Rabies is one of the oldest recognized diseases affecting humans and one of the most important zoonotic diseases in India. It has been recognized in India since the Vedic period (1500–500 BC) and is described in the ancient Indian scripture Atharvaveda, wherein Yama, the mythical God of Death, has been depicted as attended by 2 dogs as his constant companions, the emissaries of death.1 Rabies is endemic in India, a vast country with a population exceeding 1.02 billion and a land area of 3.2 million km2.2
Rabies is primarily a disease of terrestrial and airborne mammals, including dogs, wolves, foxes, coyotes, jackals, cats, bobcats, lions, mongooses, skunks, badgers, bats, monkeys and humans. The dog has been, and still is, the main reservoir of rabies in India.3 Other animals, such as monkeys, jackals, horses, cattle and rodents, seem to bite incidentally on provocation, and the fear of rabies leads the victim to seek postexposure prophylaxis. The number of cases involving monkey bites has been increasing in the last few years. Monkeys are susceptible to rabies, and their bites necessitate postexposure prophylaxis.
Incidence of human rabies
Human rabies has been eradicated in some developed countries, but it is still present in many others, including those in Southeast Asia (Figure 1).4
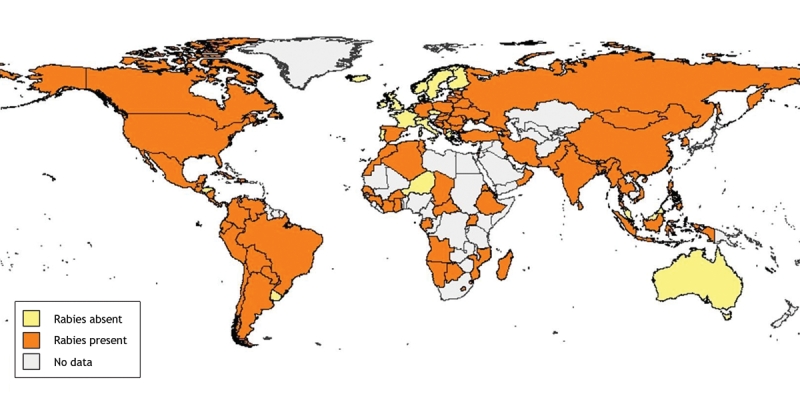
Figure 1: Presence and absence of rabies worldwide, 2006.4 Reproduced with permission from the World Health Organization.
In India, about 15 million people are bitten by animals, mostly dogs, every year and need postexposure prophylaxis. Since 1985, India has reported an estimated 25 000–30 000 human deaths from rabies annually (the lower estimate is based on projected statistics from isolation hospitals in 1985).2 The majority of people who die of rabies are people of poor or low-income socioeconomic status.3 The incidence of death from rabies in Asia is given in Figure 2.5 Because rabies is not a notifiable disease in India and there is no organized surveillance system of human or animal cases, the actual number of deaths may be much higher. The latest figure projected from the National Multicentric Rabies Survey, conducted in 2004 by the Association for Prevention and Control of Rabies in India in collaboration with the World Health Organization,1 is 20 565 deaths from rabies per year.
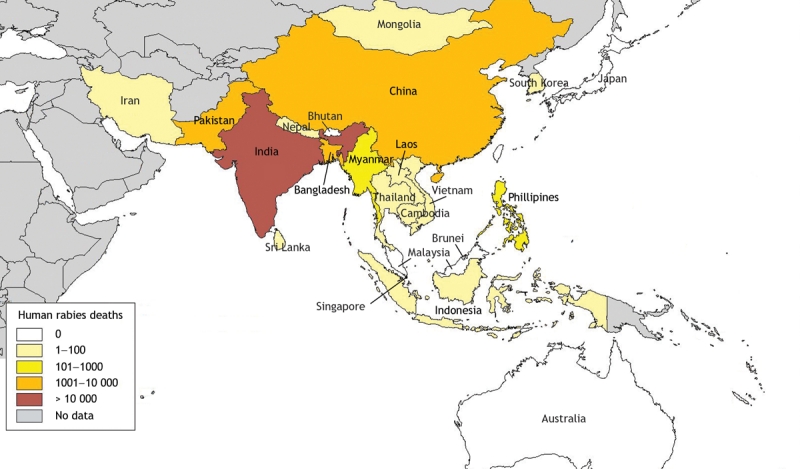
Figure 2: Incidence of human deaths from rabies in Asia, 2004.5 Reproduced with permission from the World Health Organization.
Most animal bites in India (91.5%) are by dogs, of which about 60% are strays and 40% pets. The incidence of animal bites is 17.4 per 1000 population. A person is bitten every 2 seconds, and someone dies from rabies every 30 minutes. The annual number of person-days lost because of animal bites is 38 million, and the cost of post-bite treatment is about $25 million.2
The steady increase in the number of cases involving dog bites and an ever-increasing demand for postexposure vaccination poses the question of whether India is in the midst of an epidemic of rabies in dogs or whether these increases merely reflect uncontrolled growth in the dog population and greater number of humans exposed to them.
Management of stray dog population
India has approximately 25 million dogs, with an estimated dog:man ratio of 1:36.2 The dogs fall into 4 broad categories: pets (restricted and supervised); family dogs (partially restricted, wholly dependent); community dogs (unrestricted, partially dependent); and feral dogs (unrestricted, independent). Most dogs in India, perhaps 80%, would fall into the last 3 categories.6
Until 1998 the population of stray dogs in India was kept under check by civic authorities, by impounding and euthanizing unclaimed dogs. Because of pressure from animal welfare activists, this approach was replaced by a policy of animal birth control, also referred to as the ABC Programme. In this program, stray dogs are impounded, surgically sterilized and released back into the area from where they were picked up. The success of this program hinges on the sterilization of 70% of the strays in a given geographic area within 6 months, before the next reproductive cycle begins, otherwise the entire effort is negated. This target is difficult to achieve, given the large number of strays and the limited resources. Hence the success of the animal birth control program in controlling the stray dog population is a subject of dispute and doubt.6
Diagnosis of rabies
In most cases, human rabies is diagnosed primarily on the basis of clinical symptoms and signs, and a corroborative history of or evidence of an animal bite, death of an animal, and incomplete or no vaccination following exposure.2 The facility for laboratory diagnosis and confirmation of rabies, be it in humans or in animals, is available premortem in only a few institutions in India. The standard premortem test is a fluorescent antibody test to demonstrate the presence of viral antigen. The standard postmortem test is biopsy of the patient's brain and examination for Negri bodies. Autopsies are rarely performed.
Use of vaccines and immune globulin
Twelve institutions in India were producing the nerve-tissue (Semple) vaccine in quantities necessary for use in humans (40 million mL) and animals (90 million mL) annually until 2003/04. Since then, the use of the nerve-tissue vaccine has been phased out and, as of 2008, replaced by modern tissue-culture vaccine.7 Most people received the vaccine at government and municipal anti-rabies clinics. Each case required a mean of 4.4 visits for treatment, at a cost of at least Can$50 (for the vaccine and other medicines) and a loss of 2.2 days of work.2
In the past, a large proportion of rabies patients did not receive any vaccination, and of those who did, many did not complete the full course. In the latest survey, in 2004, only 39.5% of bite victims washed the wounds with soap and water, and about 46.9% received rabies vaccination. The survey revealed that the use of tissue-culture vaccine was higher than that of nerve-tissue vaccine, and compliance to the full course was about 40.5%. However, the use of human rabies immune globulin was low (2.1%).
The 2004 survey also revealed that about 60% of infected people resort to indigenous treatment, with local applications to the wound (36.8%) and indigenous remedies (45.3%) being popular.2
Realizing that even at the dawn of 21st century thousands of people in India are dying from rabies, some of the medical professional bodies such as the Indian Academy of Pediatrics and the Association for the Prevention and Control of Rabies have taken action. They have collaborated to create awareness, develop strategies suitable to the Indian situation, popularize the use of intradermal vaccination, with a view to reduce the high cost of treatment and cooperate with the government to reduce the incidence of death from rabies, with the ultimate goal of eradicating rabies from the country.
Recommendations
To first reduce then eradicate deaths from rabies, collaborative efforts will be required from multiple stakeholders, including veterinarians, public health officials, legal authorities and other health care services (Box 1).
Box 1.

There must be strict implementation of the legal provisions for licensing and regular vaccination of pet dogs. At the same time, dedicated efforts are needed to control the population of stray dogs, through animal birth control programs and mass vaccination, and to eliminate suspected infected animals.
Public health educational programs are needed to create awareness both in the medical community and in the public regarding the dangers of inadequately managed animal bites. The importance of proper wound care, postexposure vaccination with modern tissue-culture vaccine and the administration of human rabies immune globulin, where indicated, must be reinforced.
Modern tissue-culture vaccines, which are currently administered intramuscularly, must be made more widely and easily accessible. Efforts are needed to lower the prohibitive costs of postexposure vaccination by introducing and popularizing the intradermal route of rabies vaccination, which requires just one-tenth of the intramuscular dose. The possibility of adding pre-exposure vaccination to the routine childhood immunization schedule should be considered.
The facilities for the surveillance and diagnosis of animal rabies must be improved in quality and offer wider coverage, and human rabies must be made a mandatory reportable disease.
Rozario Menezes MD Chief Medical Officer (retired) Mormugao Port Authority Consultant, Pediatrics Dr. M.M. Mesquita Hospital Vasco-da-Gama, India
@ See related articles pages 557, 562 and 567
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
REFERENCES
- 1.Deshmukh RA. Rabies. Pune (India): Yogaksema Department of Virology, Haffkine Institute; 2004.
- 2.Sudarshan MK. Assessing burden of rabies in India. WHO sponsored national multi-centric rabies survey (May 2004). Assoc Prev Control Rabies India J 2004;6:44-5.
- 3.Ghosh TK. Rabies. Proceedings of the IX National Conference of Pediatric Infectious Diseases; 2006; Chennai, India.
- 4.Presence/absence of rabies worldwide — 2006. Geneva: Department of Food Safety, Zoonoses and Foodborne diseases, World Health Organization; 2008. Available: www.who.int/rabies/rabies_maps/en/index.html (accessed 2008 Jan 28).
- 5.Human rabies deaths — 2004. Geneva: Department of Food Safety, Zoonoses and Foodborne diseases, World Health Organization; 2008. Available: www.who.int/rabies/rabies_maps/en/index.html (accessed 2008 Jan 28).
- 6.Chaudhuri S. Rabies prevention and dog population management. India's official dog control policy in context of WHO guidelines. Ecollage; 2005.
- 7.John TJ. An ethical dilemma in rabies immunisation. Vaccine 1997;15 Suppl:S12-5. [DOI] [PubMed]


