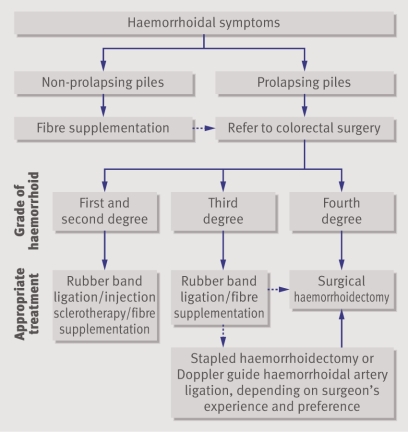
Haemorrhoids or “piles” are enlarged vascular cushions within the anal canal that have been described for many centuries and continue to form a large part of a colorectal surgeon’s workload. The exact incidence of this common condition is difficult to estimate as many people are reluctant to seek medical advice for various personal, cultural, and socioeconomic reasons, but epidemiological studies report a prevalence varying from 4.4% in adults in the United States to over 30% in general practice in London.1 2 The treatment of haemorrhoids is still evolving, and this article provides an update on the role of established and innovative treatments (fig 1).
Fig 1 Suggested algorithm for management of haemorrhoids (dotted arrows indicate failure of initial treatment)
Sources and selection criteria
Articles were retrieved from the Medline database and Cochrane library under the MeSH subheadings “hemorrhoid” and “haemorrhoid”. We included randomised controlled trials and meta-analyses.
Summary points
Haemorrhoids are enlarged vascular cushions in the anal canal
Treatment depends on the degree of prolapse and severity of symptoms
Rubber band ligation is the best outpatient treatment for haemorrhoids—up to 80% of patients are satisfied with the short term outcome
Surgery is reserved for large symptomatic haemorrhoids that do not respond to outpatient treatment
Doppler guided haemorrhoidal artery ligation and stapled haemorrhoidopexy are new alternatives to the traditional and more painful open or closed haemorrhoidectomy
What is the pathogenesis and aetiology?
The anal canal consists of three fibrovascular cushions that are fed directly by arteriovenous communications. These cushions are supported within the anal canal by a connective tissue framework, and they are important in providing a watertight seal to the anus. The degenerative effects of ageing may weaken or fragment the supporting tissues, and this along with the repeated passage of hard stool and straining produces a shearing force on the cushions, leading to their descent and prolapse. The prolapsed cushions have impaired venous return, which results in engorgement that may be further exacerbated by straining, inadequate fibre intake, prolonged time on the lavatory, and conditions such as pregnancy that raise intra-abdominal pressure. Bleeding from the engorged prolapsed haemorrhoid occurs as a result of localised mucosal trauma or inflammation, which damages the underlying blood vessels.3
How are haemorrhoids classified?
Haemorrhoids can be classified according to their relation to the dentate (pectinate) line, which demarcates the transition from the squamous epithelium below to the columnar epithelium above. Internal haemorrhoids originate above the dentate line, whereas external haemorrhoids originate below the line. The more widely used Goligher classification system describes four grades, which are based on the degree of prolapse, but this system fails to reflect the severity of the symptoms.4 The grade of haemorrhoid is important (box) and can be useful in deciding optimal treatment or in evaluating the effectiveness of the treatment given.
Different grades of haemorrhoids
First degree haemorrhoids: these bleed but do not prolapse
Second degree haemorrhoids: these prolapse but reduce spontaneously
Third degree haemorrhoids: these prolapse but can be reduced manually
Fourth degree haemorrhoids: these are permanently prolapsed and cannot be reduced
How do haemorrhoids present and how should they be assessed?
The most common symptom is painless fresh rectal bleeding, but patients may also experience pruritus, swelling, prolapse, discharge, or soiling. Severe anal pain is usually seen only if the haemorrhoid is thrombosed or strangulated.
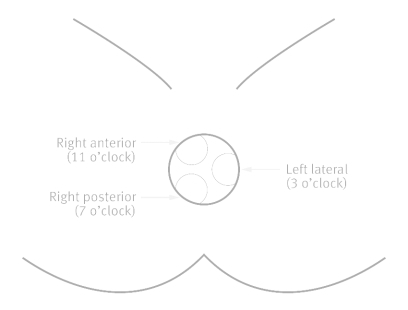
Initial examination involves inspection of the perineum followed by rectal examination and anoscopy. This will help differentiate haemorrhoids from other causes of anal canal bleeding such as fissures, fistulas, tumour, polyps, anal warts, and rectal prolapse. Large external haemorrhoids can be easily seen on inspection, but anoscopy allows the haemorrhoidal cushions to be more easily visualised in the usual left lateral, right anterior, and right posterior positions (3 o’clock, 7 o’clock, and 11 o’clock positions; fig 2). Patients older than 40 who have suspected haemorrhoidal bleeding generally require additional flexible sigmoidoscopy, colonoscopy, virtual colonoscopy, or a barium enema to exclude colorectal carcinomas and should always be referred for a specialist opinion.
Fig 2 Usual position of haemorrhoids when patient is in supine position with legs in stirrups
Haemorrhoidal disease associated with the symptoms of soiling or incontinence may require anorectal physiology studies and endoanal ultrasound, particularly if the patient is being considered for surgery. These patients have a higher risk of developing incontinence after surgery, and these investigations may help the surgeon choose the best treatment option.
Tips for non-specialists
Haemorrhoids are common in all age groups
Most patients can be treated in primary care with dietary advice and avoidance of straining
Patients with rectal bleeding alone who are over 40 should be referred to a specialist for imaging of the colon
All patients with haemorrhoids who have symptoms in the lower gastrointestinal tract—such as change in bowel habit, abdominal pain, or tenesmus—must be referred to a specialist
Anal cancer can have a similar appearance to a prolapsed haemorrhoid
How are haemorrhoids treated?
Conservative treatment
A recent meta-analysis confirmed that fibre supplements moderately improve overall symptoms and bleeding and should be recommended at an early stage.5 Other lifestyle modifications such as improving anal hygiene, taking sitz baths, increasing fluid intake, relieving constipation, and avoiding straining are used in primary care and may help in the treatment and prevention of haemorrhoids, although the evidence for this is lacking.
Over the counter topical preparations that contain a combination of local anaesthetics, corticosteroids, astringents, and antiseptics are available, and these can alleviate symptoms of pruritus and discomfort in haemorrhoidal disease. Long term use of these agents should be discouraged, particularly steroid creams, which can permanently damage or cause ulceration of the perianal skin. No randomised controlled trials are available to support their widespread use.
Venotonics such as flavonoids have been used as dietary supplements in the treatment of haemorrhoids. The mechanism of action of these drugs remains unclear, but they may improve venous tone, reduce hyperpermeability, and have anti-inflammatory effects. This treatment is popular in continental Europe and the Far East, but a recent meta-analysis concluded that limitations in methodological quality and potential publication bias raise doubts about the benefits of these agents in treating haemorrhoids.6
Outpatient treatments
Several outpatient interventions that have been available for many years remain popular in the treatment of first degree, second degree, and third degree haemorrhoids. These office based procedures cause tissue loss and ulceration or help, by causing fibrosis, to fix the mucosa of the prolapsed tissue back on to the underlying muscle.
Rubber band ligation
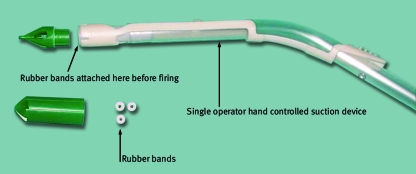
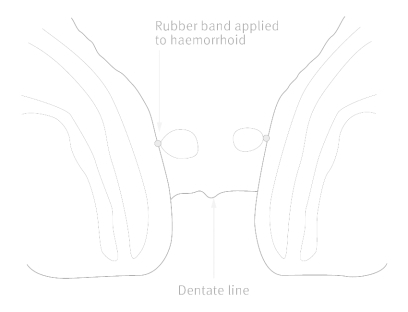
The technique of applying rubber bands to haemorrhoids was first described in 1963.7 Modification of the original method through the introduction of suction bands has allowed this procedure to be performed by a single operator (figs 3 and 4) . The original paper suggested that one haemorrhoid should be banded during each session, with repeat bandings at three week intervals. Subsequent prospective studies showed no increase in post ligation pain or complications with multiple banding, however, so many surgeons apply up to three bands at each visit.8 9 The bands should be applied above the dentate line to minimise pain, and injecting local anaesthetic into the banded haemorrhoids does not seem to reduce anal discomfort.10
Fig 3 Rubber band ligation. Suction banding equipment used for applying rubber bands to haemorrhoids
Fig 4 Rubber band ligation of two haemorrhoids. Care must be taken when applying rubber bands to avoid including sensitive skin (below the dentate line) in a band
Most large trials and a meta-analysis in 1995 suggest that rubber band ligation is the most effective outpatient treatment for haemorrhoids, with some authors suggesting that up to 80% of patients are satisfied with the short term outcome.11
Common complications of the procedure include pain and haemorrhage. All patients should be warned about the possibility of delayed haemorrhage (five to 10 days after the procedure), and the technique is contraindicated in those who are anticoagulated. Other rarely reported complications include urinary retention, liver abscesses, and perineal sepsis.12
Injection sclerotherapy
A submucosal injection of 5% oily phenol into first or second degree haemorrhoids is an alternative to banding. It has no benefit in large prolapsing haemorrhoids or those with a large external component. It is cheap and easy to perform, but it is less widely used than banding because of the high failure rate. Conservative treatment with fibre supplementation may be as effective as injection sclerotherapy.13 Complications with sclerosants are rare but include local infections, prostatitis, portal pyaemia, and erectile dysfunction.14
Other techniques
Infrared coagulation can be used to treat first or second degree haemorrhoids. Although it is associated with few complications it seems to be less effective than banding and is not widely used.15 Cryosurgery, bipolar diathermy, and direct current electrotherapy have been used, but little evidence exists to support these techniques.
Surgery
Open and closed haemorrhoidectomy
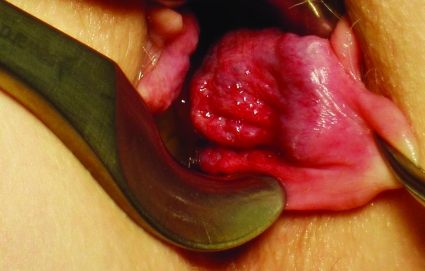
Surgery is reserved for large symptomatic haemorrhoids that have not responded to outpatient treatment (fig 5). Only a small proportion of patients referred to a coloproctologist for treatment of haemorrhoids receive surgery. The open technique for performing surgical excision of the vascular cushions was first described in 1937. This technique is popular in the United Kingdom. The haemorrhoid is dissected out from the underlying anal sphincter complex using electrocauterisation, laser surgery, the ligasure vessel sealing system, the harmonic scalpel (an ultrasonic cutting and coagulating device), or scissors. The vascular pedicle is controlled and the mucosal defects are left open and allowed to granulate by secondary intention. The closed technique, first described in 1959,16 is more popular in the United States. It is similar to the open technique, but the mucosal edges and skin are closed with a continuous suture. Both of these techniques are safe and effective, but the closed haemorrhoidectomy promotes faster wound healing.17
Fig 5 Large symptomatic haemorrhoid in the left lateral position that has not responded to outpatient treatment and is suitable for haemorrhoidectomy
Surgical haemorrhoidectomy is a painful procedure, which is increasingly being performed on a day case basis. It is important to prescribe a careful perioperative pain package. In addition to perioperative local anaesthetics and analgesics, laxatives help to reduce pain during the first postoperative motion. Prophylactic oral metronidazole,18 topical diltiazem,19 topical glyceryl trinitrate, or injected botulinum toxin20have marginal benefit in reducing pain after surgery. Complications include secondary haemorrhage (seven to 10 days after surgery), urinary retention, infection, faecal incontinence as a result of sphincter damage, and anal stenosis—usually as a result of inadequate mucosal bridges.
Doppler guided haemorrhoidal artery ligation
This technique for treating haemorrhoids was first described in 1995. It is performed using a specially designed proctoscope with an inbuilt Doppler probe that can locate feeding arteries; these vessels are then ligated using absorbable sutures. Disrupting the inflow to the vascular cushion is thought to reduce the size of the haemorrhoid. The technique is relatively painless, with minimal morbidity, and up to 60% of patients in the larger studies are satisfied with the outcome.21 Further randomised controlled trials are needed, but this offers a less mutilating alternative to surgical haemorrhoidectomy and has become popular throughout Europe during the past five years.
Stapled haemorrhoidopexy
This technique was developed in the 1990s. It is carried out using a specially designed transanal circular stapling gun that reduces prolapse by excising a circumferential ring of mucosa approximately 2-3 cm above the dentate line. This not only shortens or “hitches up” the prolapsed mucosa but also interrupts the feeding arteries to the haemorrhoid in a similar manner to Doppler guided haemorrhoidal artery ligation.
When it was developed, it was claimed that this technique would be as effective as and less painful than conventional haemorrhoidectomy and that recovery would be quicker. More than 25 randomised controlled trials have compared stapled haemorrhoidopexy with conventional haemorrhoidectomy, although many of these have a small sample size. The evidence from a recent meta-analysis suggests that the procedure is less painful and safe, and that hospital stay is shorter, with a more rapid return to normal activities.22 Long term follow-up studies suggest that recurrence rates are higher after stapled haemorrhoidopexy than after conventional haemorrhoidectomy.23 One early trial reported severe postoperative pain and faecal urgency after the stapled procedure, however, but this has not been seen in other studies.24 Other possible complications include bleeding, urinary retention, faecal incontinence rectal perforation, rectovaginal fistulas, anastomotic leak, anal stricture, and severe pelvic sepsis.14
This technique can be offered to patients with second or third degree haemorrhoids that have not responded to outpatient treatment or even fourth degree haemorrhoids that are reducible under anaesthesia. It is a less painful alternative, but patients must be fully informed about recurrence rates and complications.
Acutely thrombosed haemorrhoids
Acutely thrombosed prolapsed haemorrhoids are very painful but most can be treated at home and usually settle within 10-14 days using ice packs, stool softeners, and analgesia. Topical calcium antagonists may help to relieve the pain.25 Emergency surgery may be needed in severe cases to remove the engorged haemorrhoid or debride necrotic tissue. This can resolve symptoms more rapidly but is often associated with severe morbidity.26
Additional educational resources
Hardy A, Chan CL, Cohen CR. The surgical management of haemorrhoids—a review. Dig Surg 2005;22:26-33
Kaidar-Person O, Person B, Wexner SD. Hemorrhoidal disease: a comprehensive review. J Am Coll Surg 2007;204:102-17
American Society of Colon and Rectal Surgeons (www.fascrs.org/displaycommon.cfm?an=1&subarticlenbr=315 )—Information on haemorrhoids
Patients UK (www.patient.co.uk/showdoc/23068749/)—Information for patients on haemorrhoids
NHS Direct (www.nhsdirect.nhs.uk/articles/article.aspx?articleId=184)—Information for patients on haemorrhoids
Contributors: JHS wrote the section on surgery and AGA wrote the rest of the article. AGA is guarantor.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.Gazet JC, Redding W, Rickett JW. The prevalence of haemorrhoids. A preliminary survey. Proc R Soc Med 1970;63(suppl):78-80. [PMC free article] [PubMed] [Google Scholar]
- 2.Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology 1990;98:380-6. [DOI] [PubMed] [Google Scholar]
- 3.Thomson WH. The nature of haemorrhoids. Br J Surg 1975;62:542-52. [DOI] [PubMed] [Google Scholar]
- 4.Thomson JPS, Leicester RJ, Smith LE. Haemorrhoids. In: Coloproctology and the pelvic floor 2nd ed. 1992:373-93.
- 5.Alonso-Coello P, Mills E, Heels-Ansdell D, Lopez-Yarto M, Zhou Q, Johanson JF, et al. Fiber for the treatment of hemorrhoid complications: a systematic review and meta-analysis. Am J Gastroenterol 2006;101:181-8. [DOI] [PubMed] [Google Scholar]
- 6.Alonso-Coello P, Zhou Q, Martinez-Zapata MJ, Mills E, Heels-Ansdell D, Johanson JF, et al. Meta-analysis of flavonoids for the treatment of haemorrhoids. Br J Surg 2006;93:909-20. [DOI] [PubMed] [Google Scholar]
- 7.Barron J. Office ligation treatment of hemorrhoids. Dis Colon Rectum 1963;6:109-13. [DOI] [PubMed] [Google Scholar]
- 8.Khubchandani IT. A randomized comparison of single and multiple rubber band ligations. Dis Colon Rectum 1983;26:705-8. [DOI] [PubMed] [Google Scholar]
- 9.Poon GP, Chu KW, Lau WY, Lee JM, Yeung C, Fan ST, et al. Conventional vs. triple rubber band ligation for hemorrhoids. A prospective, randomized trial. Dis Colon Rectum 1986;29:836-8. [DOI] [PubMed] [Google Scholar]
- 10.Law WL, Chu KW. Triple rubber band ligation for hemorrhoids: prospective, randomized trial of use of local anesthetic injection. Dis Colon Rectum 1999;42(3):363-6. [DOI] [PubMed] [Google Scholar]
- 11.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum 1995;38:687-94. [DOI] [PubMed] [Google Scholar]
- 12.Chau NG, Bhatia S, Raman M. Pylephlebitis and pyogenic liver abscesses: a complication of hemorrhoidal banding. Can J Gastroenterol 2007;21:601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Senapati A, Nicholls RJ. A randomised trial to compare the results of injection sclerotherapy with a bulk laxative alone in the treatment of bleeding haemorrhoids. Int J Colorectal Dis 1988;3:124-6. [DOI] [PubMed] [Google Scholar]
- 14.Guy RJ, Seow-Choen F. Septic complications after treatment of haemorrhoids. Br J Surg 2003;90:147-56. [DOI] [PubMed] [Google Scholar]
- 15.Walker AJ, Leicester RJ, Nicholls RJ, Mann CV. A prospective study of infrared coagulation, injection and rubber band ligation in the treatment of haemorrhoids. Int J Colorectal Dis 1990;5:113-6. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson JA, Heaton JR. Closed hemorrhoidectomy. Dis Colon Rectum 1959;2:176-9. [DOI] [PubMed] [Google Scholar]
- 17.Ho YH, Buettner PG. Open compared with closed haemorrhoidectomy: meta-analysis of randomized controlled trials. Tech Coloproctol 2007;11:135-43. [DOI] [PubMed] [Google Scholar]
- 18.Carapeti EA, Kamm MA, McDonald PJ, Phillips RK. Double-blind randomised controlled trial of effect of metronidazole on pain after day-case haemorrhoidectomy. Lancet 1998;351:169-72. [DOI] [PubMed] [Google Scholar]
- 19.Silverman R, Bendick PJ, Wasvary HJ. A randomized, prospective, double-blind, placebo-controlled trial of the effect of a calcium channel blocker ointment on pain after hemorrhoidectomy. Dis Colon Rectum 2005;48:1913-6. [DOI] [PubMed] [Google Scholar]
- 20.Patti R, Almasio PL, Arcara M, Sammartano S, Romano P, Fede C, et al. Botulinum toxin vs topical glyceryl trinitrate ointment for pain control in patients undergoing hemorrhoidectomy: a randomized trial. Dis Colon Rectum 2006;49:1741-8. [DOI] [PubMed] [Google Scholar]
- 21.Scheyer M, Antonietti E, Rollinger G, Mall H, Arnold S. Doppler-guided hemorrhoidal artery ligation. Am J Surg 2006;191:89-93. [DOI] [PubMed] [Google Scholar]
- 22.Tjandra JJ, Chan MK. Systematic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy). Dis Colon Rectum 2007;50:878-92. [DOI] [PubMed] [Google Scholar]
- 23.Jayaraman S, Colquhoun PH, Malthaner RA. Stapled versus conventional surgery for hemorrhoids. Cochrane Database Syst Rev 2006;(4):CD005393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheetham MJ, Mortensen NJ, Nystrom PO, Kamm MA, Phillips RK. Persistent pain and faecal urgency after stapled haemorrhoidectomy. Lancet 2000;356:730-3. [DOI] [PubMed] [Google Scholar]
- 25.Perrotti P, Antropoli C, Molino D, De Stefano G, Antropoli M. Conservative treatment of acute thrombosed external hemorrhoids with topical nifedipine. Dis Colon Rectum 2001;44:405-9. [DOI] [PubMed] [Google Scholar]
- 26.Greenspon J, Williams SB, Young HA, Orkin BA. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum 2004;47:1493-8. [DOI] [PubMed] [Google Scholar]