Abstract
The United States Department of Health and Human Services (DHHS) has emphasized the importance of utilizing health information technologies, thus making the availability of electronic resources critical for physicians across the country. However, few empirical assessments exist regarding the current status of computerization and utilization of electronic resources in physician offices and physicians' perceptions of the advantages and disadvantages of computerization. Through a survey of physicians' utilization and perceptions of health information technology, this study found that a “digital divide” existed for eastern North Carolina physicians in smaller physician practices. The physicians in smaller practices were less likely to utilize or be interested in utilizing electronic health records, word processing applications, and the Internet.
Introduction
The U.S. Department of Health and Human Services (DHHS) has emphasized the need for health information technology (HIT), making the availability and utilization of electronic resources for physicians—regardless of the size of their practice—crucial.1 Leaders in the healthcare industry have stated that their top three priorities for strategic decisions in HIT are related to (1) improving clinical processes and workflow efficiency, (2) improving the quality of care, and (3) sharing data.2 HIT encompasses many different types of technologies, such as electronic health records (EHRs), computerized provider order entry, decision support (DS), electronic results reporting, electronic prescribing, consumer health informatics (patient decision support or personal health records), mobile computing, telemedicine, electronic health communication (e-mail), administration, data exchange networks, knowledge retrieval systems (expert or referent systems), general HIT, and others.3 Despite this broad array of technologies, the focus of the literature on HIT has been the EHR since the president's pledge that most Americans' health records would be electronic by 2014.4
Utilization of HIT within the U.S. lags behind other industrialized countries, with the U.S. healthcare sector still operating primarily using paper-based systems.5,6 According to DHHS, healthcare is the largest sector of the U.S. economy that “has not fully embraced information technology.”7 Because HIT systems could lead to healthcare cost savings in the long run, Anderson warns that “the lack of an integrated, national IT system for health in the future could further exacerbate the position of the United States relative to countries that are HIT leaders.”8
As measured by surveys of the Center for Studying Health System Change and the National Center for Health Statistics (NCHS), the healthcare sector is responding to the DHHS's message. The Community Tracking Study Physician Survey of the Center for Studying Health System Change found that the percentage of all physicians having access to IT for clinical activities, such as obtaining treatment guidelines, accessing patient notes, and exchanging clinical data with other physicians, grew steadily between 2001 and 2005.9 In 2006, approximately 29.2 percent of physicians surveyed in the National Ambulatory Medical Care Survey (NAMCS) of the NCHS reported using full (14.5 percent) or partial (14.7 percent) EHRs in their practices—a 22 percent increase since 2005 and a 60 percent increase from 2001, when 18.2 percent reported using EHRs.10,11 Adoption of EHRs is more rapid in some regions than others, with the NAMCS reporting that physicians in the West (42.3 percent) were more likely to use EHRs than were physicians in other regions.12 A positive relationship exists between use of EHRs and size of physician practice (as measured by number of physicians).13 Data indicate that the gap between physicians in smaller and larger practices in their adoption of technology has remained constant over the period of 2000–2001 through 2004–2005.14 The relationship between the size of the practice and the adoption of IT was more pronounced for certain clinical activities, such as accessing patient notes and exchanging clinical data with other physicians.15 Finally, the NAMCS results indicated that the use of EHRs was related to several other characteristics of office-based physicians.16 Increased use was associated with ownership by a health maintenance organization (rather than private practice or other types of ownership) and location in urban areas (metropolitan statistical areas). Use of EHRs varied with the number of managed care contracts (highest with 1 to 2 and lower with none, 3 to 10, and 10+). EHR use did not vary by specialty type or gender of the physician, but did decline with age.17
Empirical studies of the current status of adoption of various aspects of HIT are limited.18–20 These various aspects include decision support, computerized provider order entry, computerized prompts, electronic scheduling, personal health records, e-mail, and the EHR in specific sites, such as ambulatory, hospital, or long-term care; specific specialties, such as pediatrics or primary care; or specific patient populations, such as the chronically ill.21–23 Evidence on the current level of adoption and utilization of EHRs is inconsistent, using differing definitions of adoption and of the EHR.24,25 Moreover, only “a handful of HIT leaders” provided generalizable knowledge of their study’s reported benefit.26 Finally, while some studies provided “insights into rates of adoption or barriers to adoption of specific functionalities,” they did not provide information that was “generalizable to other functionalities.”27
One study surveyed both office managers and practitioners (physicians, physician’s assistants, and nurse practitioners) about the current level of HIT in the practice and current use of and attitudes toward HIT of the practitioners.28 The practices, within a single state, were part a collaborative of primary care clinicians and researchers dedicated to translating relevant research into practice.29 Of the office managers, 31 of 68 (46 percent) responded, and of the practitioners, 59 of 116 responded (51 percent). The survey results showed that 21 percent were using EHRs, although 100 percent of the responding practices used an administrative database for billing or coding and had at least two desktop computers per practice.30 Use of HIT was variable by application, as were the reasons for not using an application.31 Examples of reasons for not using HIT were concerns about security or privacy, unclear benefits, cost, intrusion into the practitioner-patient relationship, and lack of knowledge.32 The researchers concluded that while interest in HIT was high, adoption of several key technologies was low.33
A national survey via e-mail was conducted of the members of the American Academy of Family Physicians (AAFP) for which the AAFP had e-mail addresses (35,554).34 The response rate was 15.5 percent (5517).35 Of the respondents, 23.5 percent used EHRs.36 No difference was found across demographic groups (gender, urban/rural, region, or age group).37
A national survey studied medical group practices (defined as three or more physicians with common billing and health record systems).38 The researchers randomly selected practices from 16 stratified cells.39 This survey had three stages: (1) web, (2) paper, and (3) telephone surveys of a stratified, random sample of 750 nonresponding practices. Stages 1 and 2 resulted in response rates of 13.6 percent for practices of 5 or fewer physicians and 26.9 percent for practices with 21 or more physicians.40 Combining the three stages resulted in an overall response rate of 21.1 percent (16.1 percent for practices of 5 or fewer physicians and 33.9 percent for practices with 21 or more physicians).41 Reweighting the responses to adjust for stratification by size resulted in the researchers’ estimation that 14.1 percent of the medical group practices had EHRs.42 Smaller practices were less likely to have adopted EHRs than larger practices (about 12 percent for practices of 5 or fewer physicians and about 19 percent for practices with 10 or more physicians).43 Moreover, while the data indicated that many practices were planning to implement EHRs in the subsequent two years, smaller practices were implementing EHRs at a slower rate than larger practices.44 Finally, almost 50 percent of practices with five or fewer physicians did not have EHRs nor any plans to implement them in the subsequent two years.45
Results of a national survey of 1,000 randomly selected primary pediatric practices also demonstrated that smaller physician practices are unlikely to adopt EHRs.46 After three mailings, the researchers achieved a response rate of 58 percent. Of the respondents, 10.8 percent were in solo practices, 38.8 percent were in small practices (two to five providers; physicians, nurse practitioners, or physician's assistants), and 47.1 percent were in large practices (at least six providers), with 3.3 percent not specifying. Overall, 21.3 percent of respondents had EHRs with the percentage increasing with practice size (3.5 percent for solo practices, 14.2 percent for small practices, and 31.9 percent for large practices).47
In 2005 a Florida statewide survey was conducted of primary care physicians (general internists, pediatricians, family physicians, general practitioners, and obstetricians/gynecologists).48 After two paper mailings, a participation rate of 28.2 percent was achieved.49 Of the respondents, 16.6 percent used e-mail to communicate with their patients on a regular basis, and only 2.9 percent used e-mail with patients frequently. Additionally, respondents in urban practices and larger practices (at least 50 physicians) reported higher e-mail use than those in rural practices and smaller practices.50 This study also found that respondents who had access to high-speed Internet and who used EHRs utilized e-mail more than those who did not have access.51
A 2005 statewide survey in Massachusetts was conducted of physician practices representing all specialties.52 For each practice selected from a stratified random sample, a physician was randomly selected for survey with the resulting final sample size being 1,884 physicians.53 A response rate of 71 percent (1,345 respondents) was achieved after the initial survey was sent via express mail with a $20 cash honorarium, second and third mailings were sent without remuneration, and multiple telephone contacts were made for follow-up.54 In logistic regression analyses, practice size was the strongest independent correlate of EHR adoption. Practices with four or more physicians were more likely to have EHRs than solo practices.55 Specifically, less than 15 percent of small practices (three or fewer physicians) reported having EHRs.56 One-third of practices with four to six physicians reported having EHRs, and 52 percent of practices with seven or more physicians reported having EHRs.57 Overall, 23 percent of practices had EHRs.58 The state has a “much higher” adoption rate of EHRs than the national average with 45 percent of physicians in the state having EHRs, although only 23 percent of practices have EHRs because of the much lower adoption rate of small practices.59
Characterized as a “dearth,” even fewer empirical studies exist on the current status of adoption of various aspects of HIT by physicians serving “vulnerable populations” such as rural, low-income, uninsured, or minority populations.60 Available data focused on community health centers and clinics in California.61 For example, a 2001 survey in California of primary care physicians' offices in poor and minority communities in a large, suburban county (Orange) found high levels of access to and interest in Web-based clinical systems.62 These researchers concluded that additional studies are needed in other geographic regions to determine generalizability of their findings.63 Other researchers recommended that additional studies of relevant subsets of physicians caring for vulnerable populations be conducted.64,65
Rural areas of the United States do not have the same access to information technologies, particularly high-speed broadband connections, as urban areas.66,67 This gap in access to information technologies has come to be known as the “digital divide.” Poverty, as well as the low population densities of rural areas, has been found to be a factor in the digital divide.68,69
Eastern North Carolina is rural and poor and has a large minority population.70–72 One of the “most distinguishing features of eastern North Carolina is its pervasive poverty.”73 Thus, eastern North Carolina can be considered representative of “vulnerable populations.” Additionally, the lack of primary care physicians in eastern North Carolina is an “enduring problem.”74 Eight of ten North Carolina counties with the lowest ratios of primary care physicians per 10,000 population are in eastern North Carolina.75 Moreover, the majority of whole counties in North Carolina designated as Persistent Health Professional Shortage Areas are in eastern North Carolina.76 Approximately 1.5 times as many rural as urban physicians were in solo practices or partnerships (65.2 percent with 23.3 percent unreported).77 Thus, if a county has a physician, he or she is in a solo or small practice.
Research has established that smaller physician practices are less likely to adopt health information technology.78–80 One study found that primary care physicians’ offices in poor and minority communities in a large, suburban county had high levels of access to and interest in Web-based clinical systems.81 Finally, researchers have called for studies in other geographic areas and of physician subsets, especially those serving vulnerable populations.82–84
This research of physicians in eastern North Carolina represents a response to the call for additional research in other geographic areas and of physician subsets. The digital divide is posited not only to affect the general public, but also to affect physicians in the smaller, rural practices of eastern North Carolina. The purpose of this study was to investigate the existence of a digital divide in terms of health information technologies for physicians. For this study, HIT includes EHRs; applications that support EHRs; and applications associated with EHRs, such as practice management functions (billing, appointments, etc.), word processing (document creation), e-mail (sending and receiving), and the utilization of the Internet. Thus, the following hypotheses were examined to determine physicians’ interest in EHRs and extent of computerization of physician offices in eastern North Carolina:
H10: There is no relationship between the use of EHRs and the size of a physician practice.
H1A: The larger the physician practice, the greater the use of EHRs.
H20: There is no relationship between interest in the use of EHRs and the size of a physician practice.
H2A: The larger the physician practice, the greater the interest in the use of EHRs.
H30: There is no relationship between the utilization of EHRs in a physician practice and the practice’s interest in decision support (DS) technologies.
H3A: Physician practices currently utilizing EHRs also have an interest in utilizing DS technologies.
H40: There is no relationship between the use of practice management systems and the size of a physician practice.
H4A: The larger the physician practice, the more likely the use of practice management systems.
H50: There is no relationship between the use of word processing applications and the size of a physician practice.
H5A: The larger the physician practice, the more likely the use of word processing applications.
H60: There is no relationship between the use of e-mail and the size of a physician practice.
H6A: The larger the physician practice, the more likely the use of e-mail.
H70: There is no relationship between the use of the Internet and the size of a physician practice.
H7A: The larger the physician practice, the more likely the use of the Internet.
Methods
The research design was descriptive and cross-sectional. A mail survey was used to collect self-reported data from physicians in eastern North Carolina. A mail survey was an appropriate design because previous research demonstrated that no response bias exists between responders and nonresponders to mail surveys about use of information technology.85 An e-mail survey was precluded because the researchers did not have e-mail addresses for the subjects. The research was approved by the institutional review board of the researchers' university.
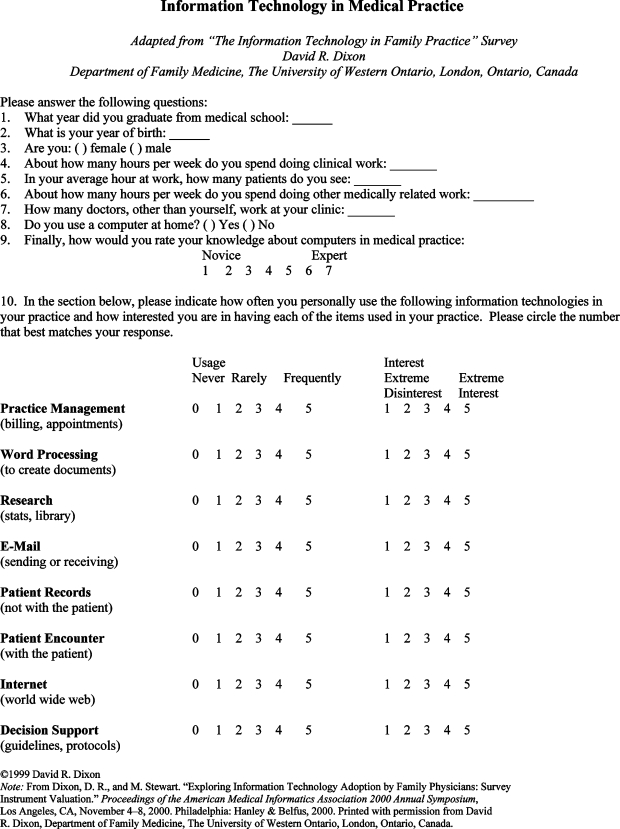
This survey used the validated instrument of Dixon and Stewart.86 The instrument is one page with 10 items (Appendix A). The instrument collects data on demographics (year of graduation from medical school, year of birth, gender), on characteristics of the practice (number of hours of clinical work per week, average number of patients seen in an hour, hours spent doing other medically related work, size), on personal use of computers and knowledge of computers in medical practice, and on use of health information technologies and interest in using these technologies. Items 9 and 10 are Likert scales.
The subjects were 9,055 physicians who practice in Raleigh, Durham, Chapel Hill, and eastern North Carolina, as listed with the North Carolina Medical Board. Response rates in the literature varied from 13.6 percent to 71 percent. Studies with designs similar to this study achieved overall response rates of 21.1 percent and 28.2 percent.87,88 Given the size of the population, the researchers determined that a random sample of 900 (10 percent) was appropriate.
Each subject was sent a cover letter; survey; and postage-paid, self-addressed envelope. The cover letter included the statement, “If you do participate, completion and return of the survey indicates your consent.” To preserve anonymity, surveys included no control numbers. Two separate mailings of the cover letter and survey were sent. Duplicate responses were removed through a comparison of responses.
Data were entered into SPSS version 13.0 for analysis. Practices of 9 or fewer physicians were categorized as “small” (Item 7 on the survey excluded the physician-respondent), and practices of 10 physicians or greater were categorized as “large.”89,90 Missing values in categorical data were coded as “unknown.” Missing values in continuous data were replaced with the mean score for all other respondents on that variable (missing data were less than 10 percent for any variable). The statistical approach appropriate for the hypotheses was bivariate correlation because the researchers were investigating relationships between the variables.
Results
The researchers received 200 responses from the 900 subjects of the random sample for an uncorrected response rate of 22 percent. For 132 subjects in the sample, the mailing address was incorrect. The corrected denominator of possible responders became 768. Of the 200 responders, 187 provided usable surveys. The corrected response rate was 24.3 percent.
Of the 187 usable surveys, 131 were from small practices (70 percent, with solo practices being 17.6 percent), 46 were from large practices (25 percent), and 10 surveys (5 percent) lacked this datum (Table 1). See Table 1 for data on demographics, selected practice characteristics, and EHR usage. After compensating for missing responses and eliminating five outlier cases (practice size greater than 201), the researchers were able to examine a sample of 182. Analyses by bivariate correlation were performed.
Table 1.
Demographic Data, Selected Practice Characteristics, and EHR Usage
| Number | Percent (%) | |
|---|---|---|
| Year of Graduation from Medical School | ||
| 1951–1954 | 3 | 1.6 |
| 1955–1964 | 13 | 7.0 |
| 1965–1974 | 31 | 16.6 |
| 1975–1984 | 61 | 32.6 |
| 1985–1994 | 56 | 29.9 |
| 1995–2004 | 23 | 12.3 |
| 2005–present | 0 | 0 |
| Age in Years | ||
| 26–35 | 10 | 5.3 |
| 36–45 | 49 | 26.2 |
| 46–55 | 68 | 36.4 |
| 56–65 | 37 | 19.8 |
| 66–75 | 19 | 10.2 |
| 76+ | 4 | 2.1 |
| Gender | ||
| Male | 129 | 69 |
| Female | 58 | 13 |
| Size of Practice | ||
| 0 to 9 | 131 | 70.1 |
| 10 or more | 56 | 29.9 |
| EHR Usage | ||
| Never Used | 59 | 31.5 |
| Rarely Used | 28 | 15.0 |
| Frequently Used | 100 | 53.5 |
Hypotheses H1 through H3 focused on EHRs and supportive applications. See Table 2 and Table 3.
Table 2.
Pearson Product-Moment Correlation of Size of Physician Practice with Utilization of and Interest in EHRs and with Utilization of Health Information Technologies (Practice Management, Word Processing, E-mail, Internet)
| Utilization of EHR | Interest in EHRs | Practice Management | Word Processing E-mail | Internet | ||
|---|---|---|---|---|---|---|
| Size of Practice | .313 | .216 | .060 | .203 | .140 | .195 |
| ρ = .000*** | ρ = .003** | ρ = .418 | ρ = .006** | ρ = .060 | ρ = .008** | |
Note. (coefficient/two-tailed test)
ρ < .05.
ρ < .01.
ρ < .001.
Table 3.
Pearson Product-Moment Correlation of Utilization of EHR and Interest in Decision Support Technology
| Interest in Decision Support Technology | |
| Utilization of EHR | .209 |
| ρ = .005** |
Note. (coefficient/two-tailed test)
ρ < .05.
ρ < .01.
ρ < .001.
Hypothesis H1 investigated the relationship between the size of the physician practice and utilization of EHRs. A Pearson two-tailed test identified a significant correlation (r = .313) at the 0.01 level (Table 2). The researchers rejected H10 that there is no relationship between the use of EHRs and the size of a physician practice. Rejecting the null hypothesis suggests that a relationship exists between the size of the physician practice and the utilization of EHRs.
Hypothesis H2 investigated the relationship between the size of the physician practice and the interest of physicians in using EHRs. The Pearson two-tailed test yielded a significant correlation (r = .216) at the 0.01 level (Table 2). The researchers rejected H20 that there was no relationship between interest in the use of EHRs and the size of a physician practice. Rejecting the null hypothesis suggests that a relationship exists between interest in the use of EHRs and the size of the physician practice.
Hypothesis H3 investigated the relationship between utilization of EHRs and interest in utilizing decision support tools (Table 3). A Pearson two-tailed test identified a statistically significant correlation (r = .209) between the utilization of EHRs in a physician practice and the practice's interest in DS technologies. The null hypothesis that there was no relationship between utilization of EHRs and interest in utilizing decision support tools was rejected. Rejecting the null hypothesis suggests that a relationship exists between utilization of EHRs and interest in utilizing decision support tools.
Hypotheses H4 through H7 focused on the relationship between the size of the physician practice and utilization of other health information technologies (practice management, word processing, e-mail, Internet; Table 2). Of the respondents, 31.5 percent never used EHRs, 15.0 percent rarely used EHRs, and 53.5 percent frequently used EHRs (Table 1).
Hypotheses H5 and H7 investigated the relationships between the size of the physician practice and utilization of word processing applications and the Internet. Pearson two-tailed tests identified significant correlations at the 0.01 level (r = .203 and r = .195, respectively; Table 2). The researchers rejected H50 and H70 that there is no relationship between the size of the physician practice and use of word processing applications or the Internet. Rejecting the null hypotheses suggested that relationships existed between the size of the physician practice and the utilization of word processing applications and the Internet.
Hypotheses H4 and H6 investigated the relationships between the size of the physician practice and utilization of practice management systems and e-mail. Pearson two-tailed tests did not identify significant correlations at the 0.01 level (r = .060 and r = .140, respectively; Table 2). The researchers failed to reject H40 and H60 that there is no relationship between the size of a physician practice and the use of practice management systems or e-mail.
Discussion
Seventy percent of the respondents were from small practices in an area that is defined as rural and poor.91–93 The study's corrected response rate, 24.3 percent, was comparable to studies with similar designs that achieved overall response rates of 21.1 percent and 28.2 percent.94,95 The study's findings indicated relationships between the size of a physician practice and use of and interest in several health information technologies.
The larger a physician practice, the more likely it was to use EHRs, or, conversely, the smaller a physician practice, the less likely it was to use EHRs (H1).
The larger a physician practice, the more likely it was that the physicians were interested in utilizing EHRs, or, conversely, the smaller a physician practice, the less likely the physicians were to be interested in utilizing EHRs (H2).
Physician practices currently using EHRs were more likely to be interested in utilizing DS technologies, or, conversely, physician practices not currently using EHRs were less likely to be interested in utilizing DS technologies (H3).
The larger the physician practice, the more likely it was that word processing applications were being used, or, conversely, the smaller the physician practice, the less likely it was that word processing applications were being used (H5).
The larger the physician practice, the more likely it was to use the Internet, or, conversely, the smaller the physician practice, the less likely it was to use the Internet (H7).
Given the geographic location, this research focused on smaller physician practices. Similar to previous research, this investigation found that smaller practices are less likely to utilize or be interested in utilizing health information technologies than larger practices.96–99 Specifically, smaller physician practices were less likely to utilize or to be interested in the following components:
EHRs, including their decision support capabilities
Word processing
Internet
The likelihood of utilization of or interest in health information technologies was similar between large and small practices for the components of practice management and e-mail. The focus on the smaller physician practice is appropriate because research has emphasized the sustainability and centrality of the small practice.100 Finally, the small practice is the “leading indicator for achieving a universally paperless health system” as the small practice is expected to be the last setting to widely adopt EHRs.101
Previous research has established that barriers to adoption of health information technologies include disruption and delays of workflow, negligible return on investment, vendor volatility, lack of capital and operating dollars, loss of productivity and income, lack of appropriate software with requisite interoperability, lack of trained staff, and concerns about privacy and security.102–107 These researchers believe that physicians in eastern North Carolina face these same barriers. Any initiative designed to increase the adoption of health information technologies in underserved areas must address these barriers.
The researchers specifically investigated the relationship between EHRs and decision support technologies because fully functional EHRs include connections to external expert and decision support systems. These systems are purported to improve the quality of care by reducing medical errors.108,109 However, one study found that pediatricians without EHRs were less likely to believe that EHRs could improve care.110 Another study reported that only 31.2 percent of physicians used clinical decision support tools most or all of the time.111 Therefore, for EHRs’ potential to be fulfilled, physicians must be willing to use the expert and decision support systems. Unlike the previously cited research, the findings of this study indicate that physicians may utilize this feature of EHRs and, thus, potentially reduce medical errors and improve the quality of care.
One limit of the research is that the researchers were only able to utilize approximately 10 percent of the database of 9,055 physicians practicing in Raleigh, Durham, Chapel Hill, and eastern North Carolina, achieving a 24.3 percent corrected response rate. The researchers faced funding constraints that precluded full utilization of the database. Moreover, additional funding, which would have allowed use of $20 incentives and express mail as implemented by other researchers, would have greatly increased the response rate.112,113 Clear limitations were that the survey instrument did not collect geographic data, such as zip code and urban or rural area, and that the researchers collected anonymous data (not being able to link responses to the sample). Knowledge of details on geographic data would have allowed greater specificity in data analysis. Another limitation was that the study collected self-reported data with all the associated shortcomings. Finally, the study collected data at one point in time.
This study detailed how the digital divide affected physicians in eastern North Carolina. Invaluable replication studies would expand the study to other regions, to the nation, and to other countries. It would be worthwhile to determine whether this study's findings have implications for physician practices in similar areas and in disparate areas. Knowledge of the process of the diffusion of technology would be extended to this sector and, particularly, as it involves physicians.
More probative studies of the specific uses of HIT are also recommended. These future studies could focus on the utilization level and efficacy of word processing applications for clinical documentation and transcription, the providers' use of the Internet to access medical research databases as a tool for evidence-based medicine, and the utilization of e-mail for provider-to-patient and provider-to-provider communication and consultation.
Conclusion
This research examined an important issue facing physicians and clinicians in North Carolina and, potentially, in other regions: the existence of a digital divide for physicians. First, this investigation of HIT examined general utilization of various health information technologies that may be commonplace in many physician practices. Thus, the research provided insight about one region's physicians' utilization of and interest in EHRs and other health information technologies. Second, the research described the status of HIT utilization and adoption in eastern North Carolina, an area of interest because it is a poor area with underserved populations. This status is particularly significant given the current attention to health disparities. Finally, the research established baseline data. Establishing baselines through descriptive investigations is important in order for policy analysts and researchers to assess their progress, over time, in promoting diffusion and adoption of health information technologies.
Small practices in eastern North Carolina are less likely to utilize or be interested in utilizing health information technologies. However, physicians in eastern North Carolina who do utilize EHRs are also interested in using decision support. It is recommended that this regional survey serve as a model to investigate the utilization of and interest in health information technologies in other underserved regions similar to eastern North Carolina. Additionally, it is recommended that the factors affecting the utilization of decision support tools be more fully explored, as these tools are associated with improvements in the quality of patient care and reduction of medical errors.
This study paid particular attention to current utilization and interest in health information systems by size and location of physicians' practices. It was determined that a digital divide exists for physician practices in eastern North Carolina. This “information gap analysis” will subsequently guide future educational offerings, consulting services, and grant applications.
Acknowledgments
The authors wish to acknowledge the efforts of Ms. Jennifer Pitt in the Department of Health Services and Information Management at East Carolina University’s College of Allied Health Sciences, without whose diligent support this study could not have been completed.
Appendix A. Survey Instrument
Contributor Information
David A. Rosenthal, department of health informatics and information management at the University of Tennessee Health Science Center in Memphis, TN.
Elizabeth J. Layman, department of health services and information management at the college of allied health sciences at East Carolina University in Greenville, NC.
Notes
- 1.US Government Accountability Office . Health Information Technology: HHS Is Taking Steps To Develop a National Strategy. Washington, DC: US Government Accountability Office; 2005. [Google Scholar]
- 2.Medical Records Institute . Medical Records Institute's Eighth Annual Survey of Electronic Health Record Trends and Usage for 2006. Boston, MA: Medical Records Institute; 2006. [Google Scholar]
- 3.Chaudhry, Basit, Jerome Wang, Shinyi Wu, Margaret Maglione, Walter Mojica, Elizabeth Roth, Sally C. Morton, and Paul G. Shekelle. “Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care.” Annals of Internal Medicine 144, no. 10 (May 16, 2006): 742–752, Web e12–e22. [DOI] [PubMed]
- 4.Iglehart, John K. “Pursuing Health IT: The Delicate Dance of Government and the Market.” Health Affairs 24, no. 5 (2005, September–October): 1100–1101. [DOI] [PubMed]
- 5.US Government Accountability Office. Health Information Technology: HHS Is Taking Steps To Develop a National Strategy
- 6.Anderson, Gerard F., Bianca K. Frogner, Roger A. Johns, and Uwe E. Reinhardt. “Health Care Spending and Use of Information Technology in OECD Countries.” Health Affairs 25, no. 3 (2006, May–June): 819–831. [DOI] [PubMed]
- 7.US Government Accountability Office. Health Information Technology: HHS Is Taking Steps To Develop a National Strategy, p. 15.
- 8.Anderson, Gerard F., Bianca K. Frogner, Roger A. Johns, and Uwe E. Reinhardt. “Health Care Spending and Use of Information Technology in OECD Countries,” p. 822. [DOI] [PubMed]
- 9.Grossman, Joy M., and Marie C. Reed. “Clinical Information Technology Gaps Persist among Physicians.” Issue Brief/Center for Studying Health System Change 106 (November 2006): 1–4. [PubMed]
- 10.Hing, Esther S., Catharine W. Burt, and David A. Woodwell. “Electronic Medical Record Use by Office-Based Physicians and Their Practices: United States, 2006.” National Center for Health Statistics–NCHS Health E-Stats. October 26, 2007. Available at www.cdc.gov/nchs/data/ad/ad393.pdf (accessed December 17, 2007).
- 11.Burt, Catharine W., Esther Hing, and David Woodwell. “Electronic Medical Record Use by Office-Based Physicians: United States, 2005.” National Center for Health Statistics–NCHS Health E-Stats. December 21, 2006. Available at www.cdc.gov/nchs/products/pubs/pubd/hestats/electronic/electronic.htm (accessed November 28, 2006).
- 12.Hing, Esther S., Catharine W. Burt, and David A. Woodwell. “Electronic Medical Record Use by Office-Based Physicians and Their Practices: United States, 2006.” [PubMed]
- 13.Ibid.
- 14.Grossman, Joy M., and Marie C. Reed. “Clinical Information Technology Gaps Persist among Physicians.” [PubMed]
- 15.Ibid.
- 16.Hing, Esther S., Catharine W. Burt, and David A. Woodwell. “Electronic Medical Record Use by Office-Based Physicians and Their Practices: United States, 2006.” [PubMed]
- 17.Ibid.
- 18.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” Health Affairs 24, no. 5 (2005, September–October): 1323–1333. [DOI] [PubMed]
- 19.Jha, Ashish K., Timothy G. Ferris, Karen Donelan, Catherine DesRoches, Alexandra Shields, Sara Rosenbaum, and David Blumenthal. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence.” Health Affairs 25, no. 6 (2006, November–December): w496–w507. [DOI] [PubMed]
- 20.Shekelle, Paul G., Sally C. Morton, Emmett B. Keeler, et al. Costs and Benefits of Health Information Technology Evidence Report/Technology Assessment No. 132 (2006, April): 1–71. AHRQ Publication No. 06-E006. Available at www.ahrq.gov/downloads/pub/evidence/pdf/hitsyscosts/hitsys.pdf (accessed December 18, 2007). [DOI] [PMC free article] [PubMed]
- 21.Ibid.
- 22.Andrews James E., Pearce Kevin A., Sydney Carey, Ireson Carol, Love Margaret. “Current State of Information Technology Use in a US Primary Care Practice-Based Research Network.”. Informatics in Primary Care. 2004;12(1):11–18. doi: 10.14236/jhi.v12i1.103. [DOI] [PubMed] [Google Scholar]
- 23.Dorr, David, Laura M. Bonner, Amy N. Cohen, Rebecca S. Shoal, Ruth Perrin, Edmund Chaney, and Alexander S. Young. “Informatics Systems to Promote Improved Care for Chronic Illness: A Literature Review.” Journal of the American Medical Informatics Association 14, no. 2 (2007, March–April): 156–163. [DOI] [PMC free article] [PubMed]
- 24.Jha, Ashish K., Timothy G. Ferris, Karen Donelan, Catherine DesRoches, Alexandra Shields, Sara Rosenbaum, and David Blumenthal. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence.” [DOI] [PubMed]
- 25.Blumenthal, David, Catherine DesRoches, Karen Donelan, et al. “Health Information Technology in the United States: The Information Base for Progress.” Report for the Robert Wood Johnson Foundation. 2006. Available at www.rwjf.org/files/publications/other/EHRReport0609.pdf (accessed December 17, 2007).
- 26.Shekelle, Paul G., Sally C. Morton, Emmett B. Keeler, et al. Costs and Benefits of Health Information Technology, p. v. [DOI] [PMC free article] [PubMed]
- 27.Blumenthal, David, Catherine DesRoches, Karen Donelan, et al. “Health Information Technology in the United States: The Information Base for Progress,” p. 3.27.
- 28.Andrews, James E., Kevin A. Pearce, Carey Sydney, Carol Ireson, and Margaret Love. “Current State of Information Technology Use in a US Primary Care Practice-Based Research Network.” [DOI] [PubMed]
- 29.Ibid.
- 30.Ibid.
- 31.Ibid.
- 32.Ibid.
- 33.Ibid.
- 34.Valdes, Ignacio, David C. Kibbe, Greg Tolleson, Mark E. Kunik, and Laura A. Petersen. “Barriers to Proliferation of Electronic Medical Records.” Informatics in Primary Care 12, no. 1 (2004, March): 3–9. [DOI] [PubMed]
- 35.Ibid.
- 36.Ibid.
- 37.Ibid.
- 38.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” [DOI] [PubMed]
- 39.Ibid.
- 40.Ibid.
- 41.Ibid.
- 42.Ibid.
- 43.Ibid.
- 44.Ibid.
- 45.Ibid.
- 46.Kemper, Alex R., Rebecca L. Uren, and Sarah J. Clark. “Adoption of Electronic Health Records in Primary Care Pediatric Practices.” Pediatrics 118, no. 1 (2006, July): e20–e24. [DOI] [PubMed]
- 47.Ibid.
- 48.Brooks, Robert G., and Nir Menachemi. “Physicians' Use of Email with Patients: Factors Influencing Electronic Communication and Adherence to Best Practices.” Journal of Medical Internet Research 8, no. 1 (2006, January–March): e2. [DOI] [PMC free article] [PubMed]
- 49.Ibid.
- 50.Ibid.
- 51.Ibid.
- 52.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, Eric G. Poon, E. John Orav, Helen G. Lo, Deborah H. Williams, and David W. Bates. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey.” Journal of the American Medical Informatics Association 14, no. 1 (2007, January–February): 110–117. [DOI] [PMC free article] [PubMed]
- 53.Ibid.
- 54.Ibid.
- 55.Ibid.
- 56.Ibid.
- 57.Ibid.
- 58.Ibid.
- 59.Ibid.
- 60.Blumenthal, David, Catherine DesRoches, Karen Donelan, et al. “Health Information Technology in the United States: The Information Base for Progress,” pp. 3.27, 4.32.
- 61.Blumenthal, David, Catherine DesRoches, Karen Donelan, et al. “Health Information Technology in the United States: The Information Base for Progress.”
- 62.Bell, Douglas S., Dianna M. Daly, and Paul Robinson. “Is There a Digital Divide among Physicians? A Geographic Analysis of Information Technology in Southern California Physician Offices.” Journal of the American Medical Informatics Association 10, no. 5 (2003, September–October): 484–493. [DOI] [PMC free article] [PubMed]
- 63.Ibid.
- 64.Jha, Ashish K., Timothy G. Ferris, Karen Donelan, Catherine DesRoches, Alexandra Shields, Sara Rosenbaum, and David Blumenthal. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence.” [DOI] [PubMed]
- 65.Blumenthal, David, Catherine DesRoches, Karen Donelan, et al. “Health Information Technology in the United States: The Information Base for Progress.”
- 66.Grubesic, Tony H. “A Spatial Taxonomy of Broadband Regions in the United States.” Information Economics and Policy 18, no. 4 (2006, November): 423–448.
- 67.Whitacre, Brian E., and Bradford F. Mills. “Infrastructure and the Rural-Urban Divide in High-Speed Residential Internet Access.” International Regional Science Review 30, no. 3 (2007, July): 249–273.
- 68.Grubesic, Tony H. “A Spatial Taxonomy of Broadband Regions in the United States.”
- 69.Whitacre, Brian E., and Bradford F. Mills. “Infrastructure and the Rural-Urban Divide in High-Speed Residential Internet Access.”
- 70.Cummings, Doyle M., Lauren Whetstone, David White, Catherine Nelson, Jo Morgan, Diane Poole, and John Morrow. “Rural Eastern Carolina Health (REACH).” North Carolina Medical Journal 60, no. 1 (1999, January–February): 26–28. [PubMed]
- 71.North Carolina State Data Center. Geographic Products–Thematic Maps: Per Capita Income, 1999, Persons Below Poverty, 1999 Available at http://census.state.nc.us/census_body.html (accessed December 7, 2007).
- 72.Wilson, James L. “Eastern North Carolina Health Care Atlas: A Resource for Healthier Communities, 2003: Executive Summary and Introduction to Web-Based Publication.” Available at www.chsrd.med.ecu.edu/Atlas2001/Executive%20Summary_090803.pdf (accessed March 19, 2007).
- 73.Ibid., p. 2.
- 74.Ibid., p. 10.
- 75.North Carolina Institute of Medicine. “Fact Sheet: Providers in Demand: North Carolina's Primary Care and Specialty Supply.” June 2007. Available at www.nciom.org/projects/supply/factsheet3.pdf (accessed December 7, 2007).
- 76.Ibid.
- 77.Horner, Ronnie D., Gregory P. Samsa, and Thomas H. Ricketts. “Preliminary Evidence on Retention Rates of Primary Care Physicians in Rural and Urban Areas.” Medical Care 31, no. 7 (1993, July): 640–648. [DOI] [PubMed]
- 78.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” [DOI] [PubMed]
- 79.Kemper, Alex R., Rebecca L. Uren, and Sarah J. Clark. “Adoption of Electronic Health Records in Primary Care Pediatric Practices.” [DOI] [PubMed]
- 80.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, Eric G. Poon, E. John Orav, Helen G. Lo, Deborah H. Williams, and David W. Bates. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey.” [DOI] [PMC free article] [PubMed]
- 81.Bell, Douglas S., Dianna M. Daly, and Paul Robinson. “Is There a Digital Divide among Physicians? A Geographic Analysis of Information Technology in Southern California Physician Offices.” [DOI] [PMC free article] [PubMed]
- 82.Ibid.
- 83.Jha, Ashish K., Timothy G. Ferris, Karen Donelan, Catherine DesRoches, Alexandra Shields, Sara Rosenbaum, and David Blumenthal. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence.” [DOI] [PubMed]
- 84.Blumenthal, David, Catherine DesRoches, Karen Donelan, et al. “Health Information Technology in the United States: The Information Base for Progress.”
- 85.Menachemi, Nir, Neset Hikmet, Mary Stutzman, and Robert G. Brooks. “Investigating Response Bias in an Information Technology Survey of Physicians.” Journal of Medical Systems 30, no. 4 (2006, August): 277–282. [DOI] [PubMed]
- 86.Dixon, David R., and Moira Stewart. “Exploring Information Technology Adoption by Family Physicians: Survey Instrument Valuation.” Proceedings of the AMIA Symposium (2000): 185–189. [PMC free article] [PubMed]
- 87.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” [DOI] [PubMed]
- 88.Brooks, Robert G., and Nir Menachemi. “Physicians' Use of Email with Patients: Factors Influencing Electronic Communication and Adherence to Best Practices.” [DOI] [PMC free article] [PubMed]
- 89.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” [DOI] [PubMed]
- 90.Brooks, Robert G., and Nir Menachemi. “Physicians' Use of Email with Patients: Factors Influencing Electronic Communication and Adherence to Best Practices.” [DOI] [PMC free article] [PubMed]
- 91.Cummings, Doyle M., Lauren Whetstone, David White, Catherine Nelson, Jo Morgan, Diane Poole, and John Morrow. “Rural Eastern Carolina Health (REACH).” [PubMed]
- 92.North Carolina State Data Center. Geographic Products–Thematic Maps: Per Capita Income, 1999, Persons Below Poverty, 1999
- 93.Wilson, James L. “Eastern North Carolina Health Care Atlas: A Resource for Healthier Communities, 2003: Executive Summary and Introduction to Web-Based Publication.”
- 94.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” [DOI] [PubMed]
- 95.Brooks, Robert G., and Nir Menachemi. “Physicians' Use of Email with Patients: Factors Influencing Electronic Communication and Adherence to Best Practices.” [DOI] [PMC free article] [PubMed]
- 96.Gans, David, John Krawlewski, Terry Hammons, and Bryan Dowd. “Medical Groups' Adoption of Electronic Health Records and Information Systems.” [DOI] [PubMed]
- 97.Kemper, Alex R., Rebecca L. Uren, and Sarah J. Clark. “Adoption of Electronic Health Records in Primary Care Pediatric Practices.” [DOI] [PubMed]
- 98.Brooks, Robert G., and Nir Menachemi. “Physicians' Use of Email with Patients: Factors Influencing Electronic Communication and Adherence to Best Practices.” [DOI] [PMC free article] [PubMed]
- 99.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, Eric G. Poon, E. John Orav, Helen G. Lo, Deborah H. Williams, and David W. Bates. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey.” [DOI] [PMC free article] [PubMed]
- 100.Cunningham, Robert. “Professionalism Reconsidered: Physician Payment in a Small-Practice Environment.” Health Affairs 23, no. 6 (2004, November–December): 36–47. [DOI] [PubMed]
- 101.Ford, Eric W., Nir Menachemi, and M. Thad Phillips. “Predicting Adoption of Electronic Health Records by Physicians: When Will Health Care Be Paperless?” Journal of the American Medical Informatics Association 13, no. 1 (2006, January–February): 106–112, 107. [DOI] [PMC free article] [PubMed]
- 102.Valdes, Ignacio, David C. Kibbe, Greg Tolleson, Mark E. Kunik, and Laura A. Petersen. “Barriers to Proliferation of Electronic Medical Records.” [DOI] [PubMed]
- 103.Kemper, Alex R., Rebecca L. Uren, and Sarah J. Clark. “Adoption of Electronic Health Records in Primary Care Pediatric Practices.” [DOI] [PubMed]
- 104.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, Eric G. Poon, E. John Orav, Helen G. Lo, Deborah H. Williams, and David W. Bates. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey.” [DOI] [PMC free article] [PubMed]
- 105.Ford, Eric W., Nir Menachemi, and M. Thad Phillips. “Predicting Adoption of Electronic Health Records by Physicians: When Will Health Care Be Paperless?” [DOI] [PMC free article] [PubMed]
- 106.Ash, Joan S., and David W. Bates. “Factors and Forces Affecting EHR System Adoption: Report of a 2004 ACMI Discussion.” Journal of the American Medical Informatics Association 12, no. 1 (2005, January–February): 8–12. [DOI] [PMC free article] [PubMed]
- 107.Miller, Robert H., Christopher West, Tiffany Martin Brown, Ida Sim, and Chris Ganchoff. “The Value of Electronic Health Records in Solo or Small Group Practices: Physicians' EHR Adoption Is Slowed by a Reimbursement System That Rewards the Volume of Services More Than It Does Their Quality.” Health Affairs 24, no. 5 (2005, September–October): 1127–1137. [DOI] [PubMed]
- 108.Hannan, Terry J. “Detecting Adverse Drug Reactions to Improve Patient Outcomes.” International Journal of Medical Informatics 55, no. 1 (1999, July 1999): 61–64. [DOI] [PubMed]
- 109.Bates, David W., and Atul A. Gawande. “Patient Safety: Improving Safety with Information Technology.” New England Journal of Medicine 348, no. 25 (2003, June 19): 2526–2534. [DOI] [PubMed]
- 110.Kemper, Alex R., Rebecca L. Uren, and Sarah J. Clark. “Adoption of Electronic Health Records in Primary Care Pediatric Practices.” [DOI] [PubMed]
- 111.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, E. John Orav, Elisabeth Burdick, Eric G. Poon, and David W. Bates. “Physicians and Electronic Health Records: A Statewide Survey.” Archives of Internal Medicine 167 (2007, March 12): 507–512. [DOI] [PubMed]
- 112.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, Eric G. Poon, E. John Orav, Helen G. Lo, Deborah H. Williams, and David W. Bates. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey.” [DOI] [PMC free article] [PubMed]
- 113.Simon, Steven R., Rainu Kaushal, Paul D. Cleary, Chelsea A. Jenter, Lynn A. Volk, E. John Orav, Elisabeth Burdick, Eric G. Poon, and David W. Bates. “Physicians and Electronic Health Records: A Statewide Survey.” [DOI] [PubMed]