Abstract
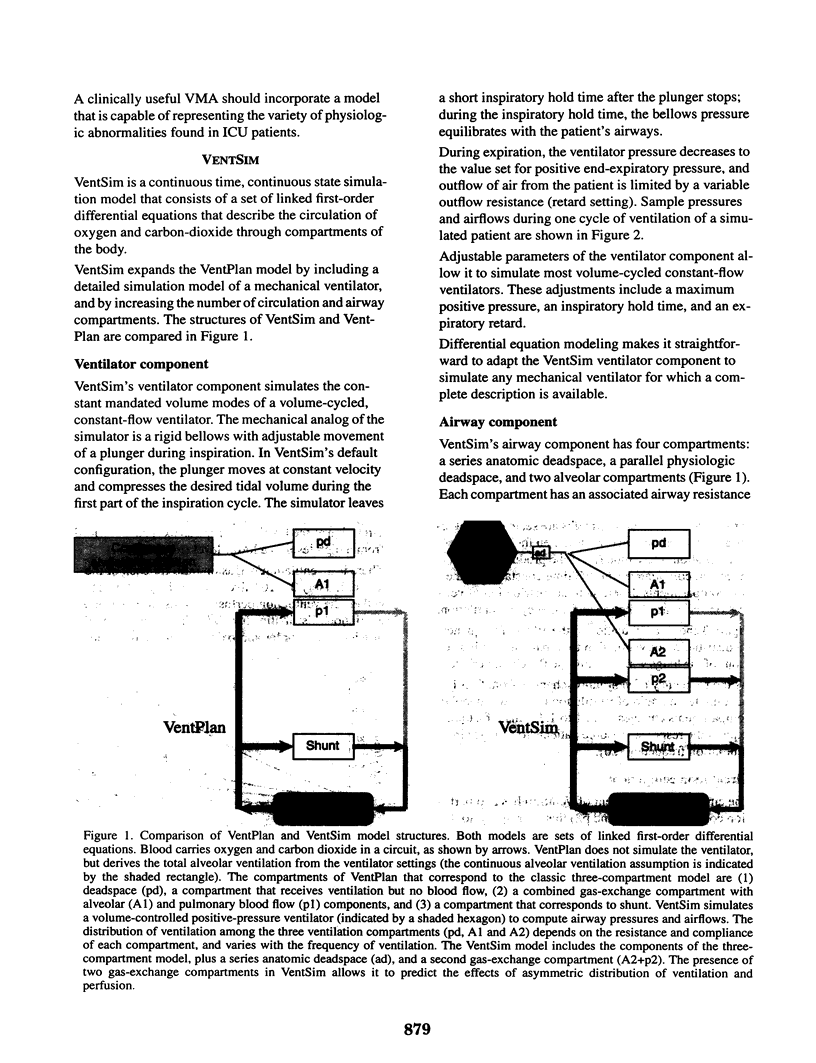
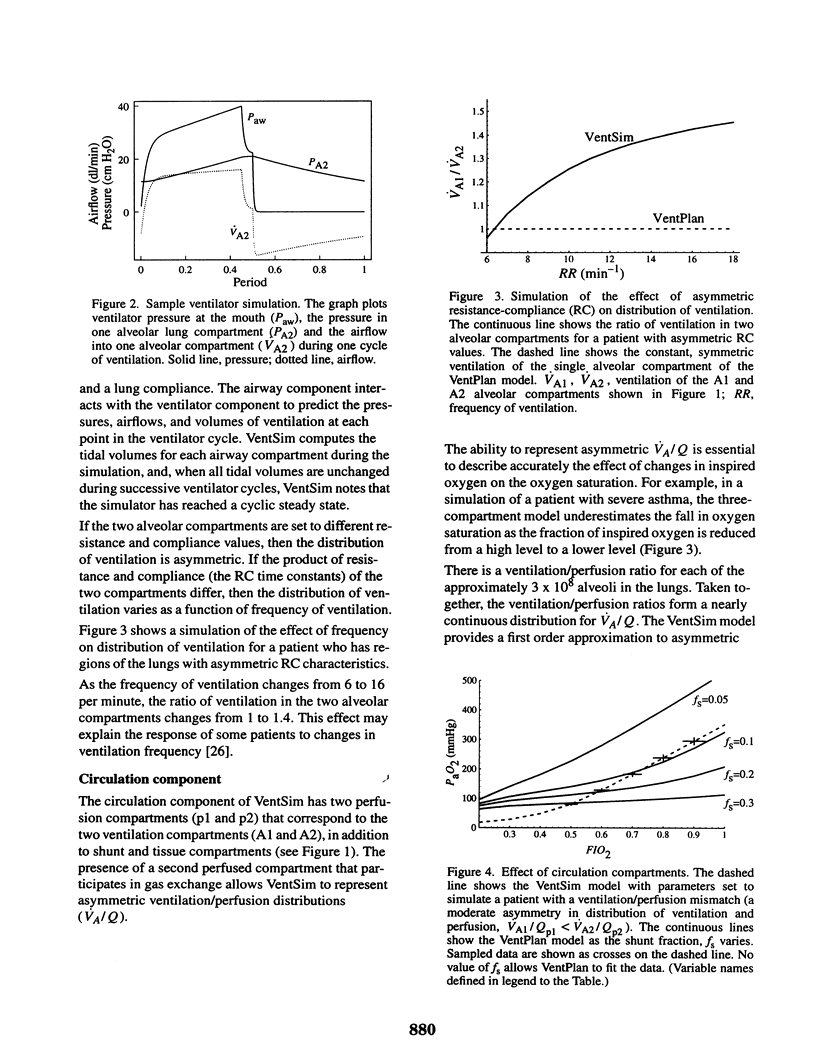
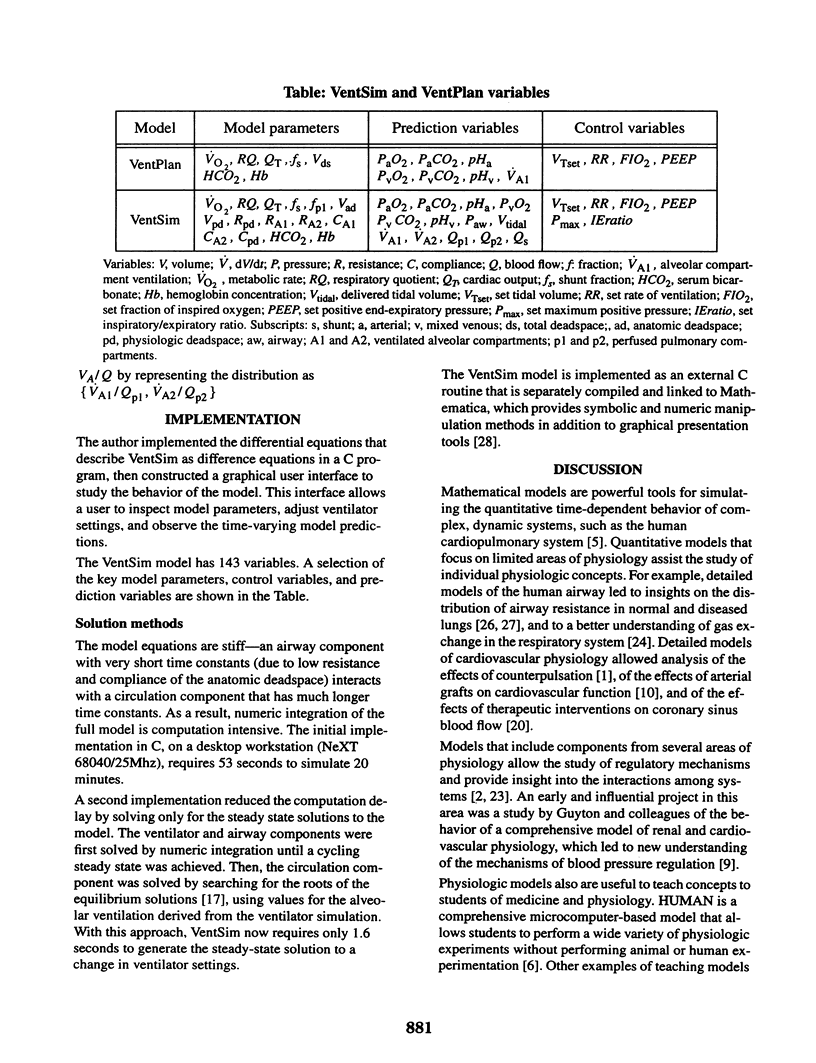
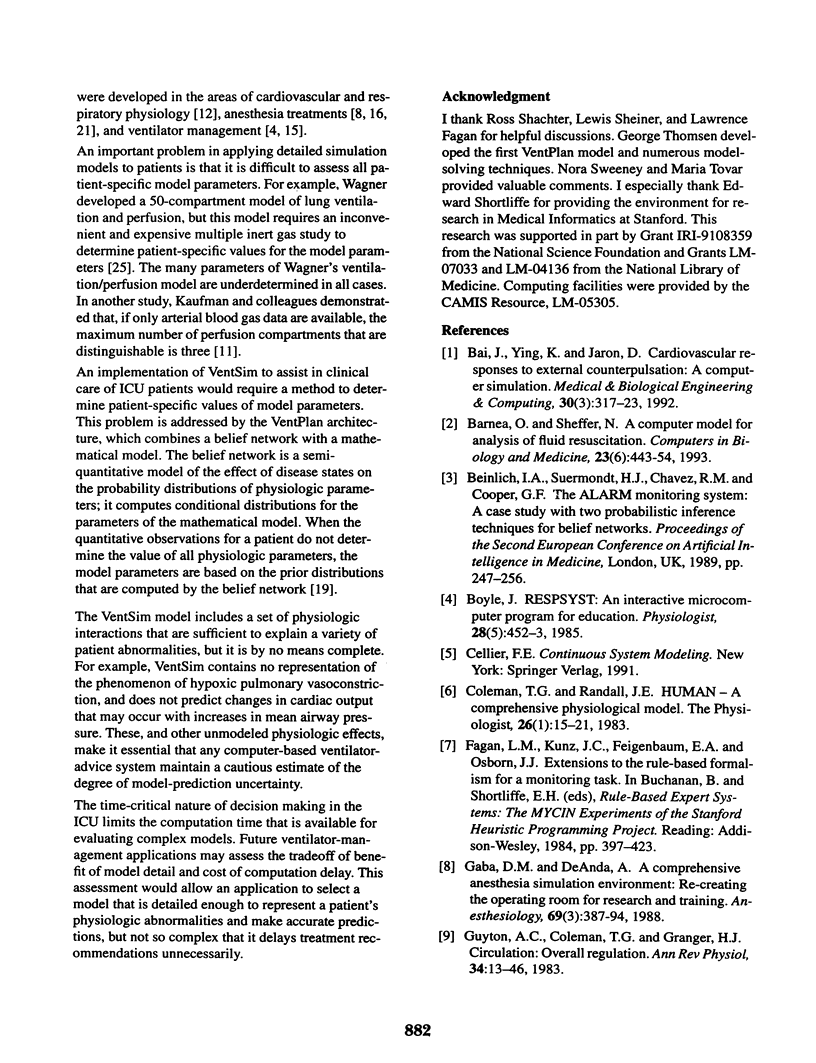
VentSim is a quantitative model that predicts the effects of alternative ventilator settings on the cardiopulmonary physiology of critically ill patients. VentSim is an expanded version of the physiologic model in VentPlan, an application that provides ventilator-setting recommendations for patients in the intensive care unit. VentSim includes a ventilator component, an airway component, and a circulation component. The ventilator component predicts the pressures and airflows that are generated by a volume-cycled, constant-flow ventilator. The airway component has anatomic and physiologic deadspace compartments, and two alveolar compartments that participate in gas exchange with two pulmonary blood-flow compartments in the circulatory component. The circulatory component also has a shunt compartment that allows a fraction of blood flow to bypass gas exchange in the lungs, and a tissue compartment that consumes oxygen and generates carbon dioxide. The VentSim model is a set of linked first-order difference equations, with control variables that correspond to the ventilator settings, dependent variables that correspond to the physiologic state, and one independent variable, time. Because the model has no steady state solution, VentSim solves the equations by numeric integration, which is computation intensive. Simulation results demonstrate that VentSim predicts the effects of a variety of physiologic abnormalities that cannot be represented in less complex models such as the VentPlan model. For a ventilator-management application, the time-critical nature of ventilator-setting decisions limits the use of complex models. Advanced ventilator-management applications may include a mechanism to select patient-specific models that balance the trade-off of benefit of model detail and cost of computation delay.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bai J., Ying K., Jaron D. Cardiovascular responses to external counterpulsation: a computer simulation. Med Biol Eng Comput. 1992 May;30(3):317–323. doi: 10.1007/BF02446970. [DOI] [PubMed] [Google Scholar]
- Barnea O., Sheffer N. A computer model for analysis of fluid resuscitation. Comput Biol Med. 1993 Nov;23(6):443–454. doi: 10.1016/0010-4825(93)90092-f. [DOI] [PubMed] [Google Scholar]
- Boyle J., 3rd RESPSYST: an interactive microcomputer program for education. Physiologist. 1985 Oct;28(5):452–453. [PubMed] [Google Scholar]
- Coleman T. G., Randall J. E. HUMAN. A comprehensive physiological model. Physiologist. 1983 Feb;26(1):15–21. [PubMed] [Google Scholar]
- Gaba D. M., DeAnda A. A comprehensive anesthesia simulation environment: re-creating the operating room for research and training. Anesthesiology. 1988 Sep;69(3):387–394. [PubMed] [Google Scholar]
- Guyton A. C., Coleman T. G., Granger H. J. Circulation: overall regulation. Annu Rev Physiol. 1972;34:13–46. doi: 10.1146/annurev.ph.34.030172.000305. [DOI] [PubMed] [Google Scholar]
- Helal M. A., Watts K. C., Marble A. E. Hydrodynamic simulation of arterial networks which include compliant and rigid bypass grafts. J Biomech. 1994 Mar;27(3):277–287. doi: 10.1016/0021-9290(94)90004-3. [DOI] [PubMed] [Google Scholar]
- Kaufman R. D., Patterson R. W., Lee A. S. Derivation of VA/Q distribution from blood-gas tensions. Br J Anaesth. 1987 Dec;59(12):1599–1609. doi: 10.1093/bja/59.12.1599. [DOI] [PubMed] [Google Scholar]
- Miller P. L. Goal-directed critiquing by computer: ventilator management. Comput Biomed Res. 1985 Oct;18(5):422–438. doi: 10.1016/0010-4809(85)90020-5. [DOI] [PubMed] [Google Scholar]
- Petrini M. F. Distribution of ventilation and perfusion: a teaching model. Comput Biol Med. 1986;16(6):431–444. doi: 10.1016/0010-4825(86)90067-3. [DOI] [PubMed] [Google Scholar]
- Philip J. H. Gas Man--an example of goal oriented computer-assisted teaching which results in learning. Int J Clin Monit Comput. 1986;3(3):165–173. doi: 10.1007/BF01716358. [DOI] [PubMed] [Google Scholar]
- Rudowski R., Bokliden A., Carstensen A., Gill H., Ludwigs U., Matell G. Multivariable optimization of mechanical ventilation. A linear programming approach. Int J Clin Monit Comput. 1991;8(2):107–115. doi: 10.1007/BF02915544. [DOI] [PubMed] [Google Scholar]
- Rutledge G. W., Thomsen G. E., Farr B. R., Tovar M. A., Polaschek J. X., Beinlich I. A., Sheiner L. B., Fagan L. M. The design and implementation of a ventilator-management advisor. Artif Intell Med. 1993 Feb;5(1):67–82. doi: 10.1016/0933-3657(93)90006-o. [DOI] [PubMed] [Google Scholar]
- Schwid H. A. A flight simulator for general anesthesia training. Comput Biomed Res. 1987 Feb;20(1):64–75. doi: 10.1016/0010-4809(87)90019-x. [DOI] [PubMed] [Google Scholar]
- Wagner P. D., Smith C. M., Davies N. J., McEvoy R. D., Gale G. E. Estimation of ventilation-perfusion inequality by inert gas elimination without arterial sampling. J Appl Physiol (1985) 1985 Aug;59(2):376–383. doi: 10.1152/jappl.1985.59.2.376. [DOI] [PubMed] [Google Scholar]
- Wiggs B. R., Moreno R., Hogg J. C., Hilliam C., Paré P. D. A model of the mechanics of airway narrowing. J Appl Physiol (1985) 1990 Sep;69(3):849–860. doi: 10.1152/jappl.1990.69.3.849. [DOI] [PubMed] [Google Scholar]


