Abstract
Context
Patterns of genetic, environmental, and phenotypic relationships among antisocial behavior and substance use disorders indicate the presence of a common externalizing liability. However, whether this liability is relatively continuous and graded, or categorical and class-like, has not been well established.
Objectives
To compare the fit of categorical and continuous models of externalizing liability in a large, nationally representative sample.
Design
Categorical and continuous models of externalizing liability were compared using interview data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC).
Setting
Face-to-face interviews conducted in the United States.
Participants
Random sample of 43 093 noninstitutionalized adult civilians living in the United States.
Main Outcome Measures
Lifetime and current (past 12 months) diagnoses of antisocial personality disorder, nicotine dependence, alcohol dependence, marijuana dependence, cocaine dependence, and other substance dependence.
Results
In the entire sample, as well as for males and females separately, using either lifetime or current diagnoses, the best-fitting model of externalizing liability was a continuous normal model. Moreover, there was a general trend toward latent trait models fitting better than latent class models, indicating that externalizing liability was continuous and graded, rather than categorical and class-like.
Conclusions
Liability to externalizing spectrum disorders is graded and continuous normal in distribution. Research regarding etiology, assessment, and treatment of externalizing disorders should target externalizing liability over a range of severity. Current diagnoses represent extremes of this continuous liability distribution, indicating that conditions currently classified as subthreshold are likely to provide important information regarding liability to externalizing phenomena.
Numerous studies have documented extensive comorbidity among antisocial behavior disorders, alcohol use disorders, and other substance use disorders.1–4 These disorders exhibit greater comorbidity among themselves than with other disorders, suggesting that a common liability underlies expression of these disorders in a single externalizing spectrum.5–7 An externalizing spectrum has been invoked to explain patterns of comorbidity in large epidemiological samples in numerous cultures,8,9 cross-sectionally5,9 as well as longitudinally.8 Patterns of genetic and environmental relationships between these disorders are also consistent with a common underlying liability,10,11 suggesting that an externalizing spectrum is evident etiologically as well as phenotypically.
Although these disorders exhibit patterns of comorbidity consistent with a common underlying liability, the nature of this liability, in terms of its distribution and relationship with observed disorders, has not been studied extensively. One possibility is that liability to externalizing spectrum disorders is continuous, and that risk of externalizing disorders is graded. Another possibility is that the liability underlying externalizing spectrum disorders is categorical, such that individuals fall into groups or classes of liability. The former hypothesis suggests that a single liability continuum predisposes individuals to express externalizing pathology in various degrees of severity. The latter hypothesis, in contrast, suggests that distinct categories of liability predispose individuals to express unique configurations of externalizing pathology, depending on the category membership (eg, antisocial behavior disorder without substance use vs substance use disorder vs no disorder).
These different conceptions of liability have important implications for research into the assessment, etiology, and treatment of externalizing disorders. Most major psychiatric classification systems, for example, are based on a categorical system of assessment and assume that individuals fall into distinct categories of pathology, each with unique configurations of behavioral expression. A finding that externalizing liability is categorical would support this conceptualization and suggest that research on externalizing etiology and treatment focus on particular classes of liability and how these classes are manifested in particular profiles of externalizing pathology (eg, antisocial behavior disorder without substance use).
A finding that externalizing liability is continuous, in contrast, would suggest that disorders currently classified as distinct might be better treated within a unified spectrum of externalizing pathology. Finding that externalizing liability is continuous would similarly suggest that research on externalizing etiology and treatment focus on this common continuum of liability and how it increases or decreases the severity of externalizing pathology.
One compelling approach to determining whether externalizing liability is continuous or categorical is to explicitly compare the fit of statistical models that differ in their characterization of the liability distribution. In this approach, continuous and categorical models of liability are explicitly compared in their ability to account for patterns of comorbidity among disorders. To the extent that categorical or continuous liability models better account for patterns of cormorbidity, that liability model is most likely to accurately describe patterns of liability in the population.
Quantitative results have shown that continuous and discrete liability distribution models can be effectively discriminated.12–14 Moreover, categorical and continuous externalizing liability models have been empirically compared in only a single study of which we are aware.15 In that study, results suggested that externalizing liability is continuous rather than categorical. However, the study was limited by a focus on a relatively circumscribed sample (ie, adults residing in Minnesota), as well as by a focus on DSM-III-R as opposed to DSM-IV diagnostic criteria.
In this work, we sought to extend our previous efforts by comprehensively comparing liability models in a large sample designed to be representative of a broad population using DSM-IV criteria. Specifically, we compared the fit of discrete and continuous externalizing liability models in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) using lifetime and current (past 12 months) diagnoses. The extremely large size (N=43 093) and representativeness of NESARC makes it particularly suitable for comparing continuous and categorical liability models. To our knowledge, this is the first study to explicitly compare the fit of continuous and categorical liability models of mental disorders in a nationally representative sample.
METHODS
SAMPLE
Wave 1 of NESARC is composed of a representative sample of 43 093 noninstitutionalized adult civilians living in the United States, aged 18 years and older. Data collection using face-to-face interviews was conducted by the National Institute of Alcohol Abuse and Alcoholism in 2001 through 2002, yielding an overall response rate of 81%. Informed consent was obtained from all participants. Results from NESARC have been published extensively in the Archives of General Psychiatry4,16 and elsewhere17; those publications may be consulted for further details regarding sample characteristics, data collection, and other aspects of NESARC.
ASSESSMENT
Analyses presented here were conducted on binary lifetime and current (ie, past-year) diagnoses in NESARC, based on DSM-IV criteria. Interviews were conducted by trained nonclinician interviewers using computer-assisted software. Interviews were conducted using the National Institute on Alcohol Abuse and Alcoholism’s (NIAAA) Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV),18 a structured interview designed for use by nonclinician interviewers. Extensive evidence of the reliability and validity of diagnoses using the AUDADIS-IV has been reported in a variety of publications.19–23
Six externalizing spectrum disorders were examined in the current study: antisocial personality disorder, nicotine dependence, alcohol dependence, marijuana dependence, cocaine dependence, and other substance dependence. Other substance dependence included use of heroin, amphetamines, sedatives, tranquilizers, opioids, hallucinogens, inhalants or solvents, or other substances not specified a priori. Individuals were considered to meet criteria for other substance dependence if they met dependence criteria for at least one of these substances.
STATISTICAL ANALYSES
Two types of models were used to model patterns of comorbidity among the 6 externalizing diagnoses: latent class models (LCMs) and latent trait models (LTMs). Latent class models represent patterns of comorbidity in terms of latent unobserved categories or classes. Latent trait models, in contrast, represent patterns of comorbidity in terms of latent unobserved continua or traits. In both LCMs and LTMs, diagnoses are assumed to be statistically independent (ie, noncomorbid) given the value of a latent variable (ie, latent class or latent trait value). Specifically in LCMs, there is assumed to be no diagnostic comorbidity among individuals who are members of the same latent class. Similarly, in LTMs, there is assumed to be no diagnostic comorbidity among individuals who have the same value of the latent trait. The latent classes of LCMs and latent traits of LTMs in this way account for comorbidity among diagnoses.
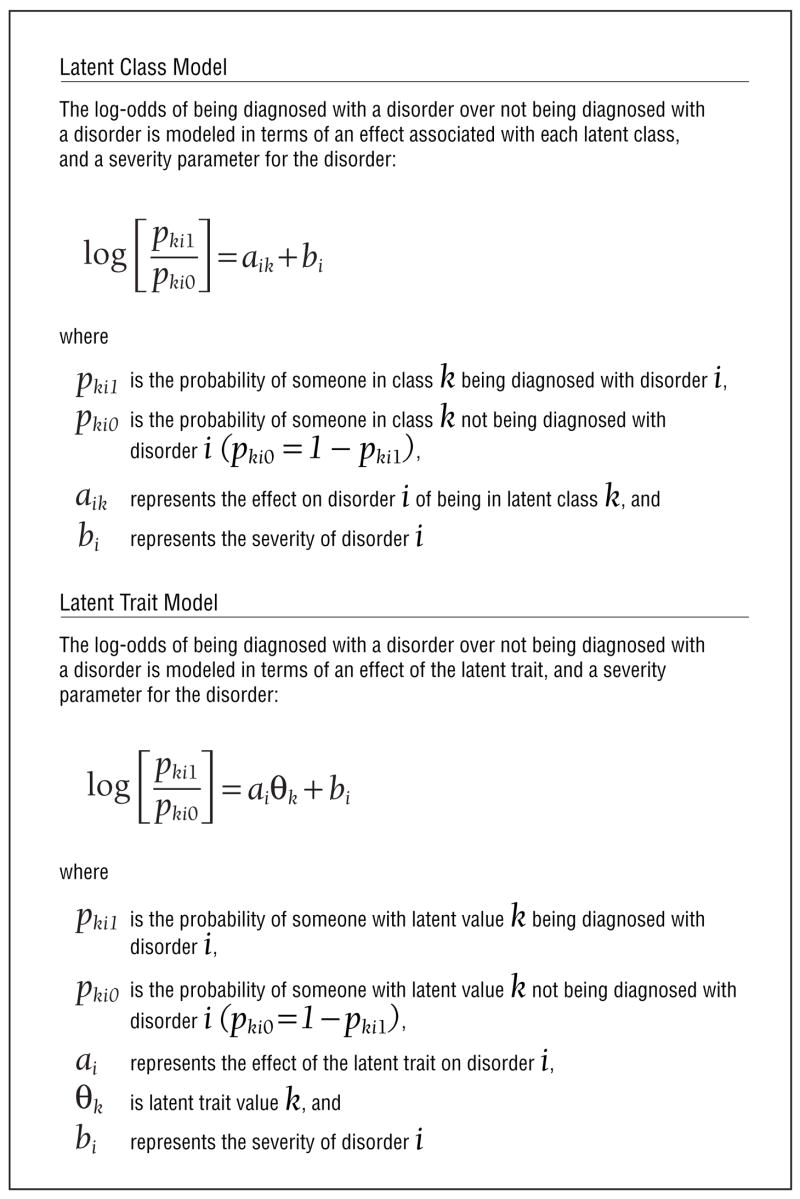
Latent class models and latent trait models, representing categorical and continuous conceptions of comorbidity among disorders, can both be compared in a single logistic modeling framework (Figure 1).24 In this framework, each model contains 2 types of parameters for the disorders. The first type of parameter represents the relationship between underlying liability and observed disorders—ie, the effect of liability on the observed disorders. The second type of parameter represents the severity of each observed disorder—ie, the probability of having each disorder above and beyond underlying liability. In the LCM, the log odds of receiving each diagnosis is modeled as a function of latent class membership, with parameters for the effect of each latent class on each observed diagnosis (aik in Figure 1), and parameters for the severity of each disorder (bi). In the LTM, in contrast, the log odds of receiving each diagnosis is modeled as a function of the latent trait, with parameters for the linear effect of liability on observed disorder (ie, slope parameters; ai) and parameters for the severity of each disorder (ie, intercept parameters; bi).
Figure 1.
Definition and interpretation of latent class and latent trait models and parameters.
In this logistic framework, LTMs can be treated as restricted versions of LCMs, in which the effect of each latent value is restricted to be linear with regard to the log odds of receiving a diagnosis. In the LCM, the latent values (ie, classes) each have an independent effect on each observed disorder. In the LTM, the latent values are linearly ordered in their effects on each observed disorder. In the LCM, therefore, the effect of each latent class on each observed disorder must be estimated; in the LTM, in contrast, a single linear effect of the latent trait on each observed disorder is estimated.
In both LCMs and LTMs, the probability of each latent value—ie, each latent class k or latent trait value θk—can be freely estimated. Alternatively, the probabilities of each latent value can be assumed to follow a specific distribution, such as a normal distribution. Thus, in both LCMs and LTMs, there are parameters representing the number and distribution of latent values, in addition to parameters representing the effect of liability on the observed disorders (ai) and the severity of each disorder (bi).
By comparing the fit of LCM and LTM models having the same number of latent classes or values (eg, the 3-class LCM and 3-value LTM), we obtained a test of whether liability is composed of graded levels of severity—specifically, whether each additional category of liability increases linearly in severity. Similarly, by comparing the fit of LTMs having having fewer vs more latent values, we obtained a test of the relative discreteness vs continuousness of liability. Finally, by comparing LTMs having many freely distributed latent values with LTMs whose values are assumed to be normally distributed, we obtained a test of the normality of the liability distribution.
We also present response functions and information functions for the best-fitting model. Response functions are graphical curves representing the probability of disorder as a function of underlying liability. Information functions, similarly, are graphical curves representing the relative amount of statistical information each disorder provides about underlying liability. In general, the maximum height of an information function is proportional to the slope parameter for that disorder. A greater slope parameter represents a stronger relationship between underlying liability and observed disorder, and thus indicates that the disorder provides greater information about underlying liability. The location of an information function, in contrast, corresponds to the severity of the disorder. Specifically, the maximum height of an information function occurs at the threshold value for a disorder, which is that point on the liability distribution at which a disorder becomes more likely than not. The threshold value for a disorder is given by the intercept for that disorder divided by its slope (−bi/ai).
Although the models being compared can be formulated in a unified logistic framework, they are not nested in one another. We therefore used an information-theoretic criterion to compare models. In particular, we used the Bayesian information criterion (BIC),25 which is appropriate for comparisons among nonnested models. Briefly, BIC balances the closeness of fit of a model against increases in model complexity. Smaller values of BIC are preferred. The difference between any 2 BICs can be directly interpreted as having corrected for expected effects of sampling variation, and is exponentially related to the posterior odds of one model vs the other. Specifically, the exponential of the negative difference in BIC can be interpreted as the posterior odds of one model over the other26 (eg, a BIC difference of −2 can be interpreted as implying that the odds of the better fitting model model over the other model are approximately e2=7.4).
Simulations have indicated that BIC correctly discriminates between LCMs and LTMs,14 and theoretical results indicate that BIC should correctly identify the population model or the best approximating model in large samples, even among nonnested alternative models.27,28 For completeness, we also present the number of parameters of each model, and the log likelihood of each model (ie, the logarithm of the probability of the observed data under each model), although these 2 criteria cannot be used alone to evaluate the fit of models.
In the current analyses, we fit latent class models including between 2 and 6 latent classes (given that there were 6 observed disorders, it was not possible to fit latent class models having more than 6 classes). In addition, we fit latent trait models with between 2 and 6 latent values, where the distribution of the latent values was freely estimated. Finally, we fit a normal latent trait model, where the distribution of the latent trait was assumed to be continuous standard normal. Models were fit to the entire sample, as well as separately by sex.
In addition to analyses comparing the fit of categorical and continuous latent variable models, we conducted analyses to determine whether parameter estimates of the best-fitting latent variable model were similar across sex and disorder. Models in which parameter estimates were constrained to be equal across sex and disorder were compared with models in which parameter estimates were allowed to differ across sex and disorder.
All analyses were conducted using the Latent GOLD29 software package (Statistical Innovations, Belmont, Mass), using sampling weights and other sampling design variables to estimate parameters and standard errors.30,31 The analytic approach taken here is similar to that taken by the authors in a previous article14 and readers are referred to that article for further details regarding the analyses. More general discussions regarding relationships between LCMs and LTMs are presented in a variety of sources.24,32,33
RESULTS
In the whole sample, the best-fitting models were trait models (Table 1). The best-fitting model overall was the continuous normal trait model. This model had the smallest value of BIC, indicating that it provided the best account of comorbidity patterns among the externalizing disorders. The second best-fitting model was the 4-value LTM. The 4-, 5-, and 6-value trait models both exhibited better fit than all of the latent class models. Among the LCMs, the best-fitting model was the 3-class model.
Table 1.
Fit Criteria for Discrete and Continuous Liability Models in the National Epidemiologic Survey on Alcohol and Related Conditions
| Criterion
|
|||
|---|---|---|---|
| Model | k* | ln(L) | BIC |
| Entire sample (N = 43 093) | |||
| Latent class models | |||
| 2 classes | 13 | −46306.66 | 46376.02 |
| 3 classes | 20 | −46023.09 | 46129.80 |
| 4 classes | 27 | −46006.01 | 46150.07 |
| 5 classes | 34 | −45996.14 | 46177.55 |
| 6 classes | 41 | −45983.80 | 46202.56 |
| Latent trait models | |||
| 2 values | 13 | −46306.66 | 46376.02 |
| 3 values | 14 | −46097.12 | 46171.82 |
| 4 values | 15 | −46026.45 | 46106.48 |
| 5 values | 16 | −46021.74 | 46107.11 |
| 6 values | 17 | −46011.51 | 46102.21 |
| Normal | 12 | −46032.62 | 46096.65 |
| Females (n = 24 575) | |||
| Latent class models | |||
| 2 classes | 13 | −21302.73 | 21368.44 |
| 3 classes | 20 | −21174.89 | 21275.99 |
| 4 classes | 27 | −21163.74 | 21300.22 |
| 5 classes | 34 | −21155.15 | 21327.02 |
| 6 classes | 41 | −21151.86 | 21359.10 |
| Latent trait models | |||
| 2 values | 13 | −21302.73 | 21368.44 |
| 3 values | 14 | −21210.25 | 21281.01 |
| 4 values | 15 | −21177.75 | 21253.57 |
| 5 values | 16 | −21176.42 | 21257.29 |
| 6 values | 17 | −21175.52 | 21261.45 |
| Normal | 12 | −21185.26 | 21245.92 |
| Males (n = 18 518) | |||
| Latent class models | |||
| 2 classes | 13 | −23558.19 | 23622.06 |
| 3 classes | 20 | −23405.57 | 23503.83 |
| 4 classes | 27 | −23387.54 | 23520.20 |
| 5 classes | 34 | −23382.78 | 23549.83 |
| 6 classes | 41 | −23373.16 | 23574.60 |
| Latent trait models | |||
| 2 values | 13 | −23558.19 | 23622.06 |
| 3 values | 14 | −23439.44 | 23508.23 |
| 4 values | 15 | −23408.12 | 23481.82 |
| 5 values | 16 | −23395.67 | 23474.28 |
| 6 values | 17 | −23395.80 | 23479.33 |
| Normal | 12 | −23407.60 | 23466.56 |
Abbreviations: BIC, Bayesian information criterion; ln(L), log likelihood.
k indicates number of parameters.
Patterns of results were notably consistent across different sample groups. General patterns of model fit were similar across females and males separately, and resembled patterns of fit in the whole sample (Table 1). As in the whole sample, among both females and males, the continuous normal trait models again exhibited the best fit. Moreover, among both females and males, the continuous normal model again exhibited the best fit, followed by the 4-, 5-, and 6-value LTMs, followed by the 3-class LCM.
Patterns of results were also notably consistent across different duration criteria. Analyses were also conducted on current (ie, past 12 months only) diagnoses, and general patterns of results did not differ from those using lifetime criteria. In the total sample using current diagnoses, the best-fitting model was again the continuous normal distribution model, followed by the 4-, 5-, and 6-value LTMs. Moreover, in both females and males, using current diagnoses, the best-fitting model was the continuous normal model, followed by LTMs.
Analyses in which parameter estimates were constrained across sex indicated that the best-fitting continuous normal liability model was one in which the slopes were constant across sex, but the intercepts differed between males and females (Table 2). That is, liability had the same relationship with probability of disorder in males and females, except that the overall probability of disorder was elevated in males. Additional model comparisons indicated that the disorders did not have equal slopes (Table 2).
Table 2.
Fit Criteria for Continuous Liability Models Constraining Parameter Estimates Across Sex and Disorder*
| Criterion
|
|||
|---|---|---|---|
| Model | K† | ln(L) | BIC |
| Slopes, intercepts differ across sex | 24 | −45449.84 | 45577.89 |
| Slopes differ, intercepts equal across sex | 18 | −45646.72 | 45742.76 |
| Slopes equal, intercepts differ across sex | 18 | −45465.10 | 45561.14 |
| Slopes equal across sex and disorder, intercepts differ | 13 | −45647.14 | 45716.51 |
| Slopes, intercepts equal across sex | 12 | −46033.12 | 46097.15 |
Abbreviations: BIC, Bayesian information criterion; ln(L), log likelihood.
Fit criteria for continuous normal liability models in which various combinations of slope and intercept parameters were constrained to be equal across sex and disorder. In all models except for the fourth model, parameters were allowed to differ across disorder.
k indicates number of parameters.
Parameter estimates under the best-fitting model indicate that the disorders provide differential information about underlying externalizing liability, and also differ in their severity along the externalizing spectrum (Table 3). Slope estimates of cocaine dependence and other substance use dependence were greater than those of the other disorders, suggesting that the former disorders, as they are assessed in NESARC, provide greater information about the underlying externalizing continuum than the other disorders. The intercepts and corresponding thresholds are generally consistent with previous research indicating that substances can be arrayed on a continuum of severity, with nicotine and alcohol use less severe than cocaine and other substance use.34,35
Table 3.
Parameter Estimates of Best-Fitting Model in Entire Sample*
| Parameter Estimates† |
|||||
|---|---|---|---|---|---|
| Males
|
Females
|
||||
| Disorder | Slope (SE) | Intercept (SE) | Threshold | Intercept (SE) | Threshold |
| Nicotine dependence | 1.67 (.03) | −2.02 (.04) | 1.21 | −2.44 (.04) | 1.46 |
| Alcohol dependence | 2.18 (.04) | −2.63 (.05) | 1.21 | −3.97 (.05) | 1.82 |
| Antisocial personality disorder | 1.76 (.03) | −3.99 (.06) | 2.27 | −5.32 (.06) | 3.02 |
| Marijuana dependence | 2.94 (.07) | −7.28 (.13) | 2.48 | −8.30 (.13) | 2.82 |
| Cocaine dependence | 3.09 (.08) | −8.04 (.18) | 2.60 | −8.83 (.18) | 2.86 |
| Other substance dependence | 3.21 (.07) | −8.18 (.15) | 2.55 | −8.82 (.15) | 2.75 |
Parameter estimates in the entire National Epidemiologic Survey on Alcohol and Related Conditions sample under best-fitting model, a continuous normal liability model with sex-specific intercepts.
Parameter estimates are explained in Figure 1 and in the text.
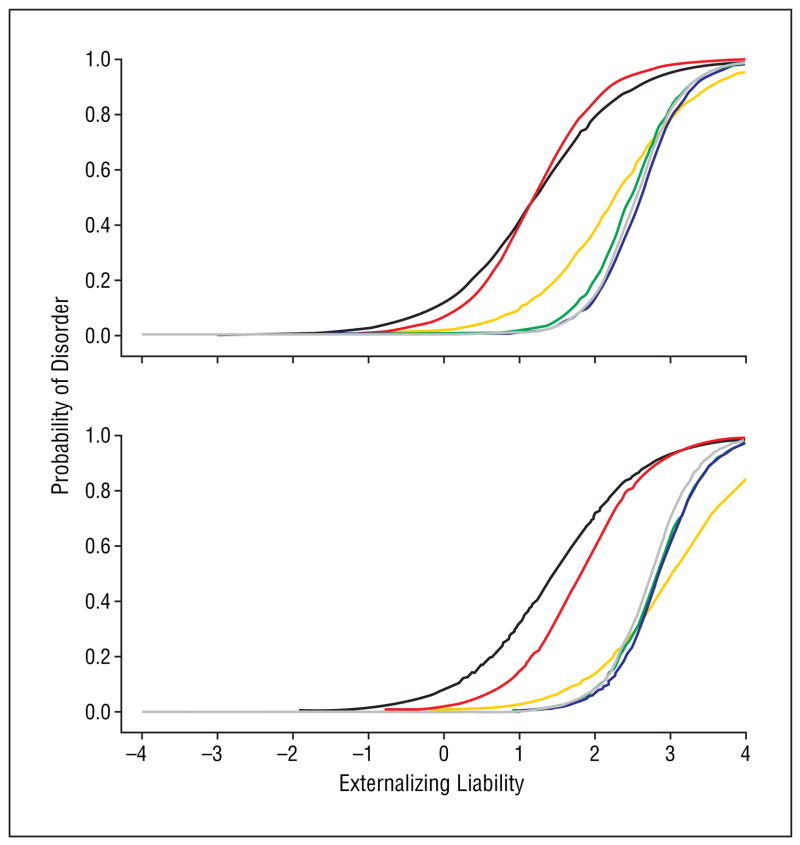
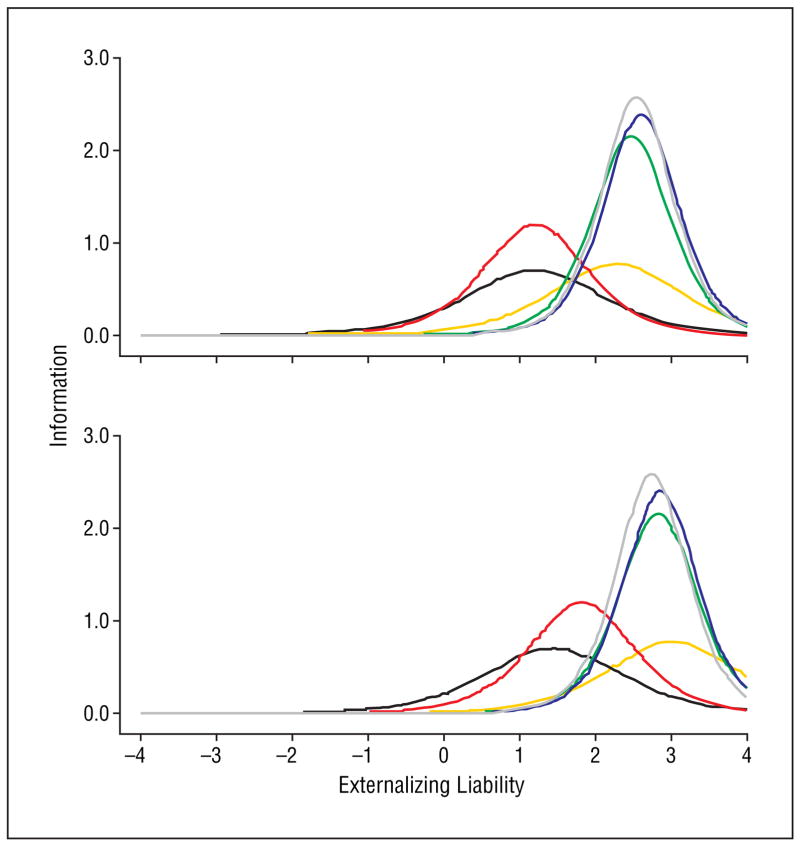
Response functions (Figure 2) and information functions (Figure 3) for each sex illustrate the differences in informativeness and severity of each disorder with regard to the underlying liability continuum. For example, for both sexes, the maximum of the other substance dependence information function was greatest among externalizing disorders, indicating that this disorder provided the greatest information about the underlying liability continuum overall. Similarly, the maximum of the nicotine dependence information function was smallest, indicating that this disorder provided the least information about the underlying externalizing liability continuum overall.
Figure 2.
Response functions of externalizing disorders under continuous normal liability model. Response functions for males are presented in the top figure; those for females are presented in the bottom figure. Response functions represent the probability of each disorder as a function of underlying liability. The response function for antisocial personality disorder is shown in orange; nicotine dependence in black; alcohol dependence in red; marijuana dependence in green; cocaine dependence in blue; other drug dependence in gray. Externalizing liability is given in standardized z-score units.
Figure 3.
Information functions of externalizing disorders under continuous normal liability model. Information functions for males are presented in the top figure; those for females are presented in the bottom figure. Information functions represent the relative amount of statistical information each disorder provides about underlying liability; information functions are described in detail in the text. Antisocial personality disorder is shown in orange; nicotine dependence in black; alcohol dependence in red; marijuana dependence in green; cocaine dependence in blue; other drug dependence in gray. Externalizing liability is given in standardized z-score units.
The response and information functions for males were shifted to the negative end of the liability continuum relative to those for females, reflecting the greater overall probability of externalizing disorder among males. The alcohol and nicotine dependence response and information functions were shifted to the more negative end of the liability continuum, indicating that those 2 disorders provided more information about less severe forms of externalizing. Similarly, the antisocial personality disorder and remaining substance dependence response and information functions were shifted to the extreme positive end of the liability continuum, indicating that those 2 disorders provided more information about more severe forms of externalizing.
COMMENT
The purpose of these analyses was to explicitly compare continuous and categorical models of externalizing liability in a large, representative epidemiological sample. In the entire sample, as well as in females and males separately, the best-fitting model was a continuous normal trait model. Moreover, in the entire sample as well as in each sex group, the next best-fitting models were also trait models, indicating that continuous conceptions of externalizing liability provided substantial gains in fit over categorical conceptions of externalizing liability, as represented by latent class models. Overall, the modeling results presented here suggest that externalizing liability is a continuum that is normal in distribution.
The current results replicate previous results from a smaller sample15 in indicating that externalizing liability is best modeled as continuous normal in distribution. In that sample as in this one, the best-fitting models were trait models and the best-fitting model was a continuous normal model. The current results extend results of the previous study by using a much larger sample that was designed to be nationally representative. The current results also extend results of the previous study to DSM-IV criteria and additional externalizing spectrum disorders. Finally, the current results extend those of the previous study in characterizing the nature of sex differences in the relationship between externalizing liability and disorder; although males and females exhibit the same general relationship between liability and disorder, the overall likelihood of externalizing disorders is elevated in males.
Although the findings presented here replicate findings in another, complimentary study,15 limitations of the current work should be noted. First, it should be noted that interviews were conducted by nonclinicians without access to independent sources of information. The distribution of externalizing liability given other sources of information remains an important topic for future research.
Second, it is important to note that the interview data was collected at a single point in time. Longitudinal data providing detailed information about stability and changes in symptomatology over time have proved useful in understanding liability to other forms of psychopathology.36,37 Similar longitudinal data on externalizing disorders would help refine our understanding of externalizing etiology and liability. Combined with a population genetic design (eg, twin, family design), longitudinal data would be especially useful in delineating the genetic and environmental developmental dynamics of externalizing liability. Such a design would help delineate, for example, whether the liability continuum acts early in development to initiate a chain reaction of disorders, or acts relatively constantly throughout development as a predisposition toward externalizing disorders. These two different accounts of externalizing psychopathology cannot be distinguished in the current data set, which contains only cross-sectional information about unrelated individuals.
The results of the current study may differ somewhat from those of the previous study15 in suggesting slightly different interpretations of how externalizing spectrum disorders reflect an underlying continuum of liability. In particular, in the previous study, adult antisocial behavior was the most informative disorder regarding externalizing liability, whereas in the current study, antisocial personality disorder was the second least informative about externalizing liability.
These interpretive differences may be because of differences between the 2 studies in the treatment of child conduct disorder criteria. In the current study, antisocial personality disorder was diagnosed according to DSM-IV criteria, which included child conduct disorder criteria. In the previous study, adult antisocial behavior was diagnosed separately from child conduct disorder, which was the least informative disorder with regard to underlying externalizing liability. Combining the 2 criteria sets in the current study may have decreased the overall informativeness of antisocial personality disorder with regard to externalizing liability. If this is the case, it suggests that the child conduct disorder criteria and adult antisocial behavior criteria are best treated as separate—albeit related—disorders, at least insofar as they reflect an externalizing spectrum. The results of the 2 studies suggest that conduct disorder does not necessarily presage adult antisocial behavior and support recent suggestions38 that conduct disorder not be treated as a prerequisite for diagnosis of adult antisocial disorder.
Despite these limitations and interpretive considerations, the current results greatly clarify the distributional qualities of externalizing liability and provide a framework for further research on externalizing phenomena. The current results also underscore an important observation about liability to mental disorders more generally—that it is possible that underlying liability to discretely assessed disorders may itself be continuous in distribution. It is notable in this regard that the dichotomous externalizing disorders are best modeled as having a continuous liability distribution—a finding which emphasizes the distinction between assessed behavior and underlying liability.
Current results indicate that general externalizing liability is best conceptualized as a continuum, with current disorders representing extremes of this continuum. The conclusion that externalizing disorders represent extremes of a continuum is not necessarily inconsistent with current diagnostic practice, as it is possible to conceive of current diagnoses as being thresholds along continua of severity. However, the existence of a unitary externalizing liability continuum indicates that the externalizing continuum itself is an important target for research and treatment, in addition to its manifestations in particular disorders. Moreover, to the extent that externalizing disorders represent extremes of a continuum, assessing less severe forms of externalizing phenomena along a graded range is likely to provide important information about pathology and functioning. This additional information might be lost if pathology were only assessed at the level represented by current diagnostic criteria. It is important that diagnostic systems recognize a common, superordinate externalizing liability, and that this liability is best assessed along a graded range of severity.
The current results provide a framework for examining the etiology of externalizing disorders. Recent studies have documented the importance of studying general externalizing liability in addition to its specific manifestations. These studies have indicated that the general liability toward externalizing spectrum disorders is highly heritable,11,39 and that this liability therefore represents an important focus for molecular genetic and neurobiological research on the etiology of externalizing spectrum disorders. Although our results do not directly address externalizing etiology, they do provide phenotypic clues for possible targets of etiologic research. For example, our results reinforce the importance of neurobiological factors affecting multiple externalizing disorders simultaneously, including substance use and antisocial behavior disorders. The ventromedial prefrontal cortex is an example of a neural region that might be targeted for further research on general externalizing liability, as it has been implicated in both substance use40 and antisocial behavior disorders.41,42
Our results indicate that molecular genetic, neurobiological, and other etiologic studies focusing on general externalizing liability are likely to be most informative if they target underlying liability as a continuum, rather than a set of discrete groups of risk. Our results also help define degrees of severity along the externalizing spectrum, which may be useful for extreme-group designs sometimes used in expensive molecular genetic or neurobiological studies.43,44 In particular, our results document the differential informativeness of various disorders along different ranges of the externalizing continuum, and suggest that different disorders may be differentially useful for examining different points on the liability distribution.
It is important to note that the continuous nature of externalizing liability does not preclude establishment of discrete categories for clinical treatment decisions. In many fields, thresholds of risk along a continuum are established according to levels of increased risk for adverse outcomes (eg, blood pressure ranges). It is possible to establish similar thresholds of externalizing liability according to levels of increased risk for adverse outcomes. These thresholds of outcome risk might then be used to target individual treatments according to level of externalizing liability.
It is also important to emphasize that the existence of an externalizing liability continuum should not be construed to suggest that individual disorders do not possess meaningful information in themselves. Although externalizing disorders are influenced by a common liability continuum, they also contain important unique variance. This conclusion is supported by various population and molecular genetic studies. Population genetic analyses of externalizing disorders demonstrate the presence of genetic influences that act on specific externalizing disorders, in addition to genetic influences that act on general externalizing liability.10,11,45 Molecular genetic studies also support this conclusion, demonstrating that in addition to genetic influences on general externalizing liability, substance use disorders are influenced by genes regulating the metabolism of specific substances.46–50 These converging lines of evidence suggest that research into the etiology of externalizing disorder is likely to be most successful when general externalizing liability is studied jointly with unique liabilities to specific externalizing disorders.
It is noteworthy in this regard that the models used here to delineate relationships between externalizing disorders and general externalizing liability could also be used to delineate relationships between symptoms of each externalizing disorder and its unique liability. Such an approach would aid in understanding what symptoms are most strongly related to general externalizing liability, and what symptoms characterize unique liabilities to specific forms of externalizing psychopathology. Characterizing manifestations of general externalizing liability, unique liabilities to specific forms of externalizing, and relationships between the two, will help better define phenotypic targets for etiologic and treatment research.
Acknowledgments
Funding/Support:This study was supported in part by grant MH65137 from the United States Public Health Service.
References
- 1.Swanson MC, Bland RC, Newman SC. Epidemiology of psychiatric disorders in Edmonton: antisocial personality disorders. Acta Psychiatr Scand Suppl. 1994;376:63–70. [PubMed] [Google Scholar]
- 2.Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: data from the Australian National Survey of Mental Health and Well-Being. Br J Psychiatry. 2002;181:306–314. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- 3.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 4.Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the united states: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- 5.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 6.Wolf AW, Schubert DS, Patterson MB, Grande TP, Brocco KJ, Pendleton L. Associations among major psychiatric diagnoses. J Consult Clin Psychol. 1988;56:292–294. doi: 10.1037//0022-006x.56.2.292. [DOI] [PubMed] [Google Scholar]
- 7.Achenbach TM. The classification of children’s psychiatric symptoms: a factor-analytic study. Psychol Monogr. 1966;80:1–37. doi: 10.1037/h0093906. [DOI] [PubMed] [Google Scholar]
- 8.Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 9.Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112:437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- 10.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 11.Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–424. [PubMed] [Google Scholar]
- 12.Haertel EH. Continuous and discrete latent structure models for item response data. Psychometrika. 1990;55:477–494. [Google Scholar]
- 13.Vermunt JK. The use of restricted latent class models for defining and testing nonparametric and parametric item response theory models. Appl Psychol Meas. 2001;25:283–294. [Google Scholar]
- 14.Markon KE, Krueger RF. A modeling approach to distinguishing between discrete and continuous forms of psychopathology. Paper presented at: 19th Annual Meeting of the Society for Research in Psychopathology; October 10, 2004; St Louis, Mo. [Google Scholar]
- 15.Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. J Abnorm Psychol. doi: 10.1037/0021-843X.114.4.537. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 17.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the united states: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 18.Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version. Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 19.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the alcohol use disorder and associated disabilities interview schedule-Alcohol/Drug-revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47:171–185. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- 20.Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D. Concordance of the DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47:195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- 21.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 22.Grant BF, Harford TC, Dawson DD, Chou PS. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- 23.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- 24.Heinen T. Latent Class and Discrete Latent Trait Models: Similarities and Differences. Thousand Oaks, Calif: Sage Publications Inc; 1996. [Google Scholar]
- 25.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–464. [Google Scholar]
- 26.Raftery AE. Bayesian model selection in structural equation models. In: Bollen KA, Long S, editors. Testing Structural Equation Models. Newbury Park, Calif: Sage Publications; 1993. pp. 163–180. [Google Scholar]
- 27.Barron AR, Cover TM. Minimum complexity density estimation. IEEE Trans Inform Theory. 1991;37:1034–1054. [Google Scholar]
- 28.Vereshchagin NK, Vitanyi PMB. Kolmogorov’s structure functions and model selection. IEEE Trans Inform Theory. 2004;50:3265–3290. [Google Scholar]
- 29.Vermunt JK, Magidson J. Latent GOLD 4.0: Basic and Advanced Belmont Mass. Statistical Innovations; 2005. [Google Scholar]
- 30.Vermunt JK. Comments on latent class analysis of complex sample survey data. J Am Stat Assoc. 2002;97:736–737. [Google Scholar]
- 31.Wedel M, ter Hofstede F, Steenkamp JEM. Mixture model analysis of complex samples. Journal of Classification. 1998;15:225–244. [Google Scholar]
- 32.Bartholomew DJ, Knott M. Latent Variable Models and Factor Analysis London. England: Arnold; 1999. [Google Scholar]
- 33.Skrondal A, Rabe-Hesketh S. Generalized Latent Variable Modeling: Multilevel, Longitudinal, and Structural Equation Models. Boca Raton, Fla: Chapman & Hall/CRC; 2004. [Google Scholar]
- 34.Kessler RC, Paton SM, Kandel DB. Reconciling unidimensional and multidimensional models of patterns of drug use. J Stud Alcohol. 1976;37:632–647. doi: 10.15288/jsa.1976.37.632. [DOI] [PubMed] [Google Scholar]
- 35.Kirisci L, Vanyukov M, Dunn M, Tarter R. Item response theory modeling of substance use: an index based on 10 drug categories. Psychol Addict Behav. 2002;16:290–298. [PubMed] [Google Scholar]
- 36.Duncan-Jones P, Fergusson DM, Ormel J, Horwood LJ. A model of stability and change in minor psychiatric symptoms: results from three longitudinal studies. Psychol Med Monogr Suppl. 1990;18:1–28. doi: 10.1017/s0264180100000813. [DOI] [PubMed] [Google Scholar]
- 37.Ormel J, Schaufeli WB. Stability and change in psychological distress and their relationship with self-esteem and locus of control: a dynamic equilibrium model. J Pers Soc Psychol. 1991;60:288–299. doi: 10.1037//0022-3514.60.2.288. [DOI] [PubMed] [Google Scholar]
- 38.Krueger RF. Continuity of axes I and II: toward a unified model of personality, personality disorders, and clinical disorders. J Personal Disord. 2005;19:233–261. doi: 10.1521/pedi.2005.19.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: a twin-family study. Arch Gen Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- 40.Davidson RJ, Putnam KM, Larson CL. Dysfunction in the neural circuitry of emotion regulation—a possible prelude to violence. Science. 2000;289:591–594. doi: 10.1126/science.289.5479.591. [DOI] [PubMed] [Google Scholar]
- 41.Best M, Williams JM, Coccaro EF. Evidence for a dysfunctional prefrontal circuit in patients with an impulsive aggressive disorder. Proc Natl Acad Sci U S A. 2002;99:8448–8453. doi: 10.1073/pnas.112604099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.London ED, Ernst M, Grant S, Bonson K, Weinstein A. Orbitofrontal cortex and human drug abuse: functional imaging. Cereb Cortex. 2000;10:334–342. doi: 10.1093/cercor/10.3.334. [DOI] [PubMed] [Google Scholar]
- 43.Risch N, Zhang H. Extreme discordant sib pairs for mapping quantitative trait loci in humans. Science. 1995;268:1584–1589. doi: 10.1126/science.7777857. [DOI] [PubMed] [Google Scholar]
- 44.Abecasis GR, Cookson WO, Cardon LR. The power to detect linkage disequilibrium with quantitative traits in selected samples. Am J Hum Genet. 2001;68:1463–1474. doi: 10.1086/320590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsuang MT, Lyons MJ, Meyer JM, Doyle T, Eisen SA, Goldberg J, True W, Lin N, Toomey R, Eaves L. Co-occurrence of abuse of different drugs in men: the role of drug-specific and shared vulnerabilities. Arch Gen Psychiatry. 1998;55:967–972. doi: 10.1001/archpsyc.55.11.967. [DOI] [PubMed] [Google Scholar]
- 46.Whitfield JB. Meta-analysis of the effects of alcohol dehydrogenase genotype on alcohol dependence and alcoholic liver disease. Alcohol Alcohol. 1997;32:613–619. doi: 10.1093/oxfordjournals.alcalc.a008303. [DOI] [PubMed] [Google Scholar]
- 47.Butt CM, King NM, Hutton SR, Collins AC, Stitzel JA. Modulation of nicotine but not ethanol preference by the mouse Chrna4 A529T polymorphism. Behav Neurosci. 2005;119:26–37. doi: 10.1037/0735-7044.119.1.26. [DOI] [PubMed] [Google Scholar]
- 48.Wang JC, Hinrichs AL, Stock H, Budde J, Allen R, Bertelsen S, Kwon JM, Wu W, Dick DM, Rice J, Jones K, Nurnberger JI, Jr, Tischfield J, Porjesz B, Edenberg HJ, Hesselbrock V, Crowe R, Schuckit M, Begleiter H, Reich T, Goate AM, Bierut LJ. Evidence of common and specific genetic effects: association of the muscarinic acetylcholine receptor M2 (CHRM2) gene with alcohol dependence and major depressive syndrome. Hum Mol Genet. 2004;13:1903–1911. doi: 10.1093/hmg/ddh194. [DOI] [PubMed] [Google Scholar]
- 49.Sipe JC, Chiang K, Gerber AL, Beutler E, Cravatt BF. A missense mutation in human fatty acid amide hydrolase associated with problem drug use. Proc Natl Acad Sci U S A. 2002;99:8394–8399. doi: 10.1073/pnas.082235799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lappalainen J, Kranzler HR, Malison R, Price LH, Van Dyck C, Rosenheck RA, Cramer J, Southwick S, Charney D, Krystal J, Gelernter J. A functional neuropeptide Y Leu7Pro polymorphism associated with alcohol dependence in a large population sample from the United States. Arch Gen Psychiatry. 2002;59:825–831. doi: 10.1001/archpsyc.59.9.825. [DOI] [PubMed] [Google Scholar]