Abstract
Purpose:
To evaluate the ability of six biomarkers to improve prediction of cardiovascular events among persons with established coronary artery disease.
Background:
Cardiovascular risk algorithms are designed to predict the initial onset of coronary artery disease, but are less effective in persons with pre-existing coronary artery disease.
Methods:
We examined the association of N-terminal prohormone brain natriuretic peptide (Nt-proBNP), cystatin C, albuminuria, C-reactive protein (CRP), interleukin-6 (IL-6), and fibrinogen with cardiovascular events in 979 Heart and Soul Study participants with coronary artery disease after adjusting for demographic, lifestyle and behavior variables; cardiovascular risk factors, cardiovascular disease severity, medication use and left ventricular ejection fraction. The outcome was a composite of stroke, myocardial infarction, or coronary heart disease death during an average of 3.5 years of follow-up.
Results:
During follow-up, 142 (15%) participants developed cardiovascular events. The highest quartiles (versus lower 3 quartiles) of five biomarkers were individually associated with cardiovascular risk after multivariate analysis: Nt-proBNP Hazard Ratio=2.13 (95% confidence interval, 1.43 - 3.18); cystatin C 1.72 (1.10 - 2.70); albuminuria 1.71 (1.15 - 2.54); CRP 2.00 (1.40 - 2.85); and IL-6 1.76 (1.22 - 2.53). When all biomarkers were included in multivariable analysis, only Nt-proBNP, albuminuria and CRP remained significant predictors of events [HR (95% CI), 1.88 (1.23 - 2.85), 1.63 (1.09 - 2.43), 1.82 (1.24 - 2.67) respectively]. The area under the receiver operator curve (AUC) for clinical predictors alone was 0.73 (95% CI, 0.68-0.78); adding Nt-proBNP, albuminuria and CRP significantly increased the AUC to 0.77 (95% CI, 0.73-0.82, p<0.005).
Conclusion:
Among persons with prevalent coronary artery disease, biomarkers reflecting hemodynamic stress, kidney damage, and inflammation added significant risk discrimination for cardiovascular events.
Keywords: biomarkers, coronary artery disease, cardiovascular events, N-terminal prohormone brain natriuretic peptide, cystatin C, albuminuria, C-reactive protein, interleukin-6, fibrinogen
Introduction
Cardiovascular biomarkers have been extensively studied for the prediction of incident development of cardiovascular disease. Among the most studied are the inflammatory biomarker, C-reactive protein (CRP), measures of hemodynamic stress, such as brain natriuretic peptide and N-terminal prohormone brain natriuretic peptide (Nt-proBNP), and the markers of kidney disease, albuminuria and cystatin C. However, the utility of these biomarkers in the secondary prevention setting has been less well studied. These biomarkers provide important prognostic information beyond that attainable with traditional cardiovascular risk factors in the setting of acute coronary syndrome.1, 2 Whether the use of multiple biomarkers improves cardiovascular risk stratification in the outpatient setting among persons with coronary artery disease is unknown.
Traditional risk factors such as cholesterol, hypertension, and smoking may have less prognostic value in the secondary prevention setting than for primary prevention; in part this may result from the more aggressive management of these risk factors, and in part due to the relative importance of heart disease severity as a risk factor for recurrent events.2 In patients with established coronary artery disease, biomarkers may have the ability to capture dynamic pathophysiological processes such as hemodynamic function, the stability of atherosclerotic plaque, and microvascular damage to the kidney that are not assessed with standard clinical measurements. On the other hand, whether these markers provide unique predictive ability beyond traditional risk factors and standard clinical information remains unknown.
In this study we evaluated the ability of biomarkers to predict risk of cardiovascular death, myocardial infarction, or stroke among a cohort of 979 ambulatory persons with coronary artery disease who were enrolled in the Heart and Soul Study. We estimated the association of Nt-proBNP, cystatin C, albuminuria, CRP, interleukin-6 (IL-6), and fibrinogen with cardiovascular events after multivariable adjustment for standard clinical information and traditional cardiovascular risk factors. Finally, we identified the biomarkers that added the greatest predictive value in this cohort and calculated their incremental contribution to risk discrimination by plotting receiver operator characteristic (ROC) curves.
Methods
Participants
The Heart and Soul Study is a prospective cohort study designed to investigate the influence of psychosocial factors on coronary artery disease progression..3, 4 Participants were recruited from several outpatient clinics in the San Francisco Bay Area without age restriction if they met one of the following inclusion criteria:
prior myocardial infarction
angiographic evidence of >50% stenosis in one or more coronary vessels
exercise-induced ischemia by treadmill or nuclear testing
prior coronary revascularization
A total of 15,438 eligible patients were mailed an invitation, and 2495 responded with interest; 505 were unreachable and 596 declined. An additional 370 patients were excluded based on recent myocardial infarction, inability to walk 1 block, or plans to relocate.
Between September 2000 and December 2002, 1024 individuals enrolled including 549 (54%) with a history of myocardial infarction, 237 (23%) with a history of revascularization, and 238 (23%) with a physician diagnosis of coronary disease (based on a positive angiogram or treadmill test in >98% of cases). The age range of participants was 36 to 97 years. Participants underwent a daylong baseline study appointment that included a medical history interview, a physical examination, a resting echocardiogram and a comprehensive health status questionnaire. Fasting (12-hour) venous samples were drawn and plasma and sera were frozen at −70° C. Subjects for whom frozen serum (n=34) or urine samples (n=11) were excluded, resulting in a sample size of 979 participants.
Measurements:
Clinical characteristics
Candidate clinical predictors included demographic (age, sex, race) and lifestyle characteristics (physical activity, body mass index (BMI), alcohol use, and current smoking), cardiovascular risk factors (self-reported hypertension and diabetes, systolic and diastolic blood pressure, LDL and HDL cholesterol, triglycerides, and hemoglobin), cardiovascular disease history (prior myocardial infarction, stroke, heart failure, and revascularization; and echocardiographic measures of ejection fraction); and medication use (aspirin, beta-blockers, renin-angiotensin-aldosterone (RAA) inhibitors, and statins). Age, race, physical activity, smoking and alcohol use, and medical history were determined by questionnaire. Participants were instructed to bring their medication bottles to the study appointment, and study personnel recorded all current medications.
Biomarkers
Blood samples were drawn in the fasting state; serum and plasma were aliquoted and stored at −70° Celsius until January 2005. Biomarkers evaluated in this study were Nt-proBNP, cystatin C, albumin/creatinine ratio (alb/creat ratio), C-reactive protein, IL-6, and fibrinogen.
We used the Roche Elecsys electrochemiluminescence immunoassay (Roche Diagnostics, Indianapolis, IN) to measure plasma levels of NT-proBNP. Serum cystatin C was measured from frozen serum samples collected at the baseline study visit using a BNII nephelometer (Dade Behring, Inc., Deerfield, IL) with a particle-enhanced immunonephelometric assay 5. Albumin and creatinine from 24-hour urine samples were measured by nephelometry and the rate Jaffe method, respectively. Urine albumin to creatinine ratios (mg albumin / g creatinine) were calculated as the index of albuminuria as recommended by the National Kidney Foundation. High sensitivity C-reactive protein was measured from serum using the Roche Integra assay and the Beckman Extended Range assay as previously described6, 7. We used the R&D Systems Quantikine HS IL-6 Immunoassay to measure the concentration of serum IL-6. Plasma fibrinogen concentrations were determined by the Clauss assay.
Outcomes
The cardiovascular events outcome was defined as time to coronary artery disease death, nonfatal myocardial infarction, or stroke. Coronary artery disease death was defined as death during the hospitalization in which an myocardial infarction was documented, or death not explained by other etiologies that occurred within one hour of the onset of terminal symptoms.8 Nonfatal myocardial infarction was defined using standard diagnostic criteria set by the American Heart Association Council on Epidemiology and Prevention.9 Stroke was defined as a new neurological deficit not known to be secondary to brain trauma, tumor, infection, or other cause.10
Annual telephone interviews were conducted with participants or their proxy to ask about interval death or hospitalization. Trained research assistants carried out the telephone interviews using standardized scripts which were reviewed with the study team on an annual basis for quality control. Quality control for determining outcome events was maintained as follows: for any reported event, medical records, electrocardiograms, death certificates, and coroner's reports were required and reviewed by two independent and blinded adjudicators. If the adjudicators agreed on the outcome classification, their classification was binding. In the event of disagreement, the adjudicators conferred, reconsidered their classification, and requested consultation from a third blinded adjudicator as necessary.
Statistical Analysis
To model the outcome, we began by constructing a parsimonious standard clinical model. A priori, we elected to force demographic characteristics and cardiovascular disease history into all of the models. Each lifestyle cardiovascular risk factor, and cardiovascular medication variable was included if it had an association with the outcome (p<0.2) in unadjusted analyses. This adjusted “clinical” model was then used as the base model to test the added prognostic information from the biomarkers.
The potential for multiple biomarkers to have independent prognostic value depends upon the unique information they provide. Therefore, we began our analysis by determining the inter-correlations of these 6 biomarkers. We categorized the biomarkers into quartiles based upon the precedent of prior studies from Heart and Soul.11-13 In addition, we used clinically applicable cutpoints for the biomarkers currently in common use: Nt-proBNP >500pg/ml, CRP >3.0 mg/L, and albuminuria >30mg/g. We constructed multivariate proportional hazard models with each biomarker added individually to the clinical model, both as log-transformed linear variables, as dichotomous variables (high quartile versus lower three quartiles), and using the clinical cutpoints where applicable. We then combined the biomarkers as linear variables along with the clinical multivariate model to allow them to compete as predictors; backwards stepwise deletion identified those significant at p<0.05. This procedure was repeated for the dichotomized biomarkers.
Finally, we evaluated the global predictive ability of the standard clinical model for the cardiovascular outcome by computing the area under the curve (AUC) for the ROC curve14. We repeated the ROC analysis with the addition of the independently predictive biomarkers identified above and compared the resulting AUC to determine statistical significance.
Role of Funding Source
None of the funding sources had any role in the study design, collection of data, interpretation of results, preparation of this manuscript, or in the decision to submit for publication.
Results
Baseline Characteristics
Nine-hundred and seventy nine individuals were included in the analysis. Mean age was 67 years, 82% were men, and 60% were white. Over an average follow-up of 3.7 years, 142 individuals had a cardiovascular event during follow-up of which there were 87 myocardial infarctions, 26 strokes, and 50 coronary heart disease deaths.
Participants who experienced a cardiovascular event were on average 5 years older and more likely to have diabetes and hypertension, but less likely to smoke compared to participants without cardiovascular events. High-density lipoprotein cholesterol levels were lower in persons with cardiovascular events, but systolic blood pressure, LDL-C, triglycerides and BMI were similar in the two groups. In addition, the participants with recurrent events had greater prevalence of heart failure, reduced ejection fraction, and greater use of renin-angiotensin inhibitors (Table 1).
Table 1.
Characteristics of the study sample according to the development of recurrent cardiovascular disease.
| Characteristics | Cardiovascular Event (N=142) |
No events (N=837) |
p value |
|---|---|---|---|
| Demographic | Mean (SD) or N (%) | ||
| Age | 71.0 (12.0) | 66.1 (10.7) | <0.0001 |
| Male | 121 (85.2%) | 677 (80.9%) | 0.22 |
| Race | 0.60 | ||
| White or Caucasian | 91 (64.1%) | 498 (59.6%) | |
| Black or African American | 23 (16.2%) | 136 (16.3%) | |
| Asian or Pacific Islander | 13 (9.2%) | 100 (12.0%) | |
| Hispanic, Latino, or Latin American | 9 (6.3%) | 76 (9.1%) | |
| Other group not listed | 6 (4.2%) | 26 (3.1%) | |
| Cardiovascular risk factor | |||
| Diabetes mellitus | 57 (40.1%) | 202 (24.2%) | 0.0001 |
| Current smoking | 31 (22.0%) | 252 (30.4%) | 0.04 |
| Hypertension (self-report) | 112 (79.4%) | 577 (69.1%) | 0.01 |
| Systolic blood pressure | 133.6 (21.5) | 132.9 (21.0) | 0.71 |
| Low density lipoprotein | 103.2 (34.2) | 104.4 (33.9) | 0.71 |
| High density lipoprotein | 43.5 (14.0) | 46.1 (14.0) | 0.04 |
| Triglycerides | 155.1 (168.0) | 138.4 (121.1) | 0.26 |
| Body Mass Index (kg/m2) | 0.46 | ||
| <25 | 38 (26.8%) | 221 (26.4%) | |
| 25-30 | 58 (40.9%) | 349 (41.7%) | |
| >30 | 46 (32.4) | 267 (31.9) | |
| Cardiovascular disease status | |||
| Prior myocardial infarction | 85 (59.9) | 437 (52.7) | 0.11 |
| Prior cerebrovascular accident | 27 (19.0) | 112 (13.5) | 0.08 |
| Prior heart failure | 38 (26.8) | 133 (16.0) | 0.002 |
| Ejection fraction < 50% | 32 (22.5) | 78 (9.3) | <0.0001 |
| Medication use | |||
| Aspirin | 112 (78.9) | 646 (77.2) | 0.66 |
| Angiotensin converting enzyme inhibitors/ Angiotensin receptor blockers | 90 (63.4) | 416 (49.7) | 0.003 |
| Statins | 88 (62.0) | 542 (64.8) | 0.52 |
| Beta-Blockers | 90 (63.4) | 474 (56.6) | 0.13 |
Correlation among Biomarkers
The inter-correlations among the 6 candidate biomarkers are presented in Table 2. Strong correlations (all>0.4) were observed among the 3 inflammatory biomarkers, CRP, IL-6, fibrinogen, as well as between Nt-proBNP and cystatin C.
Table 2.
Inter-correlations among six biomarkers measured in the Heart and Soul cohort
| Nt-proBNP | Cystatin C | Albuminuria | C-Reactive Protein |
Interleukin-6 | Fibrinogen | |
|---|---|---|---|---|---|---|
| Nt-proBNP | 1.00 | 0.46 | 0.20 | 0.13 | 0.29 | 0.11 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Cystatin C | 1.00 | 0.30 | 0.15 | 0.28 | 0.26 | |
| <0.001 | <0.001 | <0.001 | <0.001 | |||
| Albuminuria | 1.00 | 0.06 | 0.11 | 0.17 | ||
| 0.07 | <0.002 | <0.001 | ||||
| C-Reactive Protein | 1.00 | 0.52 | 0.50 | |||
| <0.001 | <0.001 | |||||
| Interleukin-6 | 1.00 | 0.41 | ||||
| <0.001 | ||||||
| Fibrinogen | 1.00 |
Nt-proBNP: N-terminal prohormone brain natriuretic peptide
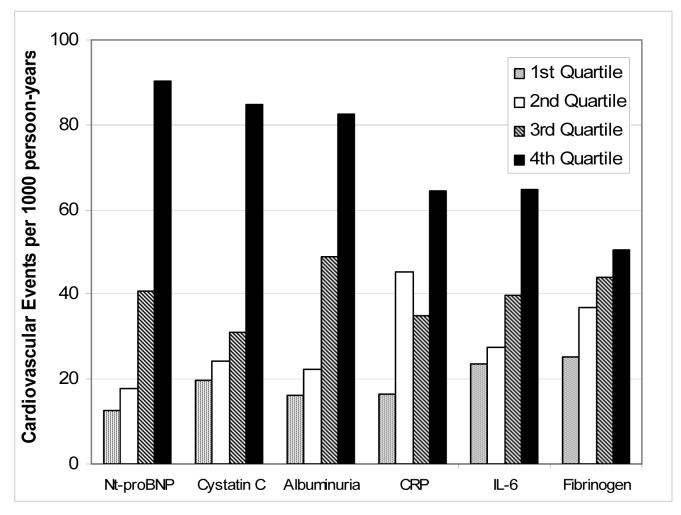
Individual biomarkers and Event risk
Quartiles of Nt-proBNP (>459pg/ml), cystatin C (>1.3mg/L), albuminuria (>19.5mg/g), CRP (>4.93mg/L), and IL-6 (>4.2mg/L) had greater risk differences from high to low quartile than fibrinogen (>443mg/dL) (Figure 1). In unadjusted models, each biomarker had strong associations with the outcome either as a linear variable or dichotomized (Table 3). In multivariate analyses, each biomarker was a linear predictor of the outcome. Nt-proBNP had the strongest association and fibrinogen the weakest. When dichotomized at the high quartile (vs. the lower 3 quartiles), each biomarker, except for fibrinogen, was an independent predictor of the outcome. When using clinical cutpoints, we found a similar association of Nt-proBNP with the outcome (hazard ratio (HR): 2.25 (1.46 - 3.48)); a somewhat stronger association of albuminuria with the higher threshold (2.25 (1.45 - 3.50)); and, a weaker association of CRP with the lower threshold (1.24 (0.85 - 1.80)).
Figure 1. Cardiovascular events incidence rates across biomarker quartiles.
Cardiovascular events incidence rates per 1000 person-years across quartiles of Nt-proBNP, cystatin C, albuminuria, CRP, IL-6 and fibrinogen.
Table 3.
Association of individual biomarkers with recurrent cardiovascular events among persons with coronary artery disease
| Linear Analysis (per SD)* | High Quartile vs. Lower Three Quartiles† | |||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Nt-proBNP | ||||
| Unadjusted | 2.13 (1.82 - 2.51) | <0.001 | 3.81 (2.73 - 5.30) | <0.001 |
| Adjusted‡ | 1.67 (1.35 - 2.06) | <0.001 | 2.13 (1.43 - 3.18) | <0.001 |
| Cystatin C | ||||
| Unadjusted | 1.59 (1.42 - 1.78) | <0.001 | 3.16 (2.27 - 4.39) | <0.001 |
| Adjusted‡ | 1.54 (1.32 - 1.80) | <0.001 | 1.72 (1.10 - 2.70) | 0.02 |
| Albuminuria | ||||
| Unadjusted | 1.59 (1.39 - 1.81) | <0.001 | 2.87 (1.90 - 4.34) | <0.001 |
| Adjusted‡ | 1.39 (1.18 - 1.63) | <0.001 | 1.71 (1.15 - 2.54) | 0.008 |
| C-Reactive Protein | ||||
| Unadjusted | 1.58 (1.33 - 1.87) | <0.001 | 2.58 (1.80 - 3.69) | <0.001 |
| Adjusted‡ | 1.52 (1.26 - 1.82) | <0.001 | 2.00 (1.40 - 2.85) | <0.001 |
| Interleukin – 6 | ||||
| Unadjusted | 1.77 (1.50 - 2.10) | <0.001 | 2.39 (1.72 - 3.34) | <0.001 |
| Adjusted‡ | 1.55 (1.28 - 1.87) | <0.001 | 1.76 (1.22 - 2.53) | 0.003 |
| Fibrinogen | ||||
| Unadjusted | 1.44 (1.21 - 1.71) | <0.001 | 1.50 (1.05 - 2.15) | 0.03 |
| Adjusted‡ | 1.26 (1.04 - 1.52) | 0.02 | 1.15 (0.78 - 1.69) | 0.48 |
Nt-proBNP: N-terminal prohormone brain natriuretic peptide
Linear analysis performed using log transformed concentrations of biomarkers
Cutpoints for high quartiles are as follows: Nt-proBNP >459pg/ml; cystatin C >1.3mg/L; albuminuria >19.5mg/g; CRP >4.93mg/L; IL-6 > 4.2mg/L; and fibrinogen >443mg/dL.
Adjusted for age, sex, race, diabetes, BMI, current smoking, prior myocardial infarction, cerebrovascular accident, chronic heart failure, ejection fraction <50, hypertension, creatinine and acetylsalicylic acid use
Biomarkers in combination
In a backward selection model, Nt-proBNP, albuminuria and CRP emerged as independent predictors of the outcome (Table 4). Because of the overlap between albuminuria and cystatin C and between CRP and IL-6, we interchanged these pairs in the final model. When replacing albuminuria, cystatin C had slightly weaker associations than albuminuria - 1.21 (95% CI 1.01-1.45, p<0.04) per standard deviation and 1.48 (95%CI 1.00-2.19, p<0.05) for the high quartile. Interleukin-6, replacing CRP, had very similar associations with CRP – 1.34 (95%CI 1.09-1.63, p<0.05) per standard deviation and 1.53 (95%CI 1.05 – 2.23, p<0.03) for the high quartile.
Table 4.
Biomarkers independently associated with recurrent cardiovascular events (N=786)
| Linear Analysis (per SD)* | High Quartile | |||
|---|---|---|---|---|
| Adjusted HR† | Adjusted HR† | |||
| (95% CI) | p-value | (95% CI) | p-value | |
| Nt-proBNP | 1.44 (1.15 - 1.80) | 0.002 | 1.88 (1.23 - 2.85) | 0.003 |
| Albuminuria | 1.26 (1.06 - 1.49) | 0.008 | 1.63 (1.09 - 2.43) | 0.02 |
| C-Reactive Protein | 1.37 (1.13 - 1.67) | 0.002 | 1.82 (1.24 - 2.67) | 0.002 |
Nt-proBNP: N-terminal prohormone brain natriuretic peptide
Linear analysis performed using log transformed concentrations of biomarkers
Adjusted for age, sex, race, diabetes, BMI, current smoking, prior myocardial infarction, cerebrovascular accident, chronic heart failure, ejection fraction <50, hypertension, creatinine and acetylsalicylic acid use, Nt-proBNP, albuminuria, and C reactive protein
To evaluate the incremental effect of the three significant biomarkers (Nt-proBNP, albuminuria, and CRP) on discrimination of risk for recurrent cardiovascular events, we compared the ROC curves for the standard clinical model with the same model including the three biomarkers (Figure 2). The AUC increased significantly from 0.73 (95 % CI, 0.68-0.78) for the standard clinical model to 0.77 (95% CI, 0.73-0.82) for the biomarkers (p<0.005).
Figure 2.
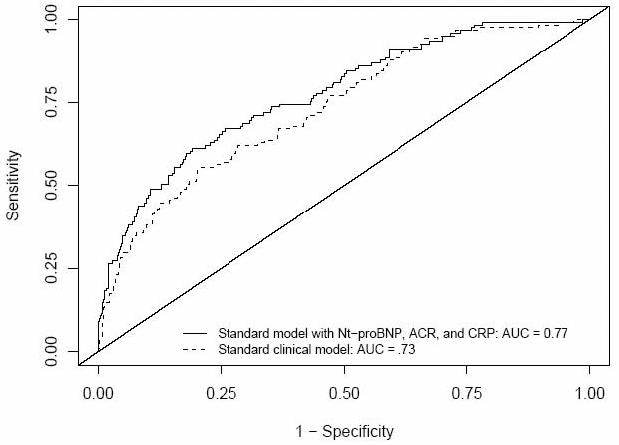
Receiver operator characteristic curves for the standard clinical model (dashed line) and for the standard clinical model plus Nt-proBNP, albuminuria and CRP (solid line).
Discussion
In this study among persons with prevalent coronary artery disease, we found that five biomarkers – Nt-proBNP, cystatin C, albuminuria, CRP and IL-6 were significant predictors of cardiovascular events beyond standard clinical information. After simultaneous adjustment for all five of these biomarkers, Nt-proBNP, albuminuria and CRP emerged as independent predictors of cardiovascular events. Collectively, these biomarkers added a moderate but statistically significant improvement in discrimination of cardiovascular risk, as evidenced by the AUC of the ROC curve increasing from 0.73 to 0.77. These results suggest that markers of hemodynamic stress, kidney damage and inflammation can augment risk prediction in persons with coronary artery disease.
Our findings complement and extend the prior literature on risk prediction among persons with coronary artery disease. In a study among 2,763 women with stable coronary artery disease enrolled in the Heart and Estrogen Protection Study (HERS), Vittinghoff and colleagues determined the most important predictors of MI and coronary heart disease death over 7 years of follow-up. They found coronary artery disease severity (angina symptoms, number of myocardial infarctions and heart failure history) and kidney dysfunction (estimated creatinine clearance <40 ml/min) to be as important predictors of recurrent events as the traditional cardiovascular risk factors, diabetes, hypertension and abnormal lipoprotein levels.2
Blankenberg and colleagues evaluated nine inflammatory biomarkers (C-reactive protein, fibrinogen, and interleukin-6, soluble tumor necrosis factor receptor-1 and -2, soluble interleukin-1 receptor antagonist, interleukin-18, soluble vascular adhesion molecule-1, soluble intercellular adhesion molecule-1,microalbuminuria, and Nt-proBNP) in an analysis from the Heart Outcomes Prevention Evaluation (HOPE) trial; the analysis included 3,199 persons (77% men) with either prevalent cardiovascular disease or diabetes and utilized the same composite outcome as our study with a follow-up interval of 4.5 years. Although soluble interleukin receptor antagonist, fibrinogen, soluble intracellular adhesion molecule -1 and Nt-proBNP were independent predictors in the final model, only Nt-proBNP significantly improved the AUC of the ROC curve (0.65 to 0.69).15 Although the AUC of the clinical model was lower in the Blankenberg paper than in our analysis – perhaps because the model did not include coronary heart disease severity or ejection fraction – both ROC curves improved by 0.04 (4% of the area under the curve) with the addition of biomarkers. Similarly, Rothenbacher and colleagues evaluated a cohort of 1,051 patients with recent acute coronary syndrome (85% men) over a four-year follow-up for the same outcome; the authors found Nt-proBNP, CRP, and creatinine to predict the outcome, but that only Nt-proBNP improved the AUC of the ROC curve (0.69 to 0.71).16
Interestingly, the three predominant biomarkers in this study represent unique pathologic mechanisms - hemodynamic stress, kidney damage, and inflammation. Incorporating these disparate biomarkers into a “multi-marker strategy” has been discussed in the setting of acute coronary syndrome, where clinical management is predominately determined by prognosis.17 Morrow and Braunwald suggested that an ideal scheme for risk stratification in patients with acute coronary syndrome might combine the traditional risk factors known to promote atherosclerosis (hyperglycemia, dyslipidemia, e.g.) with measures of inflammation (CRP, IL-6, e.g.) myocyte necrosis (troponins), hemodynamic stress (BNP or Nt-pro-BNP), and renal dysfunction/vascular damage (creatinine, microalbuminuria).17 Our study suggests that a similar paradigm may be appropriate to represent risk for recurrent cardiovascular disease in the outpatient setting.
Although these biomarkers provided moderate improvement in the global risk prediction in the secondary prevention setting, the clinical importance of this increased discriminatory capacity is unknown and its effect on patient management requires further study. Greater prognostic information among persons with coronary artery disease could be useful in evaluating the risk/benefit tradeoff of possible intervention strategies, for counseling patients about their prognosis, and for making decisions about non-cardiovascular prevention strategies, such as cancer screening. The presence of elevated Nt-proBNP levels might lead to earlier initiation of angiotensin converting enzyme inhibitors and beta blockers, but the potential benefits of screening with Nt-proBNP have not been studied. Kidney damage detected by either increased albuminuria or cystatin C might trigger the use of RAA inhibitors or more aggressive systolic blood pressure control, but such a strategy has not been evaluated. Inflammatory biomarkers like CRP, IL-6, have been consistently predictive of cardiovascular outcomes, but may not be modifiable in either primary or secondary prevention settings.
This study should be interpreted in the context of certain limitations. The cohort is predominately male, so our findings cannot necessarily be generalized to women. We measured six biomarkers in this study but there may be others with greater predictive value for recurrent cardiovascular events. Since these biomarkers were only measured upon entry into the Heart and Soul cohort, we do not know their levels at the time of their recurrent event.
In conclusion, we found that biomarkers reflective of hemodynamic stress, kidney disease and inflammation added moderate but significant discrimination for recurrent cardiovascular events beyond readily available clinical information. Future studies should evaluate whether these or other biomarkers will have clinical utility for the management of patients with established coronary artery disease.
Acknowledgements
Dr. Shlipak was funded by the American Federation for Aging Research and National Institute on Aging (Paul Beeson Scholars Program), the Robert Wood Johnson Foundation (Generalist Faculty Scholars Program), and by R01 DK066488. The Heart and Soul Study was supported by grants from the Department of Veterans Affairs (Epidemiology Merit Review Program), the Robert Wood Johnson Foundation (Generalist Physician Faculty Scholars Program), the American Federation for Aging Research (Paul Beeson Faculty Scholars Program), the Ischemia Research and Education Foundation, and the Nancy Kirwan Heart Research Fund. Dade Behring, Inc paid for the cystatin C measurements. Roche Diagnostics paid for the Nt-proBNP assays.
Footnotes
Clinical Significance
- Among stable outpatients with coronary artery disease, the risk factors for recurrent cardiovascular events have not been well characterized.
- Independent of demographic characteristics, cardiovascular risk factors and disease status, and left ventricular ejection fraction, Nt-proBNP, albuminuria and C-reactive protein were associated with increased risk for cardiovascular disease events.
- Biomarkers reflecting hemodynamic stress, kidney damage, and inflammation add significant risk discrimination for recurrent cardiovascular events.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sabatine MS, Morrow DA, de Lemos JA, et al. Multimarker approach to risk stratification in non-ST elevation acute coronary syndromes: simultaneous assessment of troponin I, C-reactive protein, and B-type natriuretic peptide. Circulation. 2002 Apr 16;105(15):1760–1763. doi: 10.1161/01.cir.0000015464.18023.0a. [DOI] [PubMed] [Google Scholar]
- 2.Vittinghoff E, Shlipak MG, Varosy PD, et al. Risk factors and secondary prevention in women with heart disease: the Heart and Estrogen/progestin Replacement Study. Ann Intern Med. 2003 Jan 21;138(2):81–89. doi: 10.7326/0003-4819-138-2-200301210-00007. [DOI] [PubMed] [Google Scholar]
- 3.Ix JH, Shlipak MG, Liu HH, et al. Association between renal insufficiency and inducible ischemia in patients with coronary artery disease: the heart and soul study. J Am Soc Nephrol. 2003 Dec;14(12):3233–3238. doi: 10.1097/01.asn.0000095642.25603.7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruo B, Rumsfeld JS, Hlatky MA, et al. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003 Jul 9;290(2):215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erlandsen EJ, Randers E, Kristensen JH. Evaluation of the Dade Behring N Latex Cystatin C assay on the Dade Behring Nephelometer II System. Scand J Clin Lab Invest. 1999 Feb;59(1):1–8. doi: 10.1080/00365519950185940. [DOI] [PubMed] [Google Scholar]
- 6.Beattie MS, Shlipak MG, Liu H, et al. C-reactive protein and ischemia in users and nonusers of beta-blockers and statins: data from the Heart and Soul Study. Circulation. 2003 Jan 21;107(2):245–250. doi: 10.1161/01.cir.0000044387.23578.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ix JH, Shlipak MG, Brandenburg VM, et al. Association Between Human Fetuin-A and the Metabolic Syndrome. Data From the Heart and Soul Study. Circulation. 2006 Mar 27; doi: 10.1161/CIRCULATIONAHA.105.588723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ix JH, Chertow GM, Shlipak MG, et al. Fetuin-A and kidney function in persons with coronary artery disease--data from the heart and soul study. Nephrol Dial Transplant. 2006 Aug;21(8):2144–2151. doi: 10.1093/ndt/gfl204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003 Nov 18;108(20):2543–2549. doi: 10.1161/01.CIR.0000100560.46946.EA. [DOI] [PubMed] [Google Scholar]
- 10.Angeja BG, Shlipak MG, Go AS, et al. Hormone therapy and the risk of stroke after acute myocardial infarction in postmenopausal women. J Am Coll Cardiol. 2001 Nov 1;38(5):1297–1301. doi: 10.1016/s0735-1097(01)01551-0. [DOI] [PubMed] [Google Scholar]
- 11.Bibbins-Domingo K, Gupta R, Na B, et al. N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. JAMA. 2007 Jan 10;297(2):169–176. doi: 10.1001/jama.297.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007 Jan 16;115(2):173–179. doi: 10.1161/CIRCULATIONAHA.106.644286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McManus D, Shlipak M, Ix JH, et al. Association of cystatin C with poor exercise capacity and heart rate recovery: data from the heart and soul study. Am J Kidney Dis. 2007 Mar;49(3):365–372. doi: 10.1053/j.ajkd.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pepe MS, Janes H, Longton G, et al. Limitations of the Odds Ratio in Gauging the Performance of a Diagnostic,Prognostic, or Screening Marker. American Journal of Epidemiology. 2004;159(9):882–890. doi: 10.1093/aje/kwh101. [DOI] [PubMed] [Google Scholar]
- 15.Blankenberg S, McQueen MJ, Smieja M, et al. Comparative impact of multiple biomarkers and N-Terminal pro-brain natriuretic peptide in the context of conventional risk factors for the prediction of recurrent cardiovascular events in the Heart Outcomes Prevention Evaluation (HOPE) Study. Circulation. 2006 Jul 18;114(3):201–208. doi: 10.1161/CIRCULATIONAHA.105.590927. [DOI] [PubMed] [Google Scholar]
- 16.Rothenbacher D, Koenig W, Brenner H. Comparison of N-terminal pro-B-natriuretic peptide, C-reactive protein, and creatinine clearance for prognosis in patients with known coronary heart disease. Arch Intern Med. 2006 Dec 11-25;166(22):2455–2460. doi: 10.1001/archinte.166.22.2455. [DOI] [PubMed] [Google Scholar]
- 17.Morrow DA, Braunwald E. Future of biomarkers in acute coronary syndromes: moving toward a multimarker strategy. Circulation. 2003 Jul 22;108(3):250–252. doi: 10.1161/01.CIR.0000078080.37974.D2. [DOI] [PubMed] [Google Scholar]