SYNOPSIS
Objective
Although measles has not been endemic in the U.S. since 1997 due to high vaccination coverage, recent U.S. measles outbreaks have been associated with individuals and groups who have refused vaccination for philosophical, cultural, or religious reasons. One such outbreak occurred in Indiana among a group of church members in May and June of 2005. Our objectives were to: (1) determine attitudes and beliefs of church leaders and members regarding vaccinations and the outbreak experience, (2) describe reasons for vaccine acceptance and nonacceptance, and (3) assess the feasibility of a knowledge and attitudes study in the context of a vaccine-preventable disease outbreak.
Methods
We conducted a focus group with church leaders and families and held 12 structured household interviews with church members directly and indirectly involved in the outbreaks.
Results
A combination of safety concerns, personal experience, and religious beliefs contributed to vaccination refusal among a subgroup of church members. While the experience with measles disease did not necessarily translate into a more positive perception of vaccines, most families that refused vaccination would accept some future vaccines under unique circumstances, such as disease presence in the community or if vaccination could be delayed until a child was older.
Conclusions
Lessons learned from this outbreak experience can inform future outbreak investigations elsewhere. Maintaining open communication with parents who refuse immunizations, as well as working with their trusted social networks, can help public health professionals facilitate alternative means of disease control during a vaccine-preventable disease outbreak in the community.
Measles disease, while still a cause of considerable morbidity and mortality internationally, is no longer endemic in the U.S.1,2 Of the 37 confirmed measles cases in the U.S. in 2004, 33 (89%) were either directly imported from abroad or epidemiologically linked to an imported case.3 Measles vaccination coverage for U.S. children has consistently been above 90% in recent years, helping to limit the size of outbreaks associated with an imported case.4,5 However, outbreaks have been associated with groups that refuse vaccination for philosophical, cultural, or religious reasons.6–8
One such outbreak occurred in May and June of 2005, when an unvaccinated 17-year-old female returned from philanthropic work in Romania and became the source of an outbreak among a church congregation.9 While the disease burden and economic impact of this outbreak have been described elsewhere,10 a better understanding of the vaccine attitudes and beliefs of church members and how those beliefs were impacted by the congregation's outbreak experience could help inform future outbreak investigations among unvaccinated groups. Therefore, the objectives of this follow-up study were to: (1) determine attitudes and beliefs of church members and leaders regarding vaccinations and the outbreak experience, (2) describe reasons for vaccine acceptance and nonacceptance, and (3) assess the feasibility of a knowledge and attitudes study in the context of a vaccine-preventable disease outbreak.
METHODS
This study used a combination of focus group and telephone interviews with families directly and indirectly involved in the outbreak. This mixed-method approach was chosen, in part, to offer flexibility in the community setting, as well as to take advantage of the complementary strengths of each method in tailoring questions that were most appropriate for the specific community involved.11
Part 1: Focus group
We conducted a focus group discussion to help us gain an in-depth understanding of the experiences of families and church leaders directly involved in the outbreak. The group discussion was also used to tailor the follow-up interview questions and methodology to the community involved to collect relevant, culturally sensitive data. A convenience sample of two church leaders and four adult church members (n = 6) took part. The adult church members represented three households that had experienced measles cases in the outbreak, either directly or as parents of pediatric cases, and were invited by church leaders to participate in the discussion. Two researchers led the discussion while a third took notes. Questions were asked using a semistructured moderator's guide developed by Centers for Disease Control and Prevention (CDC) staff. Question areas included: church advice and involvement regarding health issues; vaccine knowledge, attitudes, and beliefs; relationship with the health-care system; outbreak experiences; changes in families' vaccine beliefs after the outbreak; and the church's response to the outbreak.
With the permission of participants, the focus group was tape-recorded for transcription purposes. Group participation was voluntary, and participants were not reimbursed for their time. The discussion took approximately 90 minutes. All focus group members were given the opportunity to speak. One researcher transcribed the recording and analyzed the transcript for relevant themes using Nvivo qualitative analysis software.12
Part 2: Interviews of outbreak and comparison households
Themes that emerged from the focus group discussion were also used to create a structured interview instrument. At the suggestion of church leaders and health department personnel, the questions were formatted to be given as either a face-to-face or telephone interview, depending on the respondent's preference. Researchers reviewed the interview instrument for content, clarity, and length before it was administered.
Eleven households were directly involved in the outbreak.10 Of those households, one was never associated with the church, one was no longer associated with the church at the time of the study, and one was unavailable at the time of the study due to travel. In addition, two households took part in the focus group but not the interviews.1 Therefore, six households with measles were interviewed. An additional convenience sample of six church households that did not directly experience measles in the outbreak but were aware of the outbreak served as a comparison group. Church leaders made initial contacts with all 12 of these households.
After the initial contacts were made, researchers contacted all 12 study households by telephone to introduce the study. None of the contacted households refused participation. Participants were given the choice of being interviewed by telephone or in person; one comparison participant chose to be interviewed in person while the rest chose telephone interviews. Respondents were told that all answers would remain confidential, that their names would never be associated with their responses, and that any reports would contain only aggregate data. Two researchers conducted the interviews using the same standardized call script and interview questions. Interviews took about 15–20 minutes to complete. At the conclusion of each interview, respondents were given contact information for researchers in case they had any questions or concerns later.
Interview questions were divided into four sections: vaccination status, health-care use, vaccine attitudes and beliefs, and demographics. Questions were primarily closed-ended with multiple response options, but the instrument did include open-ended follow-up questions. Responses were entered into a Microsoft® Access database.13 We calculated frequencies of each response, stratified by outbreak status (measles household or comparison household without measles). Because this was a descriptive study with a small number of participating households, without the statistical power to conduct tests of association, the analysis was descriptive. Because most measles households experienced multiple measles cases and only one interview was done per household, the household was determined to be the unit of analysis.10 In households with multiple measles cases among children, parents were instructed to answer the interview questions on behalf of the youngest child. Similarly, respondents in comparison households were asked to answer on behalf of their youngest child; if there were no children in the household, respondents were the subject of the interview.
RESULTS
Part 1: Focus group
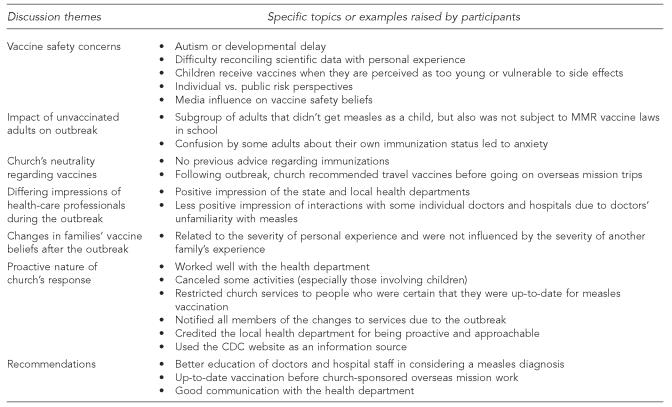
Several themes emerged from the focus group, including vaccine safety concerns, impact of unvaccinated adults on the outbreak, neutrality of the church regarding vaccination, differing impressions of health-care professionals during the outbreak, changes in families' vaccine beliefs after the outbreak, and the proactive nature of the church's response to the outbreak; these are highlighted in greater detail in the Figure.
Part 2: Interviews of outbreak and comparison households
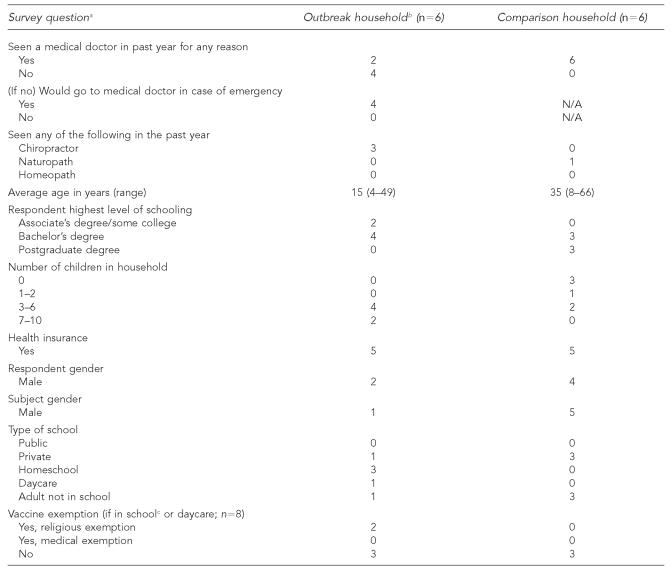
All 12 households that were approached for participation agreed to be interviewed. Eight of the 12 interview respondents were parents who answered on behalf of a child aged 18 or younger, and only one adult with measles was interviewed. Table 1 shows selected demographic characteristics of interview respondents and subjects, stratified by measles status in the outbreak.
Table 1.
Demographic characteristics of interview respondents stratified by outbreak involvement
All questions unless otherwise indicated refer to the subject of the interview; parents answered questions on behalf of subjects younger than age 18.
“Outbreak household” refers to church households that directly experienced one or more measles cases; “comparison household” refers to church households that were aware of the outbreak but did not directly experience measles cases.
Includes homeschool
N/A = not applicable
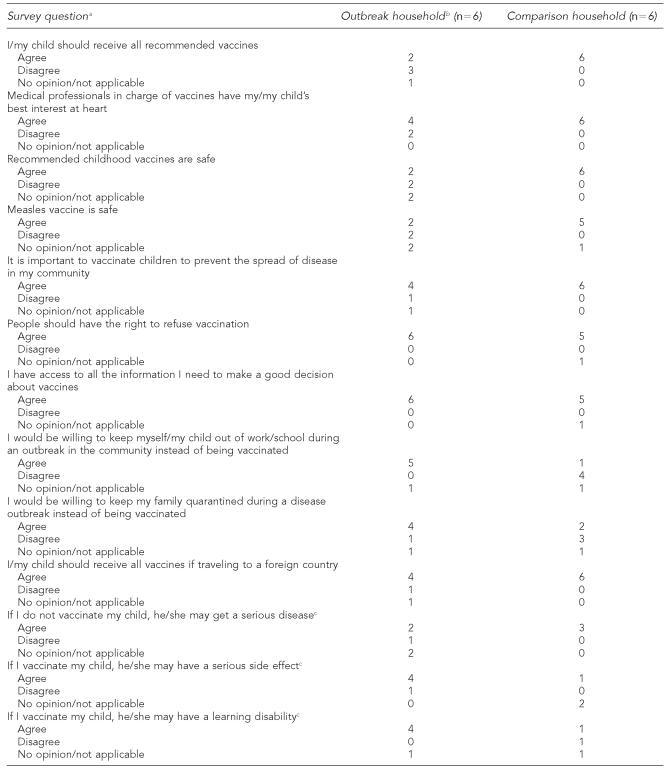
Vaccine attitudes and beliefs.
In general, outbreak households recognized the importance of vaccines, yet had concerns or doubts about their safety and necessity (Table 2). Most agreed that travel outside the U.S. was a reason to receive all recommended vaccines and that vaccination is important to stop the spread of disease in a community. However, there was less agreement that children should receive all recommended vaccines and that childhood vaccines in general and the measles vaccine in particular are safe. Most believed that childhood vaccinations may cause serious side effects or learning disabilities. All believed in the right to refuse vaccines, but were open to alternatives such as quarantine or staying out of school or work during an outbreak. All reported that they had access to enough information on vaccination.
Table 2.
Selected vaccine attitudes and beliefs of respondents stratified by outbreak involvement
All questions unless otherwise indicated refer to the subject of the interview; parents answered questions on behalf of subjects younger than age 18.
“Outbreak household” refers to church households that directly experienced one or more measles cases; “comparison household” refers to church households that were aware of the outbreak but did not directly experience measles cases.
Asked only if interview subject was a child (n = 8)
The comparison group was more positive regarding vaccine safety and necessity. All thought that they should receive all recommended vaccines as well as travel vaccines, and all agreed that vaccines in general and measles vaccine in particular are safe. All thought that vaccination was important for preventing disease in the community, yet most also agreed that people should have the right to refuse vaccination. The majority felt that they had access to enough information on vaccines.
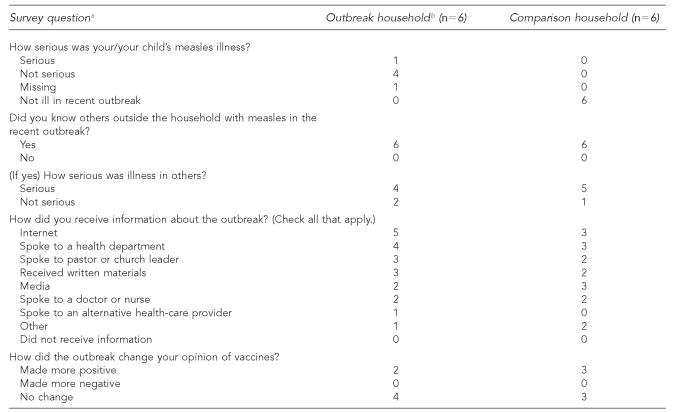
Outbreak experiences.
Most outbreak households reported that the experience did not change their opinion of vaccines (Table 3). All but one household described the illness they experienced as not serious. All also knew someone outside of the household with measles in the recent outbreak, and the majority said that they knew someone outside of the household with a serious case. Most households reported getting some type of information on measles or the outbreak from the Internet, the health department, or a church leader, and several also received information from the media or a doctor.
Table 3.
Outbreak experiences stratified by outbreak involvement
All questions unless otherwise indicated refer to the subject of the interview; parents answered questions on behalf of subjects younger than age 18.
“Outbreak household” refers to church households that directly experienced one or more measles cases; “comparison household” refers to church households that were aware of the outbreak but did not directly experience measles cases.
Half of the comparison households reported that the experience made their opinion of vaccines more positive, while half reported that the experience did not change their opinion of vaccines; however, one of the households clarified that their opinion of vaccines was already very high. All of the comparison households knew somebody with measles in the recent outbreak, and all but one reported knowing someone with a serious case of measles. The Internet, media, and health department were the most commonly listed sources of information on the outbreak for comparison households.
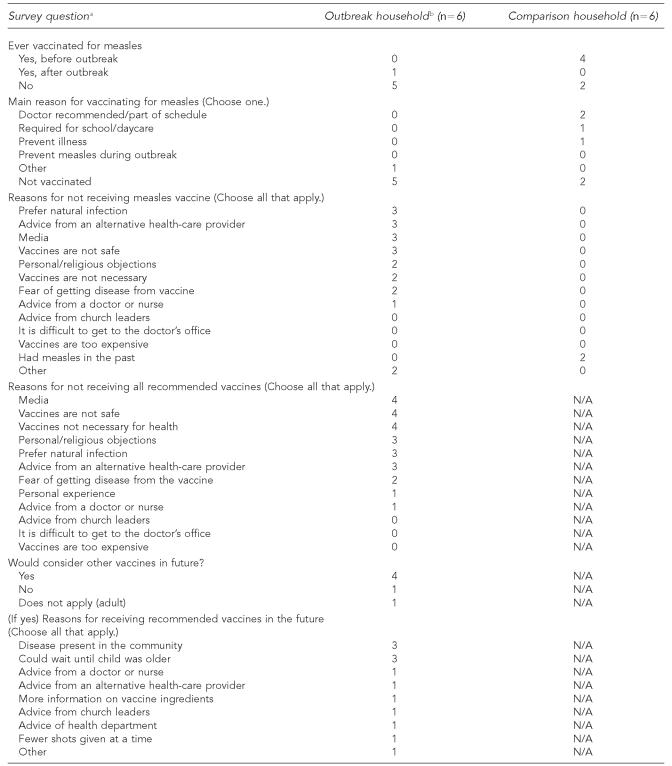
Reasons for acceptance and nonacceptance of vaccines.
Only one of the six interview subjects in the outbreak households was vaccinated with the measles-mumps-rubella (MMR) vaccine, and this was done after the outbreak (Table 4). The reasons cited most often for not receiving measles-containing vaccine included: a preference for naturally acquired infection, advice from an alternative health-care provider, media, personal religious objections to vaccination, the belief that vaccines are unsafe or unnecessary, and a fear of getting the disease from the vaccine. The same reasons were cited most often when respondents were asked about vaccines in general. Four of the six outbreak households reported that they would consider some or all recommended vaccines in the future; reasons for receiving these vaccines in the future included disease presence in the community and the ability to delay vaccination until a child was older.
Table 4.
Reasons for acceptance and nonacceptance of vaccines stratified by outbreak involvement
All questions unless otherwise indicated refer to the subject of the interview; parents answered questions on behalf of subjects younger than age 18.
“Outbreak household” refers to church households that directly experienced one or more measles cases; “comparison household” refers to church households that were aware of the outbreak but did not directly experience measles cases.
N/A = not applicable
Four of the six comparison subjects were vaccinated for measles before the outbreak; the two who were not vaccinated before the outbreak were adults who had had measles as children, before MMR vaccine was widely recommended. Among the vaccinated comparison subjects, reasons for vaccination included doctor recommendation, school requirement, and illness prevention.
DISCUSSION
A focus group was used in the context of a church-based measles outbreak to provide a more in-depth understanding of the vaccine attitudes and beliefs of members, as well as their experience with the outbreak. In turn, several of the themes raised in the focus group discussion were reinforced in structured interviews with outbreak and comparison households, including vaccine safety concerns among church members and the role of perceived disease severity in shaping vaccine attitudes and beliefs after an outbreak in the community.
While the results of this study are not generalizable due to the small number of households involved in the outbreak, several of the lessons learned from these families may be useful in future outbreaks among families that refuse vaccination. First, families and church leaders we spoke with in the focus group emphasized the importance of open and clear communication, especially between the church and the state and local health departments. Second, they highlighted the proactive role that the church community took in using its existing social network to help control the spread of measles, for instance by canceling activities involving children and restricting other activities to members who were fully vaccinated. Third, focus group participants also advocated for better education of doctors and hospital staff in considering a measles diagnosis, a suggestion that has been made previously in the context of a measles outbreak in a boarding school.14
While the church was the common link among cases, there was no formal advice regarding vaccination from the church before the outbreak. Instead, vaccine refusal was attributed to a combination of personal religious beliefs and safety concerns among a subgroup of church members; lack of access to health services was not a barrier to vaccination for this population. This suggests an opportunity for health-care providers to proactively address vaccine safety concerns among these families as well as alternatives such as a delayed or modified vaccination schedule or vaccines under special circumstances (i.e., international travel or an active local outbreak).15 This is especially important given that several families involved in the outbreak homeschooled their children or had vaccine exemptions; therefore, they were not subject to laws that require vaccination for school entry. Exemption to vaccination places individuals at increased risk of vaccine-preventable disease.16–18 Vaccine safety concerns and low perceived susceptibility and severity of vaccine-preventable diseases have been associated with nonmedical vaccine exemptions,19 and it has also been suggested that homeschooling families may be more concerned about vaccine safety than non-homeschooling families.20 Few states have a mechanism for tracking immunization rates among their homeschooling families,21 and further research is needed to identify the vaccine beliefs and behaviors, as well as the vaccine education needs, of these families.
It was unexpected that most of the outbreak households said that the experience did not make their opinion of vaccines more positive; however, additional research is needed to confirm and further explain these results. Several of these families were willing to consider certain vaccines in the future, and most reported that they would accept quarantine during any future disease outbreak in the community. This suggests that alternative means of disease control may be successful options for families that are unwilling to vaccinate.
A final objective was to test the methodology of a rapid knowledge, attitude, and belief assessment in the context of a vaccine-preventable disease outbreak. The interview instrument benefited from tailoring after the focus group discussion, and it worked well both in person and on the phone, with outbreak and comparison households, and with both adults and children (with parents answering on their behalf) as the interview subjects. The mixed-method approach also helped with data interpretation; for example, issues like vaccine safety concerns that were raised in the focus group were reinforced by interview data. The methods used can be tailored to be culturally appropriate and done within time and resource constraints.
Limitations
This study was subject to several limitations. The sample size was small (one focus group and 12 household interviews), so we were limited to a descriptive analysis of the data. Similarly, because of the qualitative nature of the focus group data, the small sample size, and the convenience sampling of comparison households, results were not generalizable beyond the community being studied. However, we included eight of the 11 households involved in the outbreak, which represented 31 of the 34 measles cases in this outbreak. Therefore, despite small numbers, we were able to meet the study objectives, which were to describe the beliefs and experiences of church members involved in the outbreak and test the study's feasibility in the context of a vaccine-preventable disease outbreak. Finally, while we asked about beliefs and behaviors before and after the outbreak, the data were cross-sectional and were gathered several weeks after the outbreak ended.
CONCLUSION
Despite these limitations, we were able to demonstrate the feasibility of a mixed-method study of the attitudes and beliefs of families involved in a measles outbreak. The study was useful in gaining in-depth insight into the attitudes and beliefs of community members regarding vaccination and their outbreak experience, especially regarding the importance of open communication with health officials and proactive involvement of the church in helping to control the spread of disease.
Although this was a descriptive study, our results suggest that the outbreak households' experience with measles did not change their opinion of vaccines. This information can be useful in interpreting outbreak investigation data, as well as suggesting approaches for preventing or controlling outbreaks of vaccine-preventable diseases in other communities with members who refuse some or all vaccination for personal or religious reasons. The methods used in this descriptive study can be adapted to meet the needs of other communities to better understand their vaccine and vaccine-preventable disease beliefs and behaviors in the context of a vaccine-preventable disease outbreak.
Figure.
Focus group discussion themes
MMR = measles-mumps-rubella
CDC = Centers for Disease Control and Prevention
Acknowledgments
The authors thank the church and its members for their participation; Amy Parker, MSN, MPH, Gustavo Dayan, MD, and Charles LeBaron, MD, Division of Viral Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC); and Wayne Staggs, MS, and the Indiana State Department of Health for information regarding the outbreak investigation and helpful editorial comments.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC.
REFERENCES
- 1.World Health Organization. Progress in reducing global measles deaths: 1999-2003. Wkly Epidemiol Rec. 2005;80:78–81. [PubMed] [Google Scholar]
- 2.Katz SL, Hinman AR. Summary and conclusions: measles elimination meeting, 16–17 March 2000. J Infect Dis. 2004;189(Suppl 1):S43–7. doi: 10.1086/377696. [DOI] [PubMed] [Google Scholar]
- 3.Measles—United States, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(48):1229–31. [PubMed] [Google Scholar]
- 4.National, state, and urban area vaccination coverage among children aged 19–35 months— United States, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(29):717–21. [PubMed] [Google Scholar]
- 5.Epidemiology of measles—United States, 2001–2003. MMWR Morb Mortal Wkly Rep. 2004;53(31):713–6. [PubMed] [Google Scholar]
- 6.Ehresmann KR, Crouch N, Henry PM, Hunt JM, Habedank TL, Bowman R, et al. An outbreak of measles among unvaccinated young adults and measles seroprevalence study: implications for measles outbreak control in adult populations. J Infect Dis. 2004;189(Suppl 1):S104–7. doi: 10.1086/377714. [DOI] [PubMed] [Google Scholar]
- 7.Imported measles case associated with nonmedical vaccine exemption—Iowa, March 2004. MMWR Morb Mortal Wkly Rep. 2004;53(11):244–6. [PubMed] [Google Scholar]
- 8.Outbreak of measles among Christian Science students—Missouri and Illinois, 1994. MMWR Morb Mortal Wkly Rep. 1994;43(25):463–5. [PubMed] [Google Scholar]
- 9.Import-associated measles outbreak—Indiana, May–June 2005. MMWR Morb Mortal Wkly Rep. 2005;54(42):1073–5. [PubMed] [Google Scholar]
- 10.Parker AA, Staggs W, Dayan GH, Ortega-Sáanchez IR, Rota PA, Lowe L, et al. Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States. N Engl J Med. 2006;355:447–55. doi: 10.1056/NEJMoa060775. [DOI] [PubMed] [Google Scholar]
- 11.Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educational Researcher. 2004;33:14–26. [Google Scholar]
- 12.QSR International. Nvivo. Victoria (Australia): QSR International; 2002. Version 2.0. Doncaster. [Google Scholar]
- 13.Microsoft Corp. Microsoft Access. Redmond (WA): Microsoft Corp; 2003. [Google Scholar]
- 14.Yeung LF, Lurie P, Dayan G, Eduardo E, Britz PH, Redd SB, et al. A limited measles outbreak in a highly vaccinated US boarding school. Pediatrics. 2005;116:1287–91. doi: 10.1542/peds.2004-2718. [DOI] [PubMed] [Google Scholar]
- 15.Diekema DS American Academy of Pediatrics Committee on Bioethics. Responding to parental refusals of immunization of children. Pediatrics. 2005;115:1428–31. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]
- 16.Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE. Individual and community risks of measles and pertussis associated with personal exemption to immunization. JAMA. 2000;284:3145–50. doi: 10.1001/jama.284.24.3145. [DOI] [PubMed] [Google Scholar]
- 17.Salmon DA, Haber M, Gangarosa EJ, Phillips L, Smith NJ, Chen RT. Health consequences of religious and philosophical exemptions from immunization laws: individual and societal risk of measles. JAMA. 1999;282:47–53. doi: 10.1001/jama.282.1.47. [DOI] [PubMed] [Google Scholar]
- 18.Omer SB, Pan WKY, Halsey NA, Stokley S, Moulton LH, Navar AM, et al. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA. 2006;296:1757–63. doi: 10.1001/jama.296.14.1757. [DOI] [PubMed] [Google Scholar]
- 19.Salmon DA, Moulton LH, Omer SB, deHart PM, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children. Arch Pediatr Adolesc Med. 2005;159:470–6. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy AM, Gust DA. Parental vaccine beliefs and child's school type. J Sch Health. 2005;75:276–80. doi: 10.1111/j.1746-1561.2005.00037.x. [DOI] [PubMed] [Google Scholar]
- 21.Rota JS, Salmon DA, Rodewald LE, Chen RT, Hibbs BF, Gangarosa EJ. Processes for obtaining nonmedical exemptions to state immunization laws. Am J Public Health. 2001;91:645–8. doi: 10.2105/ajph.91.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]