Abstract
Background and purpose:
5-lipoxygenase (5-LO) is the key enzyme in leukotriene (LT) biosynthesis from arachidonic acid (AA). Here, we examined the role of the 5-LO-product, cysteinyl-LT (Cys-LT), with a 5-LO inhibitor (zileuton) and a Cys-LT, receptor antagonist (montelukast), in the inflammatory response and tissue injury associated with spinal cord injury (SCI).
Experimental approach:
SCI was induced in mice by the application of vascular clips to the dura via a two-level T6 to T7 laminectomy for 1 min. Cord inflammation was assessed histologically and by measuring inflammatory mediators (ELISA) and apoptosis by annexin V, TUNEL, Fas ligand staining and Bax and Bcl-2 expression (immunohistochemistry and western blots). Motor function in hindlimbs was assessed by a locomotor rating scale, for 10 days after cord injury.
Key results:
SCI in mice resulted in tissue damage, oedema, neutrophil infiltration, apoptosis, tumour necrosis-α (TNF-α) and cyclooxygenase-2 (COX-2) expression, prostaglandin E2 (PGE2) and leukotriene B4 (LTB4) production, and extracellular signal-regulated kinase 1/2 (ERK1/2) phosphorylation in injured tissue. Treatment of the mice with zileuton or montelukast reduced the spinal cord inflammation and tissue injury, neutrophil infiltration, TNF-α, COX-2 and pERK1/2 expression, PGE2 and LTB4 production, and apoptosis. In separate experiments, zileuton or montelukast significantly improved the recovery of limb function over 10 days.
Conclusions and implications:
Zileuton and montelukast produced a substantial reduction of inflammatory events associated with experimental SCI. Our data underline the important role of 5-LO and Cys-LT in neurotrauma.
Keywords: zileuton, montelukast, spinal cord injury, 5-lipoxygenase, cysteinyl-leukotrienes
Introduction
Traumatic spinal cord injury (SCI) is an unexpected, catastrophic event, the consequences of which often persists for the life of the patient and influences not only the patient but also family members and society (Stover and Fine, 1987). It is known that SCI initiates a cascade of cellular and molecular events (Tator, 1995; Xu et al., 2001; Hausmann, 2003; Beattie, 2004; Gris et al., 2004) and that a progressive neuronal injury results from a combination of secondary injury factors, including ischaemia, biochemical alterations, apoptosis, excitotoxicity, neurotransmitter accumulation and lipid peroxidation/free radical injury (Carlson and Gorden, 2002). It is believed that inflammatory and immune responses are the major component of secondary injury and play a central role in regulating the pathogenesis of acute and chronic SCI (Anderson, 2002; Bethea and Dietrich, 2002; Yang et al., 2004). Studies, mostly carried out in vitro, have disclosed a series of events related to the occurrence of neuronal damage following SCI: mitogen-activated protein kinase (MAPK) activation, initiation of inflammatory responses (liberation of pro-inflammatory mediators, such as nitric oxide, tumour necrosis factor-α (TNF-α), prostaglandins (PGs) and leukotrienes (LTs)) and degeneration of neurons. In particular, it has been reported that phosphorylation of extracellular signal-regulated kinase 1/2 (ERK1/2) results in expression of genes mediating the inflammatory responses, such as those encoding for TNF-α and cyclooxygenase-2 (COX-2) (Jung et al., 2005). Moreover, although the mechanisms are not fully understood, inflammatory responses leading to endothelial damage may be involved in the secondary injury process (Demopoulos et al., 1978; Hamada et al., 1996; Taoka et al., 1997). In fact, neutrophils are the first leucocytes to arrive within the injured spinal cord (Carlson et al., 1998; McTigue et al., 1998) and can cause endothelial cell injury through the liberation of several inflammatory mediators (Xu et al., 1990), such as cytokines (Profyris et al., 2004), nitric oxide (Dietrich et al., 2004), COX-2 (Adachi et al., 2005) and 5-lipoxygenase (5-LO) metabolites (Suttorp et al., 1987; Xu et al., 1990; Mitsuhashi et al., 1994). In particular, it has been demonstrated that neutrophil infiltration in SCI is proportional to both the magnitude of trauma and the amount of leukotriene B4 (LTB4), a product of 5-LO (Suttorp et al., 1987; Xu et al., 1990). An enhanced synthesis of leukotriene C4 (LTC4) in the injured spinal cord has also been reported (Mitsuhashi et al., 1994; Nishisho et al., 1996). For example, in the canine model, a significant increase in LTC4 levels was observed and there was a good correlation between levels of LTC4 in cerebrospinal fluid and the severity of neurological damage. Moreover, the time-dependent change in LTC4 concentrations in seven patients with SCI was similar to that observed in the canine model (Nishisho et al., 1996). Other 5-LO products are also involved in SCI, as 5-hydroxyeicosatetraenoic acid levels increase after experimental SCI in rabbits and it has been hypothesized that this increase may be involved in the pathophysiology of spinal cord trauma (Jacobs et al., 1987; Shohami et al., 1987).
One of the reasons why most of the treatments utilized in preclinical studies (Leker and Shohami, 2002) have had limited success in clinical trials is because of the complexity of the secondary degenerative response. In fact, many treatments affect only one aspect of this response, and a successful treatment will probably have to target several of these mechanisms (King et al., 2006). A number of experimental animal models have been developed to simulate the pathophysiology of acute clinical spinal cord compression in humans (Beattie et al., 2002). The most commonly used model is the compression model; in this model, injury is induced by applying either a weight or an aneurysm clip to the spinal cord (Tator and Fehlings, 1991). This experimental procedure is closer to the human situation in respect to the contusion model, since it replicates the persistence of cord compression that is commonly observed in human SCI (Tator, 1995). We have demonstrated in the compression model, by the use of 5-LO knockout mice, that the absence of this enzyme caused a substantial reduction of inflammatory events characteristic of SCI (Genovese et al., 2005). As suppression of enzyme activity by gene deletion can give rise to compensatory mechanisms, we decided to investigate the role of 5-LO products using the same model of SCI. In particular, we examined cysteinyl-LTs (Cys-LTs) with a 5-LO inhibitor (zileuton) and a Cys-LT1 receptor antagonist (montelukast).
Methods
Animals
Animal care was in compliance with Italian regulations on protection of animals used for experimental and other scientific purpose (Ministerial Decree 116192) as well as with the European Economic Community regulations (Official Journal of E.C. L 358/1 12/18/1986). Male adult CD1 mice (25–30 g, Harlan Nossan, Milan, Italy) were housed in a controlled environment and provided with standard rodent chow and water.
Spinal cord injury
Mice were anaesthetized using chloral hydrate (40 μg kg−1 body weight). A longitudinal incision was made on the midline of the back, exposing the paravertebral muscles. These muscles were dissected away, exposing T5–T8 vertebrae. The spinal cord was exposed via a two-level T6–T7 laminectomy, and SCI was produced by extradural compression of the spinal cord using an aneurysm clip with a closing force of 24 g. In all of the injured groups, the spinal cord was compressed for 1 min. Sham-injured animals were only subjected to laminectomy.
After surgery, 1 ml of saline was administered subcutaneously to replace the blood volume lost during the surgery. During recovery from anaesthesia, the mice were placed on a warm heating pad and covered with a warm towel. The mice were singly housed in a temperature-controlled room at 27 °C for a survival period of 10 days. Food and water were provided to the mice ad libitum. During this period, the bladders of the animals were manually voided twice a day until the mice were able to regain normal bladder function.
Experimental groups
Mice were randomly allocated into the following groups: (1) SCI+vehicle (saline solution), subjected to SCI and given vehicle i.p. 1 h and 6 h after injury (n=50 mice, Table 1); (2) SCI+zileuton, subjected to SCI and given zileuton (50 mg kg−1 weight in saline solution p.o) 1 h and 6 h after injury (n=50 mice, Table 1); (3) SCI+montelukast, subjected to SCI and given montelukast (5 mg kg−1 weight in saline i.p.) 1 and 6 h after injury (n=50 mice, Table 1); (4) sham+vehicle, subjected to a T6–T7 laminectomy and given vehicle i.p. 1 and 6 h after laminectomy (n=50 mice, Table 1); (5) sham+zileuton, subjected to a T6–T7 laminectomy and given zileuton (50 mg kg−1, p.o.) 1 and 6 h after laminectomy (n=50mice, Table 1) and (6) sham+montelukast, subjected to a T6–T7 laminectomy and given montelukast (5 mg kg−1, i.p.) 1 h and 6 h after laminectomy (n=50mice, Table 1). In the experiments measuring motor function, the animals were treated with drugs 1 and 6 h after SCI daily until day 9.
Table 1.
Number of animals used in the different experiments
| Animal number (n) | Experiment type |
|---|---|
| 10 | Histological examination, immunohistochemical localization of MPO, TNF-α, Bax, Bcl-2 and FAS ligand, Annexin-V evaluation and TUNEL assay. |
| 10 | Myeloperoxidase activity |
| 10 | Measurement of TNF-α |
| 10 | Western blot analysis for Bax, Bcl-2, COX-2, pERK-1/2, ERK-2 and β-actin |
| 10 | Motor function |
| 10 | Measurement of PGE2 and LTB4 |
Abbreviation: ERK, extracellular signal-regulated kinase; LTB4, leukotriene B4; MPO, myeloperoxidase; PGE2, prostaglandin E2; TNF-α, tumour necrosis-α; TUNEL, terminal deoxynucleotidyltransferase-mediated UTP end labelling.
At different time points, the animals (n=10 mice from each group for each time point) were killed in order to evaluate the various parameters described below.
The dose of zileuton (50 mg kg−1) was chosen according to our earlier studies (Failla et al., 2006; Mazzon et al., 2006), while the selected dose of montelukast (5 mg kg−1) was chosen on the basis of published data (Saito et al., 2004; Lee et al., 2007).
Histological examination
Spinal cord biopsies were taken at 24 h following trauma. Tissue segments containing the lesion (1 cm on each side of the lesion) were paraffin embedded and cut into 5-μm-thick longitudinal sections. The tissue sections were deparaffinized with xylene, stained with haematoxylin/eosin and examined by light microscopy (Dialux 22 Leitz). The segments of each spinal cord were evaluated by an experienced histopathologist and all the histological studies were performed without knowledge of the treatments.
Grading of motor disturbance
The motor function of mice subjected to compression trauma was assessed once a day for 10 days after injury. Recovery from motor disturbance was graded using the modified murine Basso, Beattie and Bresnahan (BBB) (Basso et al., 1995) hindlimb locomotor-rating scale (Joshi and Fehlings, 2002a, 2002b). The following criteria were considered: 0=no hindlimb movement; 1=slight (<50% range of motion) movement of one to two joints; 2=extensive (>50% range of motion) movement of one joint and slight movement of one other joint; 3=extensive movement of two joints; 4=slight movement in all three joints; 5=slight movement of two joints and extensive movement of one joint; 6=extensive movement of two joints and slight movement of one joint; 7=extensive movement of all three joints; 8=sweeping without weight support or plantar placement and no weight support; 9=plantar placement with weight support in stance only or dorsal stepping with weight support; 10=occasional (0–50% of the time) weight-supported plantar steps and no coordination (front/hindlimb coordination); 11=frequent (50–94% of the time) to consistent (95–100% of the time) weight-supported plantar steps and no coordination; 12=frequent to consistent weight-supported plantar steps and occasional coordination; 13=frequent to consistent weight-supported plantar steps and frequent coordination; 14=consistent weight-supported plantar steps, consistent coordination and predominant paw position is rotated during locomotion (lift off and contact) or frequent plantar stepping, consistent coordination and occasional dorsal stepping; 15=consistent plantar stepping and coordination, no/occasional toe clearance, paw position is parallel at initial contact; 16=consistent plantar stepping and coordination (front/hindlimb coordination) and frequent toe clearance and predominant paw position is parallel at initial contact and rotated at lift off; 17=consistent plantar stepping and coordination and frequent toe clearance and predominant paw position is parallel at initial contact and lift off; 18=consistent plantar stepping and coordination and consistent toe clearance and predominant paw position is parallel at initial contact and rotated at lift off; 19=consistent plantar stepping and coordination and consistent toe clearance and predominant paw position is parallel at initial contact and lift off; 20=consistent plantar stepping, coordinated gait, consistent toe clearance, predominant paw position is parallel at initial contact and lift off and trunk instability; 21=consistent plantar stepping, coordinated gait, consistent toe clearance, predominant paw position is parallel at initial contact and lift off and trunk stability.
Myeloperoxidase activity
Myeloperoxidase (MPO) activity, an indicator of polymorphonuclear leucocyte (PMN) accumulation, was determined as previously described (Mullane et al., 1985) 24 h after SCI. This time was chosen in agreement with other studies (Hamada et al., 1996). At the specified time following SCI, spinal cord tissues were obtained and weighed and each piece homogenized in a solution containing 0.5% (w/v) hexadecyltrimethyl-ammonium bromide dissolved in 10 mM potassium phosphate buffer (pH 7) and centrifuged for 30 min at 20 000 g at 4 °C. An aliquot of the supernatant was then allowed to react with a solution of 1.6 mM tetramethylbenzidine and 0.1 mM H2O2. The rate of change in absorbance was measured spectrophotometrically at 650 nm. MPO activity was defined as the quantity of enzyme degrading 1 μmol of peroxide min−1 at 37 °C and was expressed in U g−1 of wet tissue.
Immunohistochemical localization of MPO, TNF-α, Bax, Bcl-2 and FAS ligand
At 24 h after SCI, the tissues were fixed in 10% (w/v) phosphate-buffered saline (PBS)-buffered formaldehyde and 8 μm sections were prepared from paraffin-embedded tissues. After deparaffinization, endogenous peroxidase was quenched with 0.3% (v/v) hydrogen peroxide in 60% (v/v) methanol for 30 min. The sections were permeabilized with 0.1% (w/v) Triton X-100 in PBS for 20 min. Nonspecific adsorption was minimized by incubating the section in 2% (v/v) normal goat serum in PBS for 20 min. Endogenous biotin or avidin binding sites were blocked by sequential incubation for 15 min with biotin and avidin, respectively. Sections were incubated overnight with anti-MPO, anti-TNF-α, anti-Bax or anti-FAS ligand rabbit polyclonal antibody, and anti-Bcl-2 polyclonal antibody rat (1:500 in PBS, v/v). Sections were washed with PBS and incubated with secondary antibody. Specific labelling was detected with a biotin-conjugated goat anti-rabbit IgG and avidin-biotin peroxidase complex. To verify the binding specificity for MPO, TNF-α, Bax, Bcl-2 and FAS ligand, some sections were also incubated with only the primary antibody (no secondary) or with only the secondary antibody (no primary). In these situations, no positive staining was found in the sections, indicating that the immunoreactions were positive in all of the experiments carried out.
Immunohistochemical photographs (n=5 photos from each sample collected from each mice in each experimental group) were assessed by densitometry as described previously (Shea, 1994) by using Optilab Graftek software on a Macintosh personal computer.
Measurement of TNF-α
Portions of spinal cord tissues, collected at 24 h after SCI, were homogenized as previously described in PBS containing 2 mM of phenylmethyl sulphonyl fluoride to evaluate TNF-α tissue levels. The assay was carried out by using a colorimetric, commercial kit (Calbiochem-Novabiochem Corporation, CA, USA) according to the manufacturer's instructions. All TNFα determinations were performed in duplicate serial dilutions.
Annexin-V evaluation
The binding of annexin-V fluorescein isothiocyanate (FITC) (Ann-V) to externalized phosphatidylserine was used as a measurement of apoptosis in spinal cord tissue section with an Ann-V-propidium iodide (PI) apoptosis detection kit (Santa Cruz, DBA, Milan, Italy) according to the manufacturer's instructions. Briefly, normal viable cells in culture will stain negative for annexin-V FITC and negative for PI. Cells induced to undergo apoptosis will stain positive for annexin-V FITC and negative for PI as early as 1 h after stimulation (Schutte et al., 1998). Cells in later stages of apoptosis and necrotic cells will both stain positive for annexin-V FITC and PI. Sections were washed as before, mounted with 90% glycerol in PBS, and observed with an LSM 510 Zeiss laser confocal microscope equipped with a × 40 oil objective.
Terminal deoxynucleotidyltransferase-mediated UTP end labelling assay
These assays were conducted using a terminal deoxynucleotidyltransferase-mediated UTP end labelling assay (TUNEL) detection kit according to the manufacturer's instruction (Apotag, HRP kit; DBA srl). In brief, sections were incubated with 15 μg ml−1 proteinase K for 15 min at room temperature and then washed with PBS. Endogenous peroxidase was inactivated by 3% H2O2 for 5 min at room temperature and then washed with PBS. Sections were immersed in TdT buffer containing deoxynucleotidyl transferase and biotinylated deoxyuridine triphosphate in TdT buffer, incubated in a humid atmosphere at 37 °C for 90 min, and then washed with PBS. The sections were incubated at room temperature for 30 min with anti-horseradish peroxidase-conjugated antibody, and the signals were visualized with diaminobenzidine.
Total protein extraction and western blot analysis for Bax, Bcl-2, COX-2, pERK-1/2, ERK-2 and β-actin
Tissue samples from SCI-injured animals (n=10) after 24 h were homogenized in a buffer containing 20 mM HEPES pH 7.6, 1.5 mM MgCl2, 400 mM NaCl, 1 mM EDTA, 1 mM EGTA, 1 mM dithiothreitol, 0.5 mM phenylmethylsulfonyl fluoride, 15 μg ml−1 trypsin inhibitor, 3 μg ml−1 pepstatin, 2 μg ml−1 leupeptin, 40 μM benzamidine, 1% Nonidet P-40, 20% glycerol and 50 mM NaF. The homogenates were centrifuged at 10 000 g for 15 min and at 4 °C, and the supernatant was collected and protein concentration was determined by Bio-Rad protein assay (Bio-Rad Laboratories GmbH, Munchen). Equal amounts of protein (50 μg) were mixed with gel loading buffer (50 mM Tris, 10% sodium dodecyl sulfate, 10% glycerol, 10% 2-mercaptoethanol and 2 mg ml−1 bromophenol) in a ratio of 1:1, boiled for 3 min and centrifuged at 10 000 g for 10 min. Each sample was loaded and electrophoresed on a 10% sodium dodecyl sulfate–polyacrylamide gel. The proteins were transferred on to nitrocellulose membranes. The membranes were blocked with 0.1% PBS-Tween containing 5% non-fat dry milk for ERK-2, Bax, Bcl-2, COX-2 and β-actin, whereas with 0.1% PBS-Tween containing 5% non-fat dry milk and 50 mM NaF for pERK-1/2. After the blocking, the membranes were incubated with the relative primary antibody overnight at 4 °C. Rabbit monoclonal antibodies, anti-Bax, anti-bcl2 (Santa Cruz Biotechnology) and anti-COX-2 (Upstate cell signalling solutions, New York), and mouse monoclonal antibodies, anti-ERK-2 (Santa Cruz Biotechnology), were diluted 1:1000 in 0.1% PBS-Tween, 5% non-fat dry milk; mouse monoclonal antibody anti-pERK1/2 (Santa Cruz Biotechnology) was diluted 1:1000 in 0.1% PBS-Tween, 5% non-fat dry milk, 50 mM NaF; mouse monoclonal antibody anti-β-actin (Sigma-Aldrich, Milan, Italy) was diluted 1:10 000 in 0.1% PBS-Tween, 5% BSA. After the incubation, the membranes were washed six times with 0.1% PBS-Tween and were incubated for 1.5 h at room temperature with horseradish peroxidase-conjugated anti-mouse secondary antibodies (Dako Cytomation, Denmark) diluted 1:1000 in 0.1% PBS-Tween containing 5% non-fat dry milk. The membranes were washed and protein bands were detected by an enhanced chemiluminescence system (Amersham Pharmacia, Amersham Biosciences, UK). Densitometric analysis was performed with a Fluor S quantitative imaging system (Bio-Rad Laboratories).
Determination of PGE2 and LTB4 levels in mouse spinal cords
The spinal cords were collected at 24 h after SCI from the animals (two to six spinal cords were pooled together) and immediately homogenized in methanol. The mediators in the tissues were extracted in 5 ml methanol for 3–5 days at −80 °C. To remove the tissue residues, the extracts were centrifuged at 1800 g for 20 min at 4 °C. Then the sample solutions were dried to remove methanol. The dried samples were suspended in an assay buffer that was supplied with each ELISA kit (Assay Designs). To determine the levels of PGE2 and LTB4 within the sensitive (that is, linear) ranges of the standard curves, the samples were diluted a further 1- to 20-fold and assayed at multiple dilutions (Marusic et al., 2005).
Statistical procedures
All values in the figures are expressed as mean±s.e.mean of n observations. For the in vivo studies, n represents the number of animals studied. In the experiments involving histology or immunohistochemistry, the figures shown are representative at least three experiments (histological or immunohistochemical staining) performed on different experimental days on the tissues section collected from all the animals in each group (n=10). The results were analysed by one-way ANOVA followed by a Bonferroni post hoc test for multiple comparisons; P<0.05 was considered significant. Basso, Beattie and Bresnahan scale data were analysed by the Mann–Whitney test and considered significant when P<0.05.
Drugs and chemical reagents
Zileuton and montelukast were obtained from Sequoia Research Products (Oxford, UK). Biotin and avidin were obtained from DBA (Milan, Italy). The antibodies against Bax, bcl2, pERK1/2 and ERK-2 were obtained from Santa Cruz Biotechnology Inc. (Milan, Italy). The antibody against COX-2 was from Upstate (NY). All other reagents and compounds used were obtained from Sigma-Aldrich.
Results
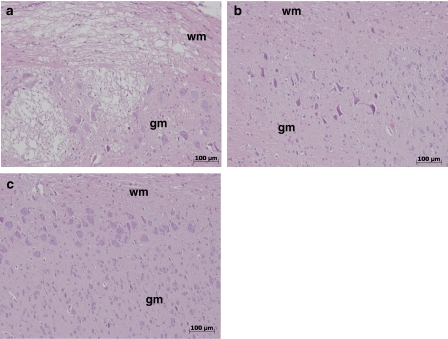
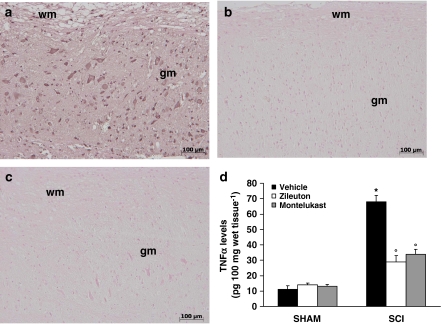
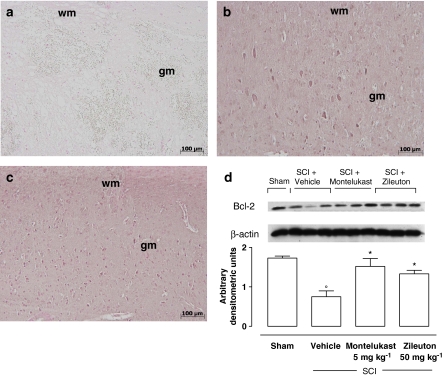
Effects of zileuton and montelukast on the severity of spinal cord trauma
Twenty-four hours after the trauma, there was significant damage to the spinal cord at the perilesional zone, as assessed by the presence of oedema, as well as an alteration of the white matter observed in SCI+vehicle-treated mice (Figure 1a) when compared with spinal cord tissue collected from sham+vehicle-treated mice. A significant protection of the SCI was observed in the tissue collected from SCI+zileuton-treated mice (50 mg kg−1 1 and 6 h after injury) (Figure 1b) or SCI+montelukast-treated-mice (5 mg kg−1 weight 1 and 6 h after injury) (Figure 1c).
Figure 1.
Effect of zileuton and montelukast on histological alterations of the spinal cord tissue 24 h after injury. (a) Twenty-four hours after trauma, a significant damage to the spinal cord from SCI+vehicle-treated mice at the perilesional area was assessed by the presence of oedema and alteration of the white matter. A significant protection from the SCI was observed in the tissue collected from SCI+zileuton (b) or montelukast-treated mice (c). This figure is representative of at least three experiments performed on different experimental days. wm, white matter; gm, grey matter. No histological alteration was observed in the spinal cord tissues from sham-operated mice (data not shown). SCI, spinal cord injury.
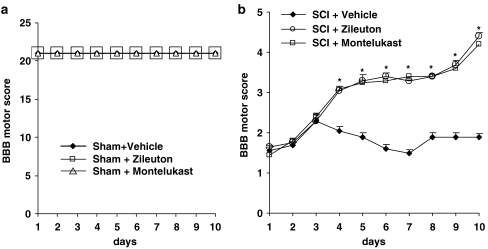
To evaluate whether histological damage to the spinal cord was associated with a loss of motor function, the modified Basso, Beattie and Bresnahan hindlimb locomotor-rating scale score was evaluated. Although motor function was only slightly impaired in sham mice groups (Figure 2a), SCI+vehicle-treated mice had significant deficits in hindlimb movement (Figure 2b). In contrast, a significant (P<0.001) amelioration of hindlimb motor disturbances was observed in SCI+zileuton-treated or montelukast-treated-mice (Figure 2b).
Figure 2.
Effect of zileuton and montelukast on hindlimb motor dysfunction after SCI. The degree of motor dysfunction of (a) Sham groups and (b) SCI groups was assessed every day for 10 days after SCI induction by Basso–Beattie–Bresnahan criteria (Basso et al., 1995). Treatment with zileuton or montelukast reduces the loss of motor function after SCI. Values shown are mean±s.e.mean of 10 mice for each group. *P<0.01 versus SCI+vehicle. SCI, spinal cord injury.
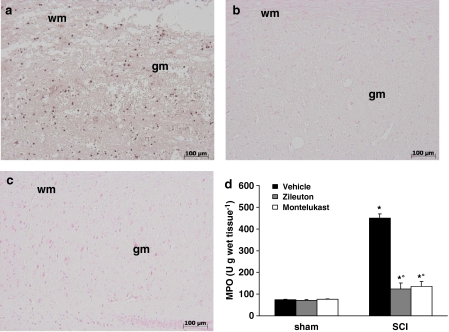
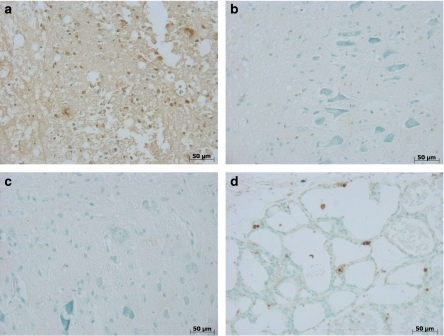
Effects of zileuton and montelukast on neutrophil infiltration
MPO activity was significantly (P<0.001) elevated at 24 h after SCI in vehicle-treated mice compared with spinal cord tissue collected from sham+vehicle-treated mice (Figure 3d). In zileuton- or montelukast-treated mice, spinal cord MPO activity, at 24 h, was significantly (P<0.001) attenuated compared with those of SCI+vehicle-treated animals. In addition, tissue sections obtained at 24 h from SCI+vehicle-treated mice demonstrated positive staining for MPO, mainly localized in the infiltrated inflammatory cells in the injured area (Figures 3a and 4). Moreover, in mice treated with zileuton (Figures 3b and 4) or montelukast (Figures 3c and 4), the staining for MPO was visibly reduced in comparison with that observed in SCI+vehicle-treated mice. There was no staining for MPO in spinal cord tissues obtained from the sham group of mice (data not shown).
Figure 3.
Effect of zileuton and montelukast on immunohistochemical localization and activity of MPO. A significant positive staining and a significant increase of MPO activity was observed in the spinal cord tissues collected from SCI+vehicle-treated mice (a, d). In mice treated with zileuton (b, d) or montelukast (c, d), the MPO staining and activity was visibly and significantly reduced in comparison with the SCI+vehicle-treated mice. No positive staining for MPO was observed in spinal cord tissues collected from sham-operated mice (data not shown). Image is representative of at least three experiments performed on different experimental days. Data are means±s.e.mean of 10 mice for each group. *P<0.01 versus sham-operated mice; °P<0.01 versus SCI+vehicle-treated mice. wm, white matter; gm, grey matter; MPO, myeloperoxidase; SCI, spinal cord injury.
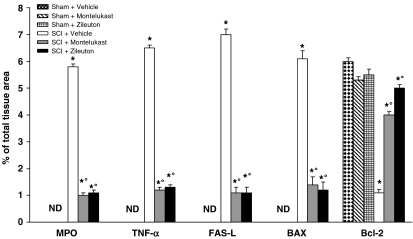
Figure 4.
Typical densitometry evaluation. Densitometry analysis of immunocytochemistry photographs (n=5 photos from each sample collected from all mice in each experimental group) for MPO, TNF-α, FAS-L, Bax and Bcl-2 from spinal cord tissues was assessed. The assay was carried out by using Optilab Graftek software on a Macintosh personal computer (CPU G3-266). Data are expressed as % of total tissue area. *P<0.01 versus Sham; °P<0.01 versus SCI. ND, not detectable; MPO, myeloperoxidase; SCI, spinal cord injury; TNF-α, tumour necrosis-α.
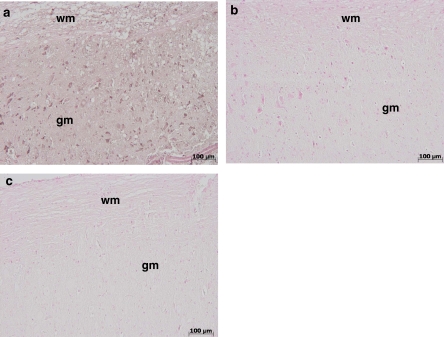
Effect of zileuton and montelukast on TNF-α levels
Immunohistological analysis of the spinal cord after SCI was performed to determine whether zileuton and montelukast may modulate the secondary inflammatory reaction also through the regulation of the secretion of cytokines, such as TNF-α. A substantial increase of TNF-α (Figures 4, 5a and d) formation was found in spinal cord samples collected from SCI+vehicle-treated mice at 24 h after SCI. Spinal cord levels of TNF-α were significantly attenuated in mice treated with zileuton or montelukast (Figures 4 and 5b–d). There was no staining for TNF-α in spinal cord obtained from sham groups of mice (data not shown).
Figure 5.
Effect of zileuton and montelukast on spinal cord levels and immunohistochemical localization of TNF-α. SCI caused, at 24 h, an increase in the release of TNF-α in spinal cord tissues (a, d). Treatment with zileuton (b, d) or montelukast (c, d) significantly inhibited the SCI-induced increase of TNF-α. No positive staining for TNF-α was observed in spinal cord tissues obtained from the sham group of mice (data not shown). Figure is representative of at least three experiments performed on different experimental days. wm, white matter; gm, grey matter. Data are means±s.e.mean of 10 mice for each group. *P<0.01 versus sham-operated mice; °P<0.01 versus SCI+vehicle-treated mice. SCI, spinal cord injury; TNF-α, tumour necrosis-α.
Effect of zileuton and montelukast on apoptosis in spinal cord tissue after injury
To test whether the tissue damage was associated with apoptotic cell death, we measured annexin V staining in the spinal cord tissues. Almost no apoptotic cells were detectable in the spinal cord tissue from sham groups of mice (data not shown). However, at 24 h after SCI, tissues obtained from SCI+vehicle-treated mice demonstrated a marked appearance of positive staining for annexin-V (Figure 6a), indicative of cells undergoing apoptosis. In addition, some cells showed a positive intracellular staining to PI, an index of cells in the late stage of apoptosis (Figure 6a1). On the contrary, spinal cord tissues section from mice treated with zileuton or montelukast demonstrated no cells in the earlier stage of apoptosis (Figures 6b and c, respectively) and a decreased presence of cells (positive for PI) in the later stages of apoptosis (Figures 6b1 and c1, respectively). The Figures 6a2, b2 and c2 staining are the combination of a and a1, b and b1, and c and c1, respectively.
Figure 6.
Effect of zileuton and montelukast on apoptosis. At 24 h after SCI, spinal cord tissues obtained from SCI+vehicle-treated mice demonstrated a marked appearance of positive stain for annexin V FITC (a), an index of cells that are induced to undergo apoptosis. Some cells showed a positive intracellular staining to PI (a1), an index of cells in the late stage of apoptosis. On the contrary, spinal cord tissues section from mice treated with zileuton or montelukast demonstrate no cells in the earlier stage (b and c, respectively) of apoptosis and fewer cells (positive to PI) in the later stages of apoptosis (b1 and c1, respectively). (a2, b2, and c2) Staining combination of a and a1, b and b1, and c and c1, respectively. The figure is representative of at least three experiments performed on different experimental days. FITC, fluorescein isothiocyanate; PI, propidium iodide SCI, spinal cord injury.
Moreover, to confirm whether tissue damage was associated with apoptotic cell death, we also measured TUNEL-like staining in the perilesional spinal cord tissue. Almost no apoptotic cells were detectable in the spinal cord tissue from sham-operated mice (data not shown). At 24 h after the trauma, tissues obtained from SCI+vehicle-treated mice demonstrated a marked appearance of dark-brown (TUNEL-positive) apoptotic cells and intercellular apoptotic fragments (Figure 7a). In contrast, tissues obtained from mice treated with zileuton (Figure 7b) or montelukast (Figure 7c) contained a smaller number of TUNEL-positive cells. Section D demonstrates the positive staining in the Kit-positive control tissue.
Figure 7.
Effect of zileuton and montelukast on TUNEL staining in perilesional spinal cord tissue. At 24 h after the trauma, tissues obtained from SCI+vehicle-treated mice demonstrated a marked appearance of dark-brown apoptotic cells and intercellular apoptotic fragments (a). In contrast, tissues obtained from mice treated with zileuton (b) or montelukast (c) demonstrated a small number of apoptotic cells or fragments. Almost no apoptotic cells were detectable in the spinal cord tissue of sham-operated mice (data not shown). Panel d demonstrates the positive staining in the Kit-positive control tissue. The figure is representative of at least three experiments performed on different experimental days. SCI, spinal cord injury; TUNEL, terminal deoxynucleotidyltransferase-mediated UTP end labelling assay.
Immunohistological staining for FAS Ligand in the spinal cord was also determined 24 h after injury. Sections of spinal cord from sham+vehicle-treated mice did not stain for FAS Ligand (data not shown), whereas spinal cord sections obtained from SCI+vehicle-treated mice exhibited positive staining for FAS Ligand (Figures 4 and 8a) mainly localized in inflammatory cells as well as in nuclei of Schwann cells in the white (wm) and grey (gm) matter of the spinal cord tissues. Treatment of mice subjected to SCI with zileuton (Figures 4 and 8b) or montelukast (Figures 4 and 8c) reduced the degree of positive staining for FAS Ligand in the spinal cord. There was no staining for FAS Ligand in spinal cord tissues obtained from the sham group of mice (data not shown).
Figure 8.
Effect of zileuton and montelukast on immunohistological staining for FAS Ligand. At 24 h after the trauma spinal cord sections obtained from SCI+vehicle-treated mice exhibited positive staining for FAS Ligand (a) mainly localized in inflammatory cells as well as in nuclei of Schwann cells in the white (wm) and grey (gm) matter of the spinal cord tissues. Treatment of mice subjected to SCI with zileuton (b) or montelukast (c) reduced the degree of positive staining for FAS Ligand in the spinal cord. There was no staining for FAS Ligand in spinal cord tissues obtained from the sham group of mice (data not shown). SCI, spinal cord injury.
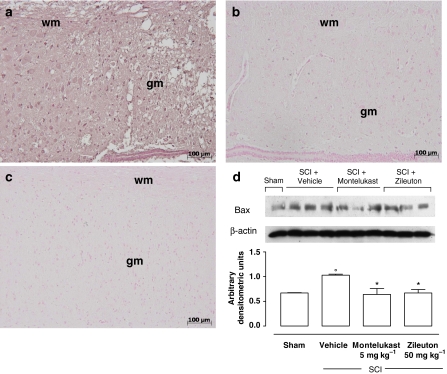
Effect of zileuton and montelukast on Bax and Bcl-2 immunohistochemistry and expression
Spinal cord tissues were taken at 24 h after SCI to determine the immunohistological staining for Bax and Bcl-2. Sections of spinal cord from sham+vehicle-treated mice showed a negative stain for Bax (data not shown), whereas those obtained from SCI+vehicle-treated mice exhibited positive staining for Bax (Figures 4 and 9a). The degree of positive staining for Bax was reduced in spinal cord tissues collected from mice treated with zileuton (Figures 4 and 9b) or montelukast (Figures 4 and 9c). Moreover, the appearance of Bax in homogenates of spinal cord tissues was investigated by western blot at 24 h after SCI. A basal level of Bax was detectable in the homogenized spinal cord tissues from sham+vehicle-treated animals (Figure 9d). Bax levels were significantly increased in the spinal cord tissues of SCI+vehicle-treated mice (Figure 9d). The treatment of mice with zileuton or montelukast prevented the SCI-mediated Bax expression (Figure 9d).
Figure 9.
Effect of zileuton and montelukast on Bax levels. At 24 h, SCI caused an increase of Bax expression in vehicle-treated mice (a). On the contrary, the degree of positive staining for Bax was reduced in spinal cord tissues collected from mice treated with zileuton (b) or montelukast (c). No positive staining for Bax was observed in the tissue section from sham-operated mice (data not shown). Figure is representative of at least three experiments performed on different experimental days. (d) Western blot analysis of extracts of spinal cord tissue collected at 24 h after injury. Basal levels of Bax was present in the tissue from sham-operated mice. Bax band is more evident in the tissue from SCI+vehicle-treated mice. The treatment with zileuton or montelukast reduced Bax levels. Data were normalized on the basis of β-actin levels. Densitometric analysis of protein expression represents the mean±s.e.mean of 10 spinal cord tissues. °P<0.01 versus sham-operated mice; *P<0.05 versus SCI+vehicle. wm, white matter; gm, grey matter; SCI, spinal cord injury.
In addition, sections of spinal cord from sham-operated mice demonstrated positive staining for Bcl-2 (data not shown). Spinal cord sections obtained from SCI+vehicle-treated mice exhibited less staining for Bcl-2 (Figures 4 and 10a). The loss of positive staining for Bcl-2 was significantly reduced in spinal cord tissues collected from mice treated with zileuton (Figures 4 and 10b) or montelukast (Figures 4 and 10c). The same results were observed by western blot analysis. In fact, a high basal level of Bcl-2 expression was detected in spinal cord homogenates from the tissue of sham+vehicle-treated mice (Figure 10d). The Bcl-2 expression was significantly diminished in whole extracts obtained from spinal cord tissues of vehicle-treated mice 24 h after SCI. Treatment of mice with zileuton or montelukast significantly increased the expression of Bcl-2 (Figure 10d).
Figure 10.
Effect of zileuton and montelukast on the Bcl-2 levels. At 24 h, SCI caused a decrease of the release of Bcl-2 expression in vehicle-treated mice (a). The degree of positive staining for Bcl-2 was increased in spinal cord tissues collected from mice treated with zileuton (b) or montelukast (c). Figure is representative of at least three experiments performed on different experimental days. (d) Western blot analysis of extracts of spinal cord tissue collected at 24 h after injury. Basal levels of Bcl-2 were present in the tissue from sham-operated mice. Bcl-2 band is less evident in the tissue from SCI+vehicle-treated mice. The treatment with zileuton or montelukast increased Bcl-2 levels. Data were normalized on the basis of β-actin levels. Densitometric analysis of protein expression represents the mean±s.e.mean of 10 spinal cord tissues. °P<0.01 versus sham; *P<0.05 versus SCI+vehicle. wm, white matter; gm, grey matter; SCI, spinal cord injury.
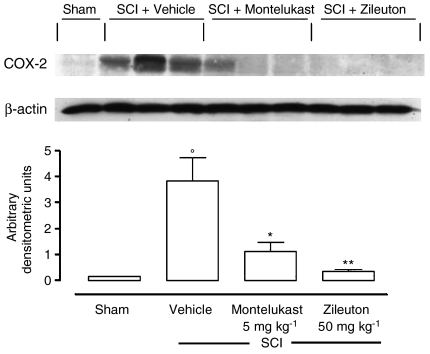
Effect of zileuton and montelukast on COX-2 expression and on activation of MAPK signal transduction pathway
As phosphorylation of ERK1/2 results in expression of genes, such as that encoding for COX-2, mediating the inflammatory responses characteristic of SCI, the expression of this enzyme and ERK1/2 phosphorylation in homogenates of spinal cord tissues was investigated by western blot at 24 h after SCI. A basal level of COX-2 was detectable in the homogenized spinal cord tissues from sham-operated animals (Figure 11). COX-2 levels were significantly increased in the spinal cord tissues of SCI+vehicle-treated mice. The treatment of mice with zileuton or montelukast reduced the SCI-mediated COX-2 expression (Figure 11).
Figure 11.
Effect of zileuton and montelukast on the COX-2 expression. Western blot analysis of extracts of spinal cord tissue collected at 24 h after injury. SCI caused an increase of COX-2 expression in vehicle-treated mice. The treatment with zileuton or montelukast reduced COX-2 levels. Densitometric analysis of protein expression represents the mean±s.e.mean of 10 spinal cord tissues. Data were normalized on the basis of β-actin levels. °P<0.01 versus sham; *P<0.05, **P<0.01 versus SCI+vehicle. COX-2, cyclooxygenase-2; SCI, spinal cord injury.
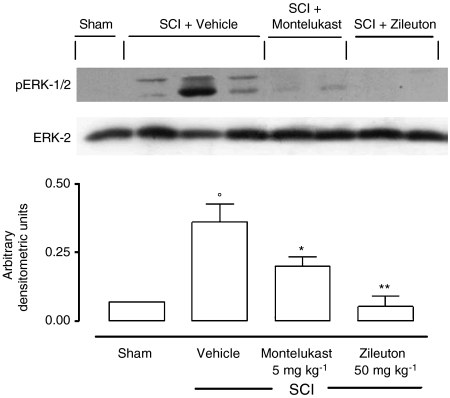
To investigate whether the increase in COX-2 expression, observed in our experimental conditions, corresponded to an activation of signal transduction pathways involved in the regulation of COX-2 expression, we analysed the activation of MAPK pathways in particular the phosphorylation of ERK1/2 24 h after SCI. As shown in Figure 11, pERK1/2 levels were significantly increased in the spinal cord tissues of SCI+vehicle-treated mice. The treatment of mice with zileuton or montelukast significantly reduced the level of pERK1/2 (Figure 12).
Figure 12.
Effect of zileuton and montelukast on ERK1/2 activation. Western blot analysis of extracts of spinal cord tissue collected at 24 h after injury. SCI caused an increase of the ERK1/2 phosphorylation in vehicle-treated mice. The treatment with zileuton or montelukast reduced pERK1/2 levels. Densitometric analysis of protein expression represents the mean±s.e.mean of 10 spinal cord tissues. Data were normalized on the basis of ERK-2 levels. °P<0.01 versus sham; *P<0.05, **P<0.01 versus SCI+vehicle. ERK1/2, extracellular signal-regulated kinase 1/2; SCI, spinal cord injury.
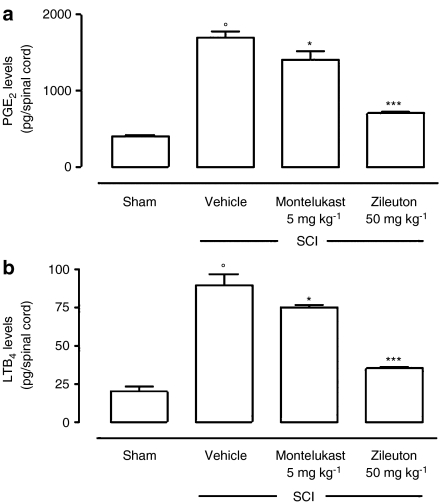
Effect of zileuton and montelukast on the production of PGE2 and LTB4
An increase of PGE2 and LTB4 formation was found in spinal cord samples collected from SCI+vehicle-treated mice at 24 h after SCI. Spinal cord levels of PGE2 and LTB4 were significantly attenuated in mice treated with zileuton or montelukast (Figures 13a and b).
Figure 13.
Effect of zileuton and montelukast on levels of PGE2 and LTB4 in spinal cord. SCI caused, at 24 h, an increase in the release of PGE2 (a) and LTB4 (b) in spinal cord tissues. Treatment with zileuton or montelukast significantly inhibited the SCI-induced increase of PGE2 (a) and LTB4 (b). Data are means±s.e.mean of 10 mice for each group. °P<0.01 versus sham-operated mice; *P<0.05; ***P<0.01 versus SCI+vehicle-treated mice. LTB4, leukotriene B4; PGE2, prostaglandin E2; SCI, spinal cord injury.
Discussion
The greater part of SCI in civilian life arises from fracture or dislocation of the vertebral column. Modern neuroscience techniques have led investigators to a better understanding of the importance of both primary (passive) and secondary (active) events in causing progressive loss of neural tissue. There are three stages of SCI where pharmacotherapy may have a therapeutic role (Greene et al., 1994, 1996). In the acute stage, treatments aimed towards diminishing the immune or inflammatory response, excitotoxicity and lipid peroxidation may limit secondary mechanisms of injury (Bracken et al., 1990). In the subacute stage, initiation of neurotrophic therapies may help to reconstitute the damaged tissue (Geisler et al., 1991, 1992). Interventions in the chronic stage of SCI will more than likely involve neurotrophic substances in combination with tissue or mesenchymal stem cell transplantation (Cheng et al., 1996; Bregman et al., 1997a, 1997b, 1998; Diener and Bregman, 1998a, 1998b). Nevertheless, only limited therapeutic measures are currently available for the treatment of SCI and only an extensive knowledge of the molecular and cellular mechanisms involved in the etiopathogenesis of SCI will lead to a crucial therapeutic intervention.
In this report, we demonstrate that a 5-LO inhibitor, zileuton, and a Cys-LT1 antagonist, montelukast, exert beneficial effects in a mouse model of SCI that mimics the human pathology. The main findings of the current study are that treatment with zileuton or montelukast improved motor recovery and reduced tissue injury, cell infiltration at the injured site, apoptotic cell death, ERK1/2 activation, and TNF-α and COX-2 levels in the injured tissue.
These results not only confirm our previous report showing that mice with a targeted deletion of the 5-LO gene (5-LO-deficient mice) are protected against experimental SCI (Genovese et al., 2005), but underline the role of Cys-LTs, although the role of other 5-LO metabolites cannot be excluded. (Sugaya et al., 2000; Bertolini et al., 2002; Hensley et al., 2006). In fact, it has been suggested that an overexpressed/overactive 5-LO pathway may lead to neurodegeneration by promoting neutrophil migration. It is well known that LTB4 and Cys-LTs are potent chemotactic factors involved in recruitment of cells at the inflammation site (Ford-Hutchinson et al., 1980; Levine et al., 1984; Bisgaard and Kristensen, 1985; Virchow et al., 2001). In particular, Cys-LTs exert their effects through binding Cys-LT1 receptors (Blain and Sirois, 2000). Moreover, in mice treated with zileuton or montelukast, a good correlation between the significant reduction of leucocyte infiltration, LT production and reduced tissue damage, evaluated by histological examination, was observed. In addition, mice treated with zileuton or montelukast showed an improvement in motor function.
Experimental evidence suggests that LTs may promote inflammation also through the regulation of other pro-inflammatory factors, such as TNF-α (Ichiyama et al., 2007; Tugtepe et al., 2007) and COX-2 (Rossi et al., 2005), which seem to be involved in neurodegeneration. Moreover, it has been demonstrated that TNF-α and COX-2 are clearly involved in the pathogenesis of experimental SCI in rats and mice (Yan et al., 2001; Bao et al., 2004; Adachi et al., 2005). In the present study, we have demonstrated, by immunohistochemistry, a significant increase of positive staining for TNF-α in SCI+vehicle mice compared with sham-operated animals. With regard to COX-2, we have recently demonstrated that in a model of inflammation in vitro, such as elicited peritoneal macrophages from mice activated with lipopolysaccharide/interferon-γ, LTC4, but not the other LTs, increased COX-2 expression and PG production (Rossi et al., 2005). The signal transduction mechanism involved in this upregulation was related to activation of the MAPK family of protein serine/threonine kinases, which includes ERK-1 and ERK-2 (Garrington and Johnson, 1999). In particular, the MAPK activation observed in the study was correlated with the phosphorylation of ERK1/2 through activation of the Cys-LT1 receptor. Similar results have been obtained in the present study as demonstrated by the decrease of COX-2, PGE2 and pERK1/2 levels in SCI+zileuton- or SCI+montelukast-treated mice, compared to SCI+vehicle-treated mice.
The LTs are regulatory signals for neural cell proliferation and differentiation (Wada et al., 2006) and apoptosis is an important mediator of secondary damage after SCI (Beattie et al., 2002). In this study, as observed previously in 5-LO knockout mice subjected to SCI (Genovese et al., 2005), the inhibition of the 5-LO pathway, by the use of zileuton or blockade of Cys-LT action by montelukast, reduced cell apoptosis (as assessed by annexin V, TUNEL and Fas ligand staining) after SCI induction in spinal cord tissue. This effect could be due to the inhibition of neutrophil infiltration. In other studies, decreased neutrophil infiltration due to the absence of 5-LO (Cuzzocrea et al., 2005) may have contributed to the attenuation of pro-apoptotic mediators, such as reactive oxygen species (Xu et al., 2005). Moreover, it is well known that Bax, a proapoptotic protein, plays an important role in the development of cell death (Chittenden et al., 1995) and in central nervous system injury (Bar-Peled et al., 1999). Likewise, it has been shown that the administration of Bcl–xL fusion protein (Bcl-2 is the most expressed antiapoptotic molecule in the adult central nervous system) into injured spinal cords significantly increased neuronal survival, suggesting that SCI-induced changes in Bcl–xL contribute considerably to neuronal death (Nesic-Taylor et al., 2005). On the basis of this evidence, we have identified apoptotic transcriptional changes in mice subjected to SCI. These include upregulation of proapoptotic Bax and downregulation of antiapoptotic Bcl-2, as assessed by Western blot assay and immunohistochemical staining. In particular, we demonstrated that zileuton and montelukast reduced the SCI-induced transcriptional changes related to apoptosis.
In conclusion, this study demonstrated that zileuton and montelukast improved motor recovery and reduced tissue injury, cell infiltration at the injured site, apoptotic cell death, pERK1/2 expression, and TNF-α and COX-2 level in injured tissue. Taken together, these results provide evidence that zileuton and montelukast were able to produce a substantial reduction of inflammatory events associated with experimental SCI and underline the important role of 5-LO and Cys-LTs in this model.
Acknowledgments
We thank Giovanni Pergolizzi and Carmelo La Spada for excellent technical assistance during this study, Caterina Cutrona for secretarial assistance and Valentina Malvagni for editorial assistance with the paper.
Abbreviations
- COX-2
cyclooxygenase-2
- Cys-LT
cysteinyl-LT
- ERK1/2
extracellular signal-regulated kinase 1/2
- 5-LO
5-lipoxygenase
- LT
leukotrienes
- LTB4
leukotriene B4
- LTC4
leukotriene C4
- MAPK
mitogen-activated protein kinase
- MPO
myeloperoxidase
- PG
prostaglandin
- SCI
spinal cord injury
- TNF-α
tumour necrosis factor-alpha
Conflict of interest
The authors state no conflict of interest.
References
- Adachi K, Yimin Y, Satake K, Matsuyama Y, Ishiguro N, Sawada M, et al. Localization of cyclooxygenase-2 induced following traumatic spinal cord injury. Neurosci Res. 2005;51:73–80. doi: 10.1016/j.neures.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Anderson AJ. Mechanisms and pathways of inflammatory responses in CNS trauma: spinal cord injury. J Spinal Cord Med. 2002;25:70–79. doi: 10.1080/10790268.2002.11753604. [DOI] [PubMed] [Google Scholar]
- Bao F, Chen Y, Dekaban GA, Weaver LC. An anti-CD11d integrin antibody reduces cyclooxygenase-2 expression and protein and DNA oxidation after spinal cord injury in rats. J Neurochem. 2004;90:1194–1204. doi: 10.1111/j.1471-4159.2004.02580.x. [DOI] [PubMed] [Google Scholar]
- Bar-Peled O, Knudson M, Korsmeyer SJ, Rothstein JD. Motor neuron degeneration is attenuated in Bax-deficient neurons in vitro. J Neurosci Res. 1999;55:542–556. doi: 10.1002/(SICI)1097-4547(19990301)55:5<542::AID-JNR2>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Basso DM, Beattie MS, Bresnahan JC. A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma. 1995;12:1–21. doi: 10.1089/neu.1995.12.1. [DOI] [PubMed] [Google Scholar]
- Beattie MS. Inflammation and apoptosis: linked therapeutic targets in spinal cord injury. Trends Mol Med. 2004;10:580–583. doi: 10.1016/j.molmed.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Beattie MS, Hermann GE, Rogers RC, Bresnahan JC. Cell death in models of spinal cord injury. Prog Brain Res. 2002;137:37–47. doi: 10.1016/s0079-6123(02)37006-7. [DOI] [PubMed] [Google Scholar]
- Bertolini A, Ottani A, Sandrini M. Selective COX-2 inhibitors and dual acting anti-inflammatory drugs: critical remarks. Curr Med Chem. 2002;9:1033–1043. doi: 10.2174/0929867024606650. [DOI] [PubMed] [Google Scholar]
- Bethea JR, Dietrich WD. Targeting the host inflammatory response in traumatic spinal cord injury. Curr Opin Neurol. 2002;15:355–360. doi: 10.1097/00019052-200206000-00021. [DOI] [PubMed] [Google Scholar]
- Bisgaard H, Kristensen JK. Leukotriene B4 produces hyperalgesia in humans. Prostaglandins. 1985;30:791–797. doi: 10.1016/0090-6980(85)90007-3. [DOI] [PubMed] [Google Scholar]
- Blain JF, Sirois P. Involvement of LTD4 in allergic pulmonary inflammation in mice: modulation by cysLT(1)antagonist MK-571. Prostaglandins Leukot Essent Fatty Acids. 2000;62:361–368. doi: 10.1054/plef.2000.0167. [DOI] [PubMed] [Google Scholar]
- Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal cord injury. N Engl J Med. 1990;322:1405–1411. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- Bregman BS, Broude E, McAtee M, Kelley MS. Transplants and neurotrophic factors prevent atrophy of mature CNS neurons after spinal cord injury. Exp Neurol. 1998;149:13–27. doi: 10.1006/exnr.1997.6669. [DOI] [PubMed] [Google Scholar]
- Bregman BS, Diener PS, McAtee M, Dai HN, James C. Intervention strategies to enhance anatomical plasticity and recovery of function after spinal cord injury. Adv Neurol. 1997a;72:257–275. [PubMed] [Google Scholar]
- Bregman BS, McAtee M, Dai HN, Kuhn PL. Neurotrophic factors increase axonal growth after spinal cord injury and transplantation in the adult rat. Exp Neurol. 1997b;148:475–494. doi: 10.1006/exnr.1997.6705. [DOI] [PubMed] [Google Scholar]
- Carlson GD, Gorden C. Current developments in spinal cord injury research. Spine J. 2002;2:116–128. doi: 10.1016/s1529-9430(01)00029-8. [DOI] [PubMed] [Google Scholar]
- Carlson SL, Parrish ME, Springer JE, Doty K, Dossett L. Acute inflammatory response in spinal cord following impact injury. Exp Neurol. 1998;151:77–88. doi: 10.1006/exnr.1998.6785. [DOI] [PubMed] [Google Scholar]
- Cheng H, Cao Y, Olson L. Spinal cord repair in adult paraplegic rats: partial restoration of hind limb function. Science. 1996;273:510–513. doi: 10.1126/science.273.5274.510. [DOI] [PubMed] [Google Scholar]
- Chittenden T, Harrington EA, O'Connor R, Flemington C, Lutz RJ, Evan GI, et al. Induction of apoptosis by the Bcl-2 homologue Bak. Nature. 1995;374:733–736. doi: 10.1038/374733a0. [DOI] [PubMed] [Google Scholar]
- Cuzzocrea S, Rossi A, Mazzon E, Di Paola R, Genovese T, Muia C, et al. 5-lipoxygenase modulate the development of colitis in mice through the regulation of adhesion molecules expression. Lab Invest. 2005;85:808–822. doi: 10.1038/labinvest.3700276. [DOI] [PubMed] [Google Scholar]
- Demopoulos HB, Yoder M, Gutman EG, Seligman ML, Flamm ES, Ransohoff J. The fine structure of endothelial surfaces in the microcirculation of experimentally injured feline spinal cords. Scan Electron Microsc. 1978;2:677–680. [Google Scholar]
- Diener PS, Bregman BS. Fetal spinal cord transplants support growth of supraspinal and segmental projections after cervical spinal cord hemisection in the neonatal rat. J Neurosci. 1998a;18:779–793. doi: 10.1523/JNEUROSCI.18-02-00779.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener PS, Bregman BS. Fetal spinal cord transplants support the development of target reaching and coordinated postural adjustments after neonatal cervical spinal cord injury. J Neurosci. 1998b;18:763–778. doi: 10.1523/JNEUROSCI.18-02-00763.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich WD, Chatzipanteli K, Vitarbo E, Wada K, Kinoshita K. The role of inflammatory processes in the pathophysiology and treatment of brain and spinal cord trauma. Acta Neurochir Suppl. 2004;89:69–74. doi: 10.1007/978-3-7091-0603-7_9. [DOI] [PubMed] [Google Scholar]
- Failla M, Genovese T, Mazzon E, Gili E, Muia C, Sortino M, et al. Pharmacological inhibition of leukotrienes in an animal model of bleomycin-induced acute lung injury. Respir Res. 2006;21:137. doi: 10.1186/1465-9921-7-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford-Hutchinson AW, Bray MA, Smith MJ. Lipoxygenase products and the polymorphonuclear leucocyte. Agents Actions. 1980;10:548–555. doi: 10.1007/BF02024162. [DOI] [PubMed] [Google Scholar]
- Garrington TP, Johnson GL. Organization and regulation of mitogen-activated protein kinase signaling pathway. Curr Opin Cell Biol. 1999;11:211–218. doi: 10.1016/s0955-0674(99)80028-3. [DOI] [PubMed] [Google Scholar]
- Geisler FH, Dorsey FC, Coleman WP. Recovery of motor function after spinal cord injury a randomized placebo-controlled trial with GM-1 ganglioside. N Engl J Med. 1991;324:1829–1838. doi: 10.1056/NEJM199106273242601. [DOI] [PubMed] [Google Scholar]
- Geisler FH, Dorsey FC, Coleman WP. GM-1 ganglioside in human spinal cord injury. J Neurotrauma. 1992;9:S517–S530. [PubMed] [Google Scholar]
- Genovese T, Mazzon E, Rossi A, Di Paola R, Cannavo G, Muia C, et al. Involvement of 5-lipoxygenase in spinal cord injury. J Neuroimmunol. 2005;166:55–64. doi: 10.1016/j.jneuroim.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Greene KA, Marciano FF, Sonntag VKH. Pharmacological strategies in the treatment of spinal cord injuries: a critical review. Crit Rev Neurosurg. 1994;4:254–264. [Google Scholar]
- Greene KA, Marciano FF, Sonntag VKH. Pharmacological management of spinal cord injury: current status of drugs designed to augment functional recovery of the injured human spinal cord. J Spinal Disord. 1996;9:355–366. [PubMed] [Google Scholar]
- Gris D, Marsh DR, Oatway MA, Chen Y, Hamilton EF, Dekaban GA, et al. Transient blockade of the CD11d/CD18 integrin reduces secondary damage after spinal cord injury, improving sensory, autonomic, and motor function. J Neurosci. 2004;24:4043–4051. doi: 10.1523/JNEUROSCI.5343-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamada Y, Ikata T, Katoh S, Nakauchi K, Niwa M, Kawai Y, et al. Involvement of an intracellular adhesion molecule 1-dependent pathway in the pathogenesis of secondary changes after spinal cord injury in rats. J Neurochem. 1996;66:1525–1531. doi: 10.1046/j.1471-4159.1996.66041525.x. [DOI] [PubMed] [Google Scholar]
- Hausmann ON. Post-traumatic inflammation following spinal cord injury. Spinal Cord. 2003;41:369–378. doi: 10.1038/sj.sc.3101483. [DOI] [PubMed] [Google Scholar]
- Hensley K, Mhatre M, Mou S, Pye QN, Stewart C, West M, et al. On the relation of oxidative stress to neuroinflammation: lessons learned from the G93A-SOD1 mouse model of amyotrophic lateral sclerosis. Antioxid Redox Signal. 2006;8:2075–2087. doi: 10.1089/ars.2006.8.2075. [DOI] [PubMed] [Google Scholar]
- Ichiyama T, Kajimoto M, Hasegawa M, Hashimoto K, Matsubara T, Furukawa S. Cysteinyl leukotrienes enhance tumour necrosis factor-alpha-induced matrix metalloproteinase-9 in human monocytes/macrophages. Clin Exp Allergy. 2007;37:608–614. doi: 10.1111/j.1365-2222.2007.02692.x. [DOI] [PubMed] [Google Scholar]
- Jacobs TP, Shohami E, Baze W, Burgard E, Gunderson C, Hallenbeck J, et al. Thromboxane and 5-HETE increase after experimental spinal cord injury in rabbits. Cent Nerv Syst Trauma. 1987;4:95–118. doi: 10.1089/cns.1987.4.95. [DOI] [PubMed] [Google Scholar]
- Joshi M, Fehlings MG. Development and characterization of a novel, graded model of clip compressive spinal cord injury in the mouse: Part 1. Clipdesign, behavioral outcomes and histopathology. J Neurotrauma. 2002a;19:175–190. doi: 10.1089/08977150252806947. [DOI] [PubMed] [Google Scholar]
- Joshi M, Fehlings MG. Development and characterization of a novel, graded model of clip compressive spinal cord injury in the mouse: Part 2. Quantitative neuroanatomical assessment and analysis of the relationships between axonal tracts, residual tissue and locomotor recovery. J Neurotrauma. 2002b;19:191–203. doi: 10.1089/08977150252806956. [DOI] [PubMed] [Google Scholar]
- Jung SB, Song CH, Yang CS, Kim SY, Lee KS, Shin AR, et al. Role of the phosphatidylinositol 3-kinase and mitogen-activated protein kinase pathways in the secretion of tumour necrosis factor-alpha and interleukin-10 by the PPD antigen of Mycobacterium tuberculosis. J Clin Immunol. 2005;25:482–490. doi: 10.1007/s10875-005-5431-1. [DOI] [PubMed] [Google Scholar]
- King VR, Huang WL, Dyall SC, Curran OE, Priestley JV, Michael-Titus AT. Omega-3 fatty acids improve recovery, whereas Omega-6 fatty acids worsen outcome, after spinal cord injury in the adult rat. J Neurosci. 2006;26:4672–4680. doi: 10.1523/JNEUROSCI.5539-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KS, Kim SR, Park HS, Park SJ, Min KH, Lee KY, et al. Cysteinyl leukotriene upregulates IL-11 expression in allergic airway disease of mice. J Allergy Clin Immunol. 2007;119:141–149. doi: 10.1016/j.jaci.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Leker RR, Shohami E. Cerebral ischemia and trauma-different etiologies yet similar mechanisms: neuroprotective opportunities. Brain Res Rev. 2002;39:55–73. doi: 10.1016/s0165-0173(02)00157-1. [DOI] [PubMed] [Google Scholar]
- Levine JD, Lau W, Kwiat G, Goetzl EJ. Leukotriene B4 produces hyperalgesia that is dependent on polymorphonuclear leukocytes. Science. 1984;225:743–745. doi: 10.1126/science.6087456. [DOI] [PubMed] [Google Scholar]
- Marusic S, Leach MW, Pelker JW, Azoitei ML, Uozumi N, Cui J, et al. Cytosolic phospholipase A2 alpha-deficient mice are resistant to experimental autoimmune encephalomyelitis. J Exp Med. 2005;202:841–851. doi: 10.1084/jem.20050665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzon E, Sautebin L, Caputi AP, Cuzzocrea S. 5-lipoxygenase modulates the alteration of paracellular barrier function in mice ileum during experimental colitis. Shock. 2006;25:377–383. doi: 10.1097/01.shk.0000209530.30564.22. [DOI] [PubMed] [Google Scholar]
- McTigue DM, Tani M, Krivacic K, Chernosky A, Kelner GS, Maciejewski D, et al. Selective chemokine mRNA accumulation in the rat spinal cord after contusion injury. J Neurosci Res. 1998;53:368–376. doi: 10.1002/(SICI)1097-4547(19980801)53:3<368::AID-JNR11>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Mitsuhashi T, Ikata T, Morimoto K, Tonai T, Katoh S. Increased production of eicosanoids, TXA2, PGI2 and LTC4 in experimental spinal cord injuries. Paraplegia. 1994;32:524–530. doi: 10.1038/sc.1994.84. [DOI] [PubMed] [Google Scholar]
- Mullane KM, Kraemer R, Smith B. Myeloperoxidase activity as a quantitative assessment of neutrophil infiltration into ischemic myocardium. J Pharmacol Methods. 1985;14:157–167. doi: 10.1016/0160-5402(85)90029-4. [DOI] [PubMed] [Google Scholar]
- Nesic-Taylor O, Cittelly D, Ye Z, Xu GY, Unabia G, Lee JC, et al. Exogenous Bcl-xL fusion protein spares neurons after spinal cord injury. J Neurosci Res. 2005;79:628–637. doi: 10.1002/jnr.20400. [DOI] [PubMed] [Google Scholar]
- Nishisho T, Tonai T, Tamura Y, Ikata T. Experimental and clinical studies of eicosanoids in cerebrospinal fluid after spinal cord injury. Neurosurgery. 1996;39:950–956. doi: 10.1097/00006123-199611000-00014. [DOI] [PubMed] [Google Scholar]
- Profyris C, Cheema SS, Zang D, Azari MF, Boyle K, Petratos S. Degenerative and regenerative mechanisms governing spinal cord injury. Neurobiol Dis. 2004;15:415–436. doi: 10.1016/j.nbd.2003.11.015. [DOI] [PubMed] [Google Scholar]
- Rossi A, Acquaviva AM, Iuliano F, Di Paola R, Cuzzocrea S, Sautebin L. Up-regulation of prostaglandin biosynthesis by leukotriene C4 in elicited mice peritoneal macrophages activated with lipopolysaccharide/interferon-γ. J Leuk Biol. 2005;78:985–991. doi: 10.1189/jlb.1004619. [DOI] [PubMed] [Google Scholar]
- Saito H, Morikawa H, Howie K, Crawford L, Baatjes AJ, Denburg E, et al. Effects of a cysteinyl leukotriene receptor antagonist on eosinophil recruitment in experimental allergic rhinitis. Immunology. 2004;113:246–252. doi: 10.1111/j.1365-2567.2004.01944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schutte B, Nuydens R, Geerts H, Ramaekers F. Annexin V binding assay as a tool to measure apoptosis in differentiated neuronal cells. J Neurosci Methods. 1998;86:63–69. doi: 10.1016/s0165-0270(98)00147-2. [DOI] [PubMed] [Google Scholar]
- Shea TB. Technical report. An inexpensive densitometric analysis system using a Macintosh computer and a desktop scanner. Biotechniques. 1994;16:1126–1128. [PubMed] [Google Scholar]
- Shohami E, Jacobs TP, Hallenbeck JM, Feuerstein G. Increased thromboxane A2 and 5-HETE production following spinal cord ischemia in the rabbit. Prostaglandins Leukot Med. 1987;28:169–181. doi: 10.1016/0262-1746(87)90161-2. [DOI] [PubMed] [Google Scholar]
- Stover SL, Fine PR. The epidemiology and economics of spinal cord injury. Paraplegia. 1987;24:225–228. doi: 10.1038/sc.1987.40. [DOI] [PubMed] [Google Scholar]
- Sugaya K, Uz T, Kumar V, Manev H. New anti-inflammatory treatment strategy in Alzheimer's disease. Jpn J Pharmacol. 2000;82:85–94. doi: 10.1254/jjp.82.85. [DOI] [PubMed] [Google Scholar]
- Suttorp N, Seeger W, Zucker-Reimann J, Roka L, Bhakdi S. Mechanism of leukotriene generation in polymorphonuclear leukocytes by staphylococcal alpha-toxin. Infect Immun. 1987;55:104–110. doi: 10.1128/iai.55.1.104-110.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taoka Y, Okajima K, Uchiba M, Murakami K, Kushimoto S, Johno M, et al. Role of neutrophils in spinal cord injury in the rat. Neuroscience. 1997;74:1177–1182. doi: 10.1016/s0306-4522(97)00011-0. [DOI] [PubMed] [Google Scholar]
- Tator CH. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathology. 1995;5:407–413. doi: 10.1111/j.1750-3639.1995.tb00619.x. [DOI] [PubMed] [Google Scholar]
- Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg. 1991;75:15–26. doi: 10.3171/jns.1991.75.1.0015. [DOI] [PubMed] [Google Scholar]
- Tugtepe H, Sener G, Cetinel S, Velioglu-Ogunc A, Yegen BC. Oxidative renal damage in pyelonephritic rats is ameliorated by montelukast, a selective leukotriene CysLT1 receptor antagonist. Eur J Pharmacol. 2007;557:69–75. doi: 10.1016/j.ejphar.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Virchow JC, Faehndrich S, Nassenstein C, Bock S, Matthys H, Luttmann W. Effect of a specific cysteinyl leukotriene-receptor 1-antagonist (montelukast) on the transmigration of eosinophils across human umbilical vein endothelial cells. Clin Exp Allergy. 2001;31:836–844. doi: 10.1046/j.1365-2222.2001.01051.x. [DOI] [PubMed] [Google Scholar]
- Wada K, Arita M, Nakajima A, Katayama K, Kudo C, Kamisaki Y, et al. Leukotriene B4 and lipoxin A4 are regulatory signals for neural stem cell proliferation and differentiation. FASEB J. 2006;20:1785–1792. doi: 10.1096/fj.06-5809com. [DOI] [PubMed] [Google Scholar]
- Xu J, Hsu CY, Liu TH, Hogan EL, Perot E, Tai H. Leukotriene B4 release and polymorphonuclear cell infiltration in spinal cord injury. J Neurochem. 1990;55:907–912. doi: 10.1111/j.1471-4159.1990.tb04577.x. [DOI] [PubMed] [Google Scholar]
- Xu J, Kim GM, Chen S, Yan P, Ahmed SH, Ku G, et al. iNOS and nitrotyrosine expression after spinal cord injury. J Neurotrauma. 2001;18:523–532. doi: 10.1089/089771501300227323. [DOI] [PubMed] [Google Scholar]
- Xu W, Chi L, Xu R, Ke Y, Luo C, Cai J, et al. Increased production of reactive oxygen species contributes to motor neuron death in a compression mouse model of spinal cord injury. Spinal Cord. 2005;43:204–213. doi: 10.1038/sj.sc.3101674. [DOI] [PubMed] [Google Scholar]
- Yan P, Li Q, Kim GM, Xu J, Hsu CY, Xu XM. Cellular localization of tumour necrosis factor-alpha following acute spinal cord injury in adult rats. J Neurotrauma. 2001;18:563–568. doi: 10.1089/089771501300227369. [DOI] [PubMed] [Google Scholar]
- Yang L, Blumbergs PC, Jones NR, Manavis J, Sarvestani GT, Ghabriel MN. Early expression and cellular localization of proinflammatory cytokines interleukin-1beta, interleukin-6, and tumour necrosis factor-alpha in human traumatic spinal cord injury. Spine. 2004;29:966–971. doi: 10.1097/00007632-200405010-00004. [DOI] [PubMed] [Google Scholar]