Abstract
Ebola virus (EBOV), a public health concern in Africa and a potential biological weapon, is classified as a biosafety level-4 agent because of its high mortality rate and the lack of approved vaccines and antivirals. Basic research into the mechanisms of EBOV pathogenicity and the development of effective countermeasures are restricted by the current biosafety classification of EBOVs. We therefore developed biologically contained EBOV that express a reporter gene instead of the VP30 gene, which encodes an essential transcription factor. A Vero cell line that stably expresses VP30 provides this essential protein in trans and biologically confines the virus to its complete replication cycle in this cell line. This complementation approach is highly efficient because biologically contained EBOVs lacking the VP30 gene grow to titers similar to those obtained with wild-type virus. Moreover, EBOVs lacking the VP30 gene are indistinguishable in their morphology from wild-type virus and are genetically stable, as determined by sequence analysis after seven serial passages in VP30-expressing Vero cells. We propose that this system provides a safe means to handle EBOV outside a biosafety level-4 facility and will stimulate critical studies on the EBOV life cycle as well as large-scale screening efforts for compounds with activity against this lethal virus.
Keywords: antiviral screening, reverse genetics, vaccine development
Ebola viruses (EBOVs) cause hemorrhagic fevers in humans and nonhuman primates, with case fatality rates of 90% in some outbreaks (1). EBOVs and the closely related Marburg viruses belong to the Filoviridae family (2). Currently, there are no approved vaccines or antivirals for use against filoviruses, making biosafety level-4 (BSL-4) containment a mandatory requirement for work with these viruses. The lack of sufficient BSL-4 space and trained personnel and the rigors of working in BSL-4 laboratories have severely hampered basic research with EBOVs as well as the development of vaccines and large-scale screening for effective antiviral compounds. These limitations have prompted examination of various steps in the EBOV viral life cycle in the absence of infectious virus: (i) replication and transcription were studied by use of reporter gene assays that are based on the expression of necessary viral components from plasmids (3–7); (ii) entry and fusion processes were assessed with pseudotyping assays that rely on the use of recombinant vesicular stomatitis or retroviruses (8–11); and (iii) budding was examined by using virus-like particles that are generated from viral proteins provided by protein expression plasmids (12–16). However, several recent findings suggest that data obtained with these artificial systems may not always be reproducible with live, authentic EBOV (17). Thus, biologically contained EBOVs that resemble wild-type virus but can be handled outside BSL-4 containment are clearly needed.
EBOVs possess a negative-sense, nonsegmented RNA genome, ≈19 kb in length, that encodes seven structural proteins and at least one nonstructural protein (1). NP, viral protein (VP)35, VP30, and L, the RNA-dependent RNA polymerase, are components of the nucleocapsid and are essential for viral replication and transcription (5). VP40 is the matrix protein and is critical for viral budding (18, 19). VP24 is essential for the formation of nucleocapsids composed of NP, VP35, and viral RNA (20). The only viral surface glycoprotein, GP, plays a role in viral attachment and entry (21–24).
Reverse genetics systems for negative-sense RNA viruses (i.e., their artificial generation and modification from cloned cDNAs) are now established in the field (25, 26). We have exploited this technology to generate EBOVs that lack the essential VP30 gene and are maintained by—and biologically confined to—a cell line expressing VP30. The resultant viruses resemble wild-type virus in their life cycle, their morphology, and their growth properties but could be handled in a non-BSL-4 laboratory, opening new opportunities for study of the EBOV life cycle and for the identification of effective antiviral compounds. EBOVs lacking the VP30 gene are also candidates for vaccine development.
Results and Discussion
Generation and Passage of EbolaΔVP30-neo Virus.
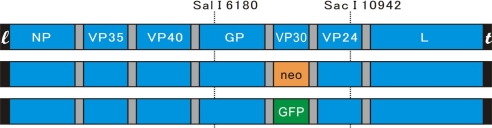
We previously established a full-length cDNA clone of the Zaire EBOV, Mayinga (26). Using a subgenomic fragment that encompasses nucleotides 6180–10942 of the viral genome (numbers refer to the positive-sense antigenome), we replaced the ORF for VP30 with that of neomycin (neo) using a series of overlapping PCR amplification steps. After confirmation of the authenticity of the PCR fragments by sequence analysis, the altered subgenomic fragment was inserted into the full-length EBOV cDNA construct via unique SalI and SacI restriction sites (Fig. 1), resulting in an EBOV cDNA genome deficient in the VP30 ORF. The artificial generation of EBOV from plasmids is afforded by flanking this viral cDNA with T7 RNA polymerase promoter and hepatitis delta virus ribozyme sequences (26).
Fig. 1.
Schematic diagram of EbolaΔVP30 constructs. The top row shows a schematic diagram of the EBOV genome flanked by the leader sequence (l) and the trailer sequence (t) in positive-sense orientation. Two unique restriction sites for SalI and SacI (positions 6180 and 10942 of the viral antigenome, respectively) allowed the subcloning of a fragment that spans the VP30 gene. The subgenomic fragment was then used to replace the VP30 gene with genes encoding neo or eGFP, respectively. By using the unique restriction sites, the altered subgenomic fragments were cloned back into the full-length EBOV cDNA construct.
To amplify VP30-deficient EBOVs, we established a stable Vero E6 cell line (designated VeroVP30) by cotransfecting Vero cells with two protein expression plasmids encoding VP30 (pCAG-VP30) and puromycin (pPur; Clontech) and selecting cell clones resistant to 5.0 μg/ml puromycin. VP30 expression in individual clones was determined by flow cytometry with antibodies to VP30. The clone with the highest percentage of VP30-expressing cells (>90% as measured by flow cytometry; data not shown) was used in further studies to amplify EbolaΔVP30 viruses.
EbolaΔVP30-neo virus was rescued under BSL-4 conditions as described previously for wild-type EBOV (26). All work involving infectious EboΔVP30 viruses and all steps before inactivation of biological material were performed under BSL-4 conditions at the National Microbiology Laboratory of the Public Health Agency of Canada.
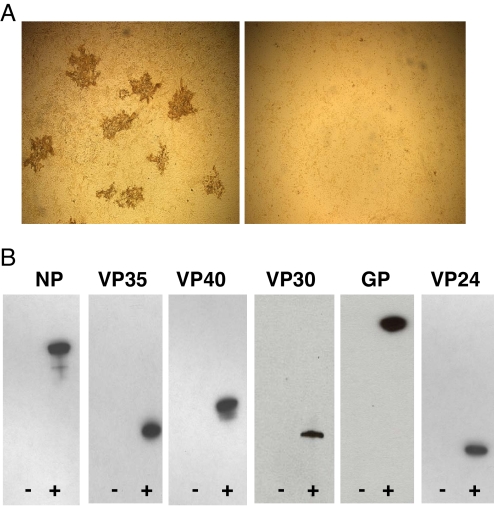
Briefly, human embryonic kidney (293T) cells were transfected with a plasmid for the transcription of the VP30-deficient EBOV RNA, with plasmids for the expression of the EBOV NP, VP30, VP35, and L proteins, and with a plasmid for the expression of T7 RNA polymerase. Five days after transfection, VeroVP30 cells were incubated with undiluted supernatant derived from plasmid-transfected cells. Seven days later, the supernatant was harvested, diluted 10-fold, and used to infect fresh VeroVP30 cells for the next passage. A total of seven passages were carried out, using the highest dilution of the inoculum that still produced replicating viruses for each passage. The presence of replicating virus was assessed by cytopathic effects and immunostaining of infected VeroVP30 cells with an antibody to VP40 (Fig. 2A Left). As a control, we also incubated the supernatants from each passage with wild-type Vero cells. As expected, we were unable to detect virus by cytopathic effects or viral antigens in wild-type Vero cells (Fig. 2A Right), demonstrating that replicating EbolaΔVP30-neo virus was confined to VeroVP30 cells.
Fig. 2.
Characterization of EbolaΔVP30-neo virus. (A) Expression of EBOV antigens by infected VeroVP30 cells. Confluent VeroVP30 cells (Left) or wild-type Vero cells (Right) were infected with EbolaΔVP30-neo for 60 min, washed, and overlaid with propagation medium with 1.5% methylcellulose. Seven days later, cells were fixed with 10% buffered formaldehyde and an immunostaining assay with an antibody to EBOV VP40 protein was performed as described in Materials and Methods. The formation of plaques in the VeroVP30 cell monolayer (Left), but not in monolayers of wild-type Vero cells (Right), illustrates that EbolaΔVP30-neo virus is biologically contained. (B) Detection of EbolaΔVP30-neo viral proteins. Supernatants derived from infected VeroVP30 (labeled +) or wild-type Vero (labeled −) cells were collected 5 days after infection and partially purified over 20% sucrose. Protein pellets were suspended in PBS and separated on polyacrylamide gels, transferred to membranes, and probed with specific antibodies to EBOV proteins.
Although the manifestation of cytopathic effects by virus in infected VeroVP30 cells suggested the formation of infectious (but biologically contained) EBOVs, we sought further evidence for the presence of virions in cell culture supernatant derived from infected VeroVP30 cells. Briefly, 5 days after VeroVP30 cells were infected with EbolaΔVP30-neo virus, supernatant was collected and partially purified over 20% sucrose. The pellet was suspended in PBS and separated on a 4–20% polyacrylamide gel. Western blot analyses were carried out with antibodies specific to the respective EBOV protein. All viral proteins (with the exception of L, for which no antibody was available) were detected (Fig. 2B, + lanes). Note that VP30 protein in virions originates from VeroVP30 cells whereas the remaining proteins are encoded by EbolaΔVP30-neo virus. By contrast, no viral proteins were detected in a control sample derived from wild-type Vero cells infected with EbolaΔVP30-neo virus (Fig. 2B, − lanes).
Genetic Stability of EbolaΔVP30-neo Virus.
A major concern with the use of VP30-deficient EBOVs is the potential recombination with VP30 sequences integrated into the genome of the VeroVP30 helper cell line. Thus, to assess the genomic stability of EbolaΔVP30-neo virus, we performed three independent passage experiments (seven passages each). Whereas EbolaΔVP30-neo virus replicated in VeroVP30 cells, viral replication was not observed in wild-type Vero cells. Total viral RNA was isolated from the cell culture supernatant of infected VeroVP30 cells after the seventh passage. A viral genomic fragment spanning the neo gene was amplified by RT-PCR, cloned, and sequenced. A total of 20 clones were sequenced, and the sequences were identical to that of the EbolaΔVP30 cDNA construct used for virus generation. Hence, there was no evidence of recombination in any of three independent passage experiments, attesting to the genomic stability of the EbolaΔVP30-neo viral genome.
To further demonstrate the biosafety of EbolaΔVP30-neo virus, we collected EbolaΔVP30-neo virus after seven consecutive passages in VeroVP30 cells and used this virus for three consecutive “blind” passages in wild-type Vero cells. Briefly, Vero cells were infected at a multiplicity of infection (m.o.i.) of 5 with EbolaΔVP30-neo virus (passage 7). Six days later, supernatant was used for the next blind passage as well as for Western blot analysis. No viral NP protein was detected after any of the blind passages (data not shown). After three consecutive blind passages, plaque assays and immunostaining were carried out in wild-type Vero cells to confirm the absence of replicating EBOV. As expected, we did not detect any replicating virus (data not shown). Collectively, these data further attest to the biosafety of the EbolaΔVP30 system.
Growth Kinetics of EbolaΔVP30-neo Virus.
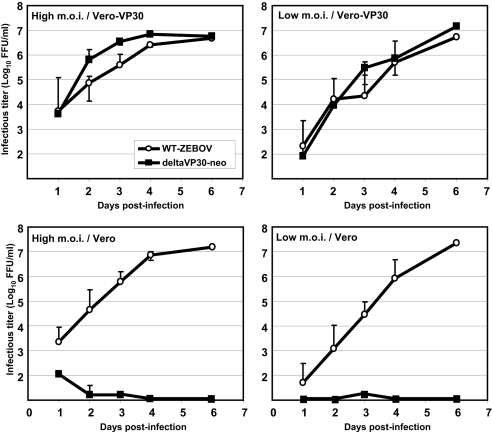
One of the major concerns raised by providing viral proteins in trans is that their amounts, expression kinetics, or both may not match those found in cells infected with wild-type virus, leading to reduced virus titers and/or aberrant virion morphology. To address this potential pitfall, we first compared the growth kinetics of EbolaΔVP30-neo virus (Fig. 3Upper) with that of wild-type EBOV (Fig. 3, open circles). VeroVP30 cells (Fig. 3 Upper) or wild-type Vero cells (Fig. 3 Lower) were infected at a high m.o.i. of 1.0 or a low m.o.i. of 0.01, and supernatant was harvested every 24 h. Virus titers of EbolaΔVP30-neo were determined in VeroVP30 cells, whereas virus titers of wild-type EBOV were determined in wild-type Vero cells. To determine virus titers, cells were overlaid with 1.5% methylcellulose and, 7 days later, assayed for VP40 expression by using an immunostaining assay. EbolaΔVP30-neo virus replicated efficiently in VeroVP30 cells at both conditions tested, reaching 107 focal-forming units per milliliter on day 6 after infection (Fig. 3 Upper, filled squares). No replication of EbolaΔVP30-neo was detected in wild-type Vero cells (Fig. 3 Lower, filled squares); the low titers that were detected for up to 3 days after infection likely reflect input virus. Together, these findings attest to the biological confinement of the EbolaΔVP30 system. The replication kinetics of EbolaΔVP30-neo in VeroVP30 cells are similar to those of wild-type EBOV in either VeroVP30 cells (Fig. 3 Upper, open circles) or wild-type Vero cells (Fig. 3 Lower, open circles), establishing the described approach as a highly efficient method for generating biologically contained EBOVs.
Fig. 3.
Replication kinetics of wild-type EBOV and EbolaΔVP30-neo virus. VeroVP30 cells (Upper) and wild-type Vero cells (Lower) were infected with EBOV or EbolaΔVP30-neo at a high m.o.i. of 1.0 (Left) or a low m.o.i. of 0.01 (Right). Supernatants were harvested every 24 h after infection for 6 days. Viral titers of the respective viruses were determined by infecting confluent VeroVP30 cells or wild-type Vero cells with 10-fold dilutions of the supernatants and subsequent immunostaining as described in Materials and Methods. Virus titers for EbolaΔVP30-neo virus (filled squares) and wild-type EBOV (open circles) were comparable in VeroVP30 cells (Upper). In wild-type Vero cells (Lower), no replication was detected for EbolaΔVP30-neo virus (filled squares).
Morphology of EbolaΔVP30-neo Virus.
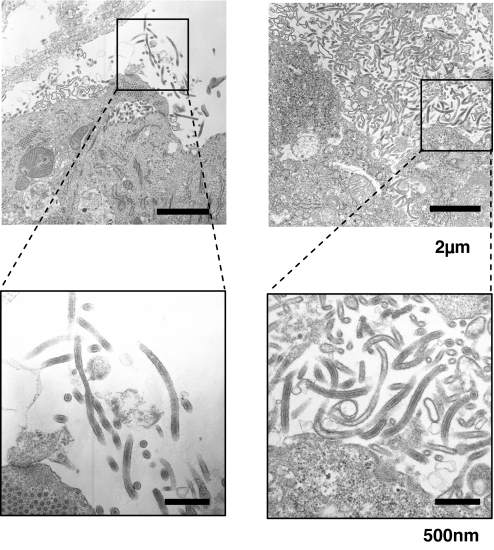
Next we assessed the morphology of EbolaΔVP30-neo virus by transmission electron microscopy (TEM). VeroVP30 cells were infected with EbolaΔVP30-neo virus and fixed 36 h later. Samples were processed for TEM as described (14). As shown in Fig. 4Right, the particles budding from VeroVP30 cells infected with EbolaΔVP30-neo virus were indistinguishable in their size and shape from wild-type EBOVs (Fig. 4 Left). Thus, providing VP30 protein in trans does not have a discernable effect on virion morphology, suggesting that the described system would be suitable for studies of virion formation and budding, for example.
Fig. 4.
Morphology of EBOVs budding from infected cells. Vero cells infected with wild-type EBOV (Left) and VeroVP30 cells infected with EbolaΔVP30-neo virus (Right) were processed for TEM 3 days after infection as described in Materials and Methods. The pictures show virus budding from infected cells. No significant differences in morphology or budding efficiencies were observed for wild-type EBOV and EbolaΔVP30-neo virus. [Magnification: ×6,000 (Upper) and ×20,000 (Lower, boxed area from Upper).]
Taken together, the above results demonstrate that the EbolaΔVP30-neo virus is biologically contained, replicates to high titers in a helper cell line, is genetically stable, and is morphologically indistinguishable from wild-type virions. Having provided proof-of-concept for the generation of biologically contained EBOVs, we next sought to assess the utility of this strategy in basic research and drug screening applications.
Generation of an EbolaΔVP30-eGFP Virus and Its Usefulness for Basic Research Applications.
We first generated an EbolaΔVP30 virus encoding eGFP instead of VP30 (Fig. 1; designated EbolaΔVP30-eGFP) using the same procedures described earlier for EbolaΔVP30-neo virus. Analogous to EbolaΔVP30-neo virus, the eGFP variant replicated efficiently with virus titers reaching 8.0 × 107 focal-forming units per milliliter. Expression of eGFP was observed as early as 10 h after infection (data not shown).
Takada et al. (27) used replication-competent vesicular stomatitis virus pseudotyped with EBOV GP and two neutralizing mAb, 133/3.16 and 226/8.1, to map EBOV GP epitopes and to generate escape mutants. To confirm with authentic EBOV virions the findings of Takada et al. (27) based on a vesicular stomatitis virus-pseudotyping system, we also generated escape mutants by amplifying EbolaΔVP30-eGFP virus in the presence of mAb 133/3.16 or 226/8.1. Each of eight escape mutants to mAb 133/3.16 possessed a histidine-to-arginine substitution at position 549 (H549R) in GP, reported by Takada et al. (27). Using mAb 226/8.1, we isolated 12 escape mutants that all contained an arginine-to-tryptophan substitution at position 134 (R134W), a mutation identical to one identified by Takada et al. (27). We, however, were unable to detect the remaining two escape mutations described by Takada et al. (27). Whether this discrepancy in escape mutants reflects differences between the biological systems used or random mutations is presently unclear. Nonetheless, these experiments illustrated one of the ways that biologically contained EBOVs could be used in basic research applications.
We concluded that biologically contained EBOVs lacking the VP30 gene afford a safe, alternative way to study authentic EBOV, to develop EBOV vaccines, and to screen chemical libraries for compounds that interfere with the EBOV life cycle. Indeed, each of the two different biologically contained viruses we generated (encoding neomycin or eGFP instead of VP30) was biologically contained, as demonstrated by their ability to replicate in VeroVP30 cells but not in wild-type Vero cells. Moreover, virus titers were in the range of 107 focal-forming units per milliliter and hence comparable to those obtained for wild-type EBOV (Fig. 3) (25, 26, 28) whereas morphological, biochemical, and virological analyses indicated that the tested properties of EbolaΔVP30 viruses are indistinguishable from those of wild-type EBOV. These physical properties, together with the results of pilot studies to illustrate the potential of biologically contained EBOVs in basic research and drug screening applications, suggest that this new system will greatly accelerate current filovirus research efforts.
Materials and Methods
Cells and Cell Lines.
Vero cells (green monkey kidney cells) were grown in Eagle's MEM supplemented with 10% FCS, l-glutamine, vitamins, nonessential amino acid solution, and antibiotics. The VeroVP30 cell line was established by cotransfecting Vero cells with pCAG-VP30 (for the expression of VP30) and pPur, a protein expression plasmid for the puromycin resistance gene (Clontech), using the transfection reagent TransIT LT-1 (Mirus). Two days after transfection, puromycin-resistant cells were selected with 5 μg/ml puromycin (Sigma). Individual cell clones were screened for VP30 expression by flow cytometry with a polyclonal peptide antibody to VP30.
Human embryonic kidney 293T cells were grown in high-glucose Dulbecco's modified Eagle's medium containing 10% FCS, l-glutamine, and antibiotics. All cells were maintained at 37°C and 5% CO2.
Flow Cytometry.
Cells were detached in PBS containing 0.02% EDTA and then washed once with cold PBS supplemented with 2% FCS and 0.1% sodium azide (wash buffer). Cells were incubated with a VP30 antibody on ice for 20 min. After washing in buffer, the cells were further incubated with a secondary antibody labeled with fluorescent isothiocyanate (Zymed). They were then washed with buffer and analyzed by FACSCalibur with CellQuest software (Becton Dickinson).
Generation of EbolaΔVP30 Viruses.
The plasmid pTM-T7G-Ebo-Rib, containing the full-length EBOV cDNA flanked by T7 RNA polymerase promoter and ribozyme sequences, is described in a previous publication (26). First, a fragment encompassing nucleotides 6180–10942 (numbers refers to the positive-sense antigenome) was subcloned into a kanamycin-resistant cloning vector. Next, the VP30 ORF was replaced with those encoding neo or eGFP, respectively, by a series of overlapping PCR amplification steps using Pfu Turbo (Stratagene). The altered subgenomic fragments were transferred back into the full-length EBOV cDNA plasmid using two unique restriction sites, SalI and SacI (Fig. 1). The resultant plasmids, designated pTM-EbolaΔVP30-neo or pTM-EbolaΔVP30-eGFP, were sequenced to verify the replacement of the VP30 ORF and the lack of any unwanted mutations.
To artificially generate EBOV, we transfected 5 × 105 293T cells with 1.0 μg of pTM-EbolaΔVP30, 2.0 μg of pCAG-L, 1.0 μg of pCAG-NP, 0.5 μg of pCAG-VP35, 0.5 μg of pCAG-VP30, and 1.0 μg of pCAG-T7 pol using TransIT LT1 (Mirus) in BSL-4 containment (26). Five days after transfection, the supernatant was harvested, cellular debris was removed by low-speed centrifugation, and the virus was amplified in VeroVP30 cells at 37°C and 5% CO2 with propagation medium containing 2% FCS in MEM supplemented with l-glutamine, vitamins, nonessential amino acid solution, and antibiotics without puromycin.
Plaque Assay and Immunostaining Assay.
To determine the titers of wild-type EBOV or EbolaΔVP30 viruses, we absorbed 10-fold dilutions of the viruses to confluent VeroVP30 or wild-type Vero cells for 1 h at 37°C, after which any unbound virus was removed by washing cells with propagation medium. The cells were then overlaid with propagation medium containing 1.5% methyl cellulose (Sigma). Seven days after infection, cells were fixed with 10% buffered formaldehyde, taken out of BSL-4, permeabilized with 0.25% Triton X-100 in PBS for 10 min, and blocked with 4% goat serum and 1% BSA in PBS for 60 min. Cells were then incubated for 60 min with a 1:1,000 dilution of a mouse anti-VP40 mAb, washed with PBS, and incubated for 60 min with a 1:1,000 dilution of an anti-mouse IgG-peroxidase-conjugated secondary antibody (Kirkegaard & Perry Laboratories). After washing with PBS, cells were incubated with 3,3′-diaminobenzidine tetrahydrochloride (Sigma) in PBS. The reaction was stopped by rinsing cells with water.
Western Blotting.
Partially purified virus resuspended in lysis buffer (50 mM Tris·HCl, pH 7.5/150 mM NaCl/0.5% Triton X-100/0.1% SDS) containing protease inhibitors [complete protease inhibitor cocktails (Roche)] was incubated at 100°C for 5 min, taken out of BSL-4, and separated on 4–20% polyacrylamide gels. Resolved proteins were transferred to Western polyvinylidine difluoride membranes (Schleicher & Schuell) and blocked overnight at 4°C with 5% skim milk in PBST [0.05% Tween 20 (Sigma) in PBS]. Blots were incubated with primary antibodies (a mouse anti-NP antibody, a rabbit anti-VP35 antibody, a rabbit anti-VP40 antibody, a mouse anti-GP antibody, a rabbit anti-VP30 antibody, or a mouse anti-VP24 antibody) for 60 min at room temperature, washed three times with PBST, incubated with the appropriate secondary antibody conjugated to horseradish peroxidase (Zymed) for 60 min, and finally washed three times with PBST. Blots were then incubated in Lumi-Light Western blotting substrate (Roche) and exposed to x-ray film (Kodak).
RNA Isolation and RT-PCR.
Cell culture supernatant from virus-infected VeroVP30 cells was inactivated with guanidinium isothiocyanate buffer and taken out of BSL-4. Viral RNA was isolated with the RNeasy Mini kit (Qiagen). RT-PCR was carried out with the RobusT One-Step RT-PCR kit (Finnzyme) using 1 μg of isolated RNA and EBOV-specific primers. The resultant PCR products were cloned into pT7Blue (Novagen) and sequenced.
TEM.
Ultrathin-section electron microscopy was performed as described previously (14). Briefly, at 36 h after infection, VeroVP30 cells infected with EbolaΔVP30-neo virus were fixed and inactivated with 2.5% glutaraldehyde in 0.1 M cacodylate buffer, taken out of BSL-4, and postfixed with 2% osmium tetroxide in the same buffer. Cells were then dehydrated with a series of ethanol gradients followed by propylene oxide before being embedded in Epon 812 Resin mixture (TAAB Laboratories Equipment). Thin sections were stained with 2% uranyl acetate and Raynold's lead and examined under a Hitachi H-7500 electron microscope at 80 kV.
Selection of Escape Mutants.
EbolaΔVP30-eGFP was diluted 10-fold (10−1 to 10−6) and incubated with the indicated mAbs at a concentration of 250–500 μg of mAb per milliliter at 37°C for 60 min. The virus/mAb mixtures were inoculated onto VeroVP30 cells for 60 min. Viruses were amplified for 5 days in the presence of antibodies. Then, viruses that grew in the presence of mAbs (as determined by GFP expression) were harvested at the highest virus-positive dilution and passaged for a total of three to six times in the presence of antibodies. Viral RNA was isolated and RT-PCR-amplified, and the GP sequence was determined by sequence analysis.
ACKNOWLEDGMENTS.
We thank John Gilbert for scientific editing. We acknowledge membership within and support from the Region V “Great Lakes” Regional Center of Excellence (National Institutes of Health Grant 1-U54-AI-057153). This work was also sponsored by grants-in-aid from the Ministry of Education, Culture, Sports, Science, and Technology and the Ministry of Health, Labor, and Welfare of Japan, by the Japan Science and Technology Agency, by National Institute of Allergy and Infectious Diseases Public Health Service research grants, and by financial support from the Public Health Agency of Canada.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
References
- 1.Sanchez A, Geisbert TW, Feldmann H. In: Fields Virology. Knipe DM, Howley PM, Griffin DE, Martin MA, Lamb RA, Roizman B, Straus SE, editors. Philadelphia: Lippincott, Williams & Wilkins; 2007. pp. 1409–1448. [Google Scholar]
- 2.Feldmann H, Geisbert TW, Jahrling PB, Klenk HD, Netesov SV, Peters CJ, Sanchez A, Swanepoel R, Volchkov V. In: Virus Taxonomy: Eighth Report of the International Committee of Taxonomy of Viruses. Fauquet C, Mayo MA, Desselberger U, Ball LA, editors. London: Elsevier; 2004. pp. 645–653. [Google Scholar]
- 3.Boehmann Y, Enterlein S, Randolf A, Muhlberger E. Virology. 2005;332:406–417. doi: 10.1016/j.virol.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Groseth A, Feldmann H, Theriault S, Mehmetoglu G, Flick R. J Virol. 2005;79:4425–4433. doi: 10.1128/JVI.79.7.4425-4433.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muhlberger E, Weik M, Volchkov VE, Klenk HD, Becker S. J Virol. 1999;73:2333–2342. doi: 10.1128/jvi.73.3.2333-2342.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modrof J, Becker S, Muhlberger E. J Virol. 2003;77:3334–3338. doi: 10.1128/JVI.77.5.3334-3338.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Modrof J, Muhlberger E, Klenk HD, Becker S. J Biol Chem. 2002;277:33099–33104. doi: 10.1074/jbc.M203775200. [DOI] [PubMed] [Google Scholar]
- 8.Yonezawa A, Cavrois M, Greene WC. J Virol. 2005;79:918–926. doi: 10.1128/JVI.79.2.918-926.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wool-Lewis RJ, Bates P. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takada A, Robison C, Goto H, Sanchez A, Murti KG, Whitt MA, Kawaoka Y. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marzi A, Wegele A, Pohlmann S. Virology. 2006;352:345–356. doi: 10.1016/j.virol.2006.04.038. [DOI] [PubMed] [Google Scholar]
- 12.Jasenosky LD, Neumann G, Lukashevich I, Kawaoka Y. J Virol. 2001;75:5205–5214. doi: 10.1128/JVI.75.11.5205-5214.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Licata JM, Johnson RF, Han Z, Harty RN. J Virol. 2004;78:7344–7351. doi: 10.1128/JVI.78.14.7344-7351.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noda T, Sagara H, Suzuki E, Takada A, Kida H, Kawaoka Y. J Virol. 2002;76:4855–4865. doi: 10.1128/JVI.76.10.4855-4865.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCarthy SE, Licata JM, Harty RN. J Virol Methods. 2006;137:115–119. doi: 10.1016/j.jviromet.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 16.Johnson RF, Bell P, Harty RN. Virol J. 2006;3:31. doi: 10.1186/1743-422X-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neumann G, Ebihara H, Takada A, Noda T, Kobasa D, Jasenosky LD, Watanabe S, Kim JH, Feldmann H, Kawaoka Y. J Virol. 2005;79:10300–10307. doi: 10.1128/JVI.79.16.10300-10307.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harty RN, Brown ME, Wang G, Huibregtse J, Hayes FP. Proc Natl Acad Sci USA. 2000;97:13871–13876. doi: 10.1073/pnas.250277297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panchal RG, Ruthel G, Kenny TA, Kallstrom GH, Lane D, Badie SS, Li L, Bavari S, Aman MJ. Proc Natl Acad Sci USA. 2003;100:15936–15941. doi: 10.1073/pnas.2533915100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang Y, Xu L, Sun Y, Nabel GJ. Mol Cell. 2002;10:307–316. doi: 10.1016/s1097-2765(02)00588-9. [DOI] [PubMed] [Google Scholar]
- 21.Chan SY, Empig CJ, Welte FJ, Speck RF, Schmaljohn A, Kreisberg JF, Goldsmith MA. Cell. 2001;106:117–126. doi: 10.1016/s0092-8674(01)00418-4. [DOI] [PubMed] [Google Scholar]
- 22.Manicassamy B, Wang J, Jiang H, Rong L. J Virol. 2005;79:4793–4805. doi: 10.1128/JVI.79.8.4793-4805.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimojima M, Takada A, Ebihara H, Neumann G, Fujioka K, Irimura T, Jones S, Feldmann H, Kawaoka Y. J Virol. 2006;80:10109–10116. doi: 10.1128/JVI.01157-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volchkov VE, Volchkova VA, Muhlberger E, Kolesnikova LV, Weik M, Dolnik O, Klenk HD. Science. 2001;291:1965–1969. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- 26.Neumann G, Feldmann H, Watanabe S, Lukashevich I, Kawaoka Y. J Virol. 2002;76:406–410. doi: 10.1128/JVI.76.1.406-410.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takada A, Feldmann H, Stroeher U, Bray M, Watanabe S, Ito H, McGregor M, Kawaoka Y. J Virol. 2003;77:1069–1074. doi: 10.1128/JVI.77.2.1069-1074.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ebihara H, Takada A, Kobasa D, Jones S, Neumann G, Theriault S, Bray M, Feldmann H, Kawaoka Y. PLoS Pathog. 2006;2:e73. doi: 10.1371/journal.ppat.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]