Abstract
Aims were to identify the demographic, psychopathology, and psychosocial factors predicting time to major depressive disorder (MDD) recovery and moderators of treatment among 114 depressed adolescents recruited from a juvenile justice center, and randomized to group cognitive-behavioral treatment (CBT) or a life skills/tutoring control condition. Nine variables predicted time to recovery over 1-year follow-up (e.g., earlier MDD onset, ADHD, functional impairment, hopelessness, negative thoughts, low family cohesion, coping skills); suicidal ideation and parental report of problem behaviors were the best predictors. CBT resulted in faster recovery time relative to control treatment specifically among adolescents with White ethnicity, recurrent MDD, and good coping skills. Results suggest that psychopathology plays a more prominent role in maintaining adolescent depression than demographic or psychosocial factors.
Keywords: cognitive-behavioral therapy, adolescents, depression, recovery, moderation
Several psychosocial treatments for adolescents with major depressive disorder (MDD) have been empirically supported (e.g., Curry, 2001), including the Adolescent Coping With Depression course (CWD-A; Clarke, Lewinsohn, & Hops, 1990), a group-based cognitive-behavior therapy (CBT) intervention. Efficacy of the CWD-A course relative to a wait-list control was initially demonstrated in two large randomized trials (Clarke, Rohde, Lewinsohn, Hops, & Seeley, 1999; Lewinsohn, Clarke, Hops, & Andrews, 1990). More recently, Rohde, Clarke, Mace, Jorgensen, & Seeley (2004) extended these findings with a sample of 93 adolescents referred from the juvenile justice system, all of whom met diagnostic criteria for both MDD and conduct disorder (CD). Rates of MDD recovery post-treatment were greater in CWD-A (17/44; 39%) compared to a life skills (LS) attention control condition (9/47; 19%), a finding that was corroborated by greater reductions in self-reported and interviewer-rated depression measures and by improvements in social functioning.
Using data from this latest trial, our aims in the present study were two-fold. First, we investigated predictors of a shorter time to MDD recovery, and second, we examined moderators of the effects of CBT on time to depression recovery. Predictors have a main effect on depression recovery time, independent of treatment, and provide information regarding the mechanisms that contribute to the maintenance of depression. Moderators interact with treatment condition in predicting time to depression recovery, and identify subgroups that benefit more from specific treatment interventions. Both predictors and moderators are assessed prior to treatment and should be independent of treatment assignment.
We conceptualized predictors and moderators as falling into the domains of demographic, psychopathology, and psychosocial factors. Psychopathology factors included both characteristics specific to depression (e.g., MDD onset age, depression severity) and indices of broader psychopathology (e.g., psychiatric comorbidity, functional impairment). Psychosocial factors are variables not directly connected to mental disorder syndromes and included variables that are directly targeted in the CBT intervention (e.g., engagement in pleasant activities, dysfunctional attitudes) and more general resiliency factors (e.g., family cohesion, positive coping).
We modeled time to MDD recovery as the dependent variable rather than the dichotomous outcome of diagnostic recovery because the former captures more detailed information regarding the speed of recovery and represents a more sensitive outcome, as it models both occurrence of the event and time to the occurrence. This methodology also allowed us to analyze data from all adolescents, including participants with incomplete data, which increases statistical power to detect effects.
We next review the available research on predictors of recovery in depressed adolescents, followed by the much more limited research on moderators of treatment effects. Data from both randomized controlled trials and longitudinal community studies are reviewed. Most of these studies predicted depression recovery as a dichotomous phenomenon rather than time to recovery.
Previously examined demographic variables include age, gender, and race/ethnicity. Younger age predicted greater recovery rates in treated children and adolescents with depression (Clarke et al., 1992; Jayson, Wood, Kroll, Fraser, & Harrington, 1998), potentially because depression is less deeply entrenched in childhood than in later adolescence and therefore more easily remits. Thus, we hypothesized that younger age would predict shorter time to MDD recovery. Neither gender nor ethnicity has consistently predicted depression recovery (Brent et al., 1998; Clarke et al., 1992; Jayson et al., 1998; Kovacs, 2001) but were examined in the present study given that the sample was unique in terms of recruitment source and degree of psychiatric comorbidity.
We hypothesized that measures of greater depression-specific psychopathology, including earlier MDD onset age, recurrence, severity, and suicidal ideation, are indices of a more pernicious form of the disorder and thus would predict longer time to MDD recovery. Treatment trials have found that greater depression severity and chronicity in adolescents are associated with lower recovery rates (Birmaher et al., 2000; Brent et al., 1998; Clarke et al., 1992; King, Hovey, Brand, & Ghaziuddin, 1997; Lewinsohn, Clarke, Rohde, Hops, & Seeley, 1996), although it appears that the predictive effects of suicidal ideation have not been examined previously. Among depressed adolescents in epidemiological samples, earlier age of MDD onset, MDD recurrent, suicidal ideation, and depression severity were associated with a longer duration of MDD episodes (Birmaher et al., 2004; Lewinsohn, Clarke, Seeley, & Rohde, 1994).
The broader psychopathology indicators of psychiatric comorbidity and functional impairment were also hypothesized to predict longer time to MDD recovery. Comorbidity exacerbates problems in functioning (e.g., Lewinsohn, Rohde, & Seeley, 1995), increases distress, and complicates the conceptualization and provision of treatment. Treatment trials have found that lifetime presence of substance use disorders predicted slower time to depression recovery (Rohde, Clarke, Lewinsohn, Seeley, & Kaufman, 2001), and higher state anxiety levels predicted lower depression recovery rates (Clarke et al., 1992). To our knowledge, prior trials have not examined the predictive effects of ADHD. Greater functional impairment also has been associated with longer depression episode duration in both patient (Jayson et al., 1998) and epidemiological adolescent samples (Kaminski & Garber, 2002).
Regarding psychosocial factors, we examined variables directly targeted in the CBT intervention, as well as variables that act as resiliency factors for depressed youth. Four CBT-specific variables were examined: negative automatic thoughts, dysfunctional attitudes, hopelessness, and engagement in pleasant activities. While these factors are closely associated with MDD, they were categorized as psychosocial measures because they refer more to psychological and social aspects of depression than to characteristics of the MDD syndrome or other psychiatric disorders. Because depressotypic cognitions and low rates of behavioral activation have been hypothesized to be key maintenance factors for MDD (Beck, 1967; Lewinsohn et al., 1996), we predicted that they would be inversely related to MDD recovery time. Lower rates of depressogenic cognitions and higher engagement in pleasant activities at intake predicted higher MDD recovery rates in treatment trials with depressed adolescents (Brent et al., 1998; Clarke et al., 1992; Lewinsohn et al., 1996). In addition, hopelessness has predicted depression post-treatment (Brent et al., 1998).
Resiliency factors refer to intrapersonal and interpersonal assets that allow the person to cope with negative life challenges and thus were hypothesized to predict a shorter time to MDD recovery. Three variables were examined as resiliency psychosocial factors: positive social adjustment, family cohesion, and good coping skills. Lower parent-adolescent conflict and parental criticism have predicted MDD recovery in clinical trials (Asarnow, Goldstein, Tompson, & Guthrie, 1993; Birmaher et al., 2000; McCleary & Sanford, 2002), however, to our knowledge, previous studies have not examined the predictive effects of social adjustment and coping skills.
Our second aim was to examine variables that interacted with treatment condition to predict shorter time to depression recovery. Moderation analyses identify subgroups that are particularly likely to benefit from CBT versus those who may be unresponsive to the intervention and for whom alternative interventions are indicated. Data on treatment moderation informs intervention theory, promotes the development of more effective interventions incorporating a greater focus on the factors implicated by these analyses, and may facilitate matching clients to the most appropriate interventions. Although increasingly viewed as important (e.g., Kazdin, 1995), to our knowledge, the question of treatment moderation with depressed adolescents has been examined in only one previous clinical trial (Barbe, Bridge, Birmaher, Kolko, & Brent, 2004; Brent et al., 1998).
Demographic factors hold intuitive appeal as potential moderator variables because they would provide an easy method of matching depressed clients to the more appropriate treatments. However, to our knowledge, no demographic factors have been found to moderate the effects of adolescent depression treatment.
With regard to psychopathology factors, we hypothesized that greater pathology would be associated with a more protracted course, which would increase the probability that treatment effects are detected. Thus, we predicted that CBT would be superior to control treatment for depressed adolescents with more severe depression or greater associated psychopathology. Barbe et al. (2004) found that suicidal depressed adolescents responded better to CBT versus nondirective supportive therapy relative to their non-suicidal counterparts. This trial also indicated that depressed adolescents with comorbid anxiety disorders responded significantly better to CBT versus family therapy or supportive therapy compared to their counterparts without anxiety disorders (Brent et al., 1998). However, the present study is the first to test whether the psychopathology factors examined here moderated the effects of group CBT treatment for depressed adolescents.
Regarding the manner in which psychosocial factors would moderate treatment response, one might theorize that CBT would be more effective for clients with the greatest initial deficits (e.g., most depressogenic thinking, least behavioral activation). This assumption has been referred to as the “compensation” model of treatment response (Rude & Rehm, 1991). However, Rude and Rehm also proposed an alternative model, entitled “capitalization,” which posits that clients may be most responsive to treatments that build on their initial strengths. Our literature review suggests that the present study may be the first to test the capitalization versus compensation distinction with regard to potential moderators of CBT treatment for depression. Because lower depressogenic cognitions and higher behavioral activation predicted greater recovery among depressed adolescents in CBT (Clarke et al., 1992; Lewinsohn et al., 1996), we hypothesized that CBT-specific variables would function under a capitalization model: depressed adolescents entering treatment with more cognitive and behavioral resources will experience greater benefit to CBT relative to comparable adolescents assigned to the control condition, whereas clients with deficits in these domains may find it more difficult to benefit from an intervention that directly focuses on these variables. Similarly, we hypothesized that resiliency factors would moderate treatment according to the capitalization model, resulting in greater efficacy for CBT. To our knowledge, only one resiliency factor has been found to moderate treatment response: Brent et al. (1998) found that CBT was more effective than alternative treatments given no maternal depression but was comparable to other treatments given high maternal depressive symptoms.
Method
Participants and Procedures
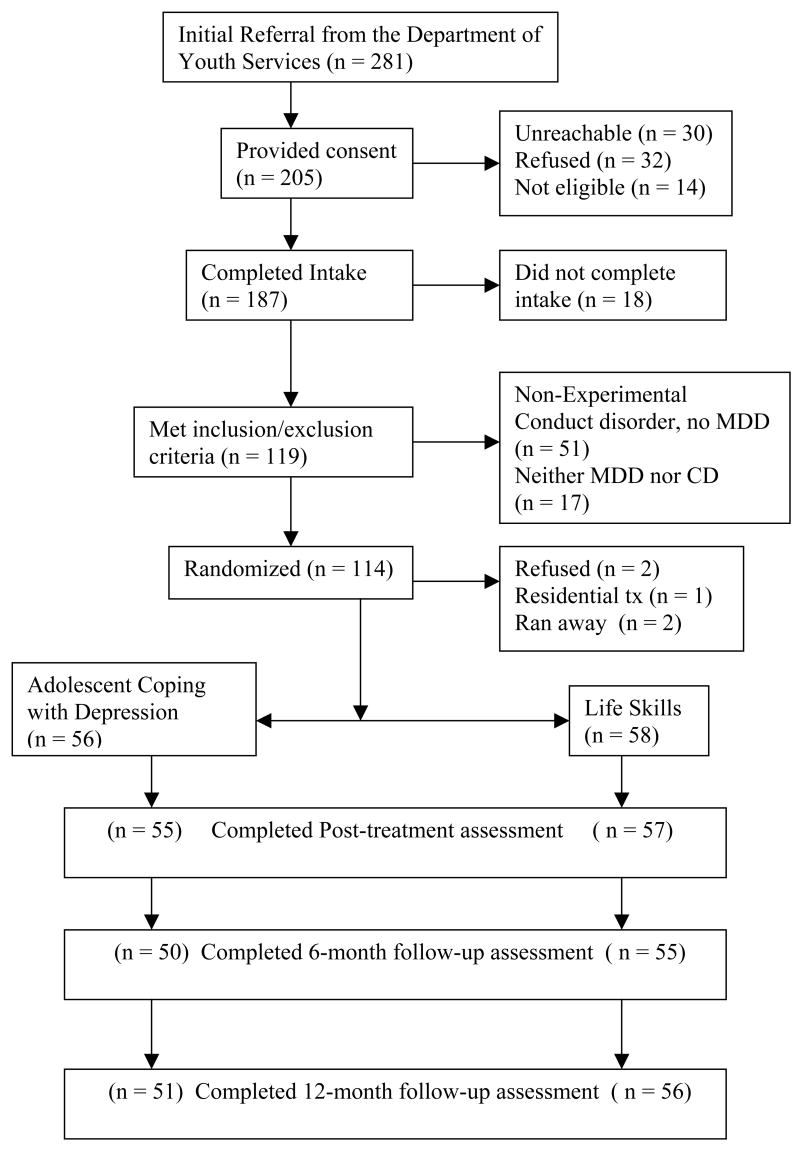
Between 1998 and 2001, 281 adolescents ages 13–17 were referred to the study by staff of the Department of Youth Services of Lane County, Oregon. Research staff obtained consent from 205 adolescents and their legal guardians (see Figure 1 for details regarding those who did not provide consents). Inclusion criteria were: (a) 13 to 17 years of age, (b) current MDD, (c) expected residence in Lane County for the next 12 months, and (d) minimum English fluency. Exclusion criteria were: (a) charges of first degree assault, robbery, homicide, or rape; and (b) psychotic symptoms. A total of 187 completed the intake assessments, of which 119 met the diagnostic inclusion criteria (see Figure 1 regarding participants not meeting inclusion criteria). We did not require concurrent CD for inclusion in the present analyses, which increased our sample size from the 93 reported in Rohde et al. (2004). Two adolescents dropped out of the study prior to randomization, one was placed in residential treatment, and two ran away. Thus, the sample consisted of 114 adolescents who were randomly assigned to the CWD-A course (n = 56) or the LS control condition (n = 58). Participants and parents (or knowledgeable adult) repeated the assessment protocols immediately post-treatment and at 6 and 12 months post-treatment (Figure 1 reports the participation rates for each of the follow-up assessments). All procedures were approved by the research center IRB. No study-related adverse events were reported and the study conformed to CONSORT (Consolidated Standards of Reporting Trials) reporting standards.
Figure 1.
Flow of participants through each stage of the study
The sample had a mean age of 15.2 years (SD = 1.4) and was 48% female. The sample included White (71%), African Americans (1%), Hispanics (1%), Asian Americans (1%), Native Americans (1%) individuals, and participants endorsing “other” or mixed ethnicity (25%). Fifteen percent of adolescents lived with both biological parents, 21% lived with a biological parent and stepparent, 23% living with biological mother only, and the remainder lived with other relatives or in other arrangements.
Assessment Procedures
Adolescents and parent/adult informants were assessed for past and current psychiatric disorders at intake using the Schedule for Affective Disorder and Schizophrenia for School Age Children-Epidemiologic Version 5 (K-SADS; Orvaschel, 1994), a semi-structured interview designed to assess DSM-IV (American Psychiatric Association, 1994) psychopathology. Interviews at post-treatment and 6-, and 12-month follow-up consisted of the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al., 1987) along with the K-SADS. The KSADS/LIFE interview provides detailed information about the course of DSM-IV disorders by providing retrospective weekly ratings of symptom levels for diagnoses made during the previous assessment, and for new disorders that have developed in the interim. Following the guidelines proposed by Frank et al. (1991) and consistent with LIFE methodology, MDD recovery was defined as 8 or more weeks of being in the asymptomatic clinical range, which is defined in the K-SADS/LIFE as having 0–2 mild symptoms.
Interviewers completed extensive training, were regularly supervised, and were blind to participants’ treatment. Interviews were audiotaped and 10% were independently re-rated by an experienced interviewer. Inter-rater kappas indicated acceptable agreement: MDD k = .88, attention-deficit/hyperactivity disorder (ADHD) k = .77, substance use disorder k = .83, and anxiety disorder k = .82. Regarding inter-rater reliability of weekly LIFE ratings, we previously obtained a mean k = .81 for weekly ratings of psychiatric symptoms (Lewinsohn et al., 1990).
At the time of each diagnostic assessment, participants and adult informants also completed depression-related questionnaire measures. To be included in the study, a measure had to have evidence of adequate internal consistency, test-retest reliability, and concurrent validity in depressed adolescents.
Demographic Variables
Three demographic factors were examined: (a) sex; (b) age; and (c) race/ethnicity (measured as White, African American, Hispanic, Asian American, Native American, and other/mixed; dichotomized into White vs. non-White for the analyses).
Depression-Specific Psychopathology Factors
Four measures specific to depression were examined: (a) age of first MDD onset, obtained from the intake K-SADS interview; (b) number of prior MDD episodes, obtained from the K-SADS; (c) depression severity, defined as scores on the Beck Depression Inventory-II (Beck, Steer, & Brown, 1996), a 21-item measure of depressive symptomatology during the past week (α = .93); and (d) suicidal ideation (Lewinsohn, Rohde, & Seeley, 1994), defined as the frequency of occurrence of suicidal ideation (e.g., “I thought about killing myself”) during the past week assessed by four 4-point items (α = .85).
Broader Psychopathology Factors
Five measures of broader psychopathology were examined: (a) current ADHD; (b) current substance use disorder (i.e., psychoactive substance abuse or dependence); (c) current anxiety disorder; (d) functional impairment, assessed by interviewer ratings of current functioning using the 100-point Children’s Global Adjustment Scale (CGAS; Shaffer et al., 1983); and (d) parent report of problem behaviors, assessed by total problem behavior scores on the Child Behavior Checklist (CBCL; Achenbach, 1991), a common parent-report measure of adolescent internalizing and externalizing symptoms and functioning (64 items, α = .92).
CBT-Specific Psychosocial Factors
Four psychosocial variables targeted by CBT were examined: (a) negative thoughts, as assessed by the 30-item Automatic Thoughts Questionnaire (ATQ; Hollon & Kendall, 1980), which measures the frequency of occurrence of negative thoughts (e.g., “My life is a mess.”) during the last week on a 5-point scale (α = .98); (b) dysfunctional attitudes, as assessed by a 9-item abbreviation of the Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978), which measures the degree of agreement with attitudes or beliefs sometimes held by depressed individuals (e.g., “I should be able to please everybody.”) on a 5-point scale (α = .80); (c) hopelessness, as assessed by the Beck Hopelessness Scale (Beck, Weissman, Lester, & Trexler, 1974), which contains 20 true/false items (e.g., “I don’t expect to get what I really want”) during the past week (KR-20 = .88); and (d) frequency of pleasant events, as assessed by the frequency of engagement in the past month of 52 events associated with improved mood (e.g., spending time in nature, exercising) from the Pleasant Events Schedule (PES; MacPhillamy & Lewinsohn, 1982) (KR-20 = .92).
Resiliency Psychosocial Factors
Three psychosocial resiliency factors were examined: (a) social adjustment, as assessed by the total adjustment score on the 23-item Social Adjustment Scale Self-Report for Youth (SAS-SR; Weissman, Orvaschel, & Padian, 1980), which measures adjustment in school, friends/spare time, family, and dating during the past two weeks using 5- or 6-point scales (α = .84); (b) family cohesion, as assessed by 9 true/false items (e.g., “Family members really help and support one another”) from the Family Environment Scale (Moos, 1974) (KR-20 = .82); and (c) coping skills (Rohde, Lewinsohn, Tilson, & Seeley, 1990), as assessed by 17 items assessing positive cognitive or behavioral coping and the absence of passive or ineffective coping. Nine items assess what individuals are likely to do when facing a stressful situation (e.g., “stay in bed”) on a 4-point scale, and the remaining eight items assess agreement with statements used to describe people (e.g., “When I am depressed, I try to keep myself busy with things that I like”) on a 4-point scale. Negative items were reverse-scored to form a continuous measure (α = .75)
Treatment Interventions
Efforts were made to equate the two conditions on session number, therapist-participant ratio, and nonspecific therapeutic factors. For both conditions, mixed-gender groups of up to 10 adolescents met for 16 two-hour sessions over 8 weeks. Mean attendance in the CWD-A and LS conditions did not significantly differ (8.4 [SD = 5.7] and 7.6 [SD = 5.7] sessions, respectively).
CWD-A condition
The CWD-A course is a group intervention that combines cognitive and behavioral strategies aimed at ameliorating the problems that affect depressed adolescents. Participants are taught skills for mood monitoring, social skills, behavioral activation, relaxation, cognitive restructuring, communication, conflict resolution, and relapse prevention. The CWD-A was modified slightly for use with this population: two therapists led the group (rather than one), a college/high school student assistant helped monitor in-session behavior and assist with reading problems, and writing assignments were simplified.
LS condition
The life skills/tutoring intervention consisted of current events review, life skills training (e.g., filling out a job application), and tutoring. The intervention was developed to educate participants on basic life skills in a supportive and nonjudgmental manner. We designed the LS condition to match the CWD-A on nonspecific therapeutic factors but provide none of the skills proposed by CBT theory to reduce depression.
Therapist Training and Protocol Adherence
Eight leaders conducted the CWD-A intervention. Therapists had at least a master’s degree in the mental health field and completed a 60-hour training. Four student helpers assisted CWD-A leaders. A certified high school teacher and five additional adult leaders conducted the LS interventions; five student helpers assisted. Detailed manuals for both conditions were developed to ensure protocol adherence, which was good (Rohde et al., 2004).
Statistical Analyses
Using an intent-to-treat analytic approach, the dependent variable was time to MDD recovery. Based on reports at the post-treatment diagnostic assessment, 14 adolescents (12%) across both condition had recovered by one week post-intake. Combining diagnostic data across the three follow-up assessments (i.e., post, 6-, and 12-month follow-up), 49 adolescents (43%) in both conditions had recovered by 12 weeks post-intake, and 88 (77%) had recovered by the end of the one-year follow-up period. Cox proportional hazards models were used for both prediction and moderation models. Time-to-event analyses such as this are a powerful and informative method of identifying clinically important effects that may be obscured in analyses that examine the proportion of individuals who are recovered at a single point in time, such as the end of treatment. In addition, time-to-event analyses allow for the inclusion of participants with incomplete data (e.g., due to study attrition). Thus, statistical power is maximized compared to an end-point recovery analytic approach. The Cox model is a regression method for survival data and provides an estimate of the hazard ratio with a confidence interval. Given that predictors and moderators must occur prior to treatment, these variables were assessed at the intake assessment. For each predictor variable, the proportional hazards assumption was tested by including a time x predictor interaction term in the Cox model as recommended by Singer & Willett (1991). A nonsignificant time × predictor interaction indicated that the proportional hazard assumption was met, in which case the interaction term was removed from the model. If the time × predictor interaction term was significant, the interaction term was retained in the model to account for the non-proportional hazards. Multivariate models were computed using all variables that had a significant univariate association. Separate multivariate models were computed to identify the predictors and moderators that made a unique contribution to MDD recovery time, using a backward elimination model-trimming process suggested by Hosmer and Lemeshow (2000). Alpha was set at p < .05 (two-tailed), which resulted in adequate power (.80) to detect a hazard ratio of 1.96 for main effects. It should be noted that the power to detect higher-order regression terms (i.e., testing moderation) is expected to be lower than the first-order terms (Aiken & West, 1991), due to increased measurement error.
Results
Predictors of Time to Depression Recovery
Univariate models
The main effects models are presented in Table 1. The first column of data contains the test statistic from the Cox proportional hazards model, with its significance level shown in column two. Statistics for three variables (suicidal ideation, hopelessness, coping skills) were based on a non-proportional hazards model due to violation of the proportional hazards assumption. The third column contains the hazard ratio, which summarizes the difference in recovery curves for those with or without the predictor variable. Interpreting hazard ratios for continuous measures are difficult because they indicate differences in recovery risk for an increase of one unit on the continuous measure. To facilitate comparison of the magnitude of effects for dichotomous and continuous measures, hazard ratios for continuous measures were re-calculated after dichotomizing the measure at the median (results are shown in parentheses). The fourth column of Table 1 displays the 95% confidence interval for the original hazard ratio. Based on a conversion of Cohen’s d to an odds ratio (Lipsey & Wilson, 2001), hazard ratios of 1.44, 2.48, and 4.28 represent small, medium, and large effects, respectively. To further illustrate the magnitude of the significant effects, we calculate the median survival times for depression recovery given the presence or absence of the predictor (continuous variables were dichotomized at the median).
Table 1.
Univariate Predictors of Time to MDD Recovery
| Variable | −2 log likelihood χ2 (1, n = 114) test | p-value | Hazard Ratio | 95% Confidence Interval |
|---|---|---|---|---|
| Demographic Factors | ||||
| Female gender | .34 | .559 | 1.14 | .75–1.72 |
| White ethnicity | .64 | .423 | 1.20 | .77–1.89 |
| Age | 2.52 | .112 | 1.13 (1.28) | .97–1.32 |
| Depression-Specific Psychopathology Factors | ||||
| Age of MDD onset | 5.11 | .024 | 1.11 (1.65) | 1.01–1.21 |
| Number of MDD episodes | .92 | .337 | .75 (.75) | .48–1.17 |
| Depression severity (BDI) | 3.13 | .077 | 1.02 (1.35) | 1.00–1.03 |
| Suicidal ideationa | 7.45 | .006 | 1.47 (4.35) | 1.11–1.92 |
| Broader Psychopathology Factors | ||||
| ADHD | 5.84 | .016 | 1.89 | 1.09–3.23 |
| Substance use disorder | .01 | .937 | 1.02 | .63–1.67 |
| Anxiety disorder | .18 | .670 | 1.10 | .71–1.69 |
| Functional impairment | 8.57 | .003 | 1.04 (1.63) | 1.01–1.07 |
| CBCL total problem score | 17.80 | <.001 | 1.03 (2.05) | 1.01–1.04 |
| CBT-Specific Psychosocial Factors | ||||
| Negative thoughts | 5.44 | .020 | 1.01(1.28) | 1.00–1.02 |
| Dysfunctional attitudes | .00 | .953 | 1.00 (1.15) | .97–1.03 |
| Hopelessnessa | 7.81 | .005 | 1.16 (5.56) | 1.04–1.28 |
| Pleasant events frequency | .71 | .400 | 1.00 (.81) | .98–1.01 |
| Resiliency Psychosocial Factors | ||||
| Social adjustment | 2.05 | .152 | .99 (.78) | .98–1.00 |
| Family cohesion | 5.34 | .021 | .92 (.69) | .85–.99 |
| Coping skillsa | 6.34 | .012 | .93 (.25) | .88–.98 |
Note. Hazard ratios are reported for Cox regression models. In parentheses are the hazard ratios for continuous measures re-calculated after dichotomizing the measure at the median. MDD = major depressive disorder; BDI = Beck Depression Inventory; ADHD = attention deficit/hyperactivity disorder; CBCL = Child Behavior Checklist.
Statistics are based on a non-proportional hazards model due to violation of the proportional hazards assumption.
Two depression-specific psychopathology measures were significant predictors of longer time to MDD recovery: earlier onset of MDD and suicidal ideation. The median time to MDD recovery for participants with early MDD onset (< 13.2 years of age) was 27 weeks (95% CI = 6.4–47.6), compared to 14 weeks (95% CI = 7.8–20.2) for participants having a later depression onset. The median MDD recovery time for participants with suicidal ideation (scores ≥ 2) was 25 weeks (95% CI = 14.3–35.7), compared to 12 weeks (95% CI = 6.0–18.0) for participants who did not have current ideation.
Three indices of broader psychopathology also predicted longer MDD recovery time: ADHD, lower psychosocial functioning, and parent-report of problem behaviors. Median MDD recovery time for adolescents with ADHD was 40 weeks (95% CI = 23.9–56.1), compared to 14 weeks (95% CI = 10.3–17.7) for non-ADHD participants. Median MDD recovery time for low functioning adolescents (CGAS < 52) was 33 weeks (95% CI = 15.4 – 50.6), compared to 12 weeks (95% CI = 6.9–17.1) for those with higher psychosocial functioning at intake. The median MDD recovery time given high CBCL total problem behavior scores (> 132.5) was 31 weeks (95% CI = 19.3–42.7) versus 12 weeks (95% CI = 8.8–15.2) among those with lower parent reports of problem behaviors.
Two CBT-specific psychosocial factors significantly predicted time to MDD recovery: higher levels of negative automatic cognitions and hopelessness. The median MDD recovery time was 23 weeks (95% CI = 14.5–31.5) for adolescents reporting high ATQ scores (≥ 55.5) scores, compared to 12 weeks (95% CI = 7.9–16.1) for those reporting low ATQ scores. The median MDD recovery time for adolescents reporting higher hopelessness (which was defined as > 6 on the Beck Hopelessness Scale) was 24 weeks (95% CI = 13.3–34.7), compared to 12 weeks (95% CI = 6.7–17.3) for adolescents reporting low hopelessness.
Two psychosocial resiliency factors were predictive of MDD recovery time: family cohesion and positive coping skills. The median MDD recovery time for adolescents reporting high family cohesion (> 5.0) was 12 weeks (95% CI = 7.5–16.5), compared to 27 weeks (95% CI = 15.8–38.2) for adolescents reporting low family cohesion. The median MDD recovery time for adolescents reporting good coping (> 45.0 on the measure) was 11 weeks (95% CI = 6.1–15.9), compared to 23 weeks (95% CI = 14.4–31.6) for those who reported poor coping. Coping skills also was a significant moderator of treatment effects, as described below.
Multivariate model
Using a backward elimination process (Hosmer & Lemeshow, 2000), a multivariate model was computed to ascertain the unique effects for the nine significant univariate predictors. Two variables made a unique contribution to predicting MDD recovery time: (a) parent-report of total problem behaviors on the CBCL; likelihood χ2 (1, n = 114) = 16.52, p < .001; and (b) suicidal ideation; likelihood χ2 (1, n = 114) = 6.52, p = .011.
Moderators of Treatment Effects
Univariate models
Treatment condition interacted with 3 of the 19 examined factors: (a) race/ethnicity; likelihood χ2 (1, n = 114) = 3.91, p = .048; (b) number of previous MDD episodes; likelihood χ2 (1, n = 114) = 3.95, p = .047; and (c) coping skills; likelihood χ2 (1, n = 114) = 7.99, p = .005. To interpret the differential effectiveness of the treatment interventions, the two continuous moderators were dichotomized at the median.
A simple effect of treatment condition was present for White participants, likelihood χ2 (1, n = 81) = 5.08, p = .024; hazard ratio = 1.76 (95% CI = 1.06–2.92). The median time to MDD recovery for White participants in the CWD-A was 11 weeks (95% CI = 6.4–15.6), compared with 27 weeks for White participants in LS (95% CI = 14.6–39.4). In contrast, no advantage for CBT was detected among non-White adolescents, likelihood χ2 (1, n = 33) = .57, p = .451; hazard ratio = 1.04 (95% CI = .56–1.93), with a median time to MDD recovery of 14 weeks (95% CI = 10.0–30.4) and 12 weeks (95% CI = 9.9–14.1) for non-White adolescents in the CWDA and LS groups, respectively.
A simple effect of treatment condition was present for adolescents with a history of two or more MDD episodes at intake, likelihood χ2 (1, n = 41) = 7.04, p = .008; hazard ratio = 2.67 (95% CI = 1.25–5.72). The median time to MDD recovery for CWD-A participants with recurrent MDD was 6 weeks (95% CI = 3.3 – 8.8) versus 38 weeks (95% CI = 25.9–50.1) for LS participants with recurrent MDD. No treatment condition effect was detected for adolescents experiencing their first MDD at intake, likelihood χ2 (1, n = 73) = .07, p = .797; hazard ratio = .94 (95% CI = .56–1.56), with median MDD recovery times of 13 weeks (95% CI = 5.8–20.2) and 17 weeks (95% CI = 13.2–20.8) for the CWD-A and LS group participants, respectively.
A simple effect of treatment condition was present for participants with high levels of positive coping skills, likelihood χ2 (1, n = 58) = 4.28, p = .039; hazard ratio = 1.79 (95% CI = 1.00–3.19). The median time to MDD recovery for CWD-A participants with good coping skills was 6 weeks (95% CI = .7 – 11.3), compared with 16 weeks for LS participants with good coping skills (95% CI = 7.2 – 24.8). In contrast, no treatment effect was detected among adolescents with poor coping skills, likelihood χ2 (1, n = 56) = .02, p = .892; hazard ratio = 1.04 (95% CI = .56–1.93), with a median time to MDD recovery of 23 weeks (95% CI = 7.8–38.2) and 27 weeks (95% CI = 18.2–35.8) for these adolescents in the CWD-A and LS groups, respectively.
Multivariate model
Using backward elimination, a multivariate model was computed to ascertain the unique effects for the three significant moderators. Two variables moderated the effect of treatment on MDD recovery time: (a) number of previous MDD episodes × condition; likelihood χ2 (1, n = 114) = 4.33, p = .038; and (b) coping skills x condition; likelihood χ2 (1, n = 114) = 4.54, p = .033.
Discussion
The present study identified the pre-treatment predictors and treatment moderators of time to MDD recovery among depressed adolescents who had been referred from a juvenile corrections setting for treatment. We discuss the prediction results first, followed by moderation, highlighting the findings with the most salient research and clinical implications.
Suicidal ideation and associated depression-related cognitions are among the strongest predictors of persistent MDD. The significance of suicidal ideation as one of two unique predictors in the multivariate model highlights its potency as a key marker. Suicidality increases treatment dropout and may impact treatment through increased depression severity and hopelessness (Barbe et al., 2004). Hopelessness in the present study also emerged as a univariate predictor of a more chronic depression, replicating the finding of Brent et al. (1998). Suicidal ideation and hopeless may impede the adolescent’s willingness to engage in treatment and ability to benefit from treatment, especially interventions that are psychosocial in nature. An alternative explanation is that these measures are markers of greater depression severity, which accounts for the protracted duration.
A third cognitive measure – the frequency of negative thoughts – also predicted longer MDD episodes. Cognitive theories of depression (e.g., Beck, 1967) posit that negative cognitions contribute to both the incidence and maintenance of depression, and higher pre-treatment levels of depressotypic thoughts have predicted lower response rates in both depressed adolescent (Brent et al., 1998; Clarke et al., 1992) and adult (Sotsky et al., 1991) treatment trials. The significant predictive role of suicidal ideation, hopelessness, and negative thoughts points to the importance of cognitive interventions specifically aimed at enhancing optimism, increasing motivation, and reducing automatic maladaptive thoughts and negative ruminations.
A second key predictor category of longer MDD duration consisted of broad psychopathology and functional impairment. These factors might maintain depression because they result in negative life events and subsequent demoralization. These factors might also reflect higher levels of other, unmeasured variables (genetic, environmental, social) that contribute to greater psychopathology in general. Parental report of total problem behaviors was highly predictive of a longer time to MDD recovery and showed a unique predictive effect. This finding, if replicated, could be due to greater objectivity or insight of parents into the degree of the adolescent’s disturbance. Conversely, parents may be aware of only the most severe disturbances in their children, which play a key role in depression maintenance. A more tentative speculation is that the parent’s negative appraisal of their child is itself contributing to the longer MDD duration (e.g., Joiner, 2000). This finding emphasizes the importance of including parental report in the assessment of depressed adolescents, at least in certain subpopulations. Functional impairment also predicted a longer time to MDD recovery, consistent with previous research with both depressed adolescents (Kaminski & Garber, 2002) and adults (Papakostas et al., 2003). A more fine-grained assessment of the nature of functioning problems, independent of psychopathology, is recommended in future research (Winters, Collett, & Myers, 2005).
Earlier MDD onset predicted longer time to depression recovery. An earlier onset of depression may result in more persistent depression because it develops when the young person has fewer coping skills and resiliency factors. Whether the first MDD occurs before or after puberty may be particularly salient (Wickramaratne & Weissman, 1998). Clinically, the finding emphasizes the importance of active screening and treatment referral efforts.
ADHD was the only narrow-band psychiatric comorbidity that significantly predicted time to MDD recovery. Given the role of functional impairment in maintaining depression, ADHD could be contributing to the maintenance of MDD due to its negative impact on functioning. Regardless of the mechanism of effect, adequately treating ADHD when it cooccurs with MDD seems imperative. The nonsignificant predictive role of other comorbidities was unexpected, given previous research (Brent et al., 1998; Rohde et al., 2001). The inconsistent pattern of findings across studies highlights the fact that detecting the impact of comorbidity on depression will be strongly influenced by the nature of the population studied and the study design.
Two resiliency factors were identified that predicted shorter depressive episodes. High family cohesion may provide a safety net of resources and support on which the depressed young person can rely. Conversely, parent-child conflict, parental criticism, and hostility are known to predict maintenance of the depressive disorder among adolescents (Birmaher et al., 2000; McCleary & Sanford, 2002). While positive copings skills predicted a faster recovery time, it also interacted with treatment condition, as discussed subsequently.
Our second aim was to identify subgroups of depressed adolescents for whom CBT was especially beneficial. To our knowledge, this issue has been examined only once before (Brent et al., 1998). In the present study, three moderators were found. First, compared to the control intervention, the CWD-A course appears to be particularly effective for depressed White adolescents. Conversely, depressed non-White adolescents in the two forms of treatment had statistically similar recovery times, with time to recovery rates approaching those for White adolescents in the CBT intervention. If replicated, this findings suggests that depressed non-White adolescents might benefit equally well from a variety of psychosocial interventions that contain positive, albeit nonspecific, therapeutic factors, whereas depressed adolescents from the majority culture require treatments specifically targeted to address cognitive and behavioral processes directly related to depression. An alternative possibility is that some aspect of the life skills control intervention was iatrogenic for White adolescents. Future research should specifically evaluate CBT relative to other treatments in well-powered, culturally diverse samples of adolescents. The present findings may have been influenced in some unknown manner by the study recruitment process and that this moderation effect was not significant in the multivariate model, which suggests that it could be accounted for by other factors.
Adolescents with recurrent MDD who received CBT treatment recovered significantly faster than those in the life skills control condition. Among adolescents in their first MDD episode, recovery times in the two treatment conditions were indistinguishable. This finding clearly needs to be replicated but suggests that nonspecific psychosocial interventions may be unhelpful for depressed adolescents with recurrent MDD, who presumably require the empirically supported and more targeted CBT intervention. Conversely, adolescents who are experiencing their first MDD episode may benefit from the nonspecific support provided by either form of treatment, perhaps because a subset of them are experiencing fairly transient depressive episodes related to specific life circumstances.
The third moderation effect suggested that CBT works best when it can capitalize on an adolescent’s existing coping skills. Adolescents with good baseline coping skills who were randomized to the CWD-A course recovered faster than those assigned to control treatment. For depressed adolescents with poor coping skills, time to MDD recovery was prolonged and unrelated to treatment type. Depressed youth with positive coping skills appear well-suited for the CWD-A course, which has the overarching goal of enhancing the adolescent’s ability to cope with life challenges. These youth may enter treatment with a pre-existing repertoire of coping skills that is augmented by this form of treatment. Alternatively, the CWD-A course may work by reactivating dormant coping skills, rather than by teaching totally new skills to unskilled youth. Conversely, depressed adolescents with coping skill deficits may be unable to engage in, and benefit from, these fairly demanding forms of treatment, and other treatment approaches, including pharmacotherapy (Treatment of Adolescents with Depression Study Team, 2004), may be more effective.
The psychosocial variable of coping skills functioned according to the capitalization model, in that adolescents entering treatment with a higher skill set were most able to benefit from CBT. Conversely, the psychopathology variable of recurrent MDD functioned according to compensation model, with CBT “compensating” for the presence of recurrent MDD. Our pattern of results is consistent with moderators reported by Brent and colleagues, who found that comorbid anxiety disorder and suicidal ideation (two psychopathology variables) followed the compensation model, whereas maternal depression (a psychosocial factor) functioned according the capitalization model. One difference between psychopathology and psychosocial factors is that psychosocial factors vary on a continuum from protective to impairing, whereas psychopathology factors vary from very impairing to less impairing (e.g., one would not say that having only a single episode of MDD is “protective”).
This study had certain limitations. First, the recruitment of depressed multi-disordered adolescents from juvenile corrections may have compromised the generalizability of our findings in unknown ways. For example, the finding that ADHD plays a more salient role than other comorbidities in predicting time to MDD recovery may be particularly true in sample of depressed adolescents with high rates of conduct disorder. In addition, the sample was predominantly White and we were unable to examine the impact of ethnicity in any greater detail than White versus non-White. Given the intriguing interaction of race/ethnicity with treatment condition, the impact of racial and ethnic differences on treatment effectiveness should be examined further. Second, additional potentially relevant predictors and moderators should be considered in future research, including stress, parental psychopathology, psychobiological functioning, personality style, and pubertal development (e.g., Kaminski & Garber, 2002; Thase, Simons, & Reynolds, 1996). Third, the time to MDD recovery was based on interventions requiring up to 6-months retrospective recalls. Some adolescents may have under-reported the duration of their depressive episode, although rapid reductions in depression symptoms are known to occur early in CBT treatment with adolescents (Renaud et al., 1998). Fourth, we were underpowered to detect small effects.
In conclusion, the present study provides intriguing directions for future research and empirically-based guidance to clinicians. The predictor results suggest salient factors to target in future treatment modifications. Indices of greater psychopathology, and to a lesser extent psychosocial factors, appear to be predominantly responsible for maintaining the young person’s depression. Some predictors (e.g., negative cognitions) are modifiable and treatments should target these factors in greater detail to increase the speed of depression recovery. Other predictors (e.g., early onset of MDD) are not readily modifiable but may inform realistic expectations regarding recovery rates or suggest when adjunctive treatment is indicated. The risk factor of early MDD onset certainly supports depression prevention efforts focused on prepubertal youth. The moderator findings suggest that CBT can be particularly effective with certain groups. Future research should continue to evaluate the predictor and moderator variables that identify depressed adolescent for whom various treatment interventions produce the most rapid effects, as this should facilitate our ability to treat this pernicious mental disorder.
Appendix Materials.
CONSORT Checklist of items to include when reporting a randomized trial
| PAPER SECTION And topic | Item | Description | Reported on Page # |
|---|---|---|---|
| TITLE & ABSTRACT | 1 | How participants were allocated to interventions (e.g., “random allocation”, “randomized”, or “randomly assigned”). | 2 |
| INTRODUCTION Background | 2 | Scientific background and explanation of rationale. | 3–9 |
| METHODS Participants | 3 | Eligibility criteria for participants and the settings and locations where the data were collected. | 9 |
| Interventions | 4 | Precise details of the interventions intended for each group and how and when they were actually administered. | 13–14 |
| Objectives | 5 | Specific objectives and hypotheses. | 3–98 |
| Outcomes | 6 | Clearly defined primary and secondary outcome measures and, when applicable, any methods used to enhance the quality of measurements (e.g., multiple observations, training of assessors). | 10–15 |
| Sample size | 7 | How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules. | 9 |
| Randomization -- Sequence generation | 8 | Method used to generate the random allocation sequence, including details of any restrictions (e.g., blocking, stratification) | 9 |
| Randomization -- Allocation concealment | 9 | Method used to implement the random allocation sequence (e.g., numbered containers or central telephone), clarifying whether the sequence was concealed until interventions were assigned. | 9 |
| Randomization -- Implementation | 10 | Who generated the allocation sequence, who enrolled participants, and who assigned participants to their groups. | 9 |
| Blinding (masking) | 11 | Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to group assignment. When relevant, how the success of blinding was evaluated. | 10 |
| Statistical methods | 12 | Statistical methods used to compare groups for primary outcome(s); Methods for additional analyses, such as subgroup analyses and adjusted analyses. | 14–15 |
| RESULTS Participant flow | 13 | Flow of participants through each stage (a diagram is strongly recommended). Specifically, for each group report the numbers of participants randomly assigned, receiving intended treatment, completing the study protocol, and analyzed for the primary outcome. Describe protocol deviations from study as planned, together with reasons. | 9–10 |
| Recruitment | 14 | Dates defining the periods of recruitment and follow-up. | 9 |
| Baseline data | 15 | Baseline demographic and clinical characteristics of each group. | 10 |
| Numbers analyzed | 16 | Number of participants (denominator) in each group included in each analysis and whether the analysis was by “intention-to-treat”. State the results in absolute numbers when feasible (e.g., 10/20, not 50%). | 9,14–15 |
| Outcomes and estimation | 17 | For each primary and secondary outcome, a summary of results for each group, and the estimated effect size and its precision (e.g., 95% confidence interval). | 15–19, 34–35 |
| Ancillary analyses | 18 | Address multiplicity by reporting any other analyses performed, including subgroup analyses and adjusted analyses, indicating those pre-specified and those exploratory. | n/a |
| Adverse events | 19 | All important adverse events or side effects in each intervention group. | 9 |
| DISCUSSION Interpretation | 20 | Interpretation of the results, taking into account study hypotheses, sources of potential bias or imprecision and the dangers associated with multiplicity of analyses and outcomes. | 19–25 |
| Generalizability | 21 | Generalizability (external validity) of the trial findings. | 19–25 |
| Overall evidence | 22 | General interpretation of the results in the context of current evidence. | 19–25 |
Acknowledgments
This project was funded by research grants MH 56238 (Dr. Rohde) and MH67183 (Dr. Stice) from the National Institute of Mental Health. The authors wish to thank the staff of the Lane County Department of Youth Services, Eugene, OR and the adolescents who participated in this project.
Contributor Information
Paul Rohde, Oregon Research Institute.
John R. Seeley, Oregon Research Institute
Noah K. Kaufman, Mesilla Valley Hospital
Gregory N. Clarke, Kaiser Permanente Center for Health Studies
Eric Stice, Oregon Research Institute.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Asarnow JR, Goldstein MJ, Tompson M, Guthrie D. One-year outcomes of depressive disorders in child psychiatric in-patients: Evaluation of the prognostic power of a brief measure of expressed emotion. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1993;43:129–137. doi: 10.1111/j.1469-7610.1993.tb00975.x. [DOI] [PubMed] [Google Scholar]
- Barbe RP, Bridge J, Birmaher B, Kolko D, Brent DA. Suicidality and its relationship to treatment outcome in depressed adolescents. Suicide and Life-Threatening Behavior. 2004;34:44–55. doi: 10.1521/suli.34.1.44.27768. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Hoeber; 1967. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Kolko D, Baugher M, Bridge J, Holder D, et al. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry. 2000;57:29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Williamson DE, Dahl RE, Axelson DA, Kaufman J, Dorn LD, et al. Clinical presentation and course of depression in youth: Does onset in childhood differ from onset in adolescence? Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:63–70. doi: 10.1097/00004583-200401000-00015. [DOI] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, et al. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hops H, Lewinsohn PM, Andrews JA, Seeley JR, Williams JA. Cognitive-behavioral group treatment of adolescent depression: Prediction of outcome. Behavior Therapy. 1992;23:341–354. [Google Scholar]
- Clarke GN, Lewinsohn PM, Hops H. Adolescent Coping With Depression Course. The therapist manual and the adolescent workbook may be downloaded for free from the Internet. 1990 http://www.kpchr.org/acwd/acwd.html.
- Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: Efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:272–279. doi: 10.1097/00004583-199903000-00014. [DOI] [PubMed] [Google Scholar]
- Curry J. Specific psychotherapies for childhood and adolescent depression. Biological Psychiatry. 2001;49:1091–1100. doi: 10.1016/s0006-3223(01)01130-1. [DOI] [PubMed] [Google Scholar]
- Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrence. Archives of General Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Kendall PC. Cognitive self-statements in depression: Development of an Automatic Thoughts Questionnaire. Cognitive Therapy and Research. 1980;4:383–395. [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. 2. New York: Wiley; 2000. [Google Scholar]
- Jayson D, Wood A, Kroll L, Fraser J, Harrington R. Which depressed patients respond to cognitive-behavioral treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:35–39. doi: 10.1097/00004583-199801000-00014. [DOI] [PubMed] [Google Scholar]
- Joiner TE., Jr Depression’s vicious scree: Self-propagating and erosive processes in depression chronicity. Clinical Psychology: Science and Practice. 2000;7:203–218. [Google Scholar]
- Kaminski KM, Garber J. Depressive spectrum disorders in high-risk adolescents: Episode duration and predictors of time to recovery. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:410–418. doi: 10.1097/00004583-200204000-00013. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Bridging child, adolescent, and adult psychotherapy: Directions for research. Psychotherapy Research. 1995;5:258–277. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott PA. Longitudinal Interval Follow-Up Evaluation (LIFE): A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- King CA, Hovey JD, Brand E, Ghaziuddin N. Prediction of positive outcomes for adolescent psychiatric inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1434–1442. doi: 10.1097/00004583-199710000-00026. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Gender and the course of major depressive disorder through adolescence in clinically referred youngsters. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1079–1085. doi: 10.1097/00004583-200109000-00017. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Hops H, Andrews JA. Cognitive-behavioral treatment for depressed adolescents. Behavior Therapy. 1990;21:385–401. [Google Scholar]
- Lewinsohn PM, Clarke GN, Rohde P, Hops H, Seeley JR. A course in coping: A cognitive-behavioral approach to the treatment of adolescent depression. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington, DC: American Psychological Association; 1996. pp. 109–135. [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempt. Journal of Consulting and Clinical Psychology. 1994;62:297–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- MacPhillamy DJ, Lewinsohn PM. The pleasant events schedule: Studies on reliability, validity, and scale intercorrelation. Journal of Consulting & Clinical Psychology. 1982;50:363–380. [Google Scholar]
- McCleary L, Sanford M. Parental expressed emotion in depressed adolescents: Prediction of clinical course and relationship to comorbid disorders and social functioning. Journal of Child Psychology and Psychiatry. 2002;43:587–595. doi: 10.1111/1469-7610.00048. [DOI] [PubMed] [Google Scholar]
- Moos RH. Family Environment Scale and preliminary manual. Palo Alto, CA: Consulting Psychologists Press; 1974. [Google Scholar]
- Orvaschel H. Schedule for affective disorders and schizophrenia for school-age children epidemiologic version-5 (K-SADS-E-5) Ft Lauderdale, FL: Nova Southeastern University; 1994. [Google Scholar]
- Papakostas GI, Petersen T, Mischoulon D, Hughes ME, Spector An R, Alpert JE, et al. Functioning and interpersonal relationships as predictors of response in treatment-resistant depression. Comprehensive Psychiatry. 2003;44:44–50. doi: 10.1053/comp.2003.50012. [DOI] [PubMed] [Google Scholar]
- Renaud J, Brent DA, Baugher M, Birmaher B, Kolko DJ, Bridge J. Rapid response to psychosocial treatment for adolescent depression: A two-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1184–1190. doi: 10.1097/00004583-199811000-00019. [DOI] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, Kaufman NK. Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:795–802. doi: 10.1097/00004583-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Mace DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:660–668. doi: 10.1097/01.chi.0000121067.29744.41. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Tilson M, Seeley JR. Dimensionality of coping and its relation to depression. Journal of Personality and Social Psychology. 1990;58:499–511. doi: 10.1037//0022-3514.58.3.499. [DOI] [PubMed] [Google Scholar]
- Rude SS, Rehm LP. Response to treatments for depression: The role of initial status on targeted cognitive and behavioral skills. Clinical Psychology Review. 1991;11:493–514. [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A Children’s Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Singer, Willett Modeling the days of our lives: Using survival analysis when designing and analyzing longitudinal studies of duration and the timing of events. Psychological Bulletin. 1991;110:268–290. [Google Scholar]
- Sotsky SM, Glass DR, Shea MR, Pilkonis PA, Collins JJ, Elkin I, et al. Patient predictors of response to psychotherapy and pharmacotherapy: Findings in the NIMH Treatment of Depression Collaborative Research Program. American Journal of Psychiatry. 1991;148:997–1008. doi: 10.1176/ajp.148.8.997. [DOI] [PubMed] [Google Scholar]
- Thase ME, Simons AD, Reynolds CF. Abnormal electroencephalographic sleep profiles in more depression: Association with response to cognitive behavioral therapy. Archives of General Psychiatry. 1996;53:99–108. doi: 10.1001/archpsyc.1996.01830020013003. [DOI] [PubMed] [Google Scholar]
- Treatment for Adolescents with Depression Study Team. The Treatment for Adolescents with Depression Study (TADS): Short-Term Effectiveness and Safety Outcomes. Journal of the American Medical Association. 2004;292:807–820. [Google Scholar]
- Weissman MM, Beck AT. Development and validation of the Dysfunctional Attitude Scale; Paper presented at the Association for the Advancement of Behavior Therapy; Chicago, Illinois. 1978. [Google Scholar]
- Weissman MM, Orvaschel H, Padian N. Children’s symptom and social functioning self-report scales: Comparison of mothers’ and children’s reports. Journal of Nervous and Mental Disease. 1980;168:736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]
- Wickramaratne PJ, Weissman MM. Onset of psychopathology in offspring by developmental phase and parental depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:933–942. doi: 10.1097/00004583-199809000-00013. [DOI] [PubMed] [Google Scholar]
- Winters NC, Collett BR, Myers K. Ten-year review of rating scales, VII: Scales assessing functional impairment. Journal of the America Academy of Child and Adolescent Psychiatry. 2005;44:309–338. doi: 10.1097/01.chi.0000153230.57344.cd. [DOI] [PubMed] [Google Scholar]