Abstract
Background
The World Health Organization (WHO) has established a set of items related to study design and administrative information that should build the minimum set of data in a study register. A more comprehensive data set for registration is currently developed by the Ottawa Group. Since nothing is known about the attitudes of academic researchers towards prospective study registration, we surveyed academic researchers about their opinion regarding the registration of study details proposed by the WHO and the Ottawa Group.
Methods
This was a web-based survey of academic researchers currently running an investigator-initiated clinical study which is registered with clinicaltrials.gov. In July 2006 we contacted 1299 principal investigators of clinical studies by e-mail explaining the purpose of the survey and a link to access a 52-item questionnaire based on the proposed minimum data set by the Ottawa Group. Two reminder e-mails were sent each two weeks apart. Association between willingness to disclose study details and study phase was assessed using the chi-squared test for trend. To explore the potential influence of non-response bias we used logistic regression to assess associations between factors associated with non-response and the willingness to register study details.
Results
Overall response was low as only 282/1299 (22%) principal investigators participated in the survey. Disclosing study documents, in particular the study protocol and financial agreements, was found to be most problematic with only 31% of respondents willing to disclose these publicly. Consequently, only 34/282 (12%) agreed to disclose all details proposed by the Ottawa Group. Logistic regression indicated no association between characteristics of non-responders and willingness to disclose details.
Conclusion
Principal investigators of non-industry sponsored studies are reluctant to disclose all data items proposed by the Ottawa Group. Disclosing the study protocol and financial agreements was found to be most problematic. Future discussions on trial registration should not only focus on industry but also on academic researchers.
Background
Since 2005 the International Committee of Medical Journal Editors (ICMJE) has required prospective registration of clinical studies in order to be considered for publication in one of their journals [1]. Moreover, the World Health Organization (WHO) has established a set of items related to study design and administrative information that should form the minimum set of data in a study register [2]. Several stakeholders were consulted on this WHO Trial Registration Data Set including academic researchers, industry and patient representatives. However, several items were highly controversial and industry representatives demanded that some items should not be disclosed during study conduct [3]. Industry representatives argued that some trial information is sensitive for competitive reason and asked for delayed disclosure of some items e.g. the scientific title of a study, primary and secondary outcomes. However, competition is also of increasing importance in academic research [4].
In 2005 the Ottawa Group published principles of trial registration [5] and a minimum data set for registration is currently being developed [6]. This set requires even more details about a study than the WHO Trial Registration Data Set (see Table 1). However, analyses of trial registration in ClinicalTrials.gov showed heterogeneous quality and completeness of the registration entries indicating varying degrees of comfort with different levels of disclosure [7]. Since nothing is known about the attitudes of academic researchers towards prospective study registration, it is unclear if they would comply with an extension of the requested study information. We therefore surveyed academic researchers about their opinions regarding the registration of study details proposed by the Ottawa Group.
Table 1.
Study details required by WHO and Ottawa Group
| WHO Trial Registration Data Set | Ottawa Group Data Set (in addition to WHO items) |
| Trial registration date | Trial acronym |
| Ethics approval | Trial website |
| Funding source(s) | Lay description |
| Primary sponsor | Registration date |
| Secondary sponsor(s) | Date ethical approval |
| Coordinating/principle investigator | Date recruitment end |
| Contact person | Date end of follow-up |
| Coordinating center | Date trial stop |
| Recruitment center locations | Trial extensions |
| Official scientific title | Date primary analyses |
| Lay title | Name of Research ethics board/institutional |
| Date recruitment start | Review board (REB/IRB) |
| Recruitment status | REB trial approval number |
| Inclusion criteria | Rationale of the trial |
| Exclusion criteria | References to systematic reviews |
| Disease/condition | Justification of interventions |
| Interventions | Trial objectives |
| Primary endpoint | Study design |
| Secondary endpoints | Number of arms |
| Trial phase/study type | Generation of allocation sequence |
| Target sample size | Randomization |
| Allocation concealment | |
| Blinding status | |
| Other design features | |
| Framework of the study | |
| Sample size calculation | |
| Planned subgroup analyses | |
| Planned analyses methods | |
| Consent forms | |
| Full protocol | |
| Contracts and financial arrangements |
Methods
Study design
This study was a survey of academic researchers currently running investigator-initiated clinical studies which were registered with clinicaltrials.gov. It was approved by the ethics committee of the University of Göttingen, Germany.
Study population
The basic population consisted of all recruiting or planned investigator-initiated clinical studies registered with the study register of the U.S. National Institutes of Health (clinicaltrials.gov) in May 2006 (n = 7988). Using computer generated random numbers we selected 1500 studies. Investigator-initiated studies were defined as all studies which were registered with a non-industry sponsor. In July 2006, all principal investigators with valid contact details were contacted by e-mail explaining the purpose of the survey and a link to access the questionnaire. Two reminder e-mails were sent each two weeks apart. No attempts were made to contact non-responders by phone because of difficulties to obtain sufficient contact details and resource constraints. Written informed consent was not sought in this internet based survey but informed consent of participants was implied because access to the questionnaire was restricted to persons approached by e-mail explaining the study.
Data collection
A web-based 52-item questionnaire was developed based on the WHO Trial Registration Data Set [2] and the proposed minimum data set from the Ottawa Group [6]. Participants were asked whether they would be willing to publicly disclose specific details about their study. The questionnaire consisted of eleven main sections (Additional file 1): Contacts and funding, title and description of the study, key dates, ethical approval, background of the study, eligibility criteria, intervention(s), outcome measures, design, documents, and results. We used five response categories to indicate willingness for disclosure: yes, no, don't know/can't decide, don't want to answer, not applicable. Each question had to be answered in order to proceed with the questionnaire. Given that the questionnaire solely consisted of questions directly related to items of the two data sets mentioned above, no piloting of the questionnaire was done.
Sample size calculation
Sample size calculation was based on confidence intervals for proportions and the following considerations: 1) a maximum width of a confidence interval for questions answerable dichotomously of 6% was considered narrow enough; 2) based on a basic population of 7988 this would require 259 responses; 3) assuming a response rate of 25% a sample size of 1036 would be needed; 4) to account for missing and invalid contact details we selected 1500 studies.
Statistical analysis
Data were analysed in Stata 9.2 using descriptive statistics for the main analysis. Responders and non-responders were compared using the chi-squared test. Association between willingness to disclose study details and study phase was assessed using the chi-squared test for trend. To explore the potential influence of non-response bias we used logistic regression to assess associations between factors associated with non-response and the willingness to register study details. We therefore included the following factors in the regression analysis: study sponsored by the National Institutes of Health and phase II study in oncology. For ease of interpretation we recoded "yes" and "not applicable" responses as 'yes' and "no", "don't want to answer", and "don't know" as 'no'. We chose this coding procedure in order to predict willingness to disclose all study details according the Ottawa criteria. Coding "not applicable" as "no" would have had the following potential consequence: e.g. if a participant is willing to disclose the whole data-set except one item which is not applicable to his context, he would have been falsely categorized as completely reluctant (i.e. "0" in regression analysis).
Results
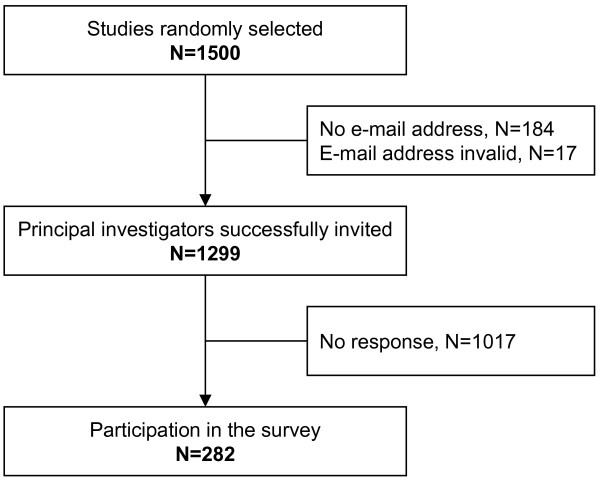
201 out of the initial 1500 studies had no (n = 184) or no valid (n = 17) e-mail address of the principal investigator available, leaving 1299 potential participants. Studies with principal investigators with no or invalid e-mail address were more likely to be sponsored by the National Institutes of Health, to be in the field of oncology, and more likely to study a drug. Of the 1299 contacted investigators, 282 (22%) responded and these formed the population for analysis (Figure 1).
Figure 1.
Study flow diagram.
Non-responders were more likely to be principal investigators of studies sponsored by the National Institutes of Health (Table 2). Studies of non-responders were also more likely to be in the field of oncology and registered as phase II studies. Given these differences in responders and non-responders, we did not calculate confidence intervals of response distributions.
Table 2.
Study characteristics
| Variables | Total | E-mail available* | E-mail not available | p** | Responders | Non-responders | p |
| Recruiting status of study | 1500 | 1299 | 201 | 0.15 | 282 | 1017 | 0.68 |
| Recruiting | 1375 (91.7) | 1196 (92.1) | 179 (89.0) | 258 (91.5) | 938 (92.23) | ||
| Not yet | 125 (8.3) | 103 (7.9) | 125 (8.3) | 24 (8.5) | 79 (7.8) | ||
| Type of sponsor | <0.001 | <0.001 | |||||
| NIH | 288 (19.2) | 207 (15.9) | 81 (40.3) | 21 (7.4) | 186 (18.3) | ||
| Other | 1212 (80.8) | 1092 (84.1) | 120 (59.7) | 261 (92.5) | 831 (81.7) | ||
| Study condition according to ICD 10 | <0.001 | 0.03 | |||||
| Infections | 69 (4.6) | 64 (4.9) | 5 (2.5) | 22 (7.8) | 42 (4.1) | ||
| Oncology | 608 (40.5) | 474 (36.5) | 134 (66.7) | 73 (25.9) | 401 (39.4) | ||
| Haematology | 23 (1.5) | 19 (1.5) | 4 (2.0) | 3 (1.1) | 16 (1.6) | ||
| Endocrinologic diseases | 85 (5.7) | 79 (6.1) | 6 (3.0) | 21 (7.4) | 58 (5.7) | ||
| Psychiatric diseases | 119 (7.9) | 109 (8.4) | 10 (4.9) | 28 (9.9) | 81 (8.0) | ||
| Neurologic diseases | 62 (4.1) | 58 (4.6) | 4 (2.0) | 14 (5.0) | 44 (4.3) | ||
| Eye | 12 (0.8) | 2 (1.0) | 10 (0.8) | 2 (0.7) | 8 (0.8) | ||
| Ear | 2 (0.1) | 2 (0.1) | 0 (0.0) | 1 (0.3) | 1 (0.1) | ||
| Cardiovascular diseases | 123 (8.2) | 118 (9.1) | 5 (2.5) | 30 (10.6) | 88 (8.6) | ||
| Lung diseases | 59 (3.9) | 53 (4.1) | 6 (3.0) | 10 (3.5) | 43 (4.2) | ||
| Digestive diseases | 43 (3.3) | 4 (2.0) | 47 (3.1) | 15 (5.2) | 28 (2.7) | ||
| Skin | 19 (1.3) | 18 (1.4) | 1 (0.5) | 3 (1.1) | 15 (1.5) | ||
| Musculoskeletal disorders | 51 (3.4) | 48 (3.7) | 3 (1.5) | 12 (4.3) | 36 (3.5) | ||
| Urology | 76 (5.1) | 72 (5.5) | 4 (2.0) | 20 (7.1) | 52 (5.1) | ||
| Pregnancy | 26 (1.7) | 23 (1.8) | 3 (1.5) | 5 (1.8) | 18 (1.8) | ||
| Perinatal disorders | 10 (0.7) | 10 (0.8) | 0 (0.0) | 3 (1.1) | 7 (0.7) | ||
| Labour | 2 (0.1) | 2 (0.1) | 0 (0.0) | 1 (0.3) | 1 (0.1) | ||
| Trauma | 39 (2.6) | 35 (2.7) | 4 (2.0) | 6 (2.1) | 29 (2.8) | ||
| Extern | 1 (0.1) | 1 (0.1) | 0 (0.0) | 1 (0.3) | 0 (0.0) | ||
| Other | 67 (4.5) | 61 (4.7) | 6 (3.0) | 12 (4.3) | 49 (4.8) | ||
| Study intervention | <0.001 | 0.10 | |||||
| Drug | 895 (59.7) | 741 (57.0) | 154 (76.6) | 143 (50.7) | 598 (58.8) | ||
| Procedure | 231 (15.4) | 211 (16.2) | 20 (9.9) | 55 (19.5) | 156 (15.3) | ||
| Behaviour | 112 (7.5) | 107 (8.2) | 5 (2.5) | 32 (11.3) | 75 (7.4) | ||
| Device | 64 (4.3) | 62 (4.8) | 2 (1.0) | 14 (5.0) | 48 (4.7) | ||
| Vaccine | 17 (1.1) | 12 (0.9) | 5 (2.5) | 3 (1.1) | 9 (0.9) | ||
| Gene therapy | 5 (0.3) | 4 (0.3) | 1 (0.5) | 0 (0.0) | 4 (0.4) | ||
| Other/not applicable | 176 (11.7) | 162 (12.5) | 14 (7.0) | 35 (12.4) | 127 (12.5) | ||
| Study phase | <0.001 | <0.01 | |||||
| Phase I | 137 (9.1) | 113 (8.7) | 24 (11.9) | 19 (6.7) | 94 (9.2) | ||
| Phase II | 357 (23.8) | 281 (21.6) | 76 (37.8) | 45 (16.0) | 236 (23.2) | ||
| Phase III | 230 (15.3) | 206 (15.9) | 24 (11.9) | 51 (8.1) | 155 (15.2) | ||
| Phase IV | 177 (11.8) | 168 (12.9) | 9 (4.5) | 48 (17.0) | 120 (11.8) | ||
| Phase I/II | 72 (4.8) | 56 (4.3) | 16 (8.0) | 6 (2.1) | 50 (4.9) | ||
| Phase II/III | 43 (2.9) | 35 (2.7) | 8 (4.0) | 6 (2.1) | 29 (2.8) | ||
| Not applicable | 484 (32.3) | 440 (33.9) | 44 (21.9) | 107 (37.9) | 333 (32.7) |
* E-mail address of principal investigator
** Chi-squared test
Categories with less than six counts overall were added to category "Other" or "Other/not applicable" for the chi-square test.
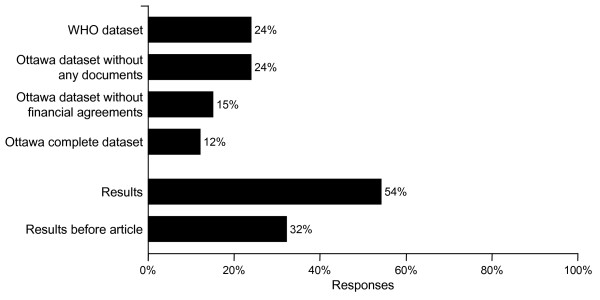
Agreement to disclose study details was very high for most individual items (Additional file 1). Willingness to register study details was lowest for details of planned subgroup analyses (49% willingness to register), sample size calculation (57%), and planned analyses methods (58%). However, disclosing study documents, in particular the study protocol and financial agreements, was found to be most problematic with only 31% of respondents willing to disclose these publicly. 151 investigators (54%) would be willing to present results of their studies in a register. However, only 89 participants (32%) would be willing to present results before submission to a peer-reviewed journal even if journal editors would accept such a presentation (a situation that would be comparable to today's practice regarding presentation at conferences).
Sixty-eight responders (24%) were willing to disclose all items required by the WHO – and clinicaltrials.gov. Only 34/282 (12%) agreed to disclose all details proposed by the Ottawa Group (Figure 2).
Figure 2.
Willingness to disclose study details. For description of each data set see Table 1.
If disclosing documents would not be required, 67/282 (24%) participants would be willing to disclose all other details. Not requiring registration of planned analyses methods including subgroup analyses only slightly increased this proportion (70/282; 25%). Restricting the data set to study details not identified as sensitive for competitive reasons by industry (scientific title, intervention, sample size calculation, outcome measures) also increased this proportion only slightly (71/282; 25%). There was no association between study phase and willingness to register details according to the data set proposed by the Ottawa Group (test for trend p = 0.59). Logistic regression indicated no association between characteristics of non-responders (study sponsored by the National Institutes of Health and phase II study in oncology) and willingness to disclose details (p > 0.15 for each explanatory variable).
Discussion
This is the first survey on opinions of academic researchers suggesting that principal investigators of non-industry sponsored studies are reluctant to disclose all data items proposed by the Ottawa Group. Disclosing the study protocol and financial agreements were found to be most problematic.
As with any survey, our study is susceptible to non-response bias. The response rate was low with only 22% of potential participants responding. It is well known that web-based surveys have lower response rates than postal surveys [8]. Exact reasons for this low response rate remain unclear for us but might be related to the length of the questionnaire, the absence of any incentive, or the topic itself [9]. Nevertheless, we found no association between characteristics associated with non-response and the willingness to disclose study details. Although the impact of non-response seems therefore less problematic this study should be viewed as exploratory. Socially desirable responses might be another problem often encountered in surveys. Drawing conclusions about the actual habit of respondents is therefore often problematic [10]. Given the recent debate about trial registration and the requirement of editors of major journals to register a clinical study, one might expect that respondents would favour registration simply to conform with opinion leaders. The high proportion of respondents willing to disclose individual study details might be viewed as an indication for socially desired response habit. However, willingness to disclose all proposed items was low indicating that respondents differentiated well between different items. Finally, because of limited information available, we were not able to explore characteristics of investigators willing to disclose study details such as country of origin or host institution.
Recent debates about the WHO Trial Registration Data Set have focused on the reluctance of industry to disclose particular study details [11,12]. Representatives of industry argue that some study details are sensitive for competitive reasons and that these details might be disclosed with some delay [13]. However, academic research is also competitive nowadays and researchers might therefore also be reluctant to disclose study details. This reluctance might be even more pronounced for study registers adopting the data set proposed by the Ottawa Group [6]. The main reasons for prospective trial registration correspond to publication and outcome reporting bias [14,15]. For example, trial participants are at risk of being misled when their consent and the trial design are not fully informed by prior research or institutional review board (IRB) members cannot fully weigh risks and benefits when some unknown proportion of the relevant data is unavailable for review [16]. Consequently, it is an ethical obligation of researchers to publish all relevant details of their clinical studies and publicly available clinical study registers help to fulfil this obligation [17].
Conclusion
As our survey suggests, academic researchers might be reluctant to disclose details of their study. Future discussions on trial registration should not only focus on industry but also on academic researchers. Consequences of more detailed registration of studies should be openly discussed when considering a minimum data set for a given trial register. These potential consequences not only include issues related to commercial and academic competition but also the increasing administrative workload of clinical researchers. Lastly, it seems important to disseminate the ethical obligation to register clinical studies more broadly.
Competing interests
ST was a member of the Ottawa Group. MS declares that he has no competing interests.
Authors' contributions
MS and ST equally participated in study design, statistical analysis and writing of the manuscript. Both authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Both authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
All questions and corresponding results. The data provide represent the results of the survey.
Acknowledgments
Acknowledgements
MS is supported by a Young Investigators' Award of the German Ministry of Education and Research (grant no. 01 GK 0516). We gratefully acknowledge Irene Kühne for her technical assistance.
Contributor Information
Martin Scherer, Email: mschere@gwdg.de.
Sven Trelle, Email: strelle@ispm.unibe.ch.
References
- DeAngelis CD, Drazen JM, Frizelle FA, Haug C, Hoey J, Horton R, Kotzin S, Laine C, Marusic A, Overbeke AJ, Schroeder TV, Sox HC, Van Der Weyden MB. Clinical trial registration: a statement from the International Committee of Medical Journal Editors. JAMA. 2004;292:1363–1364. doi: 10.1001/jama.292.11.1363. [DOI] [PubMed] [Google Scholar]
- World Health Organization Trial Registration Data Set http://www.who.int/ictrp/data_set/en/index.html
- World Health Organization Comments on International Clinical Trials Registry Platform http://www.who.int/ictrp/comments/en/index.html
- Tomlinson S. The research assessment exercise and medical research. BMJ. 2000;320:636–639. doi: 10.1136/bmj.320.7235.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krleza-Jeric K, Chan AW, Dickersin K, Sim I, Grimshaw J, Gluud C, for the Ottawa Group Principles for international registration of protocol information and results from human trials of health related interventions: Ottawa statement (part 1) BMJ. 2005;330:956–958. doi: 10.1136/bmj.330.7497.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krleza-Jeric K. Draft - The Ottawa Statement, Part Two: principles of operationalisation for international trial registration http://ottawagroup.ohri.ca/statement2.html
- Zarin DA, Tse T, Ide NC. Trial Registration at ClinicalTrials.gov between May and October 2005. N Engl J Med. 2005;353:2779–2787. doi: 10.1056/NEJMsa053234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leece P, Bhandari M, Sprague S, Swiontkowski MF, Schemitsch EH, Tornetta P, Devereaux PJ, Guyatt GH. Internet versus mailed questionnaires: a controlled comparison (2) J Med Internet Res. 2004;6:e39. doi: 10.2196/jmir.6.4.e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, Kwan I, Cooper R. Methods to influence response to postal questionnaires. The Cochrane Library. 2007;Issue 1:Art. No. MR000008. doi: 10.1002/14651858.MR000008.pub3. [DOI] [PubMed] [Google Scholar]
- Alreck PL, Settle RB. The survey research handbook. 2nd. Boston/Mass., Irwin/McGraw-Hill; 1995. [Google Scholar]
- Drazen JM, Wood AJ. Trial registration report card. N Engl J Med. 2005;353:2809–2811. doi: 10.1056/NEJMe058279. [DOI] [PubMed] [Google Scholar]
- Krleza-Jeric K. Clinical trial registration: the differing views of industry, the WHO, and the Ottawa Group. PLoS Med. 2005;2:e378. doi: 10.1371/journal.pmed.0020378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Federation of Pharmaceutical Manufacturers and Associations. European Federation of Pharmaceutical Industries and Associations. Japanese Pharmaceutical Manufacturers Association. Pharmaceutical Research and Manufacturers of America Joint position on the disclosure of sensitive information via clinical trial registries http://www.ifpma.org/clinicaltrials.html
- Simes RJ. Publication bias: the case for an international registry of clinical trials. J Clin Oncol. 1986;4:1529–1541. doi: 10.1200/JCO.1986.4.10.1529. [DOI] [PubMed] [Google Scholar]
- Chan AW, Hrobjartsson A, Haahr MT, Gotzsche PC, Altman DG. Empirical evidence for selective reporting of outcomes in randomized trials: comparison of protocols to published articles. JAMA. 2004;291:2457–2465. doi: 10.1001/jama.291.20.2457. [DOI] [PubMed] [Google Scholar]
- Zarin DA, Ide NC, Tse T, Harlan WR, West JC, Lindberg DA. Issues in the registration of clinical trials. JAMA. 2007;297:2112–2120. doi: 10.1001/jama.297.19.2112. [DOI] [PubMed] [Google Scholar]
- Irwin RS. Clinical trial registration promotes patient protection and benefit, advances the trust of everyone, and is required. Chest. 2007;131:639–641. doi: 10.1378/chest.07-0088. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
All questions and corresponding results. The data provide represent the results of the survey.