Abstract
Context
There is limited information that accounts for comorbidity on the impact of role disability associated with a wide range of mental and physical disorders in population-based samples.
Objective
To estimate the comparative effects of common mental and physical conditions on role disability in the general population using a novel method that accounts for comorbidity.
Design
Direct interviews about physical and mental conditions during the past year.
Setting
The National Comorbidity Survey Replication, a nationally representative series of face-to-face interviews.
Patients
A nationally representative sample of adults living in households (N=5962 respondents, 18 years and older).
Main Outcome Measure
Disability in major life roles was assessed with the World Health Organization Disability Assessment Schedule. Simulations that allow for complex interactions among conditions were used to estimate the conditions’ effects on disability days, when respondents were completely unable to carry out their usual daily activities because of problems with mental or physical health, in the past 12 months.
Results
An estimated 53.4 % of US adults have 1 or more of the mental or physical conditions assessed in the survey. These respondents report an average 32.1 more role-disability days in the past year than demographically matched controls, equivalent to nearly 3.6 billion days of role disability in the population. Musculoskeletal disorders and major depression had the greatest effects on disability days. Mental conditions accounted for more than half as many disability days as all physical conditions at the population level. Associations of specific conditions with disability decreased substantially after controlling for comorbidity, suggesting that prior studies, which generally did not control for comorbidity, overestimated disease-specific effects.
Conclusion
The staggering amount of health-related disability associated with mental and physical conditions should be considered in establishing priorities for the allocation of health care and research resources.
As health case spending in the United States continues to rise,1 it will be increasingly necessary to make thoughtful decisions regarding resource allocation. Such choices should be based on accurate information about the individual and population costs of particular conditions as well as the cost-effectiveness of specific interventions for these conditions. Costs of illness include direct treatment costs and indirect costs related to morbidity and mortality. Although direct costs can readily be measured through transactional billing data, limited systematic information exists on indirect costs either at the individual level (eg, impaired functioning in work and social roles, family burden)2,3 or at the societal level (eg, lost productivity, workers’ compensation).4,5 The absence of indirect cost data leads to unrealistically low estimates of the total costs of illness because available evidence suggests that indirect costs make up a substantial part of these overall costs.6–8
The importance of role disability has become increasingly recognized as a major source of indirect costs of illness because of its high economic impact on ill workers, their employers, and society.9–11 However, synthesis of estimates of condition-specific indirect costs from previous studies has been precluded by methodological differences in sampling source, measures, time frames of assessment, and specific conditions included in the analyses.9 Moreover, only a limited number of studies have controlled for comorbidity in generating estimates of disability6,12–17 and none has estimated condition-specific effects for a wide range of mental and physical conditions controlling for comorbidity in a population-based sample.
The current report presents, to our knowledge, the first nationally representative general population estimates of the adverse effects of a wide range of mental and chronic physical conditions on role disability. The aim is to estimate the relative effects of a number of commonly occurring conditions on role disability at both the individual and population levels using a novel approach that accounts for comorbidity.
METHODS
SAMPLE
Data come from the National Comorbidity Survey Replication (NCS-R),18,19 a nationally representative series of direct interviews based on a multistage clustered area probability sample of the population of US adults living in households. The interview was in 2 parts. Part 1 was administered to the full sample of 9282 respondents to assess core mental disorders. The response rate was 70.9%. A probability subsample of hard-to-recruit, predesignated respondents was selected for a brief telephone nonrespondent survey, the results of which were used to weight the main sample for nonresponse bias. The Human Subjects committees of Harvard Medical School and the University of Michigan both approved these recruitment and consent procedures. Part 2 was administered to a probability subsample of 5692 respondents that included all part 1 respondents with a core mental disorder plus a roughly 25% probability subsample of other part 1 respondents. Part 2 assessed chronic physical conditions, risk factors, and costs of illness. The part 2 sample is the focus of the current report. This sample was weighted to adjust for differential probabilities of selection within households, over-sampling of part 1 respondents with mental disorders, differential nonresponse, and residual discrepancies between the sample and the US population on the cross-classification of basic demographic and geographic variables. For the purposes of the current report, the sample was also weighted to adjust for seasonal variation in sample size. More details about the NCS-R sample design are reported elsewhere.18
MEASURES
Role disability was assessed with the World Health Organization Disability Assessment Schedule.20 Respondents were asked to report the number of days of the past 30 days when they were totally unable to work or carry out other usual activities because of problems with physical health, emotions or nerves, or use of alcohol or drugs. Good concordance of reported disability days has been documented both with payroll records of employed people21,22 and with prospective daily diary reports.23
Physical conditions were assessed with a standard chronic conditions checklist based on the list used in the US National Health Interview Survey24,25 (http://www.hcp.med.harvard.edu/ncs/replication.php). Checklists of this sort have been widely used in prior population-based studies and have been shown to yield more complete and accurate reports than estimates derived from responses to open-ended questions.26 Methodological studies in both the United States and the United Kingdom have documented good concordance between such condition reports and medical records.27–29 The prevalence estimates of these conditions in the NCS-R are in accordance with those in other large-scale community surveys.25
Seven classes of chronic physical conditions were assessed, including cancer, cardiovascular problems (heart attack, hypertension, other heart disease, stroke), diabetes mellitus, digestive problems (irritable bowel syndrome, ulcer), musculoskeletal problems (arthritis, chronic back/neck pain), respiratory problems (allergies, asthma, chronic obstructive pulmonary disease), and sensory organ impairment (hearing impairment, vision impairment). Respondents were asked to report each condition’s lifetime presence and occurrence during the past 12 months of each condition. This report considers only conditions present in the past 12 months.
Mental disorders were assessed with version 3.0 of the World Health Organization Composite International Diagnostic Interview (CIDI),30 a fully structured, lay-administered interview designed to generate research diagnoses of commonly occurring DSM-IV31 mental disorders. The 4 classes of conditions considered herein include anxiety disorders (panic disorder, generalized anxiety disorder, agoraphobia, specific phobia, social phobia, obsessive-compulsive disorder, posttraumatic stress disorder), mood disorders (major depressive episode, dysthymic disorder, bipolar disorder), impulse-control disorders (intermittent explosive disorder, adult attention-deficit/hyperactivity disorder, oppositional defiant disorder), and substance use disorders (alcohol and drug abuse with or without dependence). Generally good concordance was found in an NCS-R clinical calibration study between CIDI diagnoses and independent clinical assessment based on the Structured Clinical Interview for DSM-IV32 for anxiety, mood, and substance use disorders.33 The CIDI diagnoses of impulse-control disorders have not been validated.
Sociodemographic controls were included for age, sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), education (<high school graduate, high school graduate, some college, college graduate), family income (0–1.5, 1.6–3, 3.1–6, ≥6 times the poverty line for a family the size of the respondent’s family), and the multivariate profile of variables assessing marital status (married/cohabiting, never married, separated/divorced, widowed), employment status (employed, homemaker, student, retired, other), and the number and ages of children (0, 1, ≥2 in each of the age ranges 0–5, 6–12, 13–19, and ≥20 years).
ANALYSIS METHODS
Odds ratios were calculated to estimate the strength of associations in each of the 378 logically possible pairs among the 30 conditions considered in the analysis. Linear regression analysis was used to examine the associations of individual conditions and all conditions together with number of disability days. Multiple regression analysis with dummy predictor variables for specific conditions (eg, arthritis, depression) and combinations of comorbid conditions (eg, arthritis with depression) was used to evaluate the possibility of synergistic predictive effects of comorbid conditions on role disability. All regression equations included controls for age, sex, race/ethnicity, education, and a cross-classification of sociodemographic variables that define role incumbency (marital status, employment status, and number and ages of children).
Simulation was used to estimate the separate and joint incremental predictive effects of groups of conditions and of each individual condition. This was done by calculating the predicted number of disability days for each respondent based on the coefficients in the full best-fitting regression model and then calculating the same outcome based on simulated data sets that classified 1 or more conditions to be absent. Differences in mean predicted disability days between these 2 models were then compared and interpreted as incremental predictive effects of the conditions fixed to be absent in the restrictive models. This approach resolves the problem of estimating summary effects of conditions in the presence of multiple interactions. Because the condition specific simulations were based on the implausible assumption that prevalence of other conditions would not change in the absence of the focal condition, we also evaluated the implications of this assumption by carrying out additional simulations that estimated the combined effects of all conditions in each class by classifying multiple conditions as absent.
The recall periods of the predictors (conditions present in the past 12 months) and the outcome (number of disability days in the past 30 days) were allowed to differ based on the assumption that conditions can be recalled over a longer period than disability days. Effect size estimates were annualized to correct for this inconsistency between the recall periods of the predictors and outcome using the constant multiplier 365/30. This transformation should have yielded unbiased estimates of the associations between 12-month conditions and number of disability days in the past 12 months because the 30-day period before the interview can be considered a random month in the past year because the survey was carried out in representative subsamples throughout the year. Importantly, for purposes of justifying this assumption, respondents were randomly assigned to subsamples that differed in month of recruitment, and seasonal differences in subsample size were removed for purposes of this analysis by weighting.
Standard errors of estimates were generated using the jackknife repeated-replications method34 implemented in an SAS macro35 to adjust for the weighting and clustering in the NCS-R sample design. This method was used at the level of the simulation; that is, each simulation was replicated 84 times (based on the existence of 84 geographic primary sampling error calculation units in the sample) to generate an empirical distribution of coefficient estimates to calculate standard errors. All significance tests were evaluated at the .05 level with 2-sided tests.
RESULTS
PREVALENCE OF DISABILITY DAYS
The annualized mean of self-reported disability days was 34.6 in the total sample, equivalent to more than 7.2 billion days per year if applied to the US population among people in the age range of the sample (Table 1). Number of disability days was significantly related to employment status, with means varying from a low of 17.9 among students to a high of 121.4 among the unemployed/disabled. Employment status was controlled in all subsequent analyses.
Table 1.
Estimated Annual Individual-Level and US Population–Level Prevalence of Disability Days
| Estimated Annual Prevalence, Mean (SE) |
|||
|---|---|---|---|
| Employment Status | Sample Distribution, % | Individual Level (in Days) | Population Levela (in Millions of Days) |
| Employed | 66.7 | 20.6 (1.1) | 2876 (151) |
| Student | 3.1 | 17.9 (3.6) | 114 (23) |
| Homemaker | 5.6 | 40.6 (7.2) | 474 (84) |
| Retired | 15.0 | 42.2 (5.2) | 1319 (164) |
| Other | 9.7 | 121.4 (8.8) | 2463 (179) |
| Total | 100.0 | 34.6 (1.5) | 7247 (321) |
Population projections are based on the population size estimate from the US Bureau of the Census for 2001 in conjunction with the employment status distribution estimates from the sample.
INDIVIDUAL-LEVEL ASSOCIATIONS OF CONDITIONS WITH ROLE DISABILITY
A statistical model was built of the multivariate associations among conditions in predicting disability days at the individual level. We began with a separate linear regression model for each condition (gross effects model), which estimated the total association of each condition with the outcome, controlling for sociodemographic variables but not for other conditions. For example, cancer was associated with 41.1 disability days. All 30 conditions had positive coefficients in this model, 27 of them significant at the .05 level (Table 2, “Gross Coefficient” column). A series of multivariate models was then estimated, which included all 27 significant conditions from the gross effects model (results available on request). The additive version of this model was revised to investigate the implications of combining conditions within classes. For example, alcohol and drug abuse with dependence were combined based on the finding of equivalent coefficients for either or both of these conditions.
Table 2.
Associations of Physical and Mental Conditions With Role Disability at the Individual Level (Gross and Net Coefficients)
| Days (SE) |
||
|---|---|---|
| Gross Coefficienta | Simulated Net Coefficientb | |
| Physical conditions | ||
| Cancer | 41.1c (17.8) | 33.8c (15.9) |
| Cardiovascular | ||
| Heart attack | 35.9c (10.9) | 26.6c (10.6) |
| Heart disease | 27.4c (6.9) | … |
| High blood pressure | 15.6c (3.9) | … |
| Stroke | 55.1c (9.5) | 39.2c (10.6) |
| Diabetes mellitus | 30.5 (10.7) | |
| Digestive | ||
| Irritable bowel syndrome | 71.5c (18.8) | 53.3c (23.4) |
| Ulcer | 45.0c (7.8) | 22.3c (7.9) |
| Musculoskeletal | ||
| Arthritis | 21.6c (3.2) | 6.6c (2.6) |
| Back/neck | 38.3c (3.9) | 29.4c (4.0) |
| Respiratory | ||
| Allergies | 8.1c (2.6) | … |
| Asthma | 11.7c (3.9) | … |
| Chronic obstructive pulmonary disease | 46.0c (10.7) | 38.5c (10.3) |
| Sensory organ disorders | ||
| Hearing impaired | 28.9c (9.5) | 23.7c (7.0) |
| Vision impaired | 40.7c (8.7) | 21.4c (7.2) |
| Mental conditions | ||
| Anxiety disorders | ||
| Agoraphobia | 59.4c (13.4) | 21.0c (4.9) |
| Generalized anxiety disorder | 35.7c (7.1) | 16.9c (2.1) |
| Panic disorder | 47.4c (8.3) | 17.5c (2.8) |
| Posttraumatic stress disorder | 40.6c (8.6) | 15.2c (3.1) |
| Separation anxiety disorder | 47.3c (19.5) | 16.3c (5.4) |
| Social phobia | 37.7c (3.7) | 14.9c (2.0) |
| Specific phobia | 32.7c (4.1) | 13.7c (2.1) |
| Impulse control disorders | ||
| Attention-deficit/hyperactivity disorder | 50.7c (10.0) | … |
| Oppositional defiant disorder | 60.1c (19.1) | … |
| Intermittent explosive disorder | 16.1c (7.2) | … |
| Mood disorders | ||
| Bipolar I disorder | 51.4c (8.0) | 23.9c (7.5) |
| Bipolar II disorder | 5.5 (9.6) | … |
| Major depressive disorder | 42.5c (3.9) | 27.5c (4.1) |
| Substance conditions | ||
| Alcohol abuse or dependenced | 30.7c (6.5) | 24.9c (6.7) |
| Drug abuse or dependenced | 20.5 (10.5) | 14.9c (5.6) |
Abbreviation: ellipses, the condition was not a significant predictor in the model.
Estimates are based on linear regression controlling for age, sex, race/ethnicity, education, and the cross-classification of marital status, employment status, and the number and ages of children.
Estimates are based on linear regression controlling for the effects of variables in gross models plus comorbid disorders.
Significant at the .05 level in a 2-sided test.
The category includes abuse with or without dependence. Dependence without abuse was not assessed.
This model was then revised to include interactions. Nearly 25% of all logically possible 2-way interactions were significant at the .05 level. The vast majority of these interactions were negative, indicating that the effects of comorbid conditions are less than the sum of the effects of the 2 conditions alone. Higher-order interactions were also evaluated but were not significant either in global tests or in tests of interactions among broad profiles (eg, number of conditions, number of classes of conditions). The final nonadditive multivariate model (ie, the model including separate predictors for a number of different conditions as well as for significant interactions among conditions) was used to estimate the net association of each condition with disability days, controlling for other conditions using the simulation approach described earlier (Table 2, “Simulated Net Coefficient” column). For example, those with cancer had an average of 7.3 fewer days of disability after controlling for the effects of comorbid disorders.
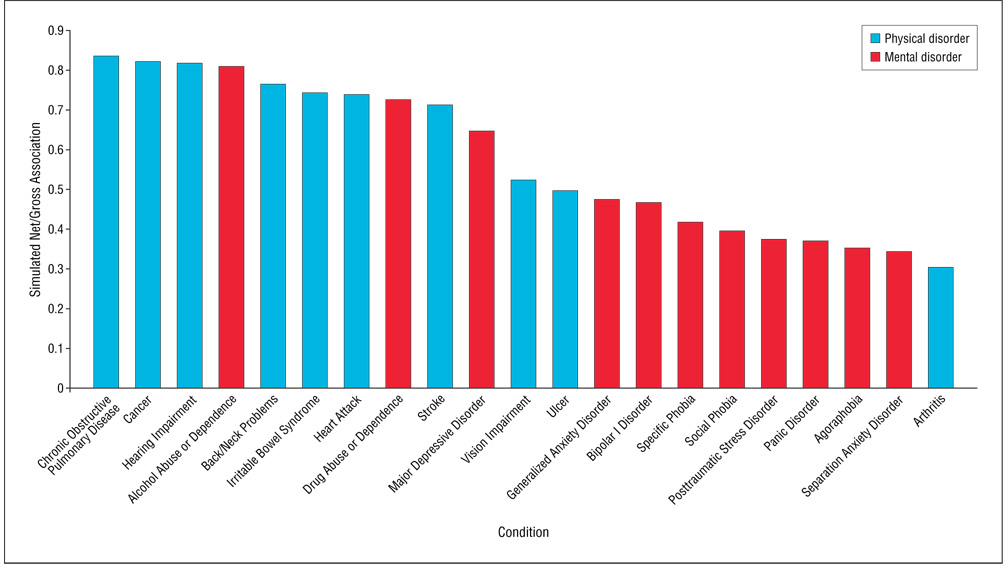
To examine the impact of comorbidity on individual level associations more fully, the effect of each condition was compared before and after incorporating comorbidity into the model (Figure 1). The coefficients in the models that controlled for comorbidity are, on average, only about half (57.9%) as large as the coefficients in the models that did not control for comorbidity (interquartile range, 39.5%–74.5%), with a range from 84% for chronic obstructive pulmonary disease and cancer to 31% for arthritis. The ratios are generally smaller for mental than physical conditions, reflecting the stronger and more consistent effects of comorbidity involving mental, as opposed to physical, conditions. The results do, however, document powerful effects of comorbidity in both types of conditions.
Figure 1.
Net vs gross estimates of disability of chronic mental and physical conditions among individuals in the US population.
POPULATION-LEVEL ASSOCIATIONS OF CONDITIONS WITH ROLE DISABILITY
The 30 conditions differ widely in self-reported prevalence, from a high of 27.3% for arthritis to a low of 0.4% for drug dependence (Table 3, “12-Month Prevalence” column). The individual-level associations in the simulated net effects model (Table 2) were projected to population-level estimates by taking into consideration their prevalence and standard errors to yield an estimate of the number of disability days per year in the US population associated with specific conditions (Table 3, “US Days per Year” column). As with the individual-level data, back/neck pain (1167.8 million disability days per year) and major depression (386.6 million days) had the largest population-level coefficients. Arthritis, despite a small individual-level coefficient, had the third largest population-level coefficient (374.6 million days) because of its very high prevalence.
Table 3.
Prevalence and Associations of Chronic Physical and Mental Conditions With Role Disability at the Population Level (Simulated Net Coefficientsa)
| 12-Month Prevalence, b % (SE) | US Days per Year in Millions, c No. (SE) | |
|---|---|---|
| Physical conditions | ||
| Cancer | 1.0 (0.2) | 71.5 (33.7) |
| Cardiovascular | ||
| Heart attack | 3.7 (0.4) | 204.0 (81.3) |
| Stroke | 2.7 (0.3) | 220.8 (59.6) |
| All cardiovascular | 5.8 (0.4) | 424.8 (85.4) |
| Chronic obstructive pulmonary disease | 2.2 (0.3) | 176.3 (47.1) |
| Digestive | ||
| Irritable bowel syndrome | 0.9 (0.2) | 104.3 (45.9) |
| Ulcer | 2.4 (0.2) | 112.7 (39.9) |
| All digestive | 3.3 (0.2) | 217.0 (55.8) |
| Musculoskeletal | ||
| Back/neck pain | 19.0 (0.8) | 1167.8 (159.2) |
| Arthritis | 27.3 (0.9) | 374.6 (150.5) |
| All musculoskeletal | 36.6 (1.1) | 1167.8 (153.9) |
| Sense organs | ||
| Hearing impairment | 3.8 (0.3) | 188.8 (56.2) |
| Vision impairment | 3.2 (0.3) | 144.0 (48.8) |
| All sense organs | 6.3 (0.4) | 393.2 (126.6) |
| All physical | 42.9 (1.1) | 2378.3 (172.2) |
| Mental conditions | ||
| Anxiety disorders | ||
| Agoraphobia | 0.8 (0.1) | 37.1 (8.7) |
| Generalized anxiety disorder | 3.1 (0.2) | 109.5 (13.8) |
| Panic disorder | 2.8 (0.2) | 101.2 (16.0) |
| Posttraumatic stress disorder | 3.5 (0.3) | 112.5 (22.9) |
| Separation anxiety disorder | 0.6 (0.1) | 19.5 (6.5) |
| Social phobia | 6.9 (0.3) | 213.8 (28.7) |
| Specific phobia | 8.8 (0.4) | 253.3 (37.8) |
| All anxiety | 18.0 (0.7) | 706.6 (119.9) |
| Mood disorders | ||
| Major depressive disorder | 6.7 (0.3) | 386.6 (58.0) |
| Bipolar I (mania) | 2.1 (0.2) | 103.1 (32.5) |
| All mood | 8.8 (0.4) | 489.7 (71.5) |
| Substance dependence | ||
| Alcohol dependence | 1.3 (0.2) | 69.9 (24.3) |
| Drug dependence | 0.4 (0.1) | 13.1 (4.9) |
| All substance | 1.6 (0.2) | 96.0 (33.0) |
| All mental or substance | 22.3 (0.7) | 1292.2 (154.2) |
| Any disorder | 53.4 (1.0) | 3588.0 (193.0) |
| Total sample | 5692 |
Prevalence estimates focus on disorders with significant coefficients in the simulated net effects model.
All coefficients are significant at the .05 level, using 2-sided tests.
Estimates are controlled for age, sex, race/ethnicity, education, and the cross-classification of marital status, employment status, and the number and ages of children.
The estimated combined coefficient for all mental conditions (1292.2 million days) is equal to roughly half (54.3%) the estimated combined coefficient for all physical conditions (2378.3 million days). The estimated combined coefficient for all physical and mental conditions (3588 million days) equals 49% of the estimated total days of role disability in the population (7247 million days), the remainder presumably due to unmeasured mental conditions, acute physical conditions, or unmeasured chronic physical conditions.
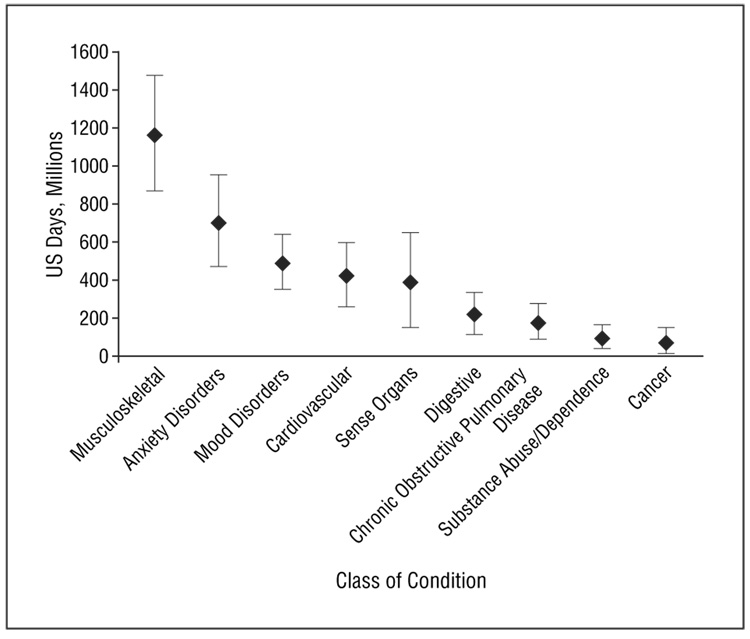
We also carried out simulations of the combined effects of classes of conditions. The mean (2 SEs) of the resulting population-level estimates for classes of conditions were then graphed and ranked in descending order for ease of interpretation (Figure 2). The estimated coefficient associated with all conditions in a class was more than the sum of the condition-specific coefficients in 3 classes (digestive, sense organs, substance abuse/dependence), less than the sum in 2 classes (musculoskeletal, anxiety disorders), and roughly equal to the sum in 2 classes (cardiovascular, mood disorders). This variation shows that the estimated effects of the individual components are net of all comorbid conditions, including within-class comorbidities, whereas the effect of the entire class includes within-class comorbidity. Depending on whether the comorbid cases have more, less, or the same number of disability days as one would expect based on an additive model, the overall net effect of the class will be higher, lower, or the same as the sum of the individual component effects. The class with by far the highest estimated combined coefficient is musculoskeletal (1167.8 million days), followed by anxiety disorders (706.6 million days), mood disorders (489.7 million days), and cardiovascular (424.8 million days).
Figure 2.
Mean (2 SEs) days of role disability at the population level attributable to each class of physical and mental condition.
COMMENT
The major contribution of this article is the application of a novel approach to the estimation of the effects of individual conditions in the presence of comorbidity. The total number of disability days associated with the conditions considered herein is staggering. Over a 1-year period, each of the 53.4% of US adults with 1 or more of these conditions is estimated to average more than 1 full month (32.1 days) of health-related role disability, equivalent to nearly 3.6 billion days out of role in the population. Such large effects demand consideration in determining priorities in health care treatment and research.
Although several previous studies have incorporated the effects of comorbidity into estimates of the effects of specific conditions on a range of indirect outcomes (eg, days out of role, quality of life, various scales of role functioning),8,13,15,16,36 to our knowledge no prior study of a population-based sample has provided estimates of condition-specific disability for a range of physical and mental disorders, controlling for associations within and between classes of comorbid disorders. Our finding that the estimated condition-specific effects of virtually all conditions decreased after accounting for comorbidity suggests that prior studies have overestimated disease-specific effects on disability. However, there is a wide range of differences in the effects of comorbidity for the conditions that we studied. For instance, whereas the estimated effects of cancer and chronic obstructive pulmonary disease only decreased by 16%, the estimated effect of arthritis decreased by 69% in the models that incorporated comorbidity.
Musculoskeletal conditions and depression had the largest estimated effects on disability of all the conditions considered herein at both the individual and population levels. In light of the variability in methods of prior studies, it is striking that previous studies have also ranked musculoskeletal disorders and major depression as the conditions associated with the largest number of disability days at both the individual26,37 and population levels.15,38 Our results suggest that these conditions should be prioritized in the allocation of health care resources. A vivid illustration of the mismatch between health care resources and disease impact is provided by Druss et al,39 who found that musculoskeletal disorders and depression have the lowest health care expenditures relative to disability of any commonly occurring conditions in the United States.
Discrepancies between population-level and individual-level estimated effects of specific conditions are primarily attributable to variations in population prevalence estimates. For example, although arthritis is estimated to have a low individual-level effect on role disability, it has the third largest estimated effect at the population level because of its high prevalence. In contrast, low-prevalence, high-impact conditions, such as cancer, have low estimated population-level effects. Finally, a number of conditions known to have major public health effects, such as diabetes and hypertension, were not included in the final models because our simulation evaluated the incremental effects of specific conditions net of the effects of other conditions and found these incremental effects to be statistically insignificant. This is presumably because the effects of diabetes and hypertension are realized largely through progression to other conditions included in our analyses (eg, cardiovascular disorder, visual impairment).
Our results confirm those of several other studies in suggesting that the individual-level effects of mental conditions are as large as those of most chronic physical conditions.13,14,36,40 We found that the number of disability days associated with all mental conditions at the population level equals more than half (54%) the number of days associated with all the physical conditions considered herein at the population level. This demonstrates the enormous significance of mental conditions to overall illness-related disability. The substantial impact of mental disorders can be attributed to their high prevalence, substantial comorbidity with physical conditions, comparatively early age at onset, and broad influence on functional impairment.
Evidence of the relative effects of different chronic conditions on role disability may be of particular interest to employers,41–43 who have been at the forefront of efforts to develop targeted health care interventions to decrease workplace disability associated with chronic conditions.44–46 Evidence is mounting that such programs can have positive return on investment when effective treatments are available.47,48 Replication of our study among employed people could help to fill the gap in empirical data to guide resource allocation decisions for health-related research. Current data on health care costs that are based primarily on prevalence, mortality, and direct health care costs of chronic diseases are only beginning to include the substantial magnitude of indirect costs due to disability, absenteeism, and lower work productivity.9 The National Institutes of Health has recently established a program to evaluate the entire agency research portfolio to ensure that their research addresses urgent public health needs.49 Evidence on the comparative human and financial costs of chronic conditions should have a central role in this new evidence-based system of research priority setting.
Our findings should be considered in the context of 4 broad classes of limitations. The first class concerns measurement errors. Although CIDI diagnoses of DSM-IV mental disorders have good concordance with independent clinical evaluations, 50,51 the checklist used to assess physical conditions was more superficial, possibly leading to underestimation of the prevalence or associations with disability of physical relative to mental conditions. However, the prevalence estimates obtained herein are similar to those in previous epidemiologic studies of physical conditions.25 The inclusion of acute conditions may have led to a greater increase in the estimated importance of physical relative to mental conditions because the most common acute conditions are physical (seasonal allergies, cold/flu, and strains/sprains).
Measurement errors also have to be considered in the outcome measure, days of role disability. Although this is the most widely used indicator of disability in the literature, recent research shows that reduced role performance on days in role also has an important effect on role disability.9,52,53 The relative effects of the conditions considered herein on reduced quantity or quality of role performance might be different from their effects on days out of role. Reports about days of role disability might also be biased by a combination of recall failure, which leads to underestimation, and “telescoping,” the tendency to recall events as occurring more recently than they actually occurred, 54 which leads to overestimation. Although previous research has shown that reports of work-loss days based on the disability questions used herein are unbiased in comparison with payroll records,21 no comparable objective measures exist to validate reports about disability on nonwork days or among people who are not employed.
The second limitation is that the different periods of measurement of disorders (12-month recall) and disability (30-day recall) could have introduced bias into the results even though our correction method leads to unbiased estimates if the profile of disability days in the 30 days before interview is typical of the profile across all months of the past year. Evidence that these profiles might not be entirely typical comes from methodological research showing that some respondents postpone participation in surveys when they have acute flare-ups of chronic conditions.55 As a result, respondents tend to be in somewhat better health during the month of interviews than during other months, causing the number of disability days in the 30 days before interview to be lower than in a typical month and creating somewhat conservative disability prevalence estimates.
The third limitation is that the cross-sectional naturalistic study design is ill suited to making causal interpretations about the associations documented herein between conditions and disability. Unmeasured common causes might influence these associations. In the case of the net coefficients, a related problem is that the incremental effect of each condition was evaluated after controlling for all other conditions even though some of these other conditions might have been consequences of the focal condition. This means that indirect effects of a focal condition on disability mediated by a comorbid condition (eg, an effect of cancer on disability due to cancer causing depression and depression causing disability) are excluded from the simulation. This will generally lead to an underestimation of the true effect of conditions on disability.
The fourth limitation is that we examined aggregate patterns in the total population rather than only among the employed. This means that we estimated the effects of conditions on days out of role rather than on days out of work. The relative effects of different conditions on days out of work among employed people might differ from the results reported herein, both because of differences in relative prevalence (ie, because some conditions are more important than others in influencing whether a person is employed) and because of differential effects on missing days of work and on missing days of other role activities (eg, days out of role on weekends among employed people and days out of role among homemakers or retired people).
Acknowledgments
Funding/Support: The NCS-R is supported by NIMH grant U01-MH60220 with supplemental support from the National Institute on Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration, Robert Wood Johnson Foundation grant 044780, and the John W. Alden Trust. Activities of the collaborating NCS-R investigators were supported by NIMH grant R01 MH070884; the John D. and Catherine T. MacArthur Foundation; the Pfizer Foundation, US Public Health Service grants R13-MH066849, R01-MH069864, and R01 DA016558; Fogarty International Center grant FIRCA R01-TW006481; the Pan American Health Organization; Eli Lilly and Co; Ortho-McNeil Pharmaceutical, Inc; GlaxoSmithKline; and Bristol-Myers Squibb.
Disclaimer: The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations or agencies or the US government.
Additional Information: Collaborating NCS-R investigators include Ronald C. Kessler (principal investigator, Harvard Medical School), Kathleen Merikangas (co–principal investigator, NIMH), James Anthony (Michigan State University), William Eaton (The Johns Hopkins University), Meyer Glantz (NIDA), Doreen Koretz (Harvard University), Jane McLeod (Indiana University), Mark Olfson (New York State Psychiatric Institute, College of Physicians and Surgeons of Columbia University), Harold Pincus (University of Pittsburgh), Greg Simon (Group Health Cooperative), Michael Von Korff (Group Health Cooperative), Philip Wang (NIMH), Kenneth Wells (University of California, Los Angeles), Elaine Wethington (Cornell University), and Hans-Ulrich Wittchen (Max Planck Institute of Psychiatry, Technical University of Dresden). A complete list of World Mental Health (WMH) publications can be found at http://www.hcp.med.harvard.edu/wmh/. A complete list of NCS publications and the full text of all NCS-R instruments can be found at http://www.hcp.med.harvard.edu/ncs. Send correspondence to ncs@hcp.med.harvard.edu. The NCS-R is carried out in conjunction with the World Health Organization WMH Survey Initiative.
Additional Contributions: The staff of the WMH Data Collection and Data Analysis Coordination Centres assisted with instrumentation, fieldwork, and consultation on data analysis.
Footnotes
Financial Disclosure: Dr Stang has been a consultant for AstraZeneca, Bristol-Meyers Squibb, GlaxoSmithKline, Centocor, Johnson & Johnson, Sepracor, Takeda, and Schering-Plough; has had research support for epidemiologic studies from AstraZeneca, Aventis, Bristol-Myers Squibb, GlaxoSmithKline, Pfizer, Sanofi-Aventis, Wyeth, Eli Lilly and Co, Ortho-McNeil, and the Pfizer Foundation. Dr Von Korff has had research support from Novartis. Dr Kessler has been a consultant for AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Co, GlaxoSmithKline, Pfizer, Sanofi-Aventis, and Wyeth and has had research support for his epidemiologic studies from Bristol-Myers Squibb, Eli Lilly and Co, Ortho-McNeil, Pfizer, and the Pfizer Foundation.
REFERENCES
- 1.Heffler S, Smith S, Won G, Clemens MK, Keehan S, Zezza M. Health spending projections for 2001–2011: the latest outlook. Health Aff (Millwood) 2002;21(2):207–218. doi: 10.1377/hlthaff.21.2.207. [DOI] [PubMed] [Google Scholar]
- 2.Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures: results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA. 1994;272(22):1741–1748. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- 3.Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JB, deGruy FV, III, Brody D, Davies M. Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 Study. JAMA. 1995;274(19):1511–1517. [PubMed] [Google Scholar]
- 4.Kessler RC, Greenberg PE, Mickelson KD, Meneades LM, Wang PS. The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med. 2001;43(3):218–225. doi: 10.1097/00043764-200103000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med. 2003;45(12):1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- 6.Druss BG, Marcus SC, Olfson M, Tanielian T, Elinson L, Pincus HA. Comparing the national economic burden of five chronic conditions. Health Aff (Millwood) 2001;20(6):233–241. doi: 10.1377/hlthaff.20.6.233. [DOI] [PubMed] [Google Scholar]
- 7.Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large US employers in 1999. J Occup Environ Med. 2003;45(1):5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hoffman C, Rice D, Sung HY. Persons with chronic conditions: their prevalence and costs. JAMA. 1996;276(18):1473–1479. [PubMed] [Google Scholar]
- 9.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. J Occup Environ Med. 2004;46(4):398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 10.Lerner D, Allaire SH, Reisine ST. Work disability resulting from chronic health conditions. J Occup Environ Med. 2005;47(3):253–264. doi: 10.1097/01.jom.0000150206.04540.e7. [DOI] [PubMed] [Google Scholar]
- 11.Verbrugge LM, Patrick DL. Seven chronic conditions: their impact on US adults’ activity levels and use of medical services. Am J Public Health. 1995;85(2):173–182. doi: 10.2105/ajph.85.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alonso J, Ferrer M, Gandek B, Ware JE, Jr, Aaronson NK, Mosconi P, Rasmussen NK, Bullinger M, Fukuhara S, Kaasa S, Leplege A. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13(2):283–298. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 13.Buist-Bouwman MA, de Graaf R, Vollebergh WA, Ormel J. Comorbidity of physical and mental disorders and the effect on work-loss days. Acta Psychiatr Scand. 2005;111(6):436–443. doi: 10.1111/j.1600-0447.2005.00513.x. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Ormel J, Demler O, Stang PE. Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the National Comorbidity Survey. J Occup Environ Med. 2003;45(12):1257–1266. doi: 10.1097/01.jom.0000100000.70011.bb. [DOI] [PubMed] [Google Scholar]
- 15.Manuel DG, Schultz SE, Kopec JA. Measuring the health burden of chronic disease and injury using health adjusted life expectancy and the Health Utilities Index. J Epidemiol Community Health. 2002;56(11):843–850. doi: 10.1136/jech.56.11.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rijken M, van Kerkhof M, Dekker J, Schellevis FG. Comorbidity of chronic diseases: effects of disease pairs on physical and mental functioning. Qual Life Res. 2005;14(1):45–55. doi: 10.1007/s11136-004-0616-2. [DOI] [PubMed] [Google Scholar]
- 17.Yu W, Ravelo A, Wagner TH, Phibbs CS, Bhandari A, Chen S, Barnett PG. Prevalence and costs of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(3) suppl:146S–167S. doi: 10.1177/1077558703257000. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13(2):69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13(2):60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003;56(6):507–514. doi: 10.1016/s0895-4356(03)00051-9. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, Pronk N, Simon G, Stang P, Ustun TB, Wang P. The World Health Organization Health and Work Performance Questionnaire (HPQ) J Occup Environ Med. 2003;45(2):156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- 22.Revicki DA, Irwin D, Reblando J, Simon GE. The accuracy of self-reported disability days. Med Care. 1994;32(4):401–404. doi: 10.1097/00005650-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, Stang PE, Ustun TB. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med. 2004;46(6) suppl:S23–S37. doi: 10.1097/01.jom.0000126683.75201.c5. [DOI] [PubMed] [Google Scholar]
- 24.Center for Disease Control and Prevention. Health, United States, 2004. Washington, DC: US Government Printing Offfice; 2004. [Google Scholar]
- 25.Schoenborn CA, Adams PF, Schiller JS. Summary health statistics for the US population: National Health Interview Survey, 2000. Vital Health Stat 10. 2003;(214):1–83. [PubMed] [Google Scholar]
- 26.Knight M, Stewart-Brown S, Fletcher L. Estimating health needs: the impact of a checklist of conditions and quality of life measurement on health information derived from community surveys. J Public Health Med. 2001;23(3):179–186. doi: 10.1093/pubmed/23.3.179. [DOI] [PubMed] [Google Scholar]
- 27.Baker MM, Stabile M, Deri C. What Do Self-reported, Objective Measures of Health Measure? Cambridge, MA: National Bureau of Economic Research; 2001. [Google Scholar]
- 28.Edwards WS, Winn DM, Kurlantzick V, Sheridan S, Berke ML, Retchin S, Collins JG. Evaluation of National Health Interview Survey Diagnostic Reporting. Vital Health Stat 2. 1994;(120):1–116. [PubMed] [Google Scholar]
- 29.Revicki DA, Rentz AM, Dubois D, Kahrilas P, Stanghellini V, Talley NJ, Tack J. Gastroparesis Cardinal Symptom Index (GCSI): development and validation of a patient reported assessment of severity of gastroparesis symptoms. Qual Life Res. 2004;13(4):833–844. doi: 10.1023/B:QURE.0000021689.86296.e4. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 32.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 33.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication [published correction appears in Arch Gen Psychiatry. 2005;62(7):709] Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kish L, Frankel MR. Inferences from complex samples. J R Stat Soc Ser A. 1974;36:1–37. [Google Scholar]
- 35.SAS Institute Inc. SAS/STAT Software: Changes and Enhancements, Release 8.2. Cary, NC: SAS Publishing; 2001. [Google Scholar]
- 36.Stewart-Brown S, Layte R. Emotional health problems are the most important cause of disability in adults of working age: a study in the four counties of the old Oxford region. J Epidemiol Community Health. 1997;51(6):672–675. doi: 10.1136/jech.51.6.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang PS, Beck A, Berglund P, Leutzinger JA, Pronk N, Richling D, Schenk TW, Simon G, Stang P, Ustun TB, Kessler RC. Chronic medical conditions and work performance in the health and work performance questionnaire calibration surveys. J Occup Environ Med. 2003;45(12):1303–1311. doi: 10.1097/01.jom.0000100200.90573.df. [DOI] [PubMed] [Google Scholar]
- 38.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 39.Druss BG, Marcus SC, Olfson M, Pincus HA. The most expensive medical conditions in America. Health Aff (Millwood) 2002;21(4):105–111. doi: 10.1377/hlthaff.21.4.105. [DOI] [PubMed] [Google Scholar]
- 40.Wells KB, Golding JM, Burnam MA. Psychiatric disorder in a sample of the general population with and without chronic medical conditions. Am J Psychiatry. 1988;145(8):976–981. doi: 10.1176/ajp.145.8.976. [DOI] [PubMed] [Google Scholar]
- 41.Fronstin P, Werntz R. The “business case” for investing in employee health: a review of the literature and employer self-assessments. EBRI Issue Brief. 2004;(267):1–27. [PubMed] [Google Scholar]
- 42.Goetzel RZ. Better outcomes through health and productivity management. Manag Care. 2005;14(10) suppl:28–36. discussion 36–27. [PubMed] [Google Scholar]
- 43.Kessler RC, Stang PE, editors. Health and Work Productivity: Making the Business Case for Quality Health Care. Chicago, IL: University of Chicago Press; 2006. [Google Scholar]
- 44.Hymel P, Loeppke R, Baase C, Berger M, Burton W, Lynch W, Parry T, Richling D, Stave G, Konicki D. Establishing a research agenda in health and productivity. J Occup Environ Med. 2004;46(6):518–520. doi: 10.1097/01.jom.0000128762.53513.cc. [DOI] [PubMed] [Google Scholar]
- 45.Pelletier KR. A review and analysis of the clinical- and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: 1998–2000 update. Am J Health Promot. 2001;16(2):107–116. doi: 10.4278/0890-1171-16.2.107. [DOI] [PubMed] [Google Scholar]
- 46.Riedel JE, Lynch W, Baase C, Hymel P, Peterson KW. The effect of disease prevention and health promotion on workplace productivity: a literature review. Am J Health Promot. 2001;15(3):167–191. doi: 10.4278/0890-1171-15.3.167. [DOI] [PubMed] [Google Scholar]
- 47.Rost K, Smith JL, Dickinson M. The effect of improving primary care depression management on employee absenteeism and productivity: a randomized trial. Med Care. 2004;42(12):1202–1210. doi: 10.1097/00005650-200412000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang PS, Simon G, Kessler RC. The economic burden of depression and the cost-effectiveness of treatment. Int J Methods Psychiatr Res. 2003;12(1):22–33. doi: 10.1002/mpr.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zerhouni EA. Setting the path for reauthorization: improving portfolio management at NIH. www.hhs.gov/asl/testify/t050422a.html. Published March 17, 2005.
- 50.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut Saiz G, Sampson NS, Kessler RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. Int J Methods Psychiatr Res. 2006;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, Wang P, Zaslavsky A, Zheng H. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13(2):122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koopman C, Pelletier KR, Murray JF, Sharda CE, Berger ML, Turpin RS, Hackleman P, Gibson P, Holmes DM, Bendel T. Stanford presenteeism scale: health status and employee productivity. J Occup Environ Med. 2002;44(1):14–20. doi: 10.1097/00043764-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 53.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289(23):3135–3144. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 54.Gaskell GD, Wright DB, O’Muircheartaigh CA. Telescoping of landmark events: implications for survey research. Public Opin Q. 2000;64(1):77–89. doi: 10.1086/316761. [DOI] [PubMed] [Google Scholar]
- 55.Wang PS, Beck AL, Berglund P, McKenas DK, Pronk NP, Simon GE, Kessler RC. Effects of major depression on moment-in-time work performance. Am J Psychiatry. 2004;161(10):1885–1891. doi: 10.1176/ajp.161.10.1885. [DOI] [PubMed] [Google Scholar]