Abstract
The term “idiom of distress” is used to describe culturally-specific experiences of suffering. Most of these studies have been conducted with small groups, making comparison of symptom profiles difficult. Female undergraduate and graduate students in Japan (N=50) and Korea (N=61) completed Beck Depression Inventory (BDI) and seven-day dairy reports of their experiences of 46 somatic symptoms. Between-culture comparisons revealed that BDI scores did not differ; however, Korean women had significantly higher somatic distress means than the Japanese women. Despite the higher Korean distress mean, regression analysis showed that somatic distress explained 30% of the variance of BDI score for the Japanese, but only 22% of the variance for the Koreans. Within-culture comparisons showed that both the High BDI Japanese and Koreans had 19 somatic distress symptoms with significantly higher means than their Low BDI counterparts; eleven somatic symptoms were shared by the two groups. Multidimensional Scaling matrices were used to compare symptom proximities and revealed cultural differences. The problems with using broad racial categories in clinical research, the clinical significance of these findings, and implications for psychiatric nursing assessment and practice are discussed.
Keywords: Japanese culture, Korean culture, Somatization, Emotional Depression, Experience Sampling Method, Cross-cultural comparison
Healthcare practitioners and researchers interested in the cultural varieties of mental illness often encounter the phrase “idioms of distress.” This concept has been used in medical anthropology and transcultural psychiatry to describe the culturally-specific experiences of psychosocial and physical suffering. There have been a significant number of clinical studies in both psychiatry and primary care reporting that Asians with psychological distress or depression exhibit more somatic distress complaints than Caucasians (Gureje, Simon, Ustin and Goldberg, 1997; Lee, 1997; Lin et al., 1992; Okazaki, 2000; Pang, 1998; Park & Hinton, 2002; Ware & Kleinman, 1992; Waza, Graham, Zyzanski and Inoue, 1999). Studies such as these have assumed that people from various cultures with the broad Asian culture region share idioms of distress. Indeed, there are no published studies which have systematically compared this phenomenon between Asian subpopulations.
Idioms of distress should not be confused with mental illness. While the distress experiences seen in diverse cultural groups sometimes signify the presence of physical or psychological disorders, they may also symbolically represent interpersonal and intrapsychic conflicts, or may be culturally coded ways of expressing social discontent (Kirmayer et al., 1998; Kirmayer & Groleau, 2001; Kleinman, 1995; Nichter, 1981; Parsons & Wakeley, 1991). This study represents an example of one research strategy that can move from small-group data, to larger group survey samples, while also embracing the possibility that there may be cultural differences between groups. Systematic comparison across larger groups will allow us to recognize patterns, and begin to disentangle the possible clinical significance of idioms of distress. This present study examines the relationship among cultural group, depression symptoms and somatic symptoms for women in two countries within the broad “Asian” racial category. Specifically, we explore the nature of the similarities and differences among the somatic symptoms that co-occur with high BDI using the Experience Sampling Method (Schwartz & Stone, 1998; Shiffman & Stone, 1998; Stone et al., 1998; Stone, Shiffman, & DeVries, 1999) to compare the somatic distress symptoms experienced by university women living in two Asian countries, Japan and Korea.
Background
The sources of the diversities of idioms of distress are varied cultural models. Cultural models are group-level templates that influence individual-level perceptions, beliefs, values, and behavioral practices. Cultural models direct individual cognition toward culturally relevant internal bodily experiences, as well as toward what those sensations mean about oneself as a member of a society (Holland & Quinn, 1987; Moscovici, 1988; Saint Arnault, in press). We believe that cognitive attention patterns, whether they are the initial perceptions of physical or emotional sensations, or later interpretations of the meanings of them, are formed developmentally as part of enculturation. As early as infancy, the prevailing cultural model “tells” the person which physical and emotional sensations, changes, and experiences should be acknowledged and articulated. In this way, cultural models shape how much attention one pays to one's constantly fluctuating physical sensations (Saint Arnault, in press).
The body is an important symbolic and experiential component in distress and suffering. While we know that complaints of physical symptoms can be seen in depressed patients from all cultural groups, the percentage of patients in international clinics that report unexplained physical symptoms ranges from 45% to 95%, with an average across all groups of 69% (Simon, VonKoroff, Piccinelli, Fullerton & Ormel, 1999). Unfortunately, most of the literature on distress and depression in Asians was conducted in the 1980's and 1990's. However, these classic works are revealing. Ethnographic and clinical studies of depression in diverse Asian groups have revealed a tendency to experience negative, depression-like emotions as symbolic and holistically interrelated with somatic sensations and interpersonal disharmony, suggesting an inclination to endorse a variety of somatic distress symptoms (Gureje et al., 1997; Hinton & Hinton, 2002; Hong et al., 1995; Iwata & Roberts, 1996; Kanno, 1981; Kawanishi, 1992; Maeno et al., 2002; Parsons & Wakeley, 1991; Simon et al., 1999). An example of this holism can be seen in an examination of interactions between Chinese physicians and their patients (Ots, 1990). Ots found that both physicians and patients related internal organs with emotions, and both groups carefully examined bodily perceptions when discussing emotions. In his sample, the liver was seen as the cause of headaches, epigastric pain, hypertension and anger, while the heart was related to anxiety, uncertainty and fear.
Koreans are reported to have high prevalence rates of depression-like symptomology in both Korea and in Korean immigrants in the US, with rates as high as 27% of women in some samples (Cho, Nam and Suh, 1998; Kuo, 1984; US Department of Health and Human Services, 2001). Ethnographic studies of highly distressed Koreans have identified several syndromes that resemble depression. These include Han (a form of regret or resentment syndrome), Hwa-byung (an anger syndrome), and Shingyungshayak (similar to the Chinese diagnosis of neurasthenia)(Kleinman, 1982). Han has been described as a passive, chronic regret and resentment syndrome, and includes the sensation of an obstruction by a lump in the epigastric and respiratory regions. Han also includes expressions of dysphoric affect, such as self pity, commonly associated with disappointments and unfulfilled aspirations. Shingyungshayak is an emotional, psychic, and bodily disorder characterized by fatigue, depression, feelings of inadequacy, headaches, hypersensitivity to sensory stimulation, and psychosomatic symptoms such as digestive disturbances and insomnia (Pang, 1998).
Hwa-Byung is the most widely-studied Korean depressive-like bodily disorder. It is sometimes described as an anger syndrome that encompasses elements of depression, resentment, somatic illness, and neurotic symptoms (Lin, 1983; Lin et al., 1992; Pang, 1998, 2000). Symptoms include active anger and resentment, insomnia, fatigue, panic, feeling of impending death, dysphoric affect, indigestion, anorexia, dyspnea, palpitations, generalized aches and pains, and feeling of a mass in the epigastrium (APA, 1994). In Chinese medical terms, Hwa-Byung is defined as a neurotic fire or anger syndrome that develops due to repression of emotions in reaction to suffering extreme injustice (Park, Kim HS, Kang and Kim J-W, 2001).
Very few studies have examined the specific array of somatic symptoms in depressive-like disorders in Koreans or Korean Americans. One such study examined the incidence of Hwa-Byung in a community-based urban sample of 2,807 women ages 41 to 65 years. They used a 60-item questionnaire to measure the prevalence of the six dimensions of this condition (quick-temper; personality characteristics such as perseveration and self-criticism; familial problems; emotional problems; physical symptoms localized on the upper part of body; and physical symptoms related to sensation of heat). The survey revealed that 4.95% (N = 139) of the women surveyed endorsed symptoms consistent with the condition (Park, Kim HS, Kang and Kim J-W, 2001). In another study, Kim (2002) developed a 25-item Depression tool that included a somatic scale with items representing Korean cultural idioms of distress, such as “heavy chest,” “mind pain” and back pain. While the author of this scale believes that the somatic subscale still needs refinement, this is an important attempt to capture the manifestations of depression among Korean Americans.
Japanese depression has been studied in a number of clinical studies as well (Kawanishi, 1992; Lock, 1987; Maeno, Kizawa, Ueno, Nakata & Sato, 2002; Mino, Aoyama, & Froom, 1994; Nakao, Yamanaka, & Kuboki, 2002; Okazaki, 1994; Takauchi, Kuo, Kim, & Leaf, 1989; Waza et al., 1999). One study examining the symptoms of depressed Japanese found that physical symptoms co-occurred with depression in 13-15% of patients (Maeno et al., 2002; Mino et al., 1994). Physical symptoms most often cited for Japanese samples include neck and shoulder pain, headache and stomach distress (Mino et al., 1994; Waza et al., 1999). Lock interviewed physicians and middle-class female patients in Japan to document and explain these futeishūso (non-specific physical complaints). Futeishūso includes symptoms such as coldness, shoulder pain, palpitations and nervousness. In her study, both the physicians and patients related these symptoms with social discontent, problems with the autonomic nervous system, pelvic inflammatory disease, and a general personality sensitivity (Lock, 1987).
Very few studies have compared somatic distress symptoms using large samples of Americans and Asian samples. However, Saint Arnault, Sakamoto and Moriwaki compared the relationship between somatic and depressive symptoms for 50 Japanese and 44 American women. Japanese had higher Somatic Distress Means (SDM) than Americans. ANOVA of SDM by BDI level revealed that the High BDI Japanese had significantly higher means than their Low BDI counterparts for 26 somatic symptoms (including stomachache, dizziness, and shoulder pain). High BDI Americans had significantly higher mean for joint pain compared to the Low BDI group (Saint Arnault, Sakamoto & Moriwaki, 2006).
Taken together, these studies demonstrate the important interconnection between physical and emotional distress for some Asian groups, and that this relationship may be different for Asians and Americans. These clinical and ethnographic studies also suggest that the somatic distress symptoms included in western instruments (sleep, appetite and lethargy) may not be sufficient to capture the somatic distresses experienced by people in Asian samples. In addition, casting a net as wide as Asia may also be inappropriate. Asian countries have sometimes been referred to as a culture region because they share Confucian and Buddhist religious traditions (Milner & Johnson, 1997). However, Asian peoples represent extreme diversity in life-ways and illness beliefs and practices. The above review provides preliminary evidence that the idioms of distress for Japanese and Korean women may share some somatic symptoms such as abdominal distress, but may also differ in other significant ways. The research presented here seeks to further illuminate these similarities and differences.
Method
Design and Sample
This research is part of a larger study examining the relationships among culture, the self, distress and depression. This present research used the Experience Sampling Method (Schwartz & Stone, 1998; Shiffman & Stone, 1998; Stone et al., 1998; Stone, Shiffman, & DeVries, 1999) to examine the somatic distress symptoms for a convenience sample of 50 Japanese and 61 Korean female college students. The women reported their distress experiences as ratings along a six-point rating scale once each day for seven days.
A convenience sample of volunteer Junior and senior undergraduates and graduate students attending classes in Psychology (Tokyo, Japan) and Nursing (Seoul, Korea) were invited to participate in the study. The mean ages of the women in these samples were different, with the Korean women having a statistically higher mean age (Japanese sample M = 19.2 years, SD =. 53; Korean sample M=26.5 years, SD=5.1 (df=2, F=68.12, p=.00). Most of the women in both samples were single; however eight of the Korean women were married. Six of the Korean women had children. Because our advisors in Japan and Korea cautioned us that asking questions about income and education is considered offensive, that information is not available.
Procedure
This study was conducted with IRB approval. Women were asked to volunteer by trained research staff, and given research instructions orally and in writing. The women were informed that they could withdraw from the study at any time, and that only code numbers identified them. Participation was consent. Completed diaries were returned to a designated location in sealed envelopes. Women were given a packet of diaries, and instructed to complete the diaries once a day for seven consecutive days. They were instructed to complete the diary at the end of the day to reflect on their experiences of the previous 24 hours. All procedural instructions and research instruments were in the participant's native language. All symptoms were translated into Japanese and Korean, translated back into English and reviewed by expert Japanese and Korean researchers for accuracy, natural usage and conceptual equivalence before data was gathered (Werner & Campbell, 1971).
Measures
Depressive symptomology
We measured the current depressive symptomology with the Beck Depression Inventory (BDI)(Beck et al., 1988). The BDI is a depression screen that consists of 21 items designed to measure depressive symptomology level. Participants rate each item on a 0-3 point scale, and scores are summed across all items. For American samples, summed scores over nine indicate mild depression. The BDI has been shown to have acceptable reliability in a variety of culturally diverse samples, with reliability coefficients ranging from .77 to .89 (Abdel-Khalek, 1998; Barrera & Garrison-Jones, 1988; Beck, Steer & Garbin, 1988; Bonicatto, Dew & Soria, 1998; Kojima, Furukawa, Takahashi, Kawai & Tokudome, 2002; Shek, 1990; Yeung, et al., 2002). In our study, reliability of the BDI was .79 for the Japanese and .94 for the Koreans.
Somatic Symptomology
We measured physical symptoms with a modified version of the Pennebaker Inventory of Limbic Languidness (PILL). The PILL is a 54-item scale that taps the intensity of occurrence of a group of common physical symptoms and sensations (Pennebaker, 1982). Two-month test-retest reliabilities for the PILL ranged from .79 to .83. For the purposes of this study, participants were asked to rate the amount that each Somatic Distress Symptom (SDS) bothered them on a scale from “1” indicating “slightly or not at all” to “6” indicating that the item was “very bothersome.” We modified the items for use with Asian samples derived from review of literature and preliminary studies. We also remove, revised or collapsed items for accurate, natural and relevant translation; added depression-specific items (no appetite, sleepy, fatigued, tiredness); and added items specific to depression-like syndromes in people from some Asian cultures (abdominal cramps, dizziness, lightheadedness, pain in joints, pain in shoulders, weakness, palpitations). This resulted in an instrument with final instrument of 46 items.
Analysis
For analysis in this study, we aggregated the daily scores for the 46 Somatic Distress Symptoms (SDS) across the seven days to obtain mean scores for each item for each woman. In addition, we calculated a mean somatic distress score for each cultural group. We also divided the BDI depressive symptomology scores into three groups (0-8, 9-14, and 15 or higher). ANOVA comparison of means are reported here for somatic symptom mean differences between the 0-8 (the Low BDI group), and 15 or higher (the High BDI group). To further understand symptom experience by culture. Multidimensional Scaling was then used for the 27 SDS symptoms for which High BDI groups of either cultural group had higher means.
Findings
Distress Level
ANOVA comparisons of mean BDI scores revealed that there was no statistically significant difference between the BDI scores for the Japanese and the Koreans. The BDI depressive symptomology scores for the Japanese sample ranged from zero to 28 (M=11.82, SD=6.68); for the Korean sample, BDI scores ranged from one to 33(M =14.0, SD=6.61). Despite the age differences between the samples, there were no significant correlations between BDI scores and the age of respondents for either cultural group.
Somatic Symptoms
There was a significant positive correlation between somatic mean score and BDI score for both the Japanese (N=50, r=.57, p=.00) and the Korean women (N=61, r=.47. p=.00). T tests revealed that the Koreans had significantly higher SDS means than the Japanese (Japanese M =1.34, SD= .40; Korean M=1.57, SD=.45) (df = 2, F = 1.89, p = .00). However, there was no significant correlation between age and somatic distress mean for the women in either group. Regression analysis revealed that the somatic means for the Japanese group predicted 30% of the variation of the BDI scores; while for Koreans, somatic means predicted 22% of the variance of the BDI mean.
Within-sample ANOVA for the Japanese by BDI group revealed that the High BDI group (N=14) had 19 symptoms that had significantly higher means when compared with the Low BDI group (N=16). The symptoms and means are displayed in Table 1, and include six abdominal-digestive symptoms (heartburn, no appetite, indigestion, abdominal cramps, abdominal pain, stomachache); nine neurological symptoms (lightheadedness, numbness, weakness, dizziness, faintness, hot flashes, chills, cold hands and feet, headache); three musculoskeletal symptoms (pain in the joints, stiff joints, pain in the shoulders); and one cardiac symptom (palpitations).
Table 1.
Somatic symptoms by culture*
| Japanese | Korean | |||
|---|---|---|---|---|
| Somatic symptom | Low BDI | High BDI | Low BDI | High BDI |
| N=16 | N=14 | N=12 | N=24 | |
| constipation | --- | --- | 1.2 (.30) | 2.2 (1.13) |
| heartburn | 1.0 (.03) | 1.6 (.92) | 1.5 (.63) | 2.6 (1.07) |
| no appetite | 1.1 (.23) | 1.6 (.94) | 1.5 (.64) | 2.3 (.85) |
| indigestion | 1.1 (.13) | 1.5 (.65) | 1.3 (.38) | 2.4 (1.06) |
| abdominal cramps | 1.0 (.00) | 1.4 (.66) | 1.0 (.12) | 1.5 (.60) |
| abdominal pain | 1.1 (.21) | 1.3 (.40) | --- | --- |
| stomachache | 1.2 (.50) | 2.0 (1.20) | --- | --- |
| fatigue | --- | --- | 2.0 (.89) | 3.0 (1.02) |
| tired | --- | --- | 2.0 (1.03) | 3.2 (1.01) |
| numbness | 1.0 (.03) | 1.3 (.57) | 1.2 (.40) | 1.8 (.91) |
| weakness | 1.1 (.29) | 1.8 (1.20) | 1.3 (.56) | 2.0 (.84) |
| dizziness | 1.1 (.19) | 1.7 (1.01) | 1.3 (.36) | 1.9 (.80) |
| faintness | 1.1(.29) | 1.9 (1.32) | 1.2 (.32) | 2.0 (.89) |
| hot flashes | 1.1 (.19) | 1.6 (.65) | 1.4 (.56) | 2.1 (1.00) |
| chills | 1.1 (.25) | 1.8 (1.11) | --- | --- |
| cold hands and feet | 1.0 (.09) | 1.9 (1.58) | --- | --- |
| headache | 1.1 (.33) | 2.2 (1.32) | --- | --- |
| lightheadedness | 1.1 (.25) | 1.9 (1.21) | --- | --- |
| sore muscles | --- | --- | 1.3 (.50) | 2.3 (1.04) |
| swollen ankles | --- | --- | 1.1 (.34) | 1.7 (.98) |
| stiff muscles | --- | --- | 1.3 (.53) | 2.1 (1.11) |
| stiff joints | 1.1 (.37) | 1.5 (.65) | 1.1 (.45) | 1.7 (.85) |
| pain in the joints | 1.1 (.18) | 1.4 (.65) | --- | --- |
| pain in the shoulders | 1.3 (.51) | 2.2 (1.40) | --- | --- |
| palpitation | 1.0 (.12) | 1.5 (.85) | 1.1 (.22) | 1.9 (.85) |
| heart racing | --- | --- | 1.1 (.13) | 1.8 (.81) |
| chest pain | --- | --- | 1.0 (.04) | 1.7 (.86) |
p<.05
The within-sample ANOVA for the Korean women by BDI group revealed that the High BDI group (N=24) had 19 symptoms that had significantly higher means when compared with the Low BDI group (N=12). The symptoms and means for the Korean sample are also displayed in Table 1, and include five abdominal-digestive symptoms (constipation, heartburn, no appetite, indigestion, abdominal cramps); seven neurological symptoms (numbness, weakness, dizziness, faintness, hot flashes, fatigue, tiredness); four musculoskeletal symptoms (sore muscles, swollen ankles, stiff muscles, stiff joints); and three cardiac symptoms (palpitation, heart racing, chest pain). Table 1 displays the SDS means and standard deviations for the High and Low BDI Japanese and Korean women (p<.05). The eleven shaded somatic distress items were those that were shared by the Japanese and Koreans women, and include heartburn, no appetite, indigestion, abdominal cramps, numbness, weakness, dizziness, faintness, hot flashes, stiff joints, and palpitations.
We used Multidimensional Scaling to further understand how symptoms cluster for the women in the two culture groups. Alscal proximity matrices are depicted in Figures 1 and 2. All High BDI SDS for each group are indicated with black markers. The Japanese matrix reveals that all of the symptoms but shoulder pain cluster together in the center of the axes. The Korean matrix reveals that only the cardiac and neurological symptoms plus abdominal cramps cluster together in the center of the axes.
Figure 1.
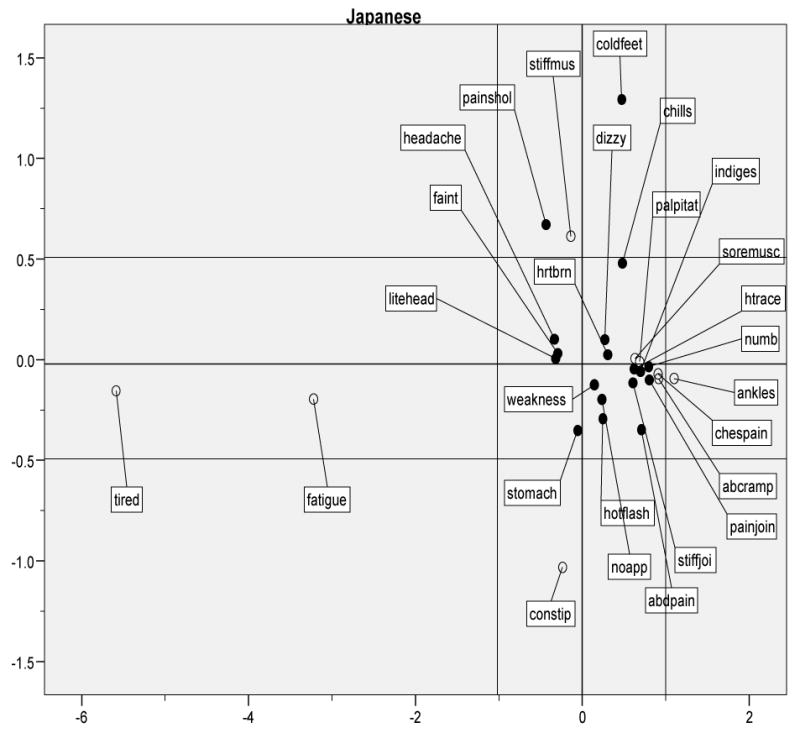
Japanese symptom MDS
Figure 2.
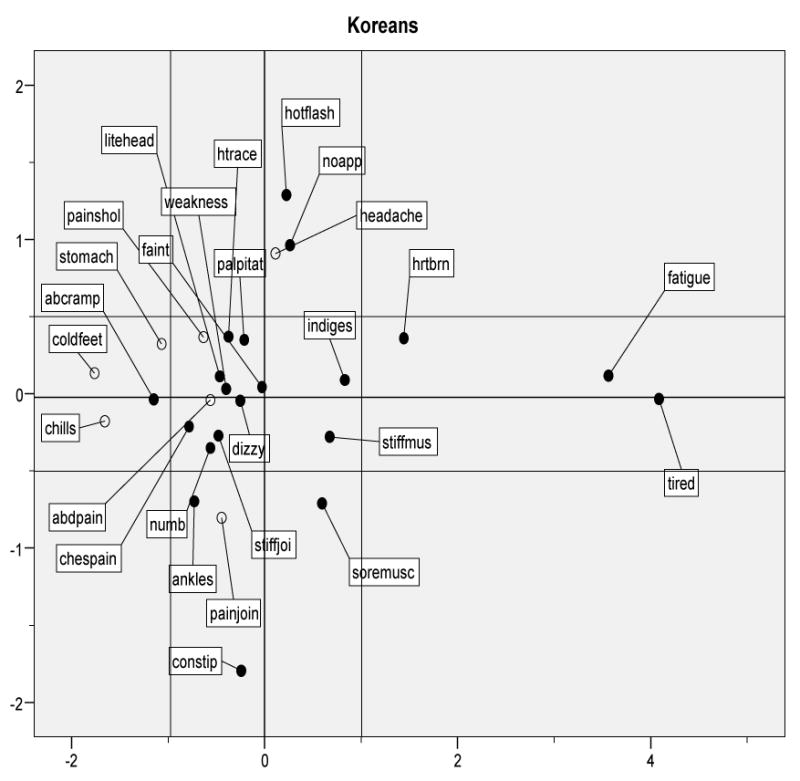
Korean Symptom MDS
Discussion
The women from both cultures had numerous and varied somatic distress symptoms, and the somatic distress means were related to their BDI scores in both groups. About half of the somatic symptoms endorsed by the women from the two Asian countries were the same. Interestingly, gastric and abdominal upset, weakness, dizziness, aches and pains, and palpitations were endorsed by High BDI women in both Asian groups as distressing. These findings map onto the literature of ethnographic and primary care studies reported in the beginning of this article. Indeed, these findings provide partial support to the notion that Japanese and Koreans may share something “Asian,” and that this may also influence idioms of distress. Finding similarities in distress profiles in wide cultural regions like Asian may be help busy practitioners narrow down all of the possible cultural differences in distress in their patient groups. The state of the science in cultural research is sophisticated enough that we can begin to develop understandings of what symptoms might be shared, which ones are specific, and why this might be so.
The differences between the somatic symptoms for the Japanese and the Korean women are subtle but noteworthy. The high BDI Japanese group had higher means for headache, numerous neurological symptoms, cold hands and feet, and shoulder pain. Fieldwork and ethnographic studies by the lead author have revealed that these are important presenting symptoms for highly distressed Japanese women in Japan and those living in the US. Interestingly, the neurological, digestive and cardiac symptoms were the ones that were proximate to each other in the MDS matrix for the Japanese. It is possible that these are the symptoms that may represent a depression sub-type. If this is so, primary care and psychiatric practitioners should assess for these symptoms. Moreover, if clinical studies reveal that these symptoms represent an important symptom cluster for the Japanese, they can be included in the target symptoms for treatment. Additional studies are also necessary to determine whether these symptoms are clinically significant, as well as whether these symptoms respond to antidepressant medication.
For the high BDI Korean women, there are two noteworthy findings. The first is that the High BDI Koreans had more cardiac and neurological symptoms than the High BDI Japanese women. This finding is also consistent with the ethnographic work cited above, and suggests that these symptoms might be important for Koreans presenting to primary or psychiatric health care providers. The second interesting finding is that while the High BDI Korean women had symptoms of constipation, fatigue and appetite disturbance (routinely assessed with western instruments), they are not proximate with the cardiac and neurological symptoms in the Korean MSD matrix. Further studies with larger samples of highly-distressed and clinical samples Koreans are necessary to understand the relationship between all of the symptoms seen in this cultural group.
The concept of display rules is helpful in the analysis of the meaning of these findings. Display rules are the social expectations about the appropriate and expected mode through which distress should be expressed (Ellsworth, 1994; Matsumoto, Tsutomu, Scherer & Wallbott, 1988; Mesquita & Karasawa, 2002). Because humans derive their conceptions of display rules, normalcy, health, deviance and illness from cultural models of display rules, consideration of these models are important in the evaluation of mental health and illness. Conventional American psychological theory suggests that direct, verbal emotional displays of distress are the universal norm, and that those who express their distress somatically are channeling their “emotional” pain through their bodies (somaticizing)(Kirmayer, Dao & Smith, 1998). This expectation is appropriate for people enculturated in a cultural model that favors emotional expression of distress such as that of the US. In other words, enculturated American people who cannot express distress in accordance with their cultural norms may have psychological barriers or pathology. As we have seen in the literature review above, in many Asian cultural models, however, the body is holistically integrated with the emotions. The distress display rules and expressions of distress through the body is the cultural norm within many Asian cultures. Therefore, we might expect to see higher somatic distress in people from Asian countries even in non-clinical groups (Saint Arnault, Sakamoto & Moriwaki, 2006). This cultural pattern is not so much stigma (strong negative reactions about having a mental illness) as it is a group-oriented social norm about display of negative emotions. In a group oriented cultural model, strong and direct displays of negative emotions are disruptive to relationships and group-harmony.1
The mean BDI score for the Japanese women was 11.8 and for the Korean women was 14; these are higher than would be expected in community-based health samples. Therefore, a cultural analysis for the use of western-derived depression measures is important here. This study used the BDI as a measure of depressive symptomology. We used this instrument because there were reliability and validity studies reported for wide variety of countries. Further, we believe that the BDI captures at least some of the distress that may be important for Japanese and Korean samples. However, previous research has shown that there may be an Asian tendency to avoid endorsement of both strong negative and positive emotions (Lee, Jones, Mineyama & Zhang, 2002). In addition, investigators have found that the East Asian beliefs and practices around the experience and expression of positive emotions may falsely inflate the depression scores on a variety of self-report depression screening instruments (Cho & Kim, 1998; Cho et al., 1998; Iwata & Buka, 2002; Iwata, Roberts & Norito, 1995; Iwata & Roberts, 1996; Iwata, Saito & Roberts, 1994; Iwata et al., 1998; Noh, Kasper and Chen, 1998). Therefore, the findings reported here may not accurately represent the incidence of depression in the women in these samples because of the avoidance of strong negative and positive emotional endorsement. Indeed, accurate depression assessment for Asian populations requires innovative research that explores the breadth of symptoms necessary to assess in Asians and other groups. This present study seeks to contribute to and stimulate this kind of research.
We believe that these data contribute to the broader debate and analysis about the validity and/or usefulness of the “Asian” concept in the diverse fields of cross-cultural psychology and international political-economic research (Fiske, 2002; Milner & Johnson, 1997; Oyserman Coon & Kemmelmeier, 2002). While most sophisticated researchers and clinicians will readily acknowledge that there is diversity within any cultural or regional group, results of studies reported in the literature rarely identify and measure those differences systematically. People who provide primary and mental health care for diverse Asian populations need this type of data to begin to identify meaningful patterns and important cultural differences within larger racial categories.
A limitation of this study is that the findings are derived from a convenience sample of female students in two cultures within the Asian culture region. We do not propose to generalize these findings across these groups, to the wider populations, or to clinical samples. However, these studies can suggest possible trends that may prompt further investigation. The findings of this study not only suggest that there may be similarities and differences in somatic distress symptoms for Japanese and Korean women, but also provides a study design that can be used to investigate the co-occurrence of somatic distress and depression in wider and more generalizable cross-cultural samples.
We believe that clinicians and researchers must develop reliable ways to measure depression-like phenomena for people from non-western cultural groups. Research on the incidence of an illness for any cultural group requires assessment with an instrument or assessment tool, and the general practice world-wide has been to use translated versions of western instruments. The widespread use of these measures across cultural groups requires the assumption that there is phenomenological equivalence between the symptoms on self-assessment indicators for the members of all of these groups—that is, the symptoms are experienced in the same way, and mean the same thing. Another assumption is that the measure in question assesses all of the relevant symptoms and indicators necessary to accurately and adequately capture the phenomenon of interest. In other words, all of the symptoms important for detecting the syndrome (in this case, depression) are present in the assessment. Unfortunately, very few studies have tackled these questions of phenomenological equivalence using symptom inventories with large groups in order to expand the symptom list to capture symptoms relevant to non-western groups.
We attempted to fill this gap by using an innovative method to discover whether there might be additional somatic symptoms experienced by Asian women with high depressive symptomology as measured by a western-derived instrument. While only a preliminary suggestion can be offered here, we find these results intriguing, and believe they warrant a series of studies in culturally-diverse, representative samples, as well as clinical samples. This study used a longitudinal method that captured distress across the span of seven days; however, we do not know the clinical significance of these symptoms. For example, the means of individual symptoms are different between the high and low BDI groups, but those means are generally low. The establishment of clinical significance is an important next step for researchers to take in understanding cultural idioms of distress. In addition, we believe that the development of an assessment instrument using important somatic symptoms across larger and more diverse samples is critical. Researchers could use factor analysis of these symptoms to delineate important subsets of related symptoms, and use these factors to determine their contribution to depression scores.
If Asians in general, and Japanese and Korean women in particular, have important somatic distresses that signal poor quality of life, difficulties in functioning and/or depression, psychiatric nurses must attend to them. American psychiatry continues to perpetuate the false dichotomy between the mind/emotions and the body every time we administer a primarily emotional assessment. Moreover, when we categorize those who show significant physical distress as having difficulties verbal expressions of emotions, we are uncritically applying western psychological theory universally. Globally-oriented psychiatric nurses know that somatic distress is less a sign of inability to express emotions and more a typical and normative idiom that conveys significant and important distress. Psychiatric nursing interventions, therefore, must begin with more comprehensive assessment tools. Next, we must research methods to respond to somatic distresses without requiring people to translate these into emotional vocabulary that we, as enculturated Americans, can understand. These interventions may include comfort measures, symptomatic relief, and interventions that aim at easing the holistic mind/body, such as Reiki, reflexology, Tai Chi, Chi Kung, Yoga, massage and other complementary therapies. Emotional and verbally-oriented counseling must be seen as important, but culturally specific, intervention strategies that are suited for people socialized in cultural models that commonly have verbal, emotional idioms of distress.
Acknowledgments
This research was supported by the Office of Research and Doctoral programs at Michigan State University College of Nursing.
Footnotes
Stigma about mental illness in many Asian cultures may be related to family shame and concerns about whether this illness might be hereditary, making children with mental illness less desirable for marriage. This present study is not focused on mental illness, per se, however, since it is not clear that the BDI captures the full extent of depression in women from these cultures. While full analysis of the social significance of certain illnesses is beyond the scope of this paper, see Saint Arnault (in press).
Contributor Information
Denise Saint Arnault, Michigan State University, B510-B West Fee Hall, Nursing Research Center, East Lansing, Michigan, USA 48824.
Oksoo Kim, Ewha Woman's University, College of Nursing Science, 11-1, Daehyun-Dong, Sudaemun-Gu, Seoul, Korea, 120-750.
References
- Abdel-Khalek AM. Internal consistency of an Arabic Adaptation of the Beck Depression Inventory in four Arab countries. Psychological Reports. 1998;82(1):264–266. doi: 10.2466/pr0.1998.82.1.264. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Aune KS, Aune RK. Cultural differences in the self-reported experience and expression of emotions in relationships. Journal of Cross-Cultural Psychology. 1996;27(1):67–81. [Google Scholar]
- Barrera M, Garrison-Jones CV. Properties of the Beck Depression Inventory as a screening instrument for adolescent depression. Journal of Abnormal Child Psychology. 1988;16:263–273. doi: 10.1007/BF00913799. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Bonicatto S, Dew AM, Soria JJ. Analysis of the psychometric properties of the Spanish version of the Beck Depression Inventory in Argentina. Psychiatry Research. 1998;79(3):277–285. doi: 10.1016/s0165-1781(98)00047-x. [DOI] [PubMed] [Google Scholar]
- Cho M, Kim K. Use of the Center for Epidemiologic Studies Depression (CES-D) Scale in Korea. Journal of Nervous and Mental Disease. 1998;186(5):304–310. doi: 10.1097/00005053-199805000-00007. [DOI] [PubMed] [Google Scholar]
- Cho M, Nam J, Suh G. Prevalence of symptoms of depression in a nationwide sample of Korean adults. Psychiatry Research. 1998;81(3):341–352. doi: 10.1016/s0165-1781(98)00122-x. [DOI] [PubMed] [Google Scholar]
- Ellsworth P. Sense, culture and sensibility. In: Markus H, Kitayama S, editors. Emotion and culture: Empirical studies in mutual influence. Washington, D.C.: American Psychological Association; 1994. pp. 23–50. [Google Scholar]
- Fiske AP. Using Individualism and Collectivism to Compare Cultures—A Critique of the Validity and Measurement of the Constructs:Comment on Oyserman et al. (2002) Psychological Bulletin. 2002;128(1):78–88. doi: 10.1037/0033-2909.128.1.78. [DOI] [PubMed] [Google Scholar]
- Gureje O, Simon GE, Ustun TB, Goldberg DP. Somatization in cross-cultural perspective: A World Health Organization study in primary care. American Journal of Psychiatry. 1997;154(7):989–995. doi: 10.1176/ajp.154.7.989. [DOI] [PubMed] [Google Scholar]
- Hinton D, Hinton S. Panic disorder, somatization, and the new cross-cultural psychiatry: the seven bodies of a medical anthropology of panic. Culture, Medicine & Psychiatry. 2002;26(2):155–178. doi: 10.1023/a:1016374801153. [DOI] [PubMed] [Google Scholar]
- Holland D, Quinn N, editors. Cultural models in language and thought. New York, NY: Cambridge University Press; 1987. [Google Scholar]
- Iwata N, Buka S. Race/ethnicity and depressive symptoms: A cross-cultural/ethnic comparison among university students in East Asia, North and South America. Social Science & Medicine. 2002;55(12):2243–2252. doi: 10.1016/s0277-9536(02)00003-5. [DOI] [PubMed] [Google Scholar]
- Iwata N, Roberts C, Norito K. Japan-US comparison of responses to depression scale items among adult workers. Psychiatry Research. 1995;58:237–245. doi: 10.1016/0165-1781(95)02734-e. [DOI] [PubMed] [Google Scholar]
- Iwata N, Roberts R. Age differences among Japanese on the Center for Epidiologic Studies Depression scale: An Ethnocultural perspective on somatization. Social Science and Medicine. 1996;43(6):967–974. doi: 10.1016/0277-9536(96)00005-6. [DOI] [PubMed] [Google Scholar]
- Iwata N, Saito K, Roberts RE. Responses to a self-administered depression scale among younger adolescents in Japan. Psychiatry Research. 1994;53(3):275–287. doi: 10.1016/0165-1781(94)90055-8. [DOI] [PubMed] [Google Scholar]
- Iwata N, Umesue M, Egashima K, Hiro H, Mizoue T, Mishima N, et al. Can positive affect items be used to assess depression disorders in the Japanese population? Psychological Medicine. 1998;28:153–158. doi: 10.1017/s0033291797005898. [DOI] [PubMed] [Google Scholar]
- Kanno S. On the somatization of symptom in psychosomatic disease: consideration of Rorschach score (author's transl) Shinrigaku Kenkyu: The Japanese Journal of Psychology. 1981;52(1):30–37. [PubMed] [Google Scholar]
- Kagawa-Singer M, Chung RCY. Toward a new paradigm: A cultural systems approach. In: Kurasaki KS, Okazaki S, editors. Asian American mental health: Assessment theories and methods. New York, NY: Kluwer Academic/Plenum Publishers; 2002. pp. 47–66. [Google Scholar]
- Kawanishi Y. Somatization of Asians: An artifact of Western Medicalization. Transcultural Psychiatric Research Review. 1992;29:5–36. [Google Scholar]
- Kirmayer LJ. Culture and psychiatric epidemiology in Japanese primary care. General Hospital Psychiatry. 1993;15(4):219–223. doi: 10.1016/0163-8343(93)90036-n. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ. Cultural variations in the clinical presentation of depression and anxiety: Implications for diagnosis and treatment. Journal of Clinical Psychiatry. 2001;62 13:22–28. [PubMed] [Google Scholar]
- Kirmayer LJ. Cultural variations in the clinical presentation of depression and anxiety: Implications for diagnosis and treatment. Journal of Clinical Psychiatry. 2001;62 13:22–28. [PubMed] [Google Scholar]
- Kirmayer LJ, Dao THT, Smith A. Somatization and psychologization: Understanding cultural idioms of distress. In: Okpaku S, editor. Clinical methods in Transcultural Psychiatry. Washington, DC: American Psychiatric Press, Inc; 1998. pp. 233–265. [Google Scholar]
- Kirmayer LJ, Groleau D. Affective disorders in cultural context. Psychiatric Clinics of North America Special Issue: Cultural psychiatry: International perspectives. 2001;24(3):465–478. doi: 10.1016/s0193-953x(05)70241-0. [DOI] [PubMed] [Google Scholar]
- Kitayama S, Markus HR, Kurokawa M. Culture, emotion, and well-being: Good feelings in Japan and the United States. Cognition & Emotion. 2000;14(1):93–124. [Google Scholar]
- Kim MT. Measuring Depression in Korean Americans: Development of the Kim Depression Scale for Korean Americans. Journal of Transcultural Nursing. 2002;13(2):109–117. doi: 10.1177/104365960201300203. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Neurasthenia and depression: A study of somatization and culture in China. Culture, Medicine & Psychiatry. 1982;6(2):117–190. doi: 10.1007/BF00051427. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Do psychiatric disorders differ in different cultures? The methodological questions. In: Kleinman A, editor. The culture and psychology reader. New York, NY: New York University Press; 1995. pp. 631–651. [Google Scholar]
- Kojima M, Furukawa TA, Takahashi H, Kawai M, Nagaya T, Tokudome S. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatry Research. 2002;110(3):291–299. doi: 10.1016/s0165-1781(02)00106-3. [DOI] [PubMed] [Google Scholar]
- Kuo WH. Prevalence of depression among Asian-Americans. Journal of Nervous & Mental Disease. 1984;172(8):449–457. doi: 10.1097/00005053-198408000-00002. [DOI] [PubMed] [Google Scholar]
- Lee JW, Jones PS, Mineyama Y, Zhang XE. Cultural differences in responses to a Likert scale. Research in Nursing & Health. 2002;25(4):295–306. doi: 10.1002/nur.10041. [DOI] [PubMed] [Google Scholar]
- Lee S. A Chinese perspective of somatoform disorders. Journal of Psychosomatic Research. 1997;43(2):115–119. doi: 10.1016/s0022-3999(97)00037-8. [DOI] [PubMed] [Google Scholar]
- Lin KM. Hwa-Byung: A Korean culture-bound syndrome? American Journal of Psychiatry. 1983;140(1):105–107. doi: 10.1176/ajp.140.1.105. [DOI] [PubMed] [Google Scholar]
- Lin KM, Lau JK, Yamamoto J, Zheng Y, et al. Hwa-Byung: A community study of Korean Americans. Journal of Nervous & Mental Disease. 1992;180(6):386–391. [PubMed] [Google Scholar]
- Lock M. Protests of a good wife and wise mother: The medicalization of distress in Japan. In: Norbeck E, Lock M, editors. Health, illness, and medical care in Japan: Cultural and social dimensions. Honolulu, HI: University of Hawaii Press; 1987. pp. 130–157. [Google Scholar]
- Lum JL. Ethnic differences in the expression of affection and other emotions. Dissertation Abstracts International: Section B: The Sciences & Engineering. 1997;58(3B):1596. [Google Scholar]
- Maeno T, Kizawa Y, Ueno Y, Nakata Y, Sato T. Depression among primary care patients with complaints of headache and general fatigue. Primary Care Psychiatry. 2002;8(2):69–72. [Google Scholar]
- Matsumoto D, Tsutomu K, Scherer K, Wallbott H. Antecedents of and reactions to emotions in the United States and Japan. Journal of Cross-Cultural Psychology. 1988;19(3):267–286. [Google Scholar]
- Mesquita B, Karasawa M. Different emotional lives. Cognition & Emotion. 2002;16(1):127–141. [Google Scholar]
- Milner A, Johnson D. The Idea of Asia. In: Ingleson J, editor. Regionalism, Subregionalism and APEC. Monash Asia Institute; 1997. pp. 1–19. [Google Scholar]
- Mino Y, Aoyama H, Froom J. Depressive disorders in Japanese primary care patients. Family Practice. 1994;11(4):363–367. doi: 10.1093/fampra/11.4.363. [DOI] [PubMed] [Google Scholar]
- Moscovici S. Notes towards a description of social representations. European Journal of Social Psychology. 1988;18(3):211–250. [Google Scholar]
- Nakao M, Yamanaka G, Kuboki T. Suicidal ideation and somatic symptoms of patients with mind/body distress in a Japanese psychosomatic clinic. Suicide & Life-Threatening Behavior. 2002;32(1):80–90. doi: 10.1521/suli.32.1.80.22179. [DOI] [PubMed] [Google Scholar]
- Nichter M. Idioms of distress: Alternatives in the expression of psychological distress. Culture, Medicine and Psychiatry. 1981;5:379–408. doi: 10.1007/BF00054782. [DOI] [PubMed] [Google Scholar]
- Noh S, Kasper V, Chen X. Measuring depression in Korean Immigrants: Assessing validity of the translated Korean version of the CES-D scale. Cross-Cultural Research: The Journal of Comparative Social Science. 1998;32(4):358–377. [Google Scholar]
- Ohnuki-Tierney E. Illness and culture in contemporary Japan: An anthropological view. London: Cambridge University Press; 1984. [Google Scholar]
- Okazaki S. Cultural variations in the self and emotional distress. Dissertation Abstracts International: Section B: The Sciences & Engineering. 1994;55(4B):1675. [Google Scholar]
- Okazaki S. Asian American and White American differences on affective distress symptoms: Do symptom reports differ across reporting methods? Journal of Cross-Cultural Psychology. 2000;31(5):603–625. [Google Scholar]
- Ots T. The angry liver, the anxious heart and the melancholy spleen: The phenomenology of perceptions in Chinese culture. Culture, Medicine & Psychiatry. 1990;14(1):21–58. doi: 10.1007/BF00046703. [DOI] [PubMed] [Google Scholar]
- Oyserman D, Coon HM, Kemmelmeier M. Rethinking individualism and collectivism: Evaluation of theoretical assumptions and meta-analysis. Psychological Bulletin. 2002;128(1):3–72. [PubMed] [Google Scholar]
- Pang KYC. Symptoms of depression in elderly Korean immigrants: Narration and the healing process. Culture, Medicine & Psychiatry. 1998;22(1):93–122. doi: 10.1023/a:1005389321714. [DOI] [PubMed] [Google Scholar]
- Pang KYC. Symptom expression and somatization among elderly Korean Immigrants. Journal of Clinical Geropsychology. 2000;6(3):199–212. [Google Scholar]
- Park YJ, Kim HS, Kang HC, Kim JW. A Survey of Hwa-Byung in Middle-Age Korean Women. Journal of Transcultural Nursing. 2001;12(2):115–122. doi: 10.1177/104365960101200205. [DOI] [PubMed] [Google Scholar]
- Park L, Hinton D. Dizziness and panic in China: associated sensations of Zang Fu organ disequilibrium. Culture, Medicine & Psychiatry. 2002;26(2):225–257. doi: 10.1023/a:1016341425842. [DOI] [PubMed] [Google Scholar]
- Parsons CD, Wakeley P. Idioms of distress: Somatic responses to distress in everyday life. Culture, Medicine & Psychiatry. 1991;15(1):111–132. doi: 10.1007/BF00050830. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW. The psychology of physical symptoms. New York: Springer-Verlag; 1982. [Google Scholar]
- Saint Arnault D, Sakamoto S, Moriwaki A. Somatic and Depressive Symptoms in Female Japanese and American Students: A Preliminary Investigation. Transcultural Psychiatry. 2006;43(2):275–286. doi: 10.1177/1363461506064867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault D. Cultural Determinants of Help Seeking: A model for research and practice. Research and Theory in Nursing Practice. doi: 10.1891/1541-6577.23.4.259. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz JE, Stone AA. Strategies for analyzing ecological momentary assessment data. Health Psychology. 1998;17(1):6–16. doi: 10.1037//0278-6133.17.1.6. [DOI] [PubMed] [Google Scholar]
- Shek DT. Reliability and factorial structure of the Chinese version of the Beck Depression Inventory. Journal of Clinical Psychology. 1990;46(1):35–43. doi: 10.1002/1097-4679(199001)46:1<35::aid-jclp2270460106>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Shiffman SM, Stone AA. Ecological momentary assessment: A new tool for behavioral medicine research. In: Krantz D, Baum A, editors. Technology and methods in behavioral medicine. Mahwah, NJ: Lawrence Erlbaum Associates, Inc., Publishers; 1998. pp. 117–131. [Google Scholar]
- Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. New England Journal of Medicine. 1999;341(18):1329–1335. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- Stone AA, Schwartz JE, Neale JM, Shiffman S, Marco CA, Hickcox M, et al. A comparison of coping assessed by ecological momentary assessment and retrospective recall. Journal of Personality & Social Psychology. 1998;74(6):1670–1680. doi: 10.1037//0022-3514.74.6.1670. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman SS, DeVries MW. Ecological momentary assessment. In: Kahneman D, Diener E, Schwarz N, editors. Well-being: The foundations of hedonic psychology. New York, NY: Russell Sage Foundation; 1999. pp. 26–39. [Google Scholar]
- Takauchi D, Kuo H, Kim K, Leaf P. Psychiatric symptom dimensions among Asian Americans and native Hawaiians: An analysis of the Symptom Checklist. Journal of Community Psychiatry. 1989 October;17:319–329. doi: 10.1002/1520-6629(198910)17:4<319::AID-JCOP2290170405>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Mental Health: Culture, Race and Ethnicity--A supplement to Mental Health: A report to the Surgeon General. Rockville, MD: Public Health Service, Office of the Surgeon General; 2001. [Google Scholar]
- Ware NC, Kleinman A. Depression in neurasthenia and chronic fatigue syndrome. Psychiatric Annals. 1992;22(4):202–208. [Google Scholar]
- Waza K, Graham AV, Zyzanski SJ, Inoue K. Comparison of symptoms in Japanese and American depressed primary care patients. Family Practice. 1999;16(5):528–533. doi: 10.1093/fampra/16.5.528. [DOI] [PubMed] [Google Scholar]
- Werner O, Campbell DT. Translating, working through interpreters, and the problem of decentering. In: Naroll R, Cohen R, editors. A handbook of method in cultural anthropology. New York: American Museum of History; 1971. pp. 398–420. [Google Scholar]
- Yeung A, Howarth S, Chan R, Sonawalla S, Nierenberg AA, Fava M. Use of the Chinese version of the Beck Depression Inventory for screening depression in primary care. Journal of Nervous & Mental Disease. 2002;190(2):94–99. doi: 10.1097/00005053-200202000-00005. [DOI] [PubMed] [Google Scholar]


