Summary
A survey was conducted on 10 polysomnographic studies on the pharmacologic treatment of the sleepiness of narcolepsy. Three studies emplyed the MSLT and 7 employed the MWT as their polygraphic measure of sleep tendency. Statistically and clinically significant therapeutic changes were apparent for pemoline, modafinil, dextroamphetamine and methylphenidate. Codeine, ritanserin and protriptyline did show statistically significant effects. The common feature among the drugs that did produce clinically significant improvements seems to be facilitatory action on central catecholaminergic transmission. Within this group of drugs, only methylphenidate and dextroamphetamine brought MWT sleep latencies to approximately 70% of normal levels.
Keywords: Narcolepsy, Methylphenidate, Amphetamine, Pemoline, CNS stimulants, Multiple Sleep Latency Test, Maintenance of Wakefulness Test
A number of recent treatment studies in narcoleptic patients (1–7) have employed objective measurement of sleepiness by multiple sleep latency testing (MSLT) (8,9) or ability to stay awake by maintenance of wakefulness testing (MWT) (10). By comparing average pre-treatment sleep latencies with averages of best sleep latencies observed on treatment, it was possible to compare the relative efficacy of putative therapeutic agents. And, by using published norms for the MSLT and MWT (6), it was possible to judge the relative efficacy of putative therapeutic agents against normal controls. This report compares the relative efficacy of methylphenidate, dextroamphetamine, protriptyline, modafinil, pemoline, viloxazine, ritanserin, codeine and gamma-hydroxybutyrate for treating excessive sleepiness in patients with narcolepsy.
METHODS
Studies
Table 1 summarizes the relevant particulars of the studies and drugs we evaluated. A total of 169 narcoleptic subjects contributed data to 10 studies. Three of the studies used the MSLT and seven used the MWT for measuring treatment efficacy. Studies varied in the length of treatment (7 days to 14 mo) and the number of doses studied (one to three). We considered results for only the highest (most effective) dose at the time points in treatment when greatest alerting effect was observed.
TABLE 1.
Summary of the study particulars for various drugs evaluated as treatments for sleepiness in patients with narcolepsy
| Drug | Maximum dose | Reference | Number of subjects | Test used | Description of study |
|---|---|---|---|---|---|
| Codeine | 150mg | Fry et al. (1) | 5 | MWT | Open label with treatment lasting 2 or more weeks. |
| Gamma-hydroxybutyrate | 25 mg/kg | Scrima et al. (2) | 12 | MSLT | Open label with treatment lasting 4–14 mo. Concomitant stimulants were allowed. |
| Gamma-hydroxybutyrate | 25 mg/kg | Scrima et al. (3) | 20 | MSLT | Randomized, double blind, crossover with treatment lasting 29 days. |
| Ritanserin | 5 mg | Arends et al. (4) | 33 | MSLT | Placebo controlled, double blind with treatment lasting 4 wk. Concomitant stimulants allowed. |
| Viloxazine | 100mg | Godbout et al. (5,6) | 36 | MWT | Multicenter, placebo controlled, crossover with treatment lasting 6 wk. |
| Pemoline | 112.5mg | Mitler et al. (6) | 14 | MWT | Baseline and three dose levels with each treatment lasting 7 days. |
| Modafinil | 300 mg | Billiard et al. (7) | 21 | MWT | Multicenter, placebo controlled crossover with treatment lasting at least 6 mo. |
| Protriptyline | 60 mg | Mitler et al. (6) | 10 | MWT | Baseline and three dose levels with each treatment lasting 7 days. |
| Dextroamphetamine | 60 mg | Mitler et al. (6) | 5 | MWT | Baseline and three dose levels with each treatment lasting 7 days. |
| Methylphenidate | 60 mg | Mitler et al. (6) | 13 | MWT | Baseline and three dose levels with each treatment lasting 7 days. |
Normal values
For the MSLT, we used the normal sleep latency of 13.4 min according to data from 17 normals (11 males and 6 females aged 33.4 ± 9.9 yr) reported by Mitler et al. (6). The rationale for using the value from this particular study was that the clinical MSLT protocol was employed, which permitted up to 20 min of sleep during MSLT trial. Thus we felt that the MSLT conditions were comparable to those experienced by most of the narcoleptic patients who served in the 10 studies under consideration here. Moreover, our mean MSLT figure of 13.4 min is within the 11.5 ± 5.1-min range reported by Roehrs et al. (11) and within the 13.8 ± 1.4-min range reported by Levine et al. (12) for normals between the ages of 30 and 39 yr. For the MWT, we used the normal baseline sleep latency of 18.9 min and the normal treatment (placebo purported to be a stimulant) sleep latency of 17.6 min according to data from nine normals (four males and five females aged 39.2 ± 8.4 yr) also reported by Mitler et al. (6).
RESULTS
Table 2 summarizes the baseline and treatment results for the various drugs. There was marked variability from study to study in baseline sleep latencies. Six drugs produced changes over baseline of more than 25%, but this increase is not always in accord with the level of statistical significance (see Table 2). For example, codeine was observed to produce a 2.8-min increase over baseline, but did not produce a statistically significant increase in MWT sleep latency, largely because only five patients were studied.
TABLE 2.
Baseline and treatment sleep latencies for the various drugs expressed as a percent of normal levels
| Drug | Reference | Baseline Sleep latency | % Normal | Treatment sleep latency | % Normal | Change | p Level |
|---|---|---|---|---|---|---|---|
| Codeine | Fry et al. (1) | 3.00 | 15.9 | 5.80 | 33.0 | 2.8 | NS |
| Gamma-hydroxybutyrate | Scrima et al. (2) | 1.40 | 10.4 | 3.00 | 22.4 | 1.6 | 0.05 |
| Gamma-hydroxybutyrate | Scrima et al. (3) | 2.50 | 18.7 | 2.80 | 20.9 | 0.3 | 0.07 |
| Ritanscrin | Arends et al. (4) | 5.70 | 42.5 | 6.30 | 47.0 | 0.6 | NS |
| Viloxazine | Godbout et al. (5,6) | 7.09 | 37.5 | 8.39 | 47.7 | 1.3 | 0.03 |
| Pemoline | Mitler et al. (6) | 7.60 | 40.2 | 9.40 | 53.4 | 1.8 | 0.05 |
| Modafinil | Billiard et al. (7) | 7.06 | 37.4 | 9.73 | 55.3 | 2.7 | 0.01 |
| Protriptyline | Mitler et al. (6) | 9.28 | 49.1 | 9.59 | 54.5 | 0.3 | NS |
| Dextroamphetamine | Mitler et al. (6) | 6.58 | 34.8 | 12.37 | 70.3 | 5.8 | 0.01 |
| Methylphenidate | Mitler et al. (6) | 10.43 | 55.2 | 14.06 | 79.9 | 3.6 | 0.01 |
The MSLT normal value is 13.4 min. The MWT normal value is 18.9 and 17.6 for baseline and treatment, respectively (see text for rationales).
DISCUSSION
A survey of various studies on the pharmacologic treatment of the sleepiness of narcolepsy disclosed that no drug brought narcoleptic patients to normal levels of sleepiness. As with all post hoc quantitative reviews, there are problems in interpretation: (A) Three studies employed the MSLT and seven employed the MWT as their polygraphic measure of sleep tendency. This raises the theoretical issue that it may be difficult to know whether any change in sleep latency on the MSLT is proportional to therapeutic effect. Our experience has been that the MSLT is not so insensitive to treatment-related changes as to make it unusable in drug efficacy evaluations. For example, a multicenter study of viloxazine (see table 3 in reference 6) found that the MSLT could detect changes in alertness associated with viloxazine treatment although the MWT was considerably more sensitive. (B) There was marked variability from study to study in baseline sleep latencies. We cannot supply a certain explanation for this variability except to suggest that studies done earlier in time, studies done on non-FDA-approved drugs and studies done at primarily research facilities may enroll narcoleptic subjects with more severe symptoms.
In spite of the aforementioned comparability problems, several broad trends can still be seen in the 10 studies evaluated here. The facts that studies varied in their choice of polygraphic protocol and the severity of symptoms really did not mask the presence of clinically significant therapeutic changes apparent for pemoline, modafinil, dextroamphetamine and methylphenidate. Figure 1 is presented as a discussion aid and gives a graphic display of the efficacy of the drugs expressed as percent of normal sleep latency (see Table 2). Gamma-hydroxybutyrate, viloxazine, pemoline, modafinil, dextroamphetamine and methylphenidate were reported to produce statistically significant improvements in the level of sleepiness as objectively measured by MSLT or MWT. Codeine, ritanserin and protriptyline were not reported to have statistically significant effects. Codeine produced proportionately large changes in MWT sleep latencies from baseline levels. However, because the codeine subjects had such low MWT sleep latencies both before and during treatment, the clinical significance of codeine’s effect is modest. For gamma-hydroxybutyrate, as Scrima and colleagues (2,3) point out, the primary therapeutic effect is in the control of cataplexy. Gamma-hydroxybutyrate’s effect on sleepiness, although just reaching, or approaching statistical significance, must still be judged as minimal because of the very short MSLT sleep latencies observed during treatment.
FIG. 1.
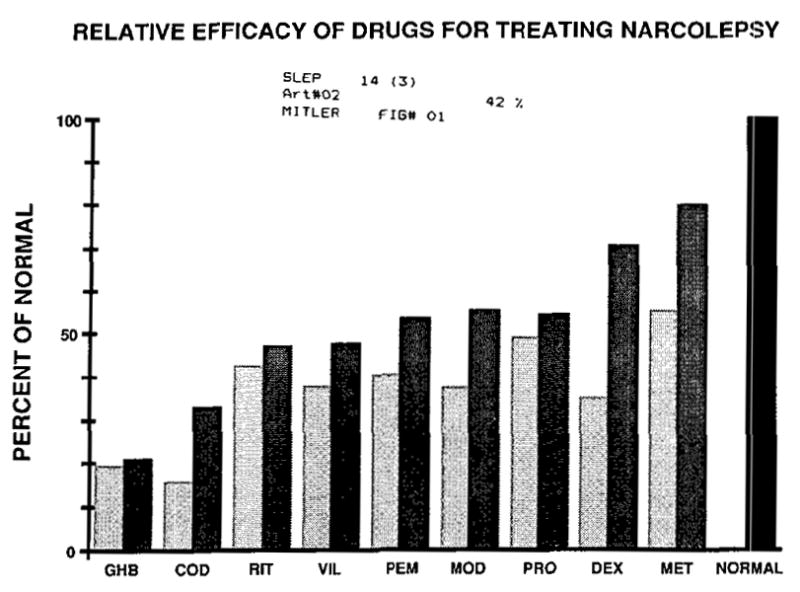
Relative efficacy of drugs for treating excessive sleepiness in patients with narcolepsy presented in terms of percent of normal levels of sleepiness (see Methods). The lightest shading denotes baseline values. The intermediate shading denotes treatment values. The darkest shading is used only for the normal values. Abbreviations: GHB = gamma-hydroxybulyrale; COD = codeine; RIT = ritanserin; VIL = viloxazine; PEM = pemoline; MOD = modafinil; PRO = protriptyline; DEX = dextroamphetamine; MET = methylphenidate.
The common feature among the drugs that did produce clinically significant improvements seems to be facilitatory action on central catecholaminergic transmission (methylphenidate, dextroamphetamine, modafinil and pemoline). Within this group of drugs, only methylphenidate and dextroamphetamine (which stimulate central release of dopamine and, to some extent, norepinephrine) brought MWT sleep latencies to above 70% of normal levels.
Acknowledgments
This work was supported by PHS Grants, R01 NS20459, MH47680, and R03 AA08235 to Dr. Mitler, by Clinical Research Center Grant RR00833 to Scripps Clinic and Research Foundation and by a grant from the American Narcolepsy Association. This is publication number 6555-NP from the Research Institute of Scripps Clinic. We are grateful to Ms. Barbara Bigby for her editorial assistance.
References
- 1.Fry JM, Pressman MR, DiPhillipo MA, Forst-Paulus M. Treatment of narcolepsy with codeine. Sleep. 1986;9:269–74. doi: 10.1093/sleep/9.1.269. [DOI] [PubMed] [Google Scholar]
- 2.Scrima L, Johnson FH, Thomas EE, Hiller FC. Effects of gamma-hydroxybutyrate (GHB) on multiple sleep latency test (MSLT) in narcolepsy patients: a long term study. Sleep Res. 1990;19:288. doi: 10.1093/sleep/13.6.479. [DOI] [PubMed] [Google Scholar]
- 3.Scrima L, Hartman PG, Johnson FH, Thomas EE, Hiller FC. Effects of gamma-hydroxybutyrate (GHB) on sleep of narcolepsy patients: a double-blind study. Sleep. 1990;13(6):479. doi: 10.1093/sleep/13.6.479. [DOI] [PubMed] [Google Scholar]
- 4.Lammers GJ, Arends J, Declerck AC, Kamphuisen HAC, Schouwink G, Troost J. Ritanserin, a serotonin 5-HT2 antagonist, reduces daytime sleepiness in narcolepsy (abstract). 10th Congress of The European Sleep Research Society; Strasbourg. 1990. p. 258. [Google Scholar]
- 5.Godbout R, Poirier G, Montplaisir J. New treatments for narcolepsy (viloxazine). Narcolepsy 3rd International Symposium; San Diego. June 1988; pp. 79–81. [Google Scholar]
- 6.Mitler MM, Hajdukovic RM, Erman M, Koziol JA. Narcolepsy. J Clin Neurophysiol. 1990;7:93–118. doi: 10.1097/00004691-199001000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billiard M. New treatments for narcolepsy (modafinil). Paper presented at the NIH Workshop on Narcolepsy; July 16, 1990; Bethesda, Maryland. [Google Scholar]
- 8.Richardson GS, Carskadon MA, Flagg W, van den Hoed J, Dement WC, Mitler MM. Excessive daytime sleepiness in man: multiple sleep latency measurement in narcoleptic and control subjects. Electroencephalogr Clin Neurophysiol. 1978;45:621–7. doi: 10.1016/0013-4694(78)90162-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carskadon MA, Dement WC, Mitler MM, Rolh T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a slandard measure of sleepiness. Sleep. 1986;9:519–24. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 10.Mitler MM, Gujavarty KS, Browman CP. Maintenance of wakefulness test: a polysomnographic technique for evaluating treatment in patients with excessive somnolence. Electroencephalogr Clin Neurophysiol. 1982;53:658–61. doi: 10.1016/0013-4694(82)90142-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roehrs T, Zorick F, McLeaghan A, Sicklesteel J, Lamphere J, Wittig R, Roth T. Sleep and MSLT norms for middle age adults. Sleep Res. 1984;13:87. [Google Scholar]
- 12.Levine B, Roehrs T, Lamphere J, Zorick F, Stepanski E, Roth T. Daytime sleepiness in young adults. Sleep Res. 1987;16:207. [Google Scholar]


