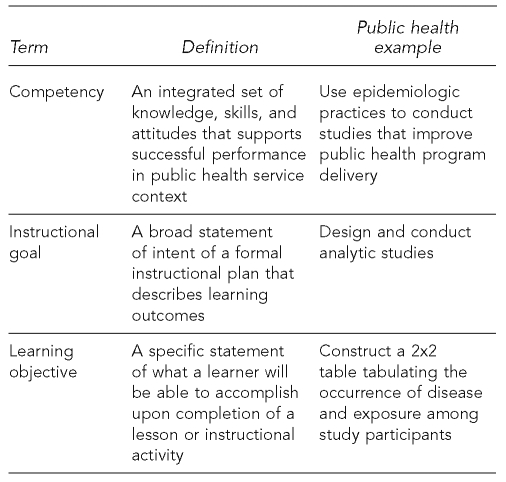
Competencies were defined as the reasonable responsibilities of graduates at their first job after program completion. Figure 1 defines key instructional design terms used during the project, with an example from public health practice.
A completed curriculum should be structured enough to use as a guideline, yet flexible enough to be customized based on ministry of health priorities.
Figure 1.
Glossary of instructional design terms
We began the needs assessment in July 2003 by reviewing the literature and curricula from established FETPs that are members of TEPHINET and through material posted on the TEPHINET website.5 We also consulted with CDC colleagues who manage the EIS.16 We reviewed the competencies and work by the Council of State and Territorial Epidemiologists and the Council on Linkages Between Academia and Public Health Practice.10,17,18 From this review, we identified 10 competency areas, such as epidemiologic methods, biostatistics, public health surveillance, and computer technology. To keep the project manageable, we agreed to focus on these 10 core competencies: those competencies that, regardless of any curriculum customization, should be included to some degree in any FETP. In September 2003, a team of instructional designers interviewed experienced field epidemiologists and resident advisors based in the U.S. and abroad. Using worksheets created for the project, we asked these experts the following questions:
What major duties or responsibilities in this competency area would you expect FETP graduates to have in their first position after completing the training program?
How frequently would they perform that duty?
How would you describe a successful graduate in this area?
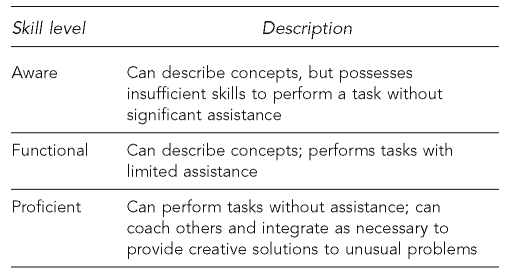
We also asked the field epidemiologists and resident advisors their assumptions about previous education, previous position, and additional skills, such as language or computer skills. The results of the interviews helped prioritize the tasks and identify the required proficiency level of a skill, described in Figure 2.
Figure 2.
Glossary of proficiency levels
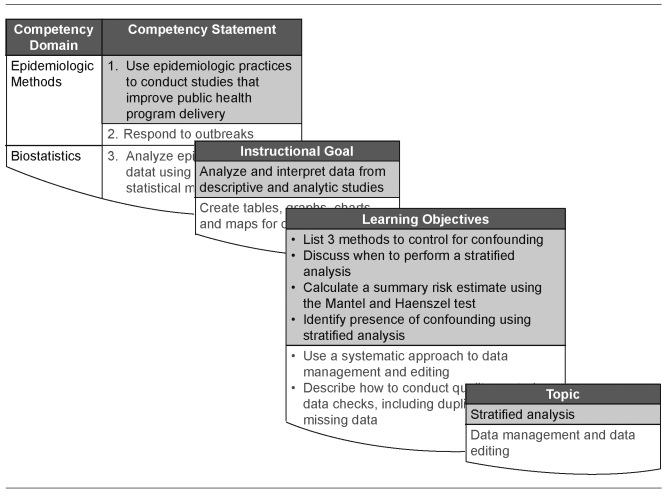
Based on these interviews, we compiled a list of competency statements within each area. To support each competency statement, the curriculum project team developed instructional goals and learning objectives that were detailed enough to inform content development, assignment of activities in the field, and learner assessment and evaluation. The purpose of an instructional goal is to guide development of an instructional activity and provide a starting point for subsequent planning.11,19 The purpose of a learning objective is to frame specific lessons within an instructional goal and provide guidelines for content development, delivery method, and evaluation.11,15,20 These instructional design techniques have been shown to be effective at developing measurable instructional elements.11,19 Figure 3 shows the competency-instructional goal-learning objectives relationships, based on the goal to improve public health. When planning a training program, learning objectives are often clustered in themes or topics.
Figure 3.
Relationship among competencies, instructional goals, and learning objectives
By September 2004, the team completed a first draft of the curriculum. We took the materials to the Third Global Scientific Conference for TEPHINET in Beijing, China, delivered a presentation to conference participants to inform them of the project, and distributed packets to 50 FETP directors from organizations around the globe. Reviewers were asked for their opinions regarding the curriculum's technical content as well as the format and usefulness of supplemental materials. Eleven reviewers representing programs in diverse countries such as Argentina, India, and Uganda returned comments, which were incorporated into subsequent drafts. A final draft was posted on the CDC DGPHCD website in August 2005 (www.cdc.gov/cogh/dgphcd).
RESULTS
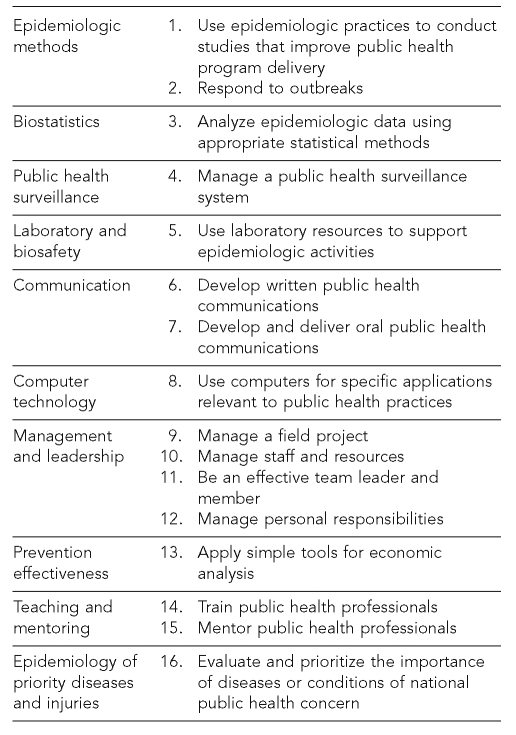
The final proposed curriculum consists of 16 competency statements, containing 47 instructional goals. Figure 4 summarizes the FETP core competencies by area. Detailed learning objectives supporting the instructional goals are grouped logically into 77 topics, ranging from Introduction to Sampling to Public Health Economics. For example, in the Epidemiologic Methods competency area, two statements were identified. One of these statements, “Use epidemiologic practices to conduct studies that improve public health program delivery,” is defined by nine instructional goals. One of these goals, “Analyze and interpret data from descriptive and analytic studies,” was further tied to six sets of learning objectives, summarized as topics such as “stratified analysis.” These detailed learning objectives can form the backbone of the development of course syllabi, training materials, field activities, and evaluation instruments.
Figure 4.
Centers for Disease Control and Prevention field epidemiology training program competencies
In addition to the final curriculum, a Curriculum at a Glance tool provides a summary of all topics for quick reference and curriculum planning. After the curriculum was released in August 2005, it quickly became the fourth most downloaded file on the DGPHCD website and remained within the top 10 downloads in subsequent months. Since its original release, the curriculum has been translated into Spanish, and it has been adapted by many of the programs supported by DGPHCD.
DGPHCD staff put the standard curriculum to immediate use as they worked with countries to develop or modify programs. In South Africa, the standard curriculum was used in 2006 as a basis for comparison with the Master of Public Health degree at the University of Pretoria. This allowed the program to compare similar subjects by learning objective and provide justification to the university to conduct certain components of the program at the National Institute of Communicable Disease. In addition, the level of detail contained within the curriculum enabled the identification of field component requirements for certain subjects. Development time was reduced, as it allowed a customized curriculum to be created and proposed to the university during the course of a two-day workshop.
In Pakistan, the standard curriculum was used as the backbone of its curriculum and accreditation workgroup discussion in the program development workshop. During this meeting, representatives from various sectors of public health and academia within Pakistan discussed the program's major elements based on competencies and outputs that are anticipated of graduates upon program completion. In contrast to prior practices of gathering different curricula from a variety of sources to develop an entire curriculum, meeting participants were able to save time by using the standard curriculum to fulfill basic requirements and focus their meeting time on tailoring the curriculum to meet Pakistan's needs. Specifically, two competencies, Community Mobilization and Ethics and Values, were added to the curriculum to address cultural and societal interests.
Existing programs in China, El Salvador, Guatemala, Honduras, Jordan, and other countries are tailoring the curriculum to meet their needs and enriching the training materials with local examples that resonate with the learners. The Brazil FETP referred to the curriculum for guidance when preparing for the next phase of its program. The Brazil team identified the timely analysis of surveillance data in the detection of outbreaks as a priority to emphasize in the training program. The Egypt and Jordan FETP programs utilized the curriculum when developing their training in the surveillance and prevention of chronic diseases. Central American countries have developed a three-tiered approach to strengthen skills in surveillance and applied epidemiology, with opportunities to learn in a progressive pyramid structure. This strategy enables some learners to participate in shorter, part-time programs, with a subset of those learners advancing to a comprehensive two-year full-time program. In 2006, the standard curriculum was used to review each program level, identify gaps, and ensure a smooth transition from one level to the next. Regional public health priorities have been easily infused into the standard curriculum, such as using the response to Hurricane Stan in Guatemala as an example for surveillance, disaster response, and communications lessons.
DISCUSSION
The standard curriculum was developed in response to a perceived need to reduce duplication of effort when developing new training programs, to lower development costs, to provide greater consistency among programs, and to establish a documented baseline against which performance indicators can be created. Although the development of a standard curriculum is thought to improve the consistency and quality of program instruction, the staff involved in this project felt it was vital to create a customizable product that could suit the needs of any given country. As a result, the curriculum was designed to be easily adapted to support a country's specific public health situation.
The next step of the project is to develop standardized training materials including content, exercises, and evaluation tools that support the curriculum learning objectives. Providing detailed training materials will further help countries establish their own programs and help sustain existing programs. Collecting and evaluating existing training resources from current and previous FETPs, as well as designing new materials, is ongoing.
To quantify the impact of a standard curriculum on the development and management of FETPs, and to evaluate if use of the standard curriculum produced its expected benefits, we propose several indicators. We suggest the development of indicators related to users' perceptions of usefulness, flexibility, and quality of the standard curriculum to measure the curriculum's effectiveness in overcoming the program challenges referenced earlier. Consistent quality despite customization can be measured by administering an evaluation of competencies that have been identified as core regardless of customization. For example, all program graduates are expected to be able to accurately analyze and interpret surveillance data. One country may prioritize behavioral risk factor surveillance, another, acute flaccid paralysis surveillance, but the data analysis competency requirement remains.
Reducing development time for the FETP curriculum should lead to more rapid implementation of an FETP, thereby releasing additional resources that can be devoted to direct training and mentoring of students. Quantifying the reduction in development time and costs through the use of the standard curriculum requires indicators that reflect the expense of modifying a standard curriculum vs. reinventing a specialized curriculum for every new country that begins an FETP. Measuring reductions in outside technical curriculum consultants, including their travel costs, to new FETP countries will also assess the benefit of a standard curriculum. Cost reductions may also be seen in the development of other public health programs, when public health workers who have become familiar with the connections among competencies, instructional goals, and learning objectives apply these principles to curriculum development.
Limitations
The development of the standard curriculum has at least four limitations. First, though a concerted effort was made to obtain input from all FETPs that are members of TEPHINET, only 20% gave input on the final draft. As programs use the curriculum, gaps may be identified and improvements can be made. Second, instructional goals and learning objectives have traditionally been used in designing discrete short-term courses. Creating detailed learning objectives to articulate a two-year program means that each country may still need to break the learning objectives into smaller units based on course structure and local requirements. Third, baseline data specific to curriculum development costs were not available to measure expected cost savings. Accurate baseline data are needed to correctly quantify any reduction in development time and costs through the use of the standard curriculum. Fourth, the use of instructional design terminology and organization embedded within a highly technical curriculum may cause some initial confusion among FETP program staff, perhaps leading to low acceptance.
CONCLUSIONS
In 2006, a working group of 35 representatives of bilateral and multilateral agencies, sponsored by the World Health Organization, proposed that a common technical framework can help support the development of a sustainable health workforce.1,21 The ADDIE model provides a common process to design, develop, and deliver training—an integral component of workforce development. This systematic approach to workforce development can help a cross-functional team address a training need methodically, with expected results that can be measured. A standard documented curriculum can reduce duplication and promote quality and consistency.
The FETP model has already been adopted in many countries that want to build human capacity in field epidemiology. Other countries may also want to begin their own training programs. Replication of the FETP model depends on many external factors, such as a country's political stability or a program's economic feasibility, and a new program's curriculum is just one contributor to a program's success. A standard field epidemiology curriculum will encourage new programs to build upon the instructional blueprint of their successful FETP predecessors, taking advantage of the common goals of all FETPs while allowing for local perspective.
The process the team employed to develop a curriculum, as well as the lessons learned, can benefit the development of other public health applied training programs, including schools of public health. In particular, the use of a cross-functional team that included instructional design professionals, epidemiologists, and other subject matter experts provided the required skills to support technical content as well as sound adult education principles. The project required the presence of key advocates to build consensus and attain agreement of the need and benefit of standardization. Finally, throughout the project the curriculum development team reminded itself that the program centers on the learner, not the instructor, and is based on performance, not merely knowledge. This reminder helped us resolve differences of opinion and develop a competency-based curriculum that supports consistently high-quality results.
Acknowledgments
The authors thank the core members of the team in the Division of Global Public Health Capacity Development who assisted with this project from beginning to end, particularly Douglas Klaucke, who launched the project, as well as Elliott Churchill, Hoang Dang, Suzanne Elbon, Ed Maes, Jim Mendlein, and Peter Nsubuga. The authors also thank the representatives of the field epidemiology training programs in 11 countries for their timely and thoughtful comments. Thanks to Pascale Krumm for her careful editing.
REFERENCES
- 1.Evans T, editor. Geneva: World Health Organization; 2006. The World Health Report 2006: working together for health. [Google Scholar]
- 2.White ME, McDonnell SM, Werker DH, Cardenas DM, Thacker SB. Partnerships in international applied epidemiology training and service, 1975–2001. Am J Epidemiol. 2001;154:993–9. doi: 10.1093/aje/154.11.993. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (US). Division of Epidemiology and Surveillance Capacity Development. [cited 2007 Jan 30]; Available from: URL: http://www.cdc.gov/cogh/dgphcd.
- 4.White M, Guibert Herrera DJ, Lim-Quizon MC. Joined-up public health initiatives. Lancet. 2006;367:1301–2. doi: 10.1016/S0140-6736(06)68556-5. [DOI] [PubMed] [Google Scholar]
- 5.Training Programs in Epidemiology and Public Health Interventions Network (TEPHINET) [cited 2007 Jan 30]; doi: 10.2105/ajph.92.2.196. Available from: URL: http://www.tephinet.org. [DOI] [PMC free article] [PubMed]
- 6.Efficiency of quarantine during an epidemic of severe acute respiratory syndrome—Beijing, China, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(43):1037–40. [PubMed] [Google Scholar]
- 7.Nsubuga P, White ME, Thacker SB, Anderson MA, Blount SB, Broome CV, et al. Public health surveillance: a tool for targeting and monitoring interventions. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evan DB, et al., editors. Disease control priorities in developing countries. 2nd ed. New York: Oxford University Press; 2006. pp. 997–1015. [Google Scholar]
- 8.Sepéulveda J, Bustreo F, Tapia R, Rivera J, Lozano R, Oléaiz G, et al. Improvement of child survival in Mexico: the diagonal approach. Lancet. 2006;368:2017–27. doi: 10.1016/S0140-6736(06)69569-X. [DOI] [PubMed] [Google Scholar]
- 9.Music SI, Schultz MG. Field epidemiology training programs: new international resources. JAMA. 1990;263:3309–11. [PubMed] [Google Scholar]
- 10.Training Programs in Epidemiology and Public Health Interventions Network. [cited 2006 Sep 14];Continuous quality improvement handbook version 1.0. 2005 Nov; Available from: URL: http://www.tephinet.org.
- 11.Smith PL, Ragan TJ. Instructional design. New York: Merrill; 1993. pp. 21–3.pp. 66pp. 91 [Google Scholar]
- 12.Knowles MS, Holton E, III, Swanson A. The adult learner. Houston (TX): Gulf Publishing Co; 1998. pp. 35–72. [Google Scholar]
- 13.Lieb S Lieb S. Principles of adult learning. [cited 2006 Dec 20]; Available from: URL: http://www.Honolulu.hawaii.edu/intranet/committees/FacDevCom/guidebk/teachtip/adults-2.htm.
- 14.Edmunds CK, Lowe KM, Murray M, Seymour A. The ultimate educator: achieving maximum adult learning through training and instruction. 2002 [Google Scholar]
- 15.Molenda M, Pershing JA, Reigeluth CM. Designing instructional systems. In: Craig RL, editor. The ASTD training and development handbook. 4th ed. New York: McGraw-Hill; 1996. pp. 266–93. [Google Scholar]
- 16.Centers for Disease Control and Prevention (US). Epidemic Intelligence Service. [cited 2007 Jan 31]; Available from: URL: http://www.cdc.gov/eis.
- 17.Centers for Disease Control and Prevention (US) and Council of State and Territorial Epidemiologists. Competencies for applied epidemiologists in governmental public health agencies (AECs) [cited 2007 Oct 16]; Available from: URL: http://www.cdc.gov/od/owcd/cdd/aec or http://www.cste.org/competencies.asp.
- 18.Council on Linkages Between Academia and Public Health Practice. Core competencies for public health professionals. [cited 2007 Oct 16]; Available from: URL: http://www.phf.org/competencies.htm.
- 19.Dick WO, Carey L, Carey JO. The systematic design of instruction. 5th ed. Boston: Allyn – Bacon; 2000. pp. 5–24. [Google Scholar]
- 20.Mager RF. 3rd ed. Atlanta: Center for Effective Performance; 1997. Preparing instructional objectives: a critical tool in the development of effective instruction; pp. 3–13. [Google Scholar]
- 21.Dal Poz MR, Quain EE, O'Neil M, McCaffery J, Elzinga G, Martineau T. Addressing the health workforce crisis: towards a common approach. Hum Resour Health. 2006;4:21. doi: 10.1186/1478-4491-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]