Abstract
Objective To explore whether or not gender predicts consultant activity rates.
Design Using data from the Hospital Episode Statistics for England 2004/2005, we explored inpatient activity rates of male and female hospital consultants, with and without adjustment for case-mix differences. As a sensitivity analysis we also explored outpatient attendances for male and female hospital consultants.
Setting Data from the Hospital Episode Statistics for England.
Main outcome measures Finished consultant episodes per year, with and without adjustment for case-mix differences, age and gender of consultant, contract held, hospital trust, specialty of practice, and clinical excellence awards, discretionary points and distinction awards.
Results Including only consultants on full-time or maximum part-time contracts, men have significantly higher activity rates than women, after accounting for age, specialty and hospital trust.
Conclusions The reasons for the different activity rates of male and female consultatns are unclear, but the implications of these results for the planning of the medical workforce are important.
Introduction
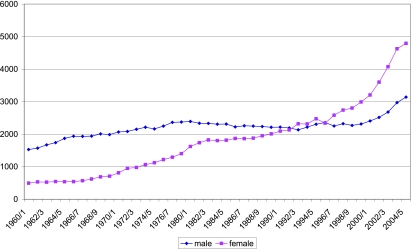
There is a clear trend towards more women doctors in the UK, working in many areas of health care. This has created debate about the likely effect of the ‘feminization’ of the medical workforce, and its implications for medical workforce planning. Figure 11 illustrates the sharply increasing proportion of women medical students in the UK. Surveys of the medical workforce2-4 confirm that women are more likely than men to work part-time, and to take career breaks (as they tend to have children later in life than other women), but also that they may be less likely to take early retirement. The overall life-cycle activity of women doctors will be revealed by ongoing cohort studies over time.
Figure 1.
UK medical school intake by gender (data source: Webster 2005)1
Women in the medical workforce may also have different patterns of work and different rates of activity. Data from Canada5 suggest that there may be differences in the activity rates of male and female physicians at all age groups. Further, a US study6 explored the productivity of male and female physicians in obstetrics and gynaecology, demonstrating small differences in activity rates, with women having slightly fewer inpatient visits per week and hours worked per week, after adjusting for age and other factors.
Earlier analysis7 has confirmed the feasibility of using NHS Hospital Episode Statistics (HES) linked with information from the medical workforce census to explore the activity rates of hospital consultants, and associations with the characteristics of consultants and their practice. These routinely collected sources of data are used here with the aim of exploring variation in activity rates of hospital consultants by their gender.
Data and methods
Data sources
HES data for England8 in 2004/05 were analysed. Each observation in the extract from HES represents one finished consultant episode (FCE), defined as a period of health care under one consultant in a hospital provider. Ten surgical and medical specialties were included (general surgery, urology, trauma and orthopaedics, ear nose and throat, ophthalmology, general medicine, gastroenterology, cardiology, paediatric medicine and geriatric medicine). The choice of specialties was made to cover a broad range of surgical and medical activity, and to include most common reasons for admission. HES data record anonymized patient characteristics, including age, sex, diagnoses, procedures and length of stay. From these data, Healthcare Resource Groups (HRGs) are assigned to each patient episode, grouping conditions and procedures that use similar levels of resource. Each HRG has an associated tariff cost, which is used as a proxy for case-mix differences.
HES data also provide information about hospital providers and a code for the consultant in charge of each episode. This consultant identifier, based on the General Medical Council (GMC) registration code, permits linking of HES episodes with other routinely collected datasets, including the Medical Workforce Census9 and the Clinical Excellence Awards database.10 These data provide information on the characteristics of consultants, including age, gender, type of contract held, and possession of clinical excellence awards, discretionary points and distinction awards.
For each consultant, after linking the datasets, the following information was available: FCEs per year, with and without adjustment for case-mix differences (proxied by tariff costs of each HRG), age of consultant, gender of consultant, contract held (full time, maximum part-time, part-time or honorary), hospital trust (if consultant worked in more than one trust, their main trust was assumed the one where they undertook the most FCEs), specialty of practice (again, if the consultant worked in more than one specialty, their main specialty was assumed to be the one where they undertook the most FCEs), and clinical excellence awards, discretionary points and distinction awards.
During the relevant data year (2004/05), consultant contracts had been renegotiated, but the medical workforce census (taken on 30 September 2004) retained information about whether consultants were previously on full-time, maximum part-time (a contract enabling private practice, but where the consultant was expected to devote substantially the whole of their time to the NHS), part-time or honorary contracts. In addition, this period represents a transition from earlier bonus payment systems (discretionary points and distinction awards) to a revised system of clinical excellence awards. Only consultants who were on full-time or maximum part-time contracts were included in the analysis. In the first model, contract and bonus payments were not included, but in a second model, contract status and possession of discretionary points and distinction awards or the equivalent (locally or nationally awarded) clinical excellence awards were included.
Statistical methods
To explore whether or not gender predicts consultant activity rates, it is necessary to isolate the effect of gender from other factors, such as the influence of age, specialty and hospital trust. Women consultants are, on average, younger than men, as the shift towards more women doctors has been relatively recent, and the proportion of women in the medical workforce is increasing over time. There is an established difference in working patterns and workloads of different cohorts of doctors,11 so age is a potential confounder. Women also choose different hospital specialties than men - some specialties (e.g. trauma and orthopaedics, urology) remain male-dominated. It may be that women choose to work in different hospitals (e.g. they may be more or less likely to work in teaching hospitals). These factors need to be included in a model exploring activity. The model is complicated by the fact that consultants, with their individual characteristics, are nested within a specialty grouping and within a hospital trust. This means that there is a need to use statistical techniques that can simultaneously handle measurements made at different levels of a hierarchy, retaining all the available information while carrying out analysis at each level. A mixed generalized linear model12 was used to estimate the effect of consultant gender on consultant activity rates, after accounting for other factors, specifically consultant age (included as a restricted cubic spline with five knots), specialty of practice (included as fixed effects) and trust (included as random effects). Previous work has suggested that contract (maximum part-time or full-time) and bonus payments (discretionary points and distinction awards) predict activity rates,7 and therefore these were included in a further model. All the models included only consultants on full-time or maximum part-time contracts, part time and honorary contract holders were excluded. All analyses were conducted using ‘PROC MIXED’ in SAS version 9.1.13
Sensitivity analysis
As FCEs are a partial measure of the overall activity of consultants, we conducted sensitivity analysis using outpatient attendances per consultant, both first and total attendances, as the dependent variable. This measure was derived from HES outpatient data, and as 2004/05 is only the second data year available, its validity is not perfect, but it provides an additional analysis to explore whether outpatient activity rates can be predicted by gender.
We conducted two additional sensitivity analyses related to the possible influence of maternity leave. Firstly, we noted for each consultant (male and female) any months where there is no NHS activity. Absent months could reflect holidays, sickness or maternity leave, so in a sensitivity analysis we excluded all consultants where one or more months showed as absent. As an alternative we inflated activity to a whole year equivalent.
Results
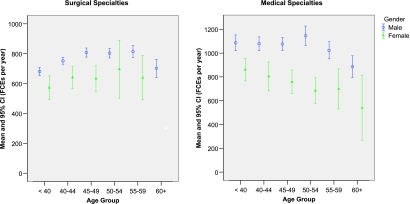
Table 1 shows the characteristics of this sample of consultants. Using consultant-level HES for England, including only full-time and maximum part-time consultants, women undertake fewer FCEs per year than men at all age groups (Figure 2). Table 2 shows the results of the mixed model estimating the effects of gender on activity rates (without and with adjustment for case-mix), after accounting for age, specialty choice and hospital trust.
Table 1.
Characteristics of consultants in this sample
| Male | Female | |
|---|---|---|
| Number of consultants in each specialty | ||
| General surgery | 1273 | 82 |
| Urology | 441 | 14 |
| Trauma and orthopaedics | 1276 | 33 |
| ENT | 387 | 23 |
| Ophthalmology | 490 | 83 |
| General medicine | 1625 | 244 |
| Gastroenterology | 179 | 22 |
| Cardiology | 346 | 34 |
| Paediatric medicine | 823 | 412 |
| Geriatric medicine | 396 | 101 |
| Number of consultants with each contract | ||
| Full time | 5271 | 967 |
| Maximum part-time | 1965 | 81 |
| Number of consultants with awards | ||
| Discretionary points or local CEAs | 3169 | 355 |
| Distinction awards or national CEAs | 817 | 74 |
| Mean (SD) age | 47 (7) | 44 (7) |
| Mean (SD) activity rate: FCEs per year | 909 (662) | 744 (670) |
| Mean (SD) activity rate: casemix-adjusted activity per year1 | 1571 (1114) | 1210 (1225) |
| Mean (SD) first outpatient attendances per year | 845 (736) | 517 (571) |
| Mean (SD) total outpatient attendances per year | 2792 (2216) | 1863 (1972) |
Note:
Casemix-adjusted activity is estimated by summing the tariff cost of the healthcare related group (HRG) that is assigned to each episode
Figure 2.
Consultant activity rate by age and gender: surgical specialties (general surgery, urology, trauma and orthopaedics, ENT and ophthalmology) and medical specialties (general medicine, gastroenterology, cardiology, paediatric medicine and geriatric medicine). (Consultants on full-time or maximum part-time contracts only.)
Table 2.
Effect of gender on activity rates - accounting for confounding variables
| Effect | Estimate | 95% confidence interval | P value |
|---|---|---|---|
| Model 1: Finished consultant episodes | |||
| Sample:1 6451 male and 886 female | |||
| Gender effect (additional activity by men) | 160 | 116 to 204 | <0.0001 |
| Model 2: Casemix adjusted activity (£000)2 | |||
| Sample: 6448 male and 884 female | |||
| Gender effect (additional activity by men) | 214 | 147 to 280 | <0.0001 |
| Model 3: FCEs including contract and bonus payments as predictors | |||
| Sample: 6451 male and 886 female | |||
| Gender effect (additional activity by men) | 153 | 109 to 197 | <0.0001 |
| Contract effect (additional activity by maximum part-time contract holders) | 75 | 39 to 112 | <0.0001 |
| Effect of discretionary point or local CEA | 48 | 17 to 79 | 0.003 |
| Effect of distinction award or national CEA | −6 | −53 to 39 | 0.8 |
| Model 4: Casemix adjusted activity (£000) including contract and bonus payments as predictors | |||
| Sample: 6448 male and 884 female | |||
| Gender effect (additional activity by men) | 204 | 138 to 271 | <0.0001 |
| Contract effect (additional activity by maximum part-time contract holders) | 97 | 42 to 153 | 0.0006 |
| Effect of discretionary point or local CEA | 67 | 19 to 113 | 0.005 |
| Effect of distinction award or national CEA | −17 | −87 to 53 | 0.6 |
Notes:
Sample sizes differ due to linking of datasets and some missing variables
Casemix-adjusted activity is estimated by summing the tariff cost of the healthcare related group (HRG) that is assigned to each episode
Men have higher activity rates than women, after accounting for age, specialty and hospital trust. Men have, on average, activity rates of 160 FCEs per year more than women (95% confidence interval 116-204, P<0.0001 [Table 2 model 1]). This is approximately a 20% difference in FCEs per year, despite including only consultants on full-time or maximum part-time contracts. Model 2 in Table 2 reports FCEs after adjusting for case-mix, and the gender difference remains highly statistically significant.
Including contract and possession of discretionary points and distinction awards (models 3 and 4) changes the gender difference very little, but it is also useful to note that those on a maximum part-time contract undertake more FCEs per year than those on a full-time contract (a difference of 75 FCEs per year, 95% CI 39-112, P<0.0001), and those holding any discretionary point or locally allocated clinical excellence award undertake 48 FCEs more per year (95% CI 17-79, P=0.003) than those without. There was no statistically significant difference between those with a distinction award or national clinical excellence award and those without. These additional results confirm earlier analysis on this subject, where in surgical specialties maximum part-time contract holders and those with a discretionary point were found to have higher inpatient activity rates.7
Sensitivity analysis
Sensitivity analyses were conducted using first and total outpatient attendances as the dependent variable, and then using only those consultants where all months had some NHS activity. The results of these further analyses are illustrated in Table 3. For both first and total outpatient attendances (models 5 and 6), we found that women consultants see fewer outpatients, and this is a highly statistically significant finding. Women did have more months without any FCEs (around 92% of men and 77% of women had some episodes in all twelve months, which could reflect maternity leave and/or child care and other responsibilities), but adjusting activity rates to a ‘whole year equivalent’ made no material change to the results. Restricting the sample of consultants to only those with some NHS activity in all months (models 7-10) did not change any of the main findings: women still appear to have lower inpatient and outpatient activity rates, and the results remain highly statistically significant.
Table 3.
Sensitivity analyses
| Effect | Estimate | 95% confidence interval | P value |
|---|---|---|---|
| Model 5: First outpatient attendances | |||
| Sample:1 6298 male and 847 female | |||
| Gender effect (additional activity by men) | 88 | 46 to 129 | <0.0001 |
| Model 6: Total outpatient attendances | |||
| Sample: 6326 male and 858 female | |||
| Gender effect (additional activity by men) | 270 | 149 to 390 | <0.0001 |
| Model 7: FCEs including only subjects with activity in all months2 | |||
| Sample: 6128 male and 741 female | |||
| Gender effect (additional activity by men) | 105 | 58 to 152 | <0.0001 |
| Model 8: Casemix adjusted activity (£000)3including only subjects with activity in all months | |||
| Sample: 6128 male and 741 female | |||
| Gender effect (additional activity by men) | 148 | 782 to 2172 | <0.0001 |
| Model 9: First outpatient attendances including only subjects with activity in all months | |||
| Sample: 6067 male and 723 female | |||
| Gender effect (additional activity by men) | 81 | 37 to 123 | 0.0002 |
| Model 10: Total outpatient attendances including only subjects with activity in all months | |||
| Sample: 6084 male and 730 female | |||
| Gender effect (additional activity by men) | 252 | 127 to 377 | <0.0001 |
Notes:
Sample sizes differ due to linking of datasets and some missing variables
Consultants are excluded from the analysis if they have any months with no NHS activity (FCEs), as this may reflect illness or maternity leave
Casemix-adjusted activity is estimated by summing the tariff cost of the healthcare related group (HRG) that is assigned to each episode
Discussion and Conclusions
The difference in activity rates between men and women is noticeable, statistically highly significant and robust. Similar results have been found in Canada5 and the US,6 but these are systems where doctors are paid primarily by fees-for-service, so lower activity rates represent an individual choice, and presumably a trade-off between income and other activities. In England, where doctors are paid a salary, and when we have included only those on full-time and maximum part-time contracts, the obvious question is why such a difference may exist?
The first possible explanation, as always in secondary analysis, is the potential for bias created by problems in the data. HES data have improved substantially in recent years, but nevertheless the accuracy, comprehensiveness and validity of HES have been questioned, particularly in terms of its use to monitor consultant performance.14 In relation to this analysis, a number of limitations may be relevant. Firstly, there may be inaccuracies in allocating activity to individual consultants. For example, when consultants work in teams, coders may have a tendency to allocate the work to the most senior consultant in preference to a newly arrived member of staff, and if patients are referred to one consultant then transferred to a more junior colleague, this may not be recorded. As the number of female consultants is still increasing slowly over time, this could in principle create a bias underestimating the workload of women. In addition, the specialty code in HES is crude - it may be that women work in different subspecialties (e.g. breast surgery), which could differ in case-mix. However, in exploring the data on length of stay, no significant difference was found in mean length of stay or mean length of episode between patients treated by male and female consultants, which does not support the hypothesis that women treat more complex patients in different subspecialties.
Beyond these data issues, we can only really speculate on possible reasons for the difference, and this is clearly a subject for further research. It is important to note that the activity included in these analyses (inpatient and outpatient) represent only part of a consultant's overall workload, and other activities, for example teaching and administration, are not reflected here. We have no information on the number or content of programmed activities chosen under the new contract, and workload choices may be different. Women consultants, perhaps particularly in specialties where they are under-represented, may have more administrative and management roles - for example work for Royal Colleges and other bodies. They may perhaps have different sized teams of more junior doctors or nurses. Differences in team sizes between hospital specialty groupings are included in this model by the inclusion of hospital and specialty as random and fixed effects, but it is not possible to account for differences in team sizes between individual consultants within hospital specialty groups, as this data is not collected centrally.
The result could reflect women taking more time with each patient, having different communication styles and perhaps being more meticulous, comprehensive and holistic in their care. This may or may not translate into better diagnoses, patient satisfaction and/or health outcomes as a result of lower overall activity - this study has no information on the effect of gender on patient outcomes, and general evidence about whether women practice medicine differently is conflicting.15 On the other hand, the difference could result from women being less likely to work substantially out of normal working hours due to family and other commitments. These and other possible explanations are potentially interesting areas for future research.
This analysis illustrates the feasibility and potential usefulness of linking routinely collected data to explore productivity and performance in the health care system, and there are many other research opportunities that could arise from this approach, including exploring further variations in consultant activity, variations between Trusts and trends over time.
The implications of these results for the planning of the medical workforce are evidently important, as feminization of the profession could lead to reduced productivity over time. The recent increase in medical school intake,1 with the substantially increased proportion of female students, could in principle create less of an increase in NHS activity than policy makers intended from this investment, unless these new women doctors are enabled to deliver greater NHS activity. The existence and the causes of gender differences in consultant activity are fundamental issues for researchers and NHS policy makers.
DECLARATIONS
Competing interests AM is chair of York NHS Hospitals Trust
Funding This paper arises from a programme of work funded by the Department of Health's Policy Research Programme which has explored variation in activity rates of English hospital consultants
Ethical approval Not applicable
Guarantor KB
Contributorship KB formulated the research question, conducted initial data organization and analyses and produced the first draft of the paper; NF conducted the mixed model in consultation with the other authors; AM contributed to research design and policy interpretation. All authors have been involved inproducing the final draft of the paper.
Acknowledgements Sources of information include Hospital Episode Statistics for England, and the Department of Health's Medical Workforce Census. The authors have benefited from useful contributions from and discussions with a number of colleagues including: Professor Nicky Cullum, Dr Giles Croft, Vivien Hendry, Dr Lisa Munro-Davies, Dr Sarah Purdy, Professor Debbie Sharp and Professor John Williams. Opinions expressed are those of the authors alone. We are indebted to Anne Burton for administrative assistance.
References
- 1.Webster R, Mellor D, Spavin B. Who are the doctors of tomorrow and what will they do?. Paper for the 9th conference of the International Medical Workforce Collaborative, Melbourne, November 2005. See http://www.health.nsw.gov.au/amwac/amwac/pdf/9_tomdocs_uk.pdf
- 2.Lambert TW, Goldacre MJ. Career destinations seven years on among doctors who qualified in the United Kingdom in 1988: a postal questionnaire survey. BMJ 1998;317: 1419-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davidson JM, Lambert TW, Goldacre MJ. Career pathways and destinations 18 years on among doctors who qualified in the United Kingdom in 1977: postal questionnaire survey. BMJ 1998;317: 1425-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldacre MJ, Lambert TW, Davidson JM. Loss of British-trained doctors from the medical workforce in Great Britain. Med Educ 2001;35: 337-44 [DOI] [PubMed] [Google Scholar]
- 5.Canadian Institute for Health Information. Canada's health care providers. Ontario: CIHI, 2005
- 6.Benedetti TJ, Baldwin L-M, Andrilla CHA, Hart LG. The productivity of Washington State's obstetrician-gynecologist workforce: does gender make a difference?. Obstet Gynecol 2004;103: 499-505 [DOI] [PubMed] [Google Scholar]
- 7.Bloor K, Maynard A, Freemantle N. Variation in activity rates of consultant surgeons and the influence of reward structures in the English NHS. J Health Serv Res Policy 2004;9: 76-84 [DOI] [PubMed] [Google Scholar]
- 8.NHS Information Centre. Hospital Episode Statistics for England, 2004/5. London: DoH, 2006
- 9.Department of Health. Medical Workforce Census, 30 September 2004. London: DoH, 2005
- 10.Advisory Committee on Clinical Excellence Awards. Clinical Excellence Awards Database 2004/5. London: DoH, 2005
- 11.Watson DE, Slade S, Buske L, Tepper J. Intergenerational differences in workloads among primary care physicians: a ten-year, population-based study. Health Affairs 2006;Nov–Dec: 1620-8 [DOI] [PubMed]
- 12.Goldstein H. Multilevel statistical models. 2. London: Arnold, 1995
- 13.SAS Institute Inc. SAS system version 9.1. Cary, NC: SAS Institute, 2006
- 14.Williams JG, Mann RY. Hospital Episode Statistics: time for clinicians to get involved?. J R Coll Phys 2002;2: 34-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kilminster S, Downes J, Gough B, Murdoch-Eaton D, Roberts T. Women in medicine - is there a problem? A literature review of the changing gender composition, structures and occupational cultures in medicine. Med Educ 2007;41: 39-49 [DOI] [PubMed] [Google Scholar]