SYNOPSIS
Objective
Nationally, infertility therapies (IFTs) are increasingly used to overcome fecundity issues. However, it is unclear to what extent noninvasive IFTs are used compared with assisted reproductive technology. To better understand outcomes related to the increasing use of all types of IFTs, we compared self-reported IFT use from a Massachusetts pilot Pregnancy Risk Assessment Monitoring System (MA-PRAMS) to IFT use recorded on birth certificates (BCs).
Methods
In 2005, Massachusetts conducted a three-month pilot study modeled after the Centers for Disease Control and Prevention's PRAMS, a population-based surveillance system that monitors pregnancy experiences. Descriptive and bivariate analyses compared responses to MA-PRAMS survey questions regarding IFT use with data collected on BCs from the same women sampled.
Results
According to MA-PRAMS, 6.1% of live births were conceived using IFTs compared with 3.1% reported on BCs. Reported IFT use varied by maternal age and plurality. For women aged 18–34 years, IFT use reported on MA-PRAMS (5.0%) was 2.5 times higher than that reported on BCs (2.0%). For women aged 35 years or older, reported IFT use was comparable in both systems. For women giving birth to singletons, IFT use reported on MA-PRAMS (5.5%) was three times higher than that reported on BCs (1.8%).
Conclusion
Higher use of IFTs was reported by MA-PRAMS than on BCs, particularly among younger women and those having singleton births. These findings suggest that self-reported IFT use might be a more sensitive method for states to use in assessing population-based IFT usage among women and monitoring trends in adverse birth outcomes.
Nationally, infertility therapies (IFTs) are increasingly used to overcome fecundity issues. IFTs consist of noninvasive procedures including fertility-enhancing drugs (FDs) and artificial insemination (AI) as well as more invasive procedures collectively called assisted reproductive technology (ART), a form of IFT in which both egg and sperm are manipulated in vitro. ART has been monitored closely in the United States by the Society of Assisted Reproductive Technology (SART) and the Centers for Disease Control and Prevention (CDC) since Congress mandated national reporting through the Fertility Clinic Success Rate and Certification Act.1
Because both ART and FDs increase the risk for multiple-infant births,2,3 they might also increase infants' risks for low birth weight, prematurity, birth defects, and death.4–7 The impact of FDs and AI on perinatal health outcomes has not been studied as closely as that of ART, and currently no national reporting system exists to monitor FDs and AI. The 2002 National Survey of Family Growth provides national estimates of IFT use but is unable to provide state-specific estimates. Timely state-level ART data have not been available through SART and CDC, and states may be interested in monitoring all types of IFTs not limited to ART. Alternative surveillance systems, more readily available at the state level, may be more appropriate to capture IFT usage.
To assess IFT data collected through state-sponsored surveillance systems and to improve the understanding of outcomes related to increasing use of IFTs, researchers evaluated the reporting of IFT use in two surveillance systems in Massachusetts, a state with high ART use. This analysis compared self-reported IFT use from a Massachusetts pilot Pregnancy Risk Assessment Monitoring System (MA-PRAMS), modeled after CDC's PRAMS, with IFT use recorded on Massachusetts birth certificates (BCs) completed by hospital clerks from patient records.
METHODS
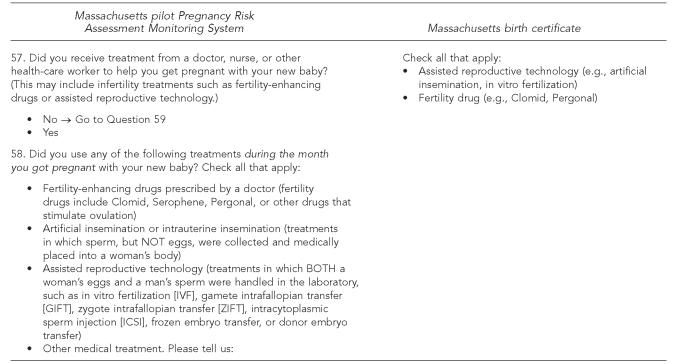
Data were obtained from MA-PRAMS and BCs maintained by the Massachusetts Department of Public Health. In 2005, the state conducted a three-month pilot study modeled after CDC's PRAMS—a population-based surveillance project conducted jointly by CDC, 37 states, and two vital records jurisdictions8—that asks about women's experiences related to pregnancy, including IFT use. (The Figure shows the actual questions related to IFT use that were asked on MA-PRAMS.) MA-PRAMS provided information on IFT use reported by a sample of women selected for the survey. MA-PRAMS data were collected from April through September 2005 from a simple random sample of 480 resident women with a recent live birth (January through March 2005). Eligible births included all live births of singletons, twins, or triplets to state-resident mothers aged 18 years or older. MA-PRAMS data were weighted for nonresponse among demographic groups of women by age, race/ethnicity, marital status, and education, and were adjusted for sampling probabilities to represent all births during this three-month period.
The general characteristics of the MA-PRAMS sample are very similar to the BC population from which the sample originated. The overall response rate for MA-PRAMS was 72.5% (n5348). Information regarding IFT use is also collected through two check boxes in the prenatal care section of the BC. (The actual check-box questions are shown in the Figure.) BC reviews provided demographic information (e.g., women's race/ethnicity and age), infant birth characteristics (e.g., plurality), and specific IFT use for the current pregnancy (e.g., ART and FDs). MA-PRAMS assessed ART use separately from AI, but ART and AI uses were combined in one check box on the BC; therefore, ART and AI use (ART/AI) information from MA-PRAMS was also combined for the purpose of this analysis. Univariate and bivariate analyses were used to compare prevalences of MA-PRAMS responses with linked BC information. Analyses were stratified by selected maternal characteristics and plurality. Differences between MA-PRAMS and BC prevalence estimates were assessed by comparing 95% confidence intervals (CIs).
Figure.
Infertility therapy questions
RESULTS
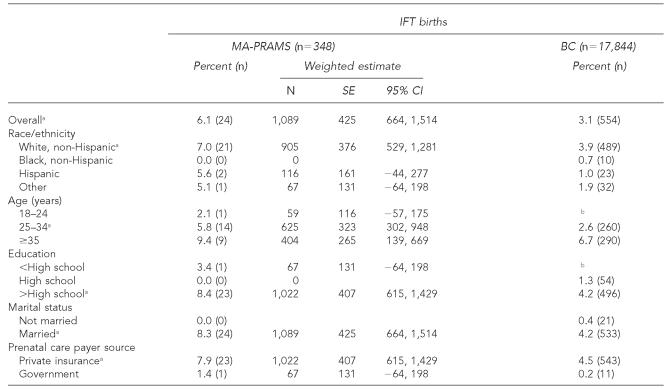
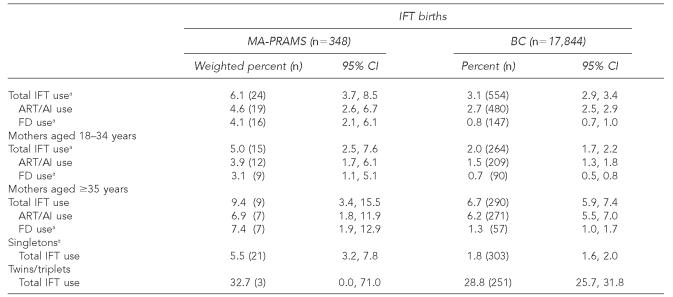
Among 17,844 infants born from January through March 2005, a higher proportion of IFT-conceived births in Massachusetts were to mothers who were white, non-Hispanic, aged 35 years or older, married, privately insured, and who had more than a high school education when compared with BCs (Table 1). Table 2 shows that according to MA-PRAMS, 6.1% (CI 3.7, 8.5) of live births were conceived using IFTs, 4.6% (CI 2.6, 6.7) using ART/AI, and 4.1% (CI 2.1, 6.1) using FDs (non-mutually exclusive categories). However, according to BCs, 3.1% (CI 2.9, 3.4) of live births were conceived using IFTs, 2.7% (CI 2.5, 2.9) using ART/AI, and 0.8% (CI 0.7, 1.0) using FDs (non-mutually exclusive categories). MA-PRAMS-reported IFT use was two times higher than that reported on BCs. Reported IFT use also varied by maternal age and plurality (Table 2). For women aged 18–34 years, IFT use reported on MA-PRAMS (5.0%, CI 2.5, 7.6) was 2.5 times higher than that reported on BCs (2.0%, CI 1.7, 2.2). For women aged 35 years or older, reported IFT use was comparable in both systems. For women giving birth to singletons, IFT use reported on MA-PRAMS (5.5%, CI 3.2, 7.8) was three times higher than that reported on BCs (1.8%, CI 1.6, 2.0). For women giving birth to twins and triplets, reporting by both systems was comparable.
Table 1.
Prevalence of infertility therapy-conceived births by maternal characteristics according to MA-PRAMS and birth certificate reviews in Massachusetts, January–March 2005
Results in which the MA-PRAMS estimate was significantly different from the number of births according to BC reviews (i.e., BC birth number not included in the MA-PRAMS 95% CI).
Calculations based on fewer than five events are suppressed to maintain the privacy of data subjects per request from the Massachusetts Department of Public Health Privacy and Data Access Office.
IFT = infertility therapy
MA-PRAMS = Massachusetts pilot Pregnancy Risk Assessment Monitoring System
BC = birth certificate
SE = standard error
CI = confidence interval
Table 2.
Prevalence of assisted reproductive technology, artificial insemination, and fertility drug-conceived births according to MA-PRAMS and birth certificate reviews in Massachusetts, January–March 2005
Significant differences between MA-PRAMS and BC reviews (nonoverlapping 95% CIs)
IFT = infertility therapy
MA-PRAMS = Massachusetts pilot Pregnancy Risk Assessment Monitoring System
BC = birth certificate
CI = confidence interval
ART = assisted reproductive technology
AI = artificial insemination
FD = fertility drug
DISCUSSION
This first look confirms that studies can be done to compare IFT birth reporting by PRAMS and BCs. Findings from MA-PRAMS suggest that IFT births are underreported on BCs, particularly among younger women and those having singleton births. Reporting differences could be attributed to several factors. Documentation of IFT use might be less likely for births of healthy singletons with no apparent complications. Also, because fertility specialists typically do not follow a pregnancy to delivery, women might return to their regular obstetrician or health-care provider after the pregnancy is stabilized to continue routine prenatal care; therefore, the delivery hospital might be unaware of the nature of the pregnancy. In addition, reporting could be affected by incomplete hospital record abstraction. Currently, hospital administrators in Massachusetts are instructed to abstract any IFT use from patients' medical records; however, the method of record abstraction might vary by hospital. Because MA-PRAMS reported higher IFT use among women with lower-risk pregnancies (e.g., younger women and singletons), the PRAMS system may provide more comprehensive information than BCs, particularly on non-ART IFTs.
PRAMS provides an opportunity for women to self-report their pregnancy experiences and reproductive history, including IFT use. Findings from this study suggest that self-reported data such as those from PRAMS might be more useful than record abstraction in improving the understanding of pregnancy experiences with IFTs. PRAMS data can be used to compare IFT users' health behaviors during pregnancy and the early postpartum period with those of nonusers, and to compare birth outcomes for infants conceived with and without IFTs. A strength of PRAMS data is that they contain and differentiate among all types of IFT use (ART, AI, FDs), and the data are weighted to allow for state-specific population-based comparisons.
Limitations
The findings in this article are subject to at least four limitations. First, MA-PRAMS had a small sample size (as reflected in relatively wide CIs around the point estimates) and represented births in Massachusetts only from January through March 2005; therefore, the findings cannot be widely generalized. Second, it is possible that IFT reporting on MA-PRAMS questionnaires and BCs varied by hospital; however, the current study did not have sufficient power to detect a difference in reporting by hospital. Massachusetts is in the process of fully implementing PRAMS and will have more data for conducting stratified analyses and providing more stable estimates in the future. The Massachusetts BC question on IFTs differs from the new U.S. Standard Certificate of Live Birth question developed by the National Center for Health Statistics and cannot be generalized to those states using the new certificate. The Massachusetts BC includes AI in the ART category, but the new U.S. Standard Certificate groups AI and FDs as one category. Nevertheless, states that have adopted the new BC might find this report useful. States that participate in CDC's PRAMS might also consider including IFT usage questions in their surveys to monitor trends in IFT births.
A third limitation is that information from CDC's ART registry on ART procedures performed by fertility clinics was not used in this analysis. It is possible that women might have reported past IFT use in addition to current use in the previous version of CDC's PRAMS survey.9 The revised wording of CDC's PRAMS IFT question to specify current use was used for this study, asking women about their IFT use during the month they got pregnant with their new babies. Nevertheless, the accuracy of self-reported IFT use cannot be assessed without access to information about actual IFT use.
Finally, CDC's PRAMS does not sample births of higher-order multiples greater than three. Given the rarity of quadruplets or higher-order multiples, however, the ascertainment of IFT use for higher multiples on BCs can be assumed to be accurate, as is suggested by our findings that reported IFT use for multiple births did not differ between surveillance systems.
CONCLUSION
Monitoring health and development beyond birth is important for infants conceived using IFTs. To appropriately allocate scarce resources, state programs should be aware of this growing population that might require additional care and services. Continued monitoring of births conceived by all types of IFTs is warranted.
Footnotes
The findings in this article are based, in part, on data provided by the Registry of Vital Records and Statistics, Massachusetts Department of Public Health.
REFERENCES
- 1. Fertility Clinic Success Rate and Certification Act of 1992, Pub. L. No. 102-493, 42 U.S.C. 263a-1 et seq. (1992 Oct 24) [PubMed]
- 2.Reynolds MA, Schieve LA, Martin JA, Jeng G, Macaluso M. Trends in multiple births conceived using assisted reproductive technology, United States, 1997–2000. Pediatrics. 2003;111(5 Pt 2):1159–62. [PubMed] [Google Scholar]
- 3.Contribution of assisted reproductive technology and ovulation-inducing drugs to triplet and higher-order multiple births—United Sates, 1980–1997. MMWR Morb Mortal Wkly Rep. 2000;49(24):535–8. [PubMed] [Google Scholar]
- 4.Multiple gestation pregnancy. The ESHRE Capri Workshop Group. Hum Reprod. 2000;15:1856–64. [PubMed] [Google Scholar]
- 5.Kiely JL. What is the population-based risk of preterm birth among twins and other multiples? Clin Obstet Gynecol. 1998;41:3–11. doi: 10.1097/00003081-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Martin JA, Park MM. Trends in twin and triplet births: 1980–97. Natl Vital Stat Rep. 1999 Sep 14;47:1–16. [PubMed] [Google Scholar]
- 7.Pharoah PO, Cooke T. Cerebral palsy and multiple births. Arch Dis Child Fetal Neonatal Ed. 1996;75:F174–7. doi: 10.1136/fn.75.3.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pregnancy Risk Assessment Monitoring System (PRAMS): methodology. [cited 2007 Apr 24]. Available from: URL: http://www.cdc.gov/prams/methodology.htm.
- 9.Schieve LA, Rosenberg D, Handler A, Rankin K, Reynolds MA. Validity of self-reported use of assisted reproductive technology treatment among women participating in the Pregnancy Risk Assessment Monitoring System in five states, 2000. Matern Child Health J. 2006;10:427–31. doi: 10.1007/s10995-006-0078-y. [DOI] [PubMed] [Google Scholar]