Abstract
With a high economic, social, and personal burden, headache remains an important health problem. How UK GPs diagnose headache in the UK is unknown. In this study, a large primary care database was used and diagnostic categories were described for 91 121 adult patients with new-onset headache, that is, patients who had not consulted for headache in the previous year. Seventy per cent of headaches were not given a diagnostic label, 24% were diagnosed as primary, and 6% as secondary headaches. It is suggested that GPs' difficulty in diagnosing headache presentations contributes to the high level of morbidity and unmet need in this disease.
Keywords: diagnosis, headache, primary care
INTRODUCTION
Headache is classified as secondary where there is a plausible identifiable cause, and primary where the cause is unknown. Although headache is not life threatening, the economic, social, and personal burden of primary headache in the community is substantial. Migraine has been most extensively studied and has been shown to affect 7.6% of males and 18.3% of females in England.1 Measures of health-related quality of life of migraineurs are similar to those for patients with other chronic conditions such as arthritis and diabetes,2 and worse than for those with asthma.3
In the UK, one in three individuals with migraine believe that their problem controls their life, and two in three believe that they cannot control it at all or, at best, rarely.4 Patients who present to their GP have a high level of headache disability which has an impact on their quality of life,5 but the needs of many individuals with primary headache remain unmet. For example, half of patients with migraine who have ever consulted for their headache remained undiagnosed, with concomitant disability.6 When they do seek help, the diagnosis is often incorrect and the condition is poorly managed.7 Although cluster headache affects only 0.01% of the population, it is one of the most painful conditions a GP will ever deal with.8 In most cases, patients with cluster headache will pass through ENT (ear nose and throat), ophthalmic, or maxillofacial departments before a diagnosis is finally made. Even then the treatment is often suboptimal.9
In the UK, the annual primary care consultation rate for headache is 4.4 per 100 patients, of whom 4% are referred to secondary care for further assessment.10 Evidence-based guidelines for diagnosis and management have been published for the management of primary headaches by the British Association for the Study of Headache (www.bash.org.uk); an accurate diagnosis is an essential first step in management.11 How GPs diagnose headache is unknown. The aim of this study was to describe diagnostic patterns using a large UK primary care database.
METHOD
A cohort study was conducted using data from the General Practice Research Database (GPRD). Doctors contributing to the GPRD, record full details of patient characteristics including all consultations and diagnoses. Data are subject to thorough validation and stringent quality checks.
Patients were aged 18 years or over. They had a description of headache in their records and no other headache classification code in the previous year. Patients were accepted from the inception of the database in January 1987 to June 2005 who had at least 1 year of full data in their records after the index headache consultation. These cases were identified by GPRD staff and the full anonymised electronic records were extracted. Index headache codes were categorised into migraine, tension-type headache, or cluster headache where these terms had been used. Similarly, where a headache code was accompanied by a further descriptor, this was classified as a secondary headache. All other codes were classified as undifferentiated headache. The records of patients with undifferentiated headache were examined for the subsequent year to identify whether a further headache diagnosis was made following the initial headache consultation. Analysis was by age in eight 10-year age bands.
RESULTS
There were 91 121 adult patients who met inclusion criteria. Primary headaches accounted for 23.9% of all headaches (cluster 4.0%, tension-type 23.0%, and migraine 73.0%); secondary headaches were diagnosed in 6.0% of patients, of which 85.0% were coded as ‘sinus headache’; 70.1% did not receive a diagnosis. Of this latter group, in the following year 5.3% received a diagnosis of a primary headache (Table 1).
Table 1.
GPs' diagnoses of headache with age.
| n (%) | |||||||
|---|---|---|---|---|---|---|---|
| Primary headache, n = 21 758 (23.9) | |||||||
| Total | Females | Cluster | Migraine | Tension | Secondary headache | Undifferentiated headache | |
| Age, years | n = 91 121 | n = 60 293 | n = 880 (4.0) | n = 15 891 (23.0) | n = 4987 (73.0) | n = 5442 (6.0) | n = 63 921 (70.1) |
| 18–29 | 22 948 | 16181 (70.5) | 240 (1.0) | 4414 (19.2) | 1468 (6.4) | 966 (4.2) | 15 860 (69.1) |
| 30–39 | 21 225 | 13967 (65.8) | 219 (1.0) | 4281 (20.2) | 1247 (5.9) | 1335 (6.3) | 14 143 (66.6) |
| 40–49 | 16 410 | 10547 (64.3) | 163 (1.0) | 3348 (20.4) | 902 (5.5) | 1134 (6.9) | 10 863 (66.2) |
| 50–59 | 12 378 | 7863 (63.5) | 120 (1.0) | 2116 (17.1) | 639 (5.2) | 1007 (8.1) | 8496 (68.6) |
| 60–69 | 8604 | 5250 (61.0) | 73 (0.8) | 1021 (11.9) | 402 (4.7) | 596 (6.9) | 6512 (75.7) |
| 70–79 | 6236 | 4048 (64.9) | 45 (0.7) | 540 (8.7) | 233 (3.7) | 297 (4.8) | 5121 (82.1) |
| 80–89 | 2911 | 2101 (72.2) | 18 (0.6) | 156 (5.3) | 84 (2.9) | 98 (3.4) | 2555 (87.8) |
| ≥90 | 409 | 336 (82.2) | 2 (0.5) | 15 (3.7) | 12 (2.9) | 9 (2.2) | 371 (90.7) |
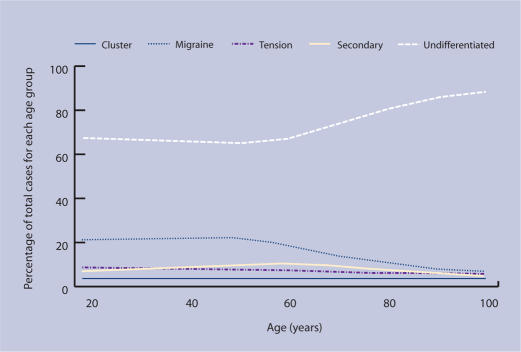
The prevalence of primary headache fell progressively after 30 years of age, with migraine remaining the most common diagnosis in all age groups. The prevalence of new undifferentiated headache rose progressively with age (Figure 1).
Figure 1.
Diagnosis of primary headache (cluster, migraine, tension-type), secondary or undifferentiated headache with age as a percentage of total cases. (n = 91 121).
How this fits in
The economic, social, and personal burden of primary headache is substantial, and headache accounts for 4% of all GP consultations. How GPs diagnose headache is not well known. This study describes how GPs diagnose new presentations of headache and how this varies with the age of the patient. In the majority of cases, a primary headache diagnosis is not made at presentation or follow up. GPs' failure to make an accurate diagnosis may contribute to high levels of morbidity and unmet need in this disease area.
DISCUSSION
Summary of main findings
In this study of new-onset headache in primary care, a formal diagnosis was not made in the majority of consultations. The proportion of patients with undifferentiated headache increased with age. This may be due to an increase in secondary headache with age leading to diagnostic uncertainty.12 Migraine was the most common diagnosis in all age groups. The reporting in this study of secondary headache diagnoses will be an underestimate. In many important secondary headaches, for example, headache due to brain tumour, GPs will code the underlying diagnosis but may not code the headache symptom that may or may not be present. However, these secondary headaches are relatively infrequent, and their exclusion should only have a minor impact on the overall results.
Of the 6% of headache cases that had a further descriptor, 85% were classified as ‘sinus headaches’. A report of 3000 patients with a history of sinus headache found that 80% had International Headache Society migraine criteria, and a further 8% were likely to have migraine. In many cases, GPs may be misdiagnosing sinus pain and missing an underlying presentation of migraine.13
Comparison with existing literature
There are few studies examining diagnoses in patients consulting with headache in primary care. One study of 1203 headache consultations across 15 countries reported a GP diagnosis of migraine in 84% of cases, non-migraine primary headache in 12%, and secondary headache in 4%. On review by an expert panel, 94% were assessed as having migraine.14 In a US study of patients consulting in primary care with headache, 69% of patients were labelled with unspecified headache. Of these, 33% were later diagnosed as having migraine.15
Strengths and limitations of the study
There are two main problems with diagnostic surveys in headache. Firstly, although diagnostic criteria for headache are formally defined by the International Headache Society,16 these may not be known to many GPs. From a clinical perspective, diagnostic criteria are invariably relaxed and will vary between GPs. Secondly, even if GPs are confident of a diagnosis, they may code for headache but enter their primary headache diagnosis in free text, which could not be accessed in this study. Thirdly, the database used did not allow coding for all diagnostic categories. For example, migraine, tension-type, and cluster headache were the only coded primary headache diagnoses available in the GPRD; however, other primary headaches are very rare.
Population studies have reported that migraine is underdiagnosed, and the high level of undiagnosed headaches in this study supports this. It may be that GPs require a number of consultations to establish a diagnosis of a primary headache. However, only 5.3% of patients with undifferentiated headache received a primary headache diagnosis in the year following presentation.
Implications for future research
The reason for GPs' failure to diagnose (or to record a diagnosis of) headache presentations, as described in this study, is not known. Evidence from other studies suggests that it may be partly due to GPs' failure to make an accurate diagnosis, contributing to the high level of morbidity and unmet need in this disease area. Research is needed to explore why GPs find it difficult to diagnose and manage headache appropriately, and to develop educational strategies to overcome this problem.
Funding body
St Thomas Medical Group and Caper Research Practices receive R&D funding from the NHS R&D Executive as GP Research Practices
Ethical approval
The study received ethical approval from the Scientific and Ethical Advisory Committee for GPRD research (MRC 783R)
Competing interests
The authors have stated that there are none
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Steiner T, Scher A, Stewart F, et al. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia. 2003;23(7):519–527. doi: 10.1046/j.1468-2982.2003.00568.x. [DOI] [PubMed] [Google Scholar]
- 2.Solomon G, Skobierand F, Gragg L. Quality of life and well-being of headache patients: measurement by the medical outcomes study instrument. Headache. 1993;33(7):351–358. doi: 10.1111/j.1526-4610.1993.hed3307351.x. [DOI] [PubMed] [Google Scholar]
- 3.Terwindt G, Ferrari M, Tijhus M, et al. The impact of migraine on quality of life in the general population — The GEM Study. Neurology. 2000;55(5):624–629. doi: 10.1212/wnl.55.5.624. [DOI] [PubMed] [Google Scholar]
- 4.Dowson A, Jagger S. The UK migraine patient survey: quality of life and treatment. Curr Med Res Opin. 1999;15(4):241–253. doi: 10.1185/03007999909116495. [DOI] [PubMed] [Google Scholar]
- 5.Ridsdale L, Clark LV, Dowson AJ, et al. How do patients referred to neurologists for headache differ from those managed in primary care? Br J Gen Pract. 2007;57(538):388–395. [PMC free article] [PubMed] [Google Scholar]
- 6.Lipton RB, Diamond S, Read M, et al. Migraine diagnosis and treatment: results from American Migraine Study II. Headache. 2001;41(7):638–645. doi: 10.1046/j.1526-4610.2001.041007638.x. [DOI] [PubMed] [Google Scholar]
- 7.Lipton RB, Scher A, Steiner T, et al. Patterns of health care utilisation for migraine in England and in the United States. Neurology. 2003;60(3):441–448. doi: 10.1212/wnl.60.3.441. [DOI] [PubMed] [Google Scholar]
- 8.Kernick D, Mathru M, Goadsby P. Cluster headache in primary care. Br J Gen Pract. 2006;56(528):486–487. [PMC free article] [PubMed] [Google Scholar]
- 9.Bahra A, Goadsby PJ. Diagnostic delays and mis-management in cluster headache. Acta Neurol Scand. 2004;109(3):175–179. doi: 10.1046/j.1600-0404.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- 10.Latinovic R, Gulliford M, Ridsdale L. Headache and migraine in primary care: consultation, prescription and referral rates in a large population. J Neurol Neurosurg Psychiatry. 2006;77(3):385–387. doi: 10.1136/jnnp.2005.073221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Flynn N, Ridsdale L. Headache in primary care: how important is diagnosis to management? Br J Gen Pract. 2002;52(480):569–573. [PMC free article] [PubMed] [Google Scholar]
- 12.Hamilton W, Kernick D. Clinical features of primary brain tumours: a case–control study using electronic primary care records. Br J Gen Pract. 2007;57(542):695–699. [PMC free article] [PubMed] [Google Scholar]
- 13.Schreiber C, Hutchinson S, Webster C, et al. Prevalence of migraine in patients with a history of self reported or physician diagnosed sinus headache. Arch Intern Med. 2004;164(16):1769–1772. doi: 10.1001/archinte.164.16.1769. [DOI] [PubMed] [Google Scholar]
- 14.Tepper S, Dahlof C, Dowson A, et al. Prevalence and diagnosis of migraine in patients consulting their physician with a complaint of headache: data from the Landmark Study. Headache. 2004;44(9):856–864. doi: 10.1111/j.1526-4610.2004.04167.x. [DOI] [PubMed] [Google Scholar]
- 15.Smith R, Hasse L, Ritchey PN, et al. Poster Session I. A: Diagnosis and clinical features. Extent of migraine and migrainous headache in NOS patients in family practice. Cephalalgia. 2001;21(4):291–292. [Google Scholar]
- 16.International Headache Society. The international classification of headache disorders. Cephalalgia. 2004;24(Suppl):1–160. 2nd edn. [Google Scholar]