Abstract
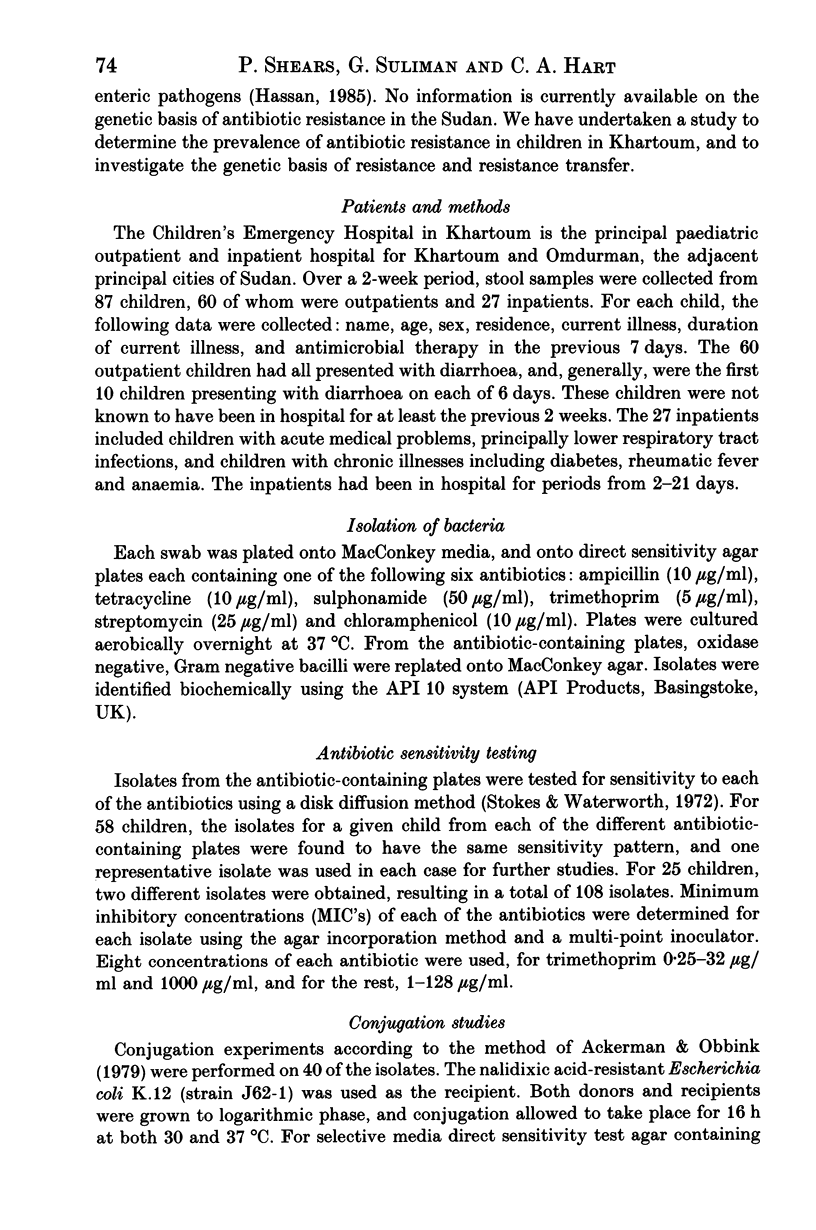
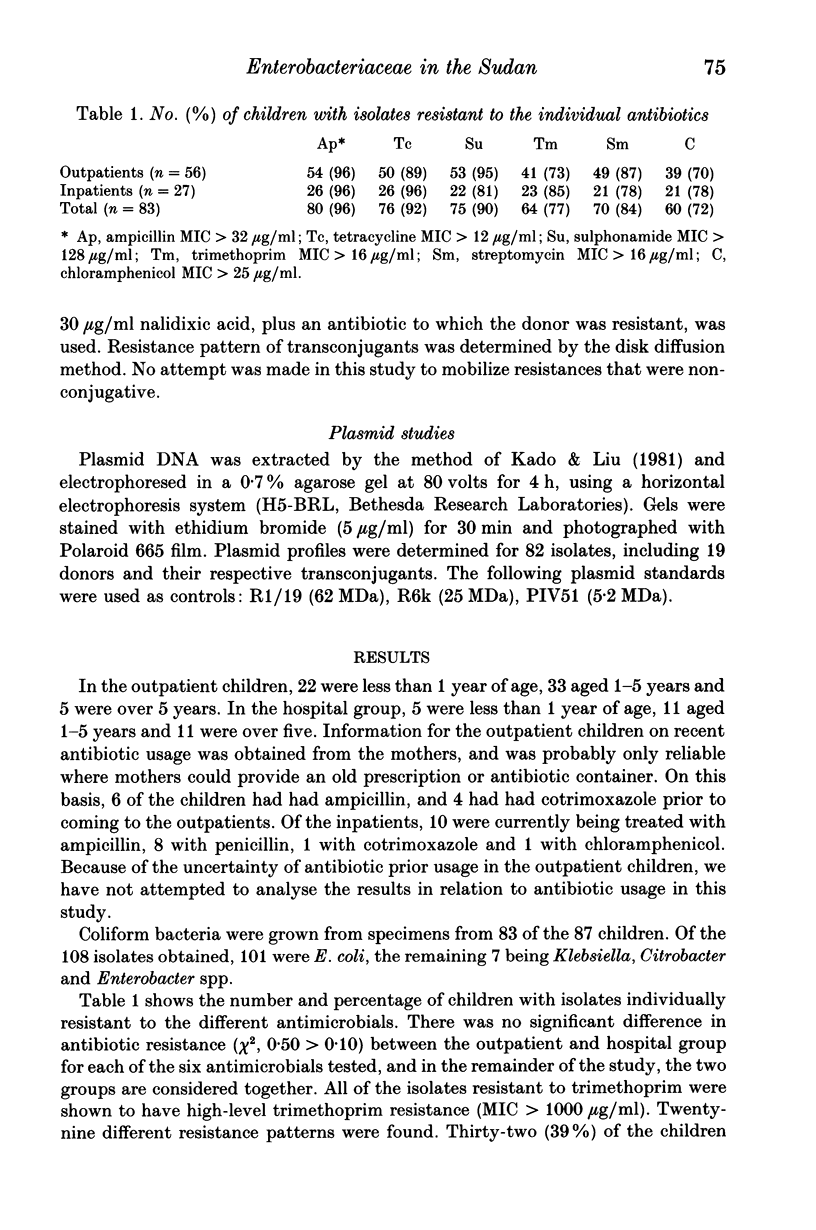
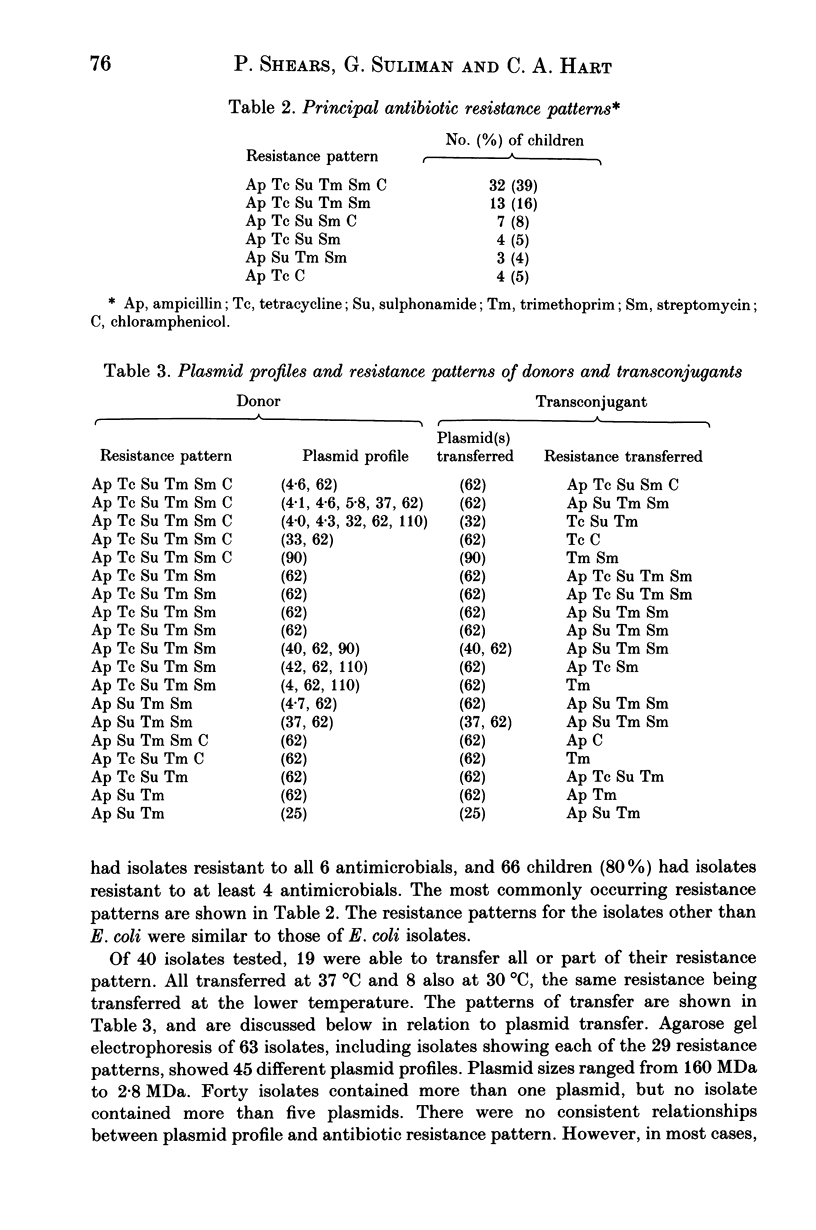
The prevalence of resistance to six commonly-used antimicrobial agents in faecal coliforms from children in Khartoum, Sudan was studied. A relatively high prevalence of resistance was found, ranging from 96% of children with isolates resistant to ampicillin to 70% of children with isolates resistant to chloramphenicol. Seventy-seven percent of children had isolates with high-level resistance to trimethoprim (MIC greater than 1000 micrograms/ml). Twenty-nine different resistance patterns were found. Thirty-nine percent of the children had isolates resistant to all six antibiotics studied, and 80% of children had isolates resistant to at least four. Transfer of resistance to each of the antimicrobials, in varying combinations, was demonstrated, but did not occur for all resistance patterns. Plasmid analysis showed plasmids ranging from 160 MDa to 2.8 MDa and isolates contained from one to five plasmids of different sizes. There were no consistent relationships between resistance pattern and plasmid profile, but multiple resistance transfer was mediated commonly by plasmids with a molecular weight of 62 MDa. The high prevalence of potentially transferable antibiotic resistance in gut commensals of children in the Sudan may be of importance in the management of enteric and other infections requiring antimicrobial treatment.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ackerman V. P., Groot Obbink D. J. Screening for transferable antibiotic resistance in the clinical laboratory. J Antimicrob Chemother. 1979 Mar;5(2):167–172. doi: 10.1093/jac/5.2.167. [DOI] [PubMed] [Google Scholar]
- Al-Jebouri M. M., Al-Meshhadani N. S. A note on antibiotic-resistant Escherichia coli in adult man, raw sewage and sewage-polluted River Tigris in Mosul, Nineva. J Appl Bacteriol. 1985 Dec;59(6):513–518. doi: 10.1111/j.1365-2672.1985.tb03354.x. [DOI] [PubMed] [Google Scholar]
- Burke J. P., Levy S. B. Summary report of worldwide antibiotic resistance: international task forces on antibiotic use. Rev Infect Dis. 1985 Jul-Aug;7(4):560–564. doi: 10.1093/clinids/7.4.560. [DOI] [PubMed] [Google Scholar]
- Farrar W. E. Antibiotic resistance in developing countries. J Infect Dis. 1985 Dec;152(6):1103–1106. doi: 10.1093/infdis/152.6.1103. [DOI] [PubMed] [Google Scholar]
- Frost J. A., Rowe B., Vandepitte J., Threlfall E. J. Plasmid characterisation in the investigation of an epidemic caused by multiply resistant Shigella dysenteriae type 1 in Central Africa. Lancet. 1981 Nov 14;2(8255):1074–1076. doi: 10.1016/s0140-6736(81)91277-0. [DOI] [PubMed] [Google Scholar]
- Hassan H. S. Sensitivity of Salmonella and Shigella to antibiotics and chemotherapeutic agents in Sudan. J Trop Med Hyg. 1985 Aug;88(4):243–247. [PubMed] [Google Scholar]
- Hossain M. M., Glass R. I., Khan M. R. Antibiotic use in a rural community in Bangladesh. Int J Epidemiol. 1982 Dec;11(4):402–405. doi: 10.1093/ije/11.4.402. [DOI] [PubMed] [Google Scholar]
- Kado C. I., Liu S. T. Rapid procedure for detection and isolation of large and small plasmids. J Bacteriol. 1981 Mar;145(3):1365–1373. doi: 10.1128/jb.145.3.1365-1373.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh C. L. Antibiotic resistance and conjugative R plasmids in clinical isolates of Enterobacteriaceae in Peninsular Malaysia. Trans R Soc Trop Med Hyg. 1986;80(1):158–161. doi: 10.1016/0035-9203(86)90221-x. [DOI] [PubMed] [Google Scholar]
- Levy S. B., Hedges R. W., Sullivan F., Medeiros A. A., Sosroseputro H. Multiple antibiotic resistance plasmids in Enterobacteriaceae isolated from diarrhoeal specimens of hospitalized children in Indonesia. J Antimicrob Chemother. 1985 Jul;16(1):7–16. doi: 10.1093/jac/16.1.7. [DOI] [PubMed] [Google Scholar]
- Mata L. J., Gangarosa E. J., Cáceres A., Perera D. R., Mejicanos M. L. Epidemic Shiga bacillus dysentery in Central America. I. Etiologic investigations in Guatemala, 1969. J Infect Dis. 1970 Sep;122(3):170–180. doi: 10.1093/infdis/122.3.170. [DOI] [PubMed] [Google Scholar]
- McDowell H. P., Shears P., Hart C. A., Martin J. Acute lymphoblastic leukaemia: trimethoprim resistant organisms during treatment. Arch Dis Child. 1987 Jun;62(6):573–575. doi: 10.1136/adc.62.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray B. E., Alvarado T., Kim K. H., Vorachit M., Jayanetra P., Levine M. M., Prenzel I., Fling M., Elwell L., McCracken G. H. Increasing resistance to trimethoprim-sulfamethoxazole among isolates of Escherichia coli in developing countries. J Infect Dis. 1985 Dec;152(6):1107–1113. doi: 10.1093/infdis/152.6.1107. [DOI] [PubMed] [Google Scholar]
- O'Brien T. F. Resistance to antibiotics at medical centres in different parts of the world. J Antimicrob Chemother. 1986 Oct;18 (Suppl 100):243–253. doi: 10.1093/jac/18.supplement_c.243. [DOI] [PubMed] [Google Scholar]
- Shahid N. S., Rahaman M. M., Haider K., Banu H., Rahman N. Changing pattern of resistant Shiga bacillus (Shigella dysenteriae type 1) and Shigella flexneri in Bangladesh. J Infect Dis. 1985 Dec;152(6):1114–1119. doi: 10.1093/infdis/152.6.1114. [DOI] [PubMed] [Google Scholar]
- Shears P., Hart C. A., Broadhead R. L., Coulter J. B. A note on antibiotic resistance in Escherichia coli isolated from children with diarrhoea in the Sudan. Ann Trop Paediatr. 1987 Mar;7(1):38–41. doi: 10.1080/02724936.1987.11748471. [DOI] [PubMed] [Google Scholar]
- Tomson G., Sterky G. Self-prescribing by way of pharmacies in three Asian developing countries. Lancet. 1986 Sep 13;2(8507):620–622. doi: 10.1016/s0140-6736(86)92438-4. [DOI] [PubMed] [Google Scholar]
- Young H. K., Jesudason M. V., Koshi G., Amyes S. G. Trimethoprim resistance amongst urinary pathogens in south India. J Antimicrob Chemother. 1986 May;17(5):615–621. doi: 10.1093/jac/17.5.615. [DOI] [PubMed] [Google Scholar]