Abstract
Adopting a developmental epidemiology perspective, the current study examines sources of risk heterogeneity for internalizing symptomatology among children of alcoholic parents (COAs). Parent-based factors, including comorbid diagnoses and the number of alcoholic parents in the family, as well as child-based factors, namely child gender, formed the indicators of heterogeneity. Following a novel approach to cross-study methods, we present a three-stage analysis involving measurement development using Item Response Theory, examination of study effects on latent trajectories over time using Latent Curve Modeling, and prediction of these latent trajectories testing our theoretically-derived hypotheses in two longitudinal investigations across both mother- and self-reported symptomatology. Specifically, we replicated previous findings that parent alcoholism has a unique effect on child internalizing symptoms, above and beyond those of both parent depression and antisocial personality disorder. However, we also found important subgroup differences, explaining heterogeneity within COAs’ risk profile in terms of the number of alcoholic parents in the family, comorbid diagnoses for the alcoholic parent and, for self-reported symptoms, child gender. Such factors serve to refine the definition of risk among COAs, suggesting a more severely impaired target group for preventive interventions, identifying the significance of familial alcoholism in individual differences underlying internalizing symptoms over time, and further specifying the distal risk matrix for an internalizing pathway to alcohol involvement.
Keywords: Parent alcoholism, high risk development, internalizing, cross-study, longitudinal analysis
Defining Risk Heterogeneity for Internalizing Symptoms among Children of Alcoholic Parents
Adopting a developmental epidemiology perspective (see Costello & Angold, 2006), the current study examines sources of risk heterogeneity for internalizing symptoms among children of alcoholic parents (COAs). Understanding factors contributing to risk heterogeneity among COAs is important for several reasons. First, internalizing symptoms are purported to form the basis for one of the pathways of risk leading to alcoholism in adults (Zucker, 2006). Thus, specifying the risk factors encompassed by parent alcoholism that are associated with internalizing symptoms may in part explain both COAs’ greater risk for eventual alcohol disorders as well as identify subgroup(s) of COAs most likely to show internalizing symptoms. Second, studies that have tracked the development of internalizing symptoms from early childhood into late adolescence indicate significant individual differences in the emergence of these symptoms over time (e.g., Ge, Lorenz, Conger, Elder & Simons, 1994; Kim, Capaldi & Stoolmiller, 2003). Thus, understanding risk heterogeneity among COAs also identifies sources of individual difference impacting the developmental emergence of internalizing symptoms. Third, by refining the risk indicator of parent alcoholism, target populations for preventive interventions may be defined with greater specificity and sensitivity and the phenomenological net defining risk processes leading to internalizing symptoms among COAs may be honed. And, fourth, identifying sources of heterogeneity in COAs’ risk for internalizing symptoms contributes indirectly to the growing literature on developmentally-informed phenotypes for alcoholism by clarifying one early link in the emergent process potentially underlying an internalizing form of adult alcoholism. For these reasons, we examined heterogeneity in the developmental trajectories of internalizing symptoms among COAs from early childhood into late adolescence across both mother- and self-reported symptoms, pooling data from two, independent longitudinal investigations.
COAs’ risk for internalizing symptoms
Evidence suggests that the relation between parent alcoholism and child internalizing symptoms is weaker than that between parent alcoholism and child externalizing symptoms (Chassin, Rogosch & Barrera, 1991; Edwards, Leonard & Eiden, 2001). Nonetheless, previous studies consistently support COAs' greater risk for internalizing symptoms compared to children of non-alcoholic parents, with COAs as young as 18 months showing elevated parent-reports on internalizing symptoms (Edwards et al., 2001). Similar results come from studies focusing on early and middle childhood (Loukas, Piejak, Bingham, Fitzgerald, & Zucker, 2001; Puttler, Zucker, Fitzgerald, & Bingham, 1998; Tubman, 1993). Studies by Chassin and colleagues (Chassin et al., 1991; Chassin, Pitts, DeLucia & Todd, 1999) show that adolescent COAs have higher maternal reports of internalizing symptoms than their peers, and that this risk continues into young adulthood when COAs show higher rates of affective and anxiety disorders.
Scant literature delineates the processes underlying the association between parent alcoholism and child internalizing symptoms, though theories of risk processes underlying an internalizing pathway to adult alcoholism (Zucker, 2006) and the development of adolescent internalizing symptoms, most notably depression, may be informative (Graber, 2004). Both literatures indicate that internalizing symptoms emerge from a combination of environmental risk factors and genetic liability. As such, we posit that COAs are at risk for greater internalizing symptoms via greater environmental stress exposure to which they respond with impaired coping strategies and a diathesis for internalized expressions of resulting distress.
Several lines of evidence support a genetic risk for internalizing symptoms in COAs. Family linkage and twin studies demonstrate at least modest co-transmission for internalizing disorders and alcoholism (Kendler, Neale, Heath, Kessler, & Eaves, 1994; Merikangas, Leckman, Prusoff, Pauls & Weissman, 1985; Zucker, 2006). Psychosocial studies report greater neuroticism and inhibition among COAs (Jansen, Fitzgerald, Ham, & Zucker, 1995; Sher, 1993), heritable temperament and personality indices associated with elevated risk for internalizing symptoms (Graber, 2004). Indeed, several studies report prospective prediction of adolescent alcohol involvement from childhood internalizing problems (Caspi, Moffit, Newman & Silva, 1996; Kellam, Ensminger & Simon, 1980; Zucker, Chermack, & Curran, 2000). Together, these findings indicate the potential for either co-transmission or a shared genetic diathesis for alcoholism and internalizing symptoms; thus, COAs may have greater genetic vulnerability for internalizing as related to an inherited risk for alcoholism.
In addition, early stress exposure and family conflict may be components of this risk process. Previous studies show elevated rates of depression among children exposed to family violence, conflict and other environmental stressors (DuRocher & Cummings, 2006), particularly when such stressors are cumulative, occur in tandem with developmental transitions, or are exacerbated by pre-existing vulnerabilities (Graber, 2004). The impact of early stressors and family conflict may be heightened among COAs due to increased exposure (Chassin, Pillow, Curran, & Molina, 1993), less effective coping skills (Hussong & Chassin, 2004), deficits in social competence and thus social resources (Hussong, Zucker, Wong, Fitzgerald, & Puttler, 2005) and more neurotic response styles (Sher, 1993). Moreover, COAs may show greater risk for internalizing symptoms due to the nesting of such risk structures (e.g., heightened genetic vulnerability within high-risk environments; Wong, Zucker, Puttler, & Fitzgerald, 1999), with this risk exacerbated by important developmental transitions, such as puberty, resulting in greater risk upon entry to adolescence than in childhood. We posit that these processes apply to a subsample of COAs and thus defining those COAs at greatest risk for internalizing symptoms over the early lifecourse is primary to defining how this risk process might operate.
Risk Heterogeneity
Although previous studies consistently show greater internalizing symptoms among COAs, not all COAs manifest this risk. To understand such heterogeneity, factors associated with variation in risk load among COAs require further delineation. Parent-based factors accounting for variability in other negative outcomes among COAs include comorbid diagnoses and the number of alcoholic parents in the family (Hussong et al., 2005; Puttler et al., 1998). Such factors may also demarcate points of heterogeneity among COAs that are relevant for examining risk for internalizing symptoms. Child-based factors that may serve a similar purpose, such as child gender, are under-studied as potential moderators of risk for internalizing symptoms associated with parent alcoholism. Finally, epidemiological studies of anxiety and depression indicate changes in the prevalence of internalizing symptoms with development (Compas et al., 1997).
Various theorists posit that the diagnosis of alcoholism may be meaningfully subtyped on the basis of co-occurring psychopathologies, most notably depression (often referred to as negative affect or depressive alcoholism) and antisociality (often referred to as antisocial alcoholism; Babor, 1996; Zucker, Ellis, Bingham & Fitzgerald, 1996; Zucker, 2006). These subtypes purportedly differ not only in associated symptomatology, but also in the course of alcohol involvement and associated problems over time, gender-sensitive susceptibilities, and genetic liability. Moreover, parents who differ in these subtypes of alcoholism may also differ in the risk for negative outcomes they convey to their offspring.
Depressive alcoholism may carry greater risk for internalizing symptoms in children because it represents genetic liability for both depression and alcoholism (Kendler, Prescott, Myers & Neale, 2003; Preisig, Fenton, Stevens & Merikangas, 2001); because children are exposed to and may model styles of drinking that emphasize emotional dysfunction (e.g., self-medication); because these parents are less likely to promote such resilience skills as active coping that may protect their at-risk offspring from the stressors of growing up in an alcoholic home (Hussong & Chassin, 2004); or because of the myriad of risks that these children face associated with having a depressed parent (Kaslow, Deering & Racusin, 1994). In addition, comorbidity alone is often associated with more severe disturbance, both in individual functioning and in the family context, and thus both depressive and antisocial alcoholism may increase stress exposure for COAs. However, little research has examined heterogeneity among COAs at risk for internalizing symptoms as a function of subtypes of parent alcoholism. Other than those focusing on paternal antisocial alcoholism (e.g., Fitzgerald, Zucker, & Yang, 1995), studies of sub-typing within parent alcoholism have been rare. The current study addresses this issue.
The number of alcoholic parents in the home may also impact severity of risk for internalizing symptoms in COAs. Given the impact of assortative mating (Maes et al., 1998; particularly in COAs, Boye-Beaman, Leonard & Senchak, 1991) and the lower base rates of alcoholism in women (Grant, Dawson, Stinson, Chou, Dufour & Pickering, 2004), a family with an alcoholic mother often also has an alcoholic father, so the impact of maternal alcoholism is often not practically distinguishable from that of having two alcoholic parents. As such, having two alcoholic parents may convey significantly greater risk for internalizing symptoms than having a single alcoholic parent because the primary caretaker for the child is more likely to be affected, the familial stress load and dysfunction within the home is likely heightened (Chassin et al., 1991; Hussong & Chassin, 2004), and the child lacks the potential protective influence of a non-affected parent (Werner, 1986; though this influence is not always supported, Curran & Chassin, 1996). Supporting this hypothesis, COAs show greater risk, defined as lower social competence, when they have two rather than one alcoholic parent as early as three years of age (Hussong et al., 2005).
The gender of the child may also impact heterogeneity in COAs’ risk for internalizing symptoms. Although studies of adolescent depression suggest that girls and boys show diverging trajectories around age 12 (Angold & Costello, 2001), these effects are less clear in studies of internalizing symptoms (rather than depression, specifically), rating scales as opposed to diagnostic interviews, and parent- rather than self- reported symptoms (Angold & Costello, 2001; Compas et al., 1997). Nonetheless, the impact of parent alcoholism on child internalizing symptoms may vary by child gender due to gendered patterns of expressing distress (e.g., Costello, Mustillo, Erkanli, Keeler & Angold, 2003) that may become intensified with the onset of puberty and adolescence (Wichstrom, 1999). Few studies have tested for such gender differences, though equal risk for parent-reported internalizing symptoms in male and female COAs has emerged from studies of children aged two through eight (Loukas et al., 2001; Puttler et al., 1998).
A final consideration in examining heterogeneity in COAs' risk for internalizing symptoms is the extent to which this risk is specific to parent alcoholism. Chassin et al. (1991) found that parent alcoholism uniquely predicted drug use and internalizing symptoms, above and beyond parental affective disorders and antisocial personality disorder, though parent affective disorder also uniquely predicted internalizing symptoms. Similarly, maternal depression and alcoholism have shown unique effects from one another in predicting behavior problems in young children (Fitzgerald et al., 1993). However, other research has failed to show greater internalizing in COAs as compared to children with a depressed parent (Jacob & Leonard, 1986) and to young children without an alcoholic parent, after controlling for maternal depression (Edwards et al., 2001). Together, these studies provide mixed support for the hypothesis that parent depression, rather than parent alcoholism, may be responsible for COAs' greater risk for internalizing symptoms. However, they do not consider the extent to which the co-occurrence of these disorders defines a particularly deleterious context for child development. Namely, children whose parents show both alcoholism and depression may show markedly greater risk for internalizing symptoms than children whose parents are only alcoholic.
In sum, the presence of comorbid diagnoses, the number of impaired parents in the home, and child gender may each refine our risk index for internalizing symptoms among COAs over the early life course. These risk indices may also serve to heightened COAs’ risk with puberty and the transition to adolescence. Specifically, we expected increased risk for internalizing symptoms among COAs whose parents show depressive and perhaps antisocial alcoholism, who have two alcoholic parents rather than one, and who are female. Due to the potential co-transmission of genetic risk for internalizing symptoms and adult alcoholism, we expected children of parents with depressed alcoholism to show greater risk for internalizing symptoms than would children of parents with antisocial alcoholism or with alcoholism alone. Moreover, risk mechanisms associated with greater exposure to stress and conflict may be enhanced in youth with more dense family alcoholism (two alcoholic parents rather than one) or parents with comorbid subtypes of alcoholism because of increased risk factors (higher genetic load) and greater disruptions within the family process (due to more severe family psychopathology impacting levels of conflict).
The Current Study
The current study investigates the extent to which comorbid parental diagnoses, number of alcoholic parents, and child gender can refine the concept of risk among COAs as specific to given sub-populations. Because such sub-populations are naturally rarer than the broader population of COAs, larger samples of these at-risk children have been difficult and expensive to recruit and study, especially within a longitudinal design. By pooling across two prominent studies of COAs, our analyses benefit from a larger sample of COAs and from longitudinal investigations of how such subgroups may vary over time.
The contributing studies have several methodological strengths that bolster potential weaknesses associated with multi-study methods. Each study utilizes a contrast group to permit direct comparison between COAs and their demographically similar peers. Moreover, each study sampled from the community and thus avoided the problems associated with treatment samples. They also provide broad assessments of variables that co-occur with parent alcoholism, permitting analyses delineating the specificity of these effects. Finally, these studies include strategies to avoid reporter bias through direct ascertainment of parent alcoholism and multiple reporter assessment techniques. The strengths of these individual studies thus contribute to our confidence in pursuing cross-study analyses of them. Using this cross-study approach, the current study offers a unique and rigorous test of factors underlying risk heterogeneity among COAs for the development of internalizing trajectories over the early life course, from ages 2 through 17, as based on two reporters, mothers and their children.
Method
Samples and Procedures
Two studies contribute data to the current analyses. Each study used a longitudinal, high-risk design in which COAs and controls with non-alcoholic parents were assessed repeatedly.
The Michigan Longitudinal Study (MLS) used a rolling, community-based recruitment procedure to assess three cohorts of children from families with alcoholic parents as well as children from matched, contrasting families without an alcoholic parent (Zucker, Fitzgerald, et al., 2000). In cohort one, 338 males, initially aged 2–5, and their parents completed a series of in-home interviews.1 Of these, 262 included an alcoholic parent and 76 were matched controls. COA families were identified through court-arrest records for male drunk drivers with a minimum blood alcohol concentration (of 0.15% at first arrest or 0.12% if multiple arrests) as well as through community canvassing. Inclusion criteria for COA families were that fathers meet Feighner diagnostic criteria for alcoholism during adulthood based on self-reports (Feighner et al., 1972), reside with their biological sons aged 3–5, and be in intact marriages with their sons’ biological mothers at the time of first contact and that sons show no evidence of fetal alcohol syndrome. (FAS was assessed by M.A.-level clinical psychologists trained in early child assessment who had experience using the Fetal Alcohol Study Group guidelines (Sokol & Claren, 1989) to evaluate facial dysmorphology, growth retardation, and other criteria to make the classification. For more details see Bingham, Fitzgerald, Fitzgerald & Zucker, 1996 and Noll, Zucker, Fitzgerald & Curtis, 1992). Contrast families were recruited through community canvassing in the neighborhoods in which COA families resided and were matched to COA families on the basis of age and sex of the target child and parallelism of community characteristics; both parents of controls had to be free of lifetime adult alcoholism and drug abuse/dependence diagnoses. Assessment waves involving both parents and the child(ren) (see following) were at three-year intervals.
Cohort two were girls from the cohort one families who were recruited when cohort one boys were at Wave 2. Because cohort one inclusion criteria involved having families with at least one male child and no restrictions on other children, these families had fewer girls. To provide age parallelism with cohort one child ages, where possible, and to begin assessments at ages 3–5, a broader age range was used to recruit girls. One target girl per family was enrolled if she was aged 3–11, with those aged 3–5 receiving the Wave 1 battery, those aged 6–8 receiving the Wave 2 battery, those aged 9–11 receiving the Wave 3 battery, and (at follow-up) those aged 12–14 receiving the Wave 4 battery. Similarly, the third cohort contained all additional siblings of the male target child in cohort one who were aged 3–11 at the time of data collection, with assessment batteries structured by age as for cohort one. The siblings in cohorts two and three were reassessed in all subsequent waves of data collection and received measures that paralleled the male target children in cohort one based on age of assessment. Because children in cohorts two and three were recruited later in time and could enter the study at older ages, fewer waves of data collection were available for these participants by design. A total of 152 girls (from 152 families) comprised cohort two and an additional 106 siblings (from 84 families) comprised cohort three.
Across all three cohorts, 596 children from 338 families provided four waves of data, separated by three-year intervals. A total of 399, 339, 402, and 418 participants had reports on their functioning available at waves 1–4, respectively, yielding an overall participation rate of 73% for those with at least two waves of data in the sample (see Zucker, Fitzgerald, et al., 2000, for a detailed description of sample criteria and recruitment procedures). These data were augmented by annual assessments completed by participating children (but not parents) beginning at age 11 and ranging up through age 17 (for the current study).
Each family completed a primarily in-home assessment conducted by trained staff that was blind to family diagnostic status. Although protocol length varied by wave of assessment, parent assessments typically involved 9–10 hours of data collection and child assessments were typically 7 hours (except for annual interviews which took one hour) each spread over seven testing sessions. Families were compensated $300 for their involvement if the assessment was carried out on a one-child family and $375 if two children were involved. Seventy percent of eligible court families and 93 percent of community canvassed families agreed to participate (overall participation rate was 84 percent).
In the Adolescent/ Adult Family Development Project (AFDP; Chassin et al., 1991), 454 adolescents and their parents completed repeated, computerized, in-home interviews. Of these, 246 included a biological and custodial alcoholic parent whereas 208 were matched controls. COA families were recruited by means of court records (n=103), wellness questionnaires from a health maintenance organization (n=22), and community telephone surveys (n=120). Inclusion criteria for COA families were Hispanic or non-Hispanic Caucasian ethnicity, Arizona residency, having a 10.5–15.5 year old adolescent, English-speaking, lack of cognitive limitations precluding an interview, and a biological and custodial parent who met DSM-III lifetime criteria for alcohol abuse or dependence. (Although not an exclusion criteria, fetal alcohol effects are unlikely in this sample given the low rate of heavy drinking, only 14 mothers in the full sample drank twice weekly at 3 or more drinks per occasion as per mothers’ report or fathers’ reports of mothers’ drinking; Chassin et al., 1991). Lifetime presence of parent alcoholism was determined through diagnostic interviews with parents using the Diagnostic Interview Schedule or through spousal report using the Family History Research Diagnostic Criteria (if the alcoholic parent was not interviewed). Matched control families were recruited by phone screens of families identified through reverse directory searches based on identified COAs. Control families matched COA families on the basis of ethnicity, family composition, target child’s sex and age and socioeconomic status. Direct interview data confirmed that neither biological nor custodial parents met criteria for a lifetime alcoholism diagnosis. Recruitment biases have been found to be minimal (Chassin, Barrera, Bech, & Kossak-Fuller, 1992; Chassin et al., 1991). Although contact rates were low (38.3% from archival records and 44.2% from reverse directories), participation rates were high (72.8% of eligible COA families and 77.3% of eligible control families participated). No recruitment biases were found for alcoholism indicators (available in archival data), although lower participation rates among lower SES and Hispanic families were found.
These families were initially interviewed when the adolescents were aged 11–15 (wave 1) and re-interviewed on an annual basis when the adolescents were aged 12–16 (wave 2) and 13–17 (wave 3). Sample retention has been high, with 97% interviewed at all of the first three waves (for details, see Chassin et al., 1992). Adolescents and parents completed computer-based interviews separately on each occasion and each received up to $65 for participation.
Because analyses used the accelerated longitudinal structure of these aggregate data (see Mehta & West, 2000 for a discussion of this approach), the mother- and self-report samples are described with respect to the underlying age distribution rather than assessment waves (see Figure 1). Across MLS and AFDP, 782 mothers participated in at least one assessment period, reporting on 1028 children and adolescents. For mother-report analyses, all waves of assessment were analyzed for those who had at least one mother-report of internalizing symptoms between ages 2 and 17 and who had complete parental psychopathology data. The resulting sample of 811 participants from 597 families was 63% male, 12% minority (primarily Hispanic), and 66% COA, with 42% having parents with a high school education or less and 28% having at least a college degree (see Table 1). Analyses indicated that excluded cases were similar to those retained in ethnicity, child gender, and parent diagnoses, although excluded cases were more likely to be from MLS (χ2(1, n = 1028)=8.85, p=.003), had a higher proportion of parental antisocial personality (χ2(1, n = 895)=17.25, p<.001), and had lower parental education (t(1026) = 4.11, p < .0001).
Figure 1.
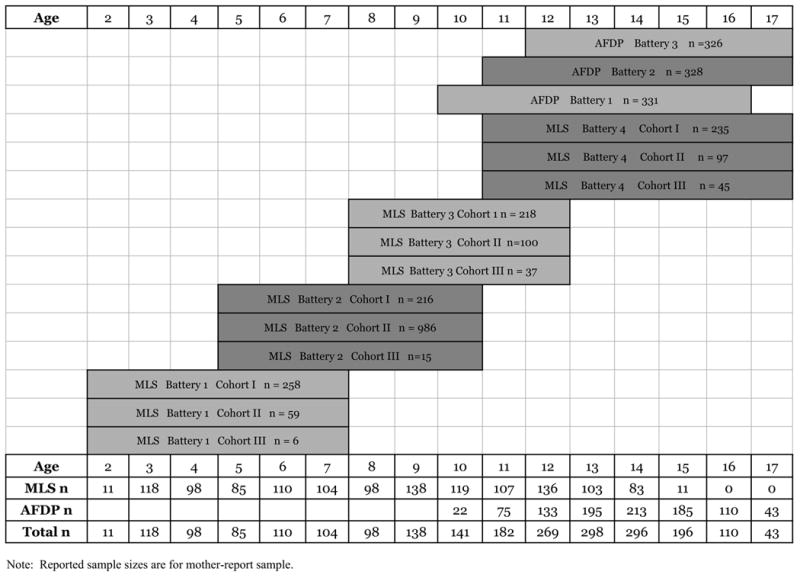
Cross Study Design
Table 1.
Demographic characteristics within and across studies and reporters
| Mother-report | Self-report | |||||
|---|---|---|---|---|---|---|
| MLS | AFDP | Total | MLS | AFDP | Total | |
| % male | 69.58 | 53.17 | 62.89 | 70.32 | 53.17 | 63.51 |
| % Caucasian | 98.13 | 73.11 | 87.92 | 98.21 | 73.11 | 88.24 |
| % Hispanic | 0.00 | 26.89 | 10.97 | 0.00 | 26.89 | 10.68 |
| % black | 1.87 | 0.00 | 1.11 | 1.79 | 0.00 | 1.08 |
| Parent education: | ||||||
| % with high school education or less | 55.62 | 21.45 | 41.68 | 54.58 | 21.45 | 41.42 |
| % college graduate | 22.92 | 35.35 | 27.99 | 23.90 | 35.35 | 28.45 |
| % 2 alcoholic parents | 35.83 | 6.34 | 23.80 | 33.67 | 6.34 | 22.81 |
| % 1 alcoholic parent (mother alcoholic) | 2.71 | 4.53 | 3.45 | 2.79 | 4.53 | 3.48 |
| % 1 alcoholic parent (father alcoholic) | 35.63 | 44.41 | 39.21 | 39.24 | 44.41 | 41.30 |
| % control (neither parent alcoholic) | 25.83 | 44.71 | 33.54 | 24.30 | 44.71 | 32.41 |
| % parental depression | 24.79 | 17.22 | 21.70 | 28.49 | 17.22 | 24.01 |
| % parental ASP | 19.38 | 9.67 | 15.41 | 18.53 | 9.67 | 15.01 |
Note. Self-report N = 833, Mother-report N = 811. There were N = 771 participants with both self- and mother-report internalizing data.
As with the mother-report data, all waves of assessment were analyzed for participants who had at least one self-report of internalizing symptoms between ages 10 and 17 and who had complete parental psychopathology data. The resulting sample of 833 participants from 612 families was 64% male, 12% minority (primarily Hispanic), and 68% COA, with 41% of families having parents with less than a high school education and 28% having at least a college degree (see Table 1). Analyses indicated that excluded cases were similar to those retained in parental antisocial personality, although excluded cases were more likely to be in AFDP than MLS (χ2(1, n = 971)=118.35, p<.0001), to be female (χ2(1, n = 971)=5.31, p=.02), to be ethnic minority (χ2(1, n = 971)=30.64, p<.0001), to have lower parental education (marginally; t(964)=1.88, p=.06), and to have higher rate of parental depression (χ2(1, n = 850)=19.31, p<.0001), but were less likely to be COA (χ2(1, n = 970)=9.72, p=.002).2
Measures
Demographic variables included participant gender (0 = female; 1 = male), age, ethnicity (0=Caucasian, 1=Hispanic or African American) and parent education (maximum of either parent's educational status assessed through parental report on a 6-point scale ranging from (0) less than 12 years or not a high school graduate to (5) graduate or professional school training).
Parent alcoholism3 was assessed by parent self-report in MLS and AFDP. In MLS, parental alcohol use disorder at Wave 1 was assessed by the Diagnostic Interview Schedule (DIS-Version III; Robins, Helzer, Croughan, & Ratcliff, 1980), the Short Michigan Alcohol Screening Test (SMAST; Selzer, Vinokur, & van Rooijan, 1975), and the Drinking and Drug History Questionnaire (DDHQ; Zucker, Fitzgerald, & Noll, 1990). On the basis of information collected by all three instruments, a lifetime diagnosis was made by a trained clinician using DSM-IV criteria.4 In each subsequent wave, past three year diagnoses were made. Inter-rater reliability for the diagnosis was excellent (kappa =.81).
In AFDP, parents completed assessments for lifetime alcoholism at wave 1 and for past year drinking and alcohol-related consequences at waves 2 and 3. At wave 1, when possible, parents were directly interviewed using a computerized version of the DIS to assess diagnostic status using DSM-III lifetime criteria. In cases where a biological parent was not directly interviewed (21% of fathers and 4% of mothers in the current subsample), the reporting parent was used as the informant using the FH-RDC (Andreasen, Endicott, Spitzer, & Winokur, 1977).5 For waves 2 and 3, we created proxy diagnoses based on parent reports of drinking frequency and their experience of alcohol-related consequences and dependence symptoms reflecting DSM-IV criteria for alcohol abuse and dependence (using items from Mayfield, McLeod, & Hall, 1974; Sher, 1993). Parents endorsing at least weekly drinking and experiencing either one of four abuse symptoms or any three of seven dependence symptoms in the past year were diagnosed as having a current (within the past year) alcohol disorder. In the current analyses, parents in MLS and AFDP were assigned to the impaired group if they met these criteria for alcohol abuse or dependence at any wave of assessment.
Parent comorbid diagnoses were assessed via parent interview. Lifetime affective disorder (major depression or dysthymia) and antisocial personality disorder (ASP) were obtained by DIS interview in the MLS, and by the computerized DIS in AFDP. In AFDP, parents completed the DIS and received lifetime diagnoses of affective disorder or ASP at wave 1. In MLS, parents completed the DIS at each wave of assessment. The diagnosis of an affective disorder was based on meeting criteria at any assessment prior to the first wave of data collection for that child. (Because parents could, for example, complete a lifetime assessment for their first child at wave 1 and subsequently a past three year assessment for a second child entering the study at wave 2, a diagnosis was given if the parent met criteria at any wave of assessment prior to that child’s entry into the study. Thus, for each child, parent affective disorder was a child-level variable representing a lifetime diagnosis temporally precedent to the child’s first wave of data collection.) An ASP diagnosis was based on wave 1 only because this disorder, by definition, yields a lifetime diagnosis. The diagnosis is based on the DIS, supplemented by information provided by the 46-item self-report Antisocial Behavior Inventory (ASB; Zucker, Ellis, Fitzgerald, Bingham, & Sanford, 1996) which assesses the frequency of aggressive/antisocial activity in childhood and adulthood. For current analyses, parent affective and ASP disorders, respectively, were considered present if either biological parent received a diagnosis.
Child internalizing symptoms were assessed via mother- and self-report. In both studies, participants completed the CBCL (MLS) or an adapted form of the CBCL (AFDP; Achenbach & Edelbrock, 1981). In the current study, we examined 13 items from the CBCL anxiety-depression subscale (although three items were not administered to adolescents in AFDP and thus coded as missing for these participants). The response scale ranged from 0–2 for parent report and for self-report in MLS and from 0–4 for self-report in AFDP, with an assessment window of past 6 months for MLS and past 3 months for AFDP.6 For the current study, we chose to dichotomize items as absent (0) or present (>0) because of sparse endorsement which introduced estimation problems and model instability.
Analytic Approach
Our statistical approach permits simultaneous analysis of data drawn from different longitudinal studies. Although we are drawing on existing methodologies, we combine these techniques in novel ways consistent with what McArdle and Horn (2002) refer to as mega-analysis. This methodology involved three primary phases.
First, we developed consistent measurement that is sensitive to differences due to contributing study through the use of item response theory (IRT; e.g., Embretson & Reise, 2000). IRT has several strengths in measurement evaluation and development. Perhaps most salient for constructing symptom scales is the ability to consider differential item contributions to the scale scores (as opposed to equal unit weighting as assumed by traditional alternatives such as proportion scores). In IRT, items contribute to scale scores depending on the pattern of responses endorsed across all administered items, such that items more strongly related to the latent trait being measured provide greater influence on scale scores than those that are less discriminating relative to the trait. As a result, IRT-based scores capture greater true score variability in the pattern of symptom endorsement than do proportion scores. Other advantages of IRT over traditional scoring methods include the creation of a true interval-level metric for the latent construct and the availability of techniques for testing and incorporating measurement invariance across discrete groups, such as those defined by study membership, age, and gender (see Curran, Edwards, Wirth, Hussong, & Chassin, in press; Khoo, West, Wu, & Kwok, 2006).
Second, we used these IRT-derived scores to model trajectories of internalizing symptoms over time using latent curve modeling (LCM). These methods examined study differences in trajectories of internalizing symptomatology using techniques for incorporating cohort-sequential designs and missing data estimation (Bollen & Curran, 2005). Moreover, these analyses benefited from the greater variability of IRT-derived scores that can thus be used to index greater intra- and inter-individual variability in symptom trajectories over time (Curran et al., in press). And, third, we tested our substantive questions of interest in conditional growth models in which predictors of these trajectories were examined.
Results
Cross Study Analysis Phase I: Measurement
Because AFDP and MLS differ to some extent in methodology and sample composition, we first evaluated measurement invariance in our CBCL measure of internalizing symptoms and used information about invariance to develop comparable scales for mother- and self-reported internalizing that share a common metric across studies. Specifically, we used IRT to evaluate differential item functioning (or DIF; e.g., Thissen, Steinberg, & Wainer, 1993) as a test of whether items functioned similarly in relation to the underlying construct of internalizing symptoms across important subgroups based on child age, gender and study membership. Next, incorporating the results of DIF testing, we calibrated items to calculate optimal item parameters for creating scale scores. Because the responses to each item were dichotomized, it was appropriate to fit a two-parameter logistic IRT model (2PL; Thissen & Orlando, 2001). With this IRT model, each item is characterized by a logistic function, or item characteristic curve, with its own discrimination and severity (or threshold) parameters. This curve describes the probability of endorsing an item given the scale value of the latent construct (typically denoted as θ) being measured, where θ is assumed to have a standard normal distribution. The discrimination parameter describes the extent to which the item is related to the latent trait being measured (akin to a factor loading), whereas the severity parameter represents the level of theta at which a respondent has a 50% probability of endorsing the item. Finally, we used the resulting parameters to estimate individual time-specific scores for each report of internalizing symptoms.
Both DIF testing and item calibration were conducted by including all available participants with at least one internalizing assessment within reporter, regardless of other missing data. Thus, our calibration samples of N = 1026 for mother-reports and N=971 for self-reports were larger than our analysis samples (described above). We conducted DIF tests using Thissen’s (2001) IRTLRDIF software (following Thissen et al., 1993). First, we tested for DIF according to age, where the calibration sample was dichotomized into young and old groups [age 2 to 11 (n = 475) vs. age 12 to 17 (n=551) for mother-reports and age 10 to 13 (n=429) vs. age 14 to 17 (n=542) for self-reports].7 For each item, a χ2 statistic tested whether the discrimination and threshold IRT parameters were (jointly) significantly different according to group membership.8 Upon finding DIF for a given item, follow-up χ2 tests determined whether the discrimination parameter, threshold parameter, or both significantly differed across groups. Seven internalizing items showed significant age DIF for mother-reports and no items did so for self-reports (see Table 2).
Table 2.
Results of DIF testing and item calibration for mother- and self-reported internalizing scales
| Items showing no DIF in either mother- or self-reports | ||||
| Mother-Reports | Self-Reports | |||
| Item Description | Discrimination | Severity | Discrimination | Severity |
| Feels lonely | 1.76 (.17) | 0.72 (.07) | ||
| Afraid might do bad things | 1.32 (.24) | 1.45 (.21) | ||
| Feels has to be perfect | 0.98 (.12) | 0.54 (.11) | ||
| Feels unloved | 2.33 (.28) | 1.46 (.10) | ||
| Feels worthless | 2.44 (.24) | 0.98 (.06) | 2.66 (.32) | 1.33 (.08) |
| Nervous/highstrung/tense | 1.34 (.15) | 1.30 (.13) | ||
| Self-conscious2 | 1.37 (.14) | −0.11 (.07) | 1.31 (.19) | 0.20 (.11) |
| Unhappy/sad/depressed | 2.49 (.25) | 0.95 (.06) | 2.29 (.22) | 0.77 (.06) |
| Worries a lot | 2.07 (.19) | 0.43 (.06) | 1.88 (.18) | 0.52 (.06) |
| Feels others are out to get him/her2 | 1.55 (.21) | 1.93 (.18) | 1.40 (.28) | 1.80 (.28) |
| Items showing Age, Gender or Study DIF | ||||
| Mother-Reports | Self-Reports | |||
| Item Description | Discrimination | Severity | Discrimination | Severity |
| Feels lonely | 1.48 (.12) | 1.06(.12)Y | ||
| 1.47 (.12)O | ||||
| Cries a lot1 | 0.76 (.10)YG | 0.59 (.34)YG | 1.84 (.16) | 0.70 (.10)G |
| 0.76 (.10)YB | 1.49 (.24)YB | 1.80 (.12)B | ||
| 1.98 (.40)OG | 1.24 (.15)OG | |||
| 1.07 (.32)OB | 2.76 (.65)OB | |||
| Afraid might do bad things2 | 1.09 (.22)Y | 1.52 (.30)Y | ||
| 1.91 (.27)O | 1.40 (.13)O | |||
| Feels has to be perfect | 1.64 (.23)Y | 0.43 (.11)Y | ||
| 0.79 (.15)O | 0.06 (.16)O | |||
| Feels unloved | 1.32 (.22)Y | 0.96 (.18)Y | ||
| 1.96 (.26)O | 1.07 (.10)O | |||
| Nervous/highstrung/tense | 1.70 (.24)M | 0.54 (.10)M | ||
| 2.10 (.28)A | 0.59 (.08)A | |||
| Too fearful/anxious | 2.00 (.16) | 1.20 (.11)Y | 2.64 (.35)M | 0.90 (.09)M |
| 1.41 (.13)OG | 1.31 (.20)A | 0.80 (.13)A | ||
| 1.11 (.12)OB | ||||
| Too guilty1 | 2.62 (.24) | 1.70 (.14)Y | 1.63 (.14) | 1.67 (.14)M |
| 1.31 (.08)O | 0.95 (.10)A | |||
Note: N=1026 for mother-report and N=971 for self-reports. Superscripts denote item showed DIF by age (Y=young, O=old), gender (G=girls, B=boys) and study (M=MLS, A=AFDP). The young sub-group refers to children aged 10 through 14 and the old sub-group refers to children aged 15 trough 17.
Discrimination parameters constrained to be equal in self-report analyses.
Items for which only MLS data were available by self-report.
To derive separate item parameter estimates by age group, items with age DIF were split into two “sub-items”, one for young participants and one for old participants, with the sub-item not pertaining to a particular group coded as missing. After creating the sub-items, we tested for gender DIF among the sub-items and original items that did not show age DIF. Three items showed significant gender DIF for mother-reports and one item did so for self-reports. After creating additional sub-items for these items with gender DIF, we tested for DIF by study membership.9 None of the items showed significant study DIF for mother-reports but three items did so for self-reports. By thus testing and accounting for DIF, we controlled for potential measurement confounds in subsequent growth models using IRT-scaled internalizing scores.
In the calibration phase, we estimated the discrimination and severity parameters for each of the items. We established a common IRT metric for the two studies using a type of common-items equating called “concurrent calibration,” such that single-population item parameters were estimated from a combined data set containing data from both studies (Wingersky & Lord, 1984). We fit the 2PL model to the item responses from the calibration sample using MULTILOG (Thissen, 1991), obtaining separate parameter estimates for sub-items that were created as a result of DIF testing.10 The item parameter estimates and their standard errors are given in Table 2.
In the scoring phase, we used these item parameter estimates to calculate IRT-scaled internalizing scores for each participant’s set of repeated observations based on her or his item responses. We followed the scoring method described by Thissen and Orlando (2001), using maximum a posteriori (MAP) values for each participant’s set of repeated measures, computed with MULTILOG. These scores served as the observed dependent variables in the growth models described below.
Cross Study Analysis Phase 2: Constructing Trajectories
Mean values by age and by study for the IRT-scaled internalizing scores are presented in Figure 2 for both mother- and self-reports. We fit a series of LCMs to the internalizing IRT scores across all ages, using full-information maximum likelihood estimation (e.g., Arbuckle, 1996) to account for the fact that, by virtue of each study’s design, no participant provided complete data across all ages. Additionally, because some of the participants in the MLS were siblings, we used the method of Muthén and Satorra (1995) to adjust standard errors and model fit statistics that account for this source of non-independence among observations. All models were estimated with Mplus (Muthén & Muthén, 2004).
Figure 2.
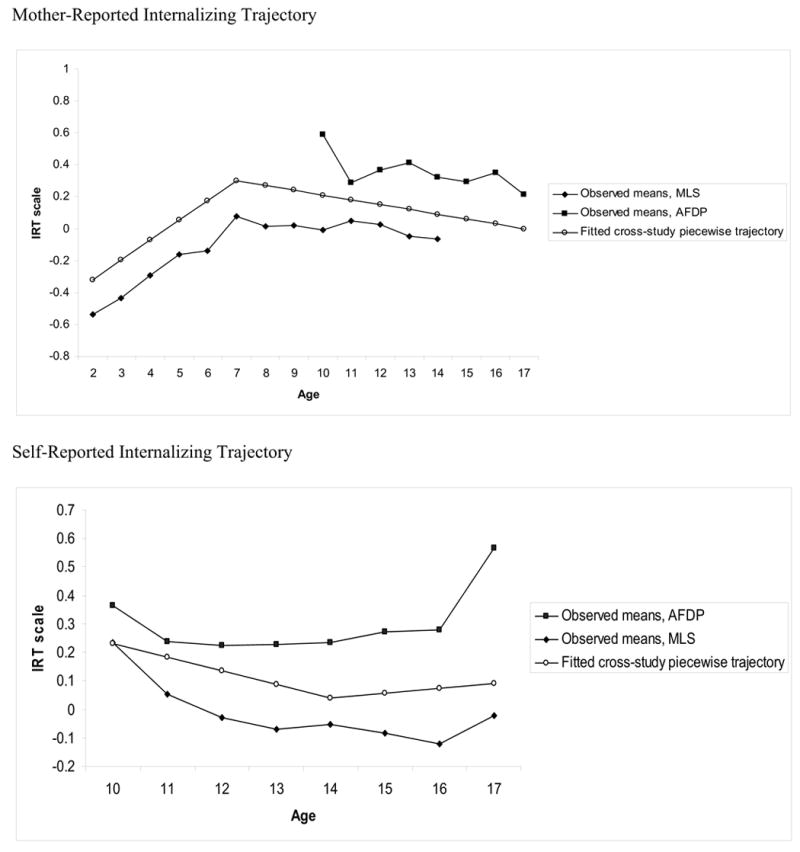
Observed Means by Study with Fitted Cross-Study Piecewise Trajectory
We first fit a series of unconditional growth curve models to specify the optimal functional form of growth for the internalizing scores and to establish a firm basis for moving to conditional growth models examining the effects of covariates on random growth factors (McArdle, 1988). These forms of growth included a simple linear model, a quadratic model, and a set of piecewise linear models with varying ages for the “knot point” at which the two linear pieces were joined (Bollen & Curran, 2005). Because these models were not formally nested, we compared their fit to the data by examining the match between the model-implied growth trajectories and the observed means at each age.
For mother-reports, a piecewise linear model with the first linear piece describing change from age 2 to 7 and the second describing change from age 7 to 17 provided the best balance between model fit and parsimonious interpretation.11 The model was parameterized so that the intercept factor represented internalizing at age 13 to capture the transition to adolescence. (Alternate intercept codes were probed during model testing when significant influences on slope factors suggested age differences in relevant main effects and results are reported in endnotes). For self-reports, a piecewise linear model with the first linear piece describing change from age 10 to 14 and the second describing change from age 14 to 17 was selected. As with mother-reports, the model was parameterized so that the intercept factor represented internalizing at age 13. These piecewise models defined the basic functional form of growth in the internalizing scores for our remaining growth models examining the longitudinal relationships between our covariates of theoretical interest and internalizing.
Baseline model: Internalizing growth model conditioned on study and demographic covariates
Because the pattern of mean internalizing scores in Figure 2 showed clear differences as a function of study, our initial model described internalizing trajectories across ages conditioned on study as well as demographic covariates, namely gender, ethnicity, and parental education. In addition, for this and each subsequent model, we tested whether study membership moderated the relationships between each covariate and the latent intercept and slope factors. (Because only participants from the MLS were observed during age 2 to 7, we did not test whether study moderated the relations between covariates and the first slope factor for mother-reports.) Finally, non-significant study by covariate interaction terms were dropped in the final reported models (although all main effects were retained) to facilitate model interpretation and to stabilize model estimation.12 Parameter estimates for the relationships between the growth factors and the demographic covariates are in Tables 3 and 4 for both reporters. Importantly, there was no evidence that study significantly moderated any of the relationships between the demographic variables and the growth factors for either reporter; thus, only main effects and interactions with time (i.e., predictions of slope) were retained.
Table 3.
LGM results testing effect of number of alcoholic parents on mother- report of internalizing trajectories
| Growth factor: | Intercept (age 13) | Slope age 2–7 | Slope age 7–17 | |||
|---|---|---|---|---|---|---|
| Covariate | b | se | b | se | b | se |
| Baseline | ||||||
| Study | 0.46a | 0.07 | −0.04d | 0.02 | ||
| Gender | −0.09 | 0.05 | 0.04 | 0.03 | −0.04b | 0.01 |
| Ethnicity | −0.05 | 0.09 | 0.02 | 0.07 | 0.00 | 0.03 |
| Parent Education | −0.07c | 0.03 | 0.01 | 0.01 | −0.01 | 0.01 |
| Model 1 | ||||||
| Study | 0.66a | 0.09 | −0.03 | 0.02 | ||
| Gender | −0.07 | 0.05 | 0.04 | 0.03 | −0.04b | 0.01 |
| Ethnicity | −0.06 | 0.08 | 0.02 | 0.07 | 0.00 | 0.03 |
| Parent Education | −0.06c | 0.03 | 0.01 | 0.01 | 0.00 | 0.01 |
| # alcoholic parents: 0 vs. 1 (MLS)1 | 0.12 | 0.10 | −0.02 | 0.04 | 0.01 | 0.02 |
| # alcoholic parents: 0 vs. 1 (AFDP)1,2 | −0.17c | 0.08 | 0.01 | 0.02 | ||
| # alcoholic parents: 2 vs. 11 | 0.31a | 0.09 | −0.03 | 0.04 | 0.03d | 0.02 |
| Model 2 | ||||||
| Study | 0.65a | 0.08 | −0.03 | 0.02 | ||
| Gender | −0.07 | 0.05 | 0.04 | 0.03 | −0.04b | 0.01 |
| Ethnicity | −0.04 | 0.08 | 0.01 | 0.06 | −0.01 | 0.03 |
| Parent Education | −0.05c | 0.02 | 0.01 | 0.02 | 0.00 | 0.01 |
| # alcoholic parents: 0 vs. 1 (MLS)1 | 0.15 | 0.10 | −0.02 | 0.04 | 0.02 | 0.02 |
| # alcoholic parents: 0 vs. 1 (AFDP)1,2 | −0.11 | 0.08 | 0.02 | 0.02 | ||
| # alcoholic parents: 2 vs. 11 | 0.28a | 0.08 | −0.02 | 0.03 | 0.02 | 0.02 |
| Parent depression | 0.36a | 0.08 | 0.04 | 0.03 | 0.00 | 0.02 |
| Parent ASP | 0.02 | 0.09 | −0.04 | 0.05 | 0.04 | 0.02 |
Note. N = 811. Study is coded 0 = MLS, 1 = AFDP; Gender is coded 0 = female, 1 = male; Ethnicity is coded 0 = Caucasian, 1 = ethnic minority.
p < .001,
p < .01,
p < .05,
p < .10. Regression coefficients for # alcoholic parents: 0 vs. 1 for MLS and AFDP are within-study simple slope effects.
The comparison group is having one alcoholic parent in these dummy codes.
Report of simple slopes found upon probing for AFDP.
Table 4.
LGM results testing effect of number of alcoholic parents on self-reported internalizing trajectories
| Growth factor: | Intercept (age 13) | Slope age 10–14 | Slope age 14–17 | |||
|---|---|---|---|---|---|---|
| Covariate | b | se | b | se | b | se |
| Baseline | ||||||
| Study | 0.23a | 0.06 | 0.04 | 0.03 | 0.01 | 0.04 |
| Gender | −0.18a | 0.05 | −0.10a | 0.03 | 0.01 | 0.03 |
| Ethnicity | −0.02 | 0.08 | −0.11c | 0.05 | 0.04 | 0.06 |
| Parent Education | −0.01 | 0.02 | −0.03c | 0.01 | 0.00 | 0.01 |
| Model 1 | ||||||
| Study | 0.25a | 0.06 | 0.05 | 0.04 | 0.01 | 0.04 |
| Gender | −0.18a | 0.05 | −0.10b | 0.03 | 0.01 | 0.03 |
| Ethnicity | −0.03 | 0.08 | −0.11c | 0.05 | 0.04 | 0.06 |
| Parent Education | 0.00 | 0.02 | −0.03c | 0.01 | 0.00 | 0.01 |
| # alcoholic parents: 0 vs. 11 | −0.17b | 0.06 | 0.01 | 0.03 | 0.03 | 0.03 |
| # alcoholic parents: 2 vs. 1 (MLS)1 | 0.16d | 0.08 | 0.03 | 0.04 | −0.01 | 0.04 |
| # alcoholic parents: 2 vs. 1 (AFDP)1,2 | 0.43b | 0.15 | 0.03 | 0.04 | −0.01 | 0.04 |
| Model 2 | ||||||
| Study | 0.24a | 0.06 | 0.05 | 0.04 | 0.01 | 0.04 |
| Gender | −0.18a | 0.05 | −0.10a | 0.03 | 0.01 | 0.03 |
| Ethnicity | −0.02 | 0.08 | −0.11c | 0.05 | 0.04 | 0.06 |
| Parent Education | 0.00 | 0.02 | −0.03c | 0.01 | 0.01 | 0.01 |
| # alcoholic parents: 0 vs. 11 | −0.14c | 0.06 | −0.01 | 0.03 | 0.03 | 0.04 |
| # alcoholic parents: 2 vs. 11,2 | 0.19c | 0.08 | 0.06 | 0.04 | −0.03 | 0.04 |
| Parent depression | 0.13c | 0.06 | −0.06d | 0.03 | −0.04 | 0.03 |
| Parent ASP (MLS) | −0.07 | 0.08 | −0.07 | 0.04 | 0.09d | 0.05 |
| Parent ASP (AFDP) | 0.24d | 0.13 | −0.07 | 0.04 | 0.09d | 0.05 |
Note. N = 833. Study is coded 0 = MLS, 1 = AFDP; Gender is coded 0 = female, 1 = male; Ethnicity is coded 0 = Caucasian, 1 = ethnic minority.
p < .001,
p < .01,
p < .05,
p < .10. Regression coefficients for # alcoholic parents: 2 vs. 1 and Parent ASP are within-study simple slope effects for MLS and AFDP.
The comparison group is having one alcoholic parent in these dummy codes.
Report of simple slopes found upon probing for AFDP.
For mother-reports (see Table 3), gender was not significantly related to the intercept factor or the first linear slope factor, suggesting that boys and girls showed similar increases in internalizing scores from age 2 to 7. However, gender was significantly associated with the second linear slope factor (p = .002), such that among boys, internalizing scores significantly decreased on average from age 7 to 17 (p < .001), whereas among girls, internalizing scores were largely constant across these ages (p = .34; see Figure 3 for model-implied internalizing trajectories by gender along with observed means). 13 Additionally, parental education was significantly related to the intercept factor (p = .01), such that higher levels of parental education were associated with lower levels of internalizing at age 13. None of the remaining relations between demographic covariates and the growth factors was significant.
Figure 3.
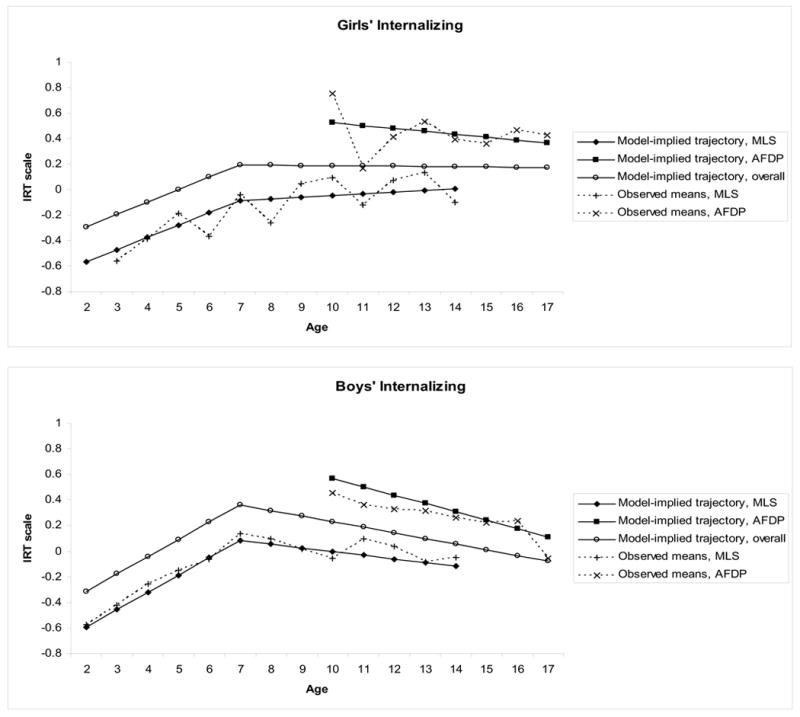
Baseline Model Showing Piecewise Growth Model by Gender with Observed Means for Mother-Reports
Controlling for these demographic covariates, study membership was significantly related to the intercept factor (p < .001), such that participants in the AFDP had higher age 13 internalizing scores. The relation between study membership and the second slope factor was marginally significant (p = .07). However, within both studies, the mean slope for age 7 to 17 did not differ from zero (p = .34 for MLS; p = .23 for AFDP), indicating that participants maintained relatively consistent levels of internalizing over these ages, after controlling for the effects of the demographic covariates.14 Finally, the mean of the first linear slope factor was significantly greater than zero (p < .001), reflecting that internalizing scores increased, on average, from age 2 to 7. This slope factor did not support the estimation of a random component, so its variance was set to zero. The residual variances of the intercept factor and the second slope factor were significantly greater than zero (p < .001 for intercept; p = .04 for second slope). The baseline model accounted for 11.3% of the variance in the intercept factor and 24.0% of the variance in the slope factor defining mother-reported internalizing trajectories.
In the self-report model (see Table 4), gender was also significantly related to the intercept factor (p < .001) and to the first linear slope factor (p = .002), such that girls had higher internalizing scores at age 13 that remained relatively stable, whereas boys had lower scores at age 13 that significantly decreased from age 10 to 13 (p < .0001) but did not change from age 13 to 17 (p = .20; see Figure 4). Although neither ethnicity nor parent education predicted age 13 intercepts, both were associated with change over time. Specifically, ethnicity was significantly associated with the first slope factor (p = .002), such that among ethnic minority participants, internalizing scores significantly decreased on average from age 10 to 14 (p = .002), whereas among white participants, internalizing scores stayed at approximately the same level across these ages (p = .23). Parental education also predicted the first slope (p = .04), such that higher levels of education were associated with greater decreases in internalizing from ages 10 to 14. Controlling for these demographic covariates, study membership was significantly related to the intercept factor for self-reports (p < .001), such that participants in the AFDP had higher age 13 internalizing scores, although study membership did not predict change over time. Finally, the residual variances of each growth factor were significantly greater than zero (p < .001 for intercept; p = .01 for first slope; p = .001 for second slope). The baseline model accounted for 6.6% of the variance in the intercept factor and 15.8 and 0.8% of the variance in the slope factors for ages 10–14 and 14–17, respectively, defining self-reported internalizing trajectories.
Figure 4.
Baseline Model Showing Piecewise Growth Model by Gender with Observed Means for Self-Reports
Probing study effects
Due to our interest in cross-study methods, we also explored possible explanations for the study effect on internalizing trajectories (focusing on the mother-report model as an example). First, because these models control for parental education, ethnicity and gender, differences in base rates of these demographic factors across studies do not explain study differences in internalizing symptomatology. Second, subsequent models showed that neither different proportions of parental depression and antisociality (see results of model 2 below) nor of boys and girls across the COA and control groups (i.e., gender x COA interactions; see results of model 4 below) explained these study differences. Third, we found no evidence that outlying observations influenced study differences in internalizing symptoms.15 Fourth, we found no differences in these results as a function of whether we examined IRT-based internalizing scores or proportion scores. Fifth, item analyses indicated that study differences were not driven by a subset of internalizing symptoms. Finally, we considered differences in assessment procedures. However, instrument differences in the time frame of assessment (six months in MLS and three months in AFDP), should result in an opposite pattern of study differences than that found here. As such, no obvious explanation for study differences was identified that could then be modeled. We thus chose to include our study indicator as a covariate in all subsequent models and to test for study differences in the relation between all predictors and internalizing to correct for potential study differences in hypothesis testing.
In sum, both gender and parent education significantly explained individual differences in mother-reported internalizing trajectories whereas gender, ethnicity and parent education were each related to self-reported internalizing trajectories. Below, we describe models that expand on this baseline model to determine whether heterogeneity in parent alcoholism further accounts for individual differences in internalizing trajectories.
Cross Study Analysis Phase 3: Hypothesis Testing
Model 1: Internalizing growth model conditioned on number of alcoholic parents
We examined heterogeneity within parental alcoholism effects on internalizing trajectories as a function of whether one or both parents had an alcohol use disorder. We created two dummy coded variables in which participants with one alcoholic family (the baseline group; with 8.09 and 7.77% of these impaired parents being mothers) were compared to those without an alcoholic parent (0 vs. 1 comparison) and to those with two alcoholic parents (2 vs. 1 comparison). We first added these dummy codes and the interaction between the dummy codes and study membership to our baseline model (see Model 1, Tables 3 and 4).
For mother-reports, study membership did not moderate the effects of having two alcoholic parents versus one alcoholic parent; however, study did moderate the effects of having one alcoholic parent versus none (p = .03). Specifically, participants in the AFDP with one alcoholic parent had significantly higher levels of internalizing at age 13 than controls (p = .04), whereas this comparison was not significant among participants in the MLS. The dummy code comparing participants with two versus one alcoholic parent was significantly associated with the intercept factor (p < .001) and marginally associated with the slope factor for age 7 to 17 (p = .07). Participants with two alcoholic parents had higher levels of age 13 internalizing and steeper increases than participants with only one alcoholic parent.16 The addition of parent alcoholism predictors accounted for an additional 4.8% and 3.7% of the variance in the intercept and slope for mother-reported trajectories of internalizing symptoms beyond the baseline model.
For self-reports, study membership did not moderate the effect of having one alcoholic parent versus none; however, study did (marginally) moderate the effect of the intercept factor on having one alcoholic parent versus two alcoholic parents (p = .09). Specifically, in both studies, participants with two alcoholic parents had significantly higher levels of internalizing at age 13 than those with one (p = .05 for MLS; p = .003 for AFDP), though this difference was greater among AFDP participants. The dummy code comparing participants with one alcoholic parent versus none was significantly associated with the intercept factor (p = .004), such that participants with one alcoholic parent had higher levels of age 13 internalizing than controls. Neither of the parent alcoholism dummy codes significantly predicted the two slope factors. The inclusion of parent alcoholism predictors accounted for an additional 2.3, 0.5, and 0.5% of the variance in the intercept and two slope factors for the self-reported trajectories of internalizing symptoms beyond the baseline model.
Model 2: Internalizing growth model conditioned on number of alcoholic parents and other parental psychopathology
We next tested the unique effects of parental alcoholism, specifically evaluating whether the effects described above for Model 1 remained predictive of internalizing trajectories while controlling for affective and ASP disorders. There was no evidence that study membership interacted with the effects of either of these covariates on the growth curve factors for mother-reports (see Model 2, Table 3). Parental depression was significantly associated with the intercept factor (p < .001), such that age 13 internalizing scores were higher for participants who had a depressed parent than for other participants. Importantly, despite this effect of parental depression, the comparison between participants with two alcoholic parents versus one remained significantly associated with the intercept factor (p < .001). However, the dummy variable comparing participants with one alcoholic parent to controls did not account for significant differences in the intercept factor over and above parental depression and ASP in either study (even though the study by dummy variable interaction remained significant). Parental depression and ASP were not significantly related to the slope factors. Finally, parental alcoholism no longer impacted the second slope over and above the effects of parental depression and ASP. The final model accounted for an additional 4.9 and 2.8% of variance over the baseline model in the intercept and slope factors for mother-reported internalizing trajectories.
For self-reports (see Model 2, Table 4), study membership interacted with parent ASP to predict the intercept factor (p = .04), such that parent ASP was marginally associated with higher age 13 internalizing in AFDP but not MLS. Parental depression predicted the intercept (p = .03) and (marginally) the first slope factor (p = .06). Specifically, participants with depressed parents had higher internalizing scores at age 13 but showed greater decreases in internalizing scores over early adolescence. That is, participants with a depressed parent showed elevated risk for internalizing symptoms from ages 11 to 13, but not afterwards, when their internalizing scores were similar to those of participants without a depressed parent. 17 Importantly, the comparison between participants with one alcoholic parent and controls remained significant (p = .02), as did the comparison between participants with two alcoholic parents versus one (p = .02).
Together, these results suggest that having two alcoholic parents is a unique risk factor for increased mother- and self-reported internalizing at age 13 over and above other parental diagnoses, but not consistently for rates of change in internalizing. Moreover, having even a single alcoholic parent was also uniquely related to self-, though not mother-, reported internalizing trajectories. The final model accounted for an additional 1.1, 5.1 and 3.1% of the variance over the baseline model in the intercept and slope factors for self-reported internalizing trajectories.
Models 3a and 3b: Internalizing growth model conditioned on subtypes of parental alcoholism
Next, we considered subtype differences in the form of parent alcoholism by first classifying each parent into one of four categories: no alcohol diagnosis (i.e., controls), an alcohol-only diagnosis (i.e., no comorbidity within the alcoholic parent for depression or ASP), comorbid alcohol and depression diagnosis without ASP (i.e., depressed subtype), or comorbid alcohol and ASP diagnosis (i.e., antisocial subtype).18 Because this analysis aimed to disaggregate heterogeneous types of parental alcoholism, parents with a depression or ASP diagnosis but not alcoholism were considered controls, thus providing a more conservative test of parent alcoholism risk more generally. Based on these categories for each parent’s alcoholism, we then classified each child into one of four groups: control (i.e., no alcoholic parents, mother-report n = 272, self-report n = 270), parent alcohol only (i.e., one or both parents have an alcohol diagnosis, but neither parent’s alcohol diagnosis is comorbid, mother-report n = 363, self-report n = 377), parent depressed subtype (at least one depressed subtype parent but neither parent antisocial subtype, mother-report n = 57, self-report n = 67), and parent ASP subtype (at least one parent antisocial subtype, mother- and self-report n = 119). To probe differences between these four groups of participants in internalizing trajectories, we created a set of contrast variables (model 3a) as well as a set of dummy variables (model 3b) that were included as predictors along with study, child gender, child ethnicity and parent education. Although these two coding comparisons elicit the same model fit, they test different sets of hypotheses comparing the parent alcoholism subtypes. Results for Models 3a and 3b are in Tables 5 (mother-reports) and 6 (self-reports).
Table 5.
LGM results testing effect of parent alcoholism subtypes on mother-report of internalizing trajectories
| Growth factor: | Intercept (age 13) | Slope age 2–7 | Slope age 7–17 | |||
|---|---|---|---|---|---|---|
| Covariate | b | se | b | se | b | se |
| Model 3a | ||||||
| Control vs. COA contrast | 0.06a | 0.02 | 0.00 | 0.01 | 0.01 | 0.00 |
| Alcohol-only vs. comorbid contrast | 0.11a | 0.03 | 0.00 | 0.01 | 0.01 | 0.01 |
| Depressed vs. ASP subtype contrast | 0.16c | 0.08 | 0.03 | 0.04 | 0.01 | 0.02 |
| Model 3b | ||||||
| Control vs. alcohol only | −0.04 | 0.06 | −0.01 | 0.03 | 0.00 | 0.01 |
| Depressed subtype vs. alcohol only | 0.49a | 0.15 | 0.03 | 0.05 | 0.02 | 0.02 |
| ASP subtype vs. alcohol only | 0.17d | 0.09 | −0.03 | 0.05 | 0.04 | 0.02 |
Note. N = 811. Effects of study, gender, ethnicity, and parent education are not in the table although they were covariates in each model.
p < .001,
p < .01,
p < .05,
p < .10.
Model 3a: Contrast codes
The contrast variables tested whether (1) trajectories for controls differed from those with alcoholic parents, regardless of subtype, (2) trajectories of those in the alcohol-only group differed from those with parents in the comorbid subtypes (combined), and (3) trajectories differed for those in the depressed versus antisocial subtype. Consistent with previous models, the contrast comparing controls with those in the three subtype groups was significantly associated with the intercept factor (p < .001), such that participants with an alcoholic parent had higher levels of internalizing than control participants. Additionally, the regression of the intercept factor on the contrast comparing participants in the alcohol-only subtype group with participants in the two comorbid subtype groups was significant (p < .001), such that age 13 internalizing scores were higher for participants in the comorbid groups than for participants in the alcohol-only groups. The final contrast was marginally associated with the intercept factor (p = .05), such that participants in the depressed subtype group had higher age 13 internalizing scores than participants in the ASP subtype group. Finally, none of the contrast variables was associated with either slope factor, nor were any contrast by study interaction terms associated with the growth factors.
For self-reports, the contrasts comparing controls with those in the three subtype groups was significantly associated with the intercept factor (p = .004). In addition, the contrast comparing those in the alcohol only subtype group with the comorbid subtype group was a marginally significant predictor of the intercept factor (p = .08) and of the first slope factor (p = .08), such that comorbid parental alcoholism was associated with higher levels of internalizing symptoms at age 13 and greater decreases in internalizing from age 10 to 14 relative to the alcohol-only group. In other words, the increased risk for internalizing symptoms associated with comorbid parent alcoholism that is apparent in early adolescence diminishes by late adolescence to levels consistent with that for the alcoholic-only subgroup. The final contrast code comparing the depressed subtype group with the ASP subtype group was not significantly related to either the intercept factor or the first slope factor. None of the contrast codes was significantly related to the second slope factor. Although these results show that parent alcoholism comorbidity is generally related to higher levels of internalizing, at least in early adolescence, they do not clearly indicate which of these two parent alcoholism subtypes differs from the alcohol-only subtype. Thus, we now turn to Model 3b to examine these relationships further.
Model 3b: Dummy codes
The dummy variables were defined such that the alcohol-only group was the reference group. For mother reports, the alcohol-only subtype group did not differ from controls. However, the regression of the intercept factor on the dummy code comparing the alcohol-only subtype with the depressed subtype was significant (p < .001). Specifically, participants in the depressed subtype group had higher age 13 internalizing scores than participants in the alcohol-only group. Similarly, participants in the ASP subtype group had higher age 13 internalizing scores than participants in the alcohol-only group, although this relationship was only marginally significant (p = .07). Consistent with Model 3a, analysis of these dummy codes did not suggest that the slope factors differed across the four groups, nor were dummy code by study interactions associated with the internalizing trajectories.
For self-reports, the dummy code comparing the alcohol-only subtype group with controls was significantly related to the intercept factor (p = .01), such that control participants had lower age 13 internalizing scores than participants who had an alcoholic parent without comorbidity. As with mother-reports, the dummy code comparing the alcohol-only subtype group with the depressed subtype was also significantly related to the internalizing intercept at age 13 (p = .03). Although no difference was found between the alcohol-only subtype and the ASP subtype group in predicting the intercept, marginally significant associations were found with the first (p = .07) and second (p = .06) slope factors. Specifically, the ASP subtype group had greater average decreases in internalizing from age 10 to 14 as well as greater average increases in internalizing from age 14 to 17 relative to the alcohol-only group. None of the remaining relationships between the dummy codes and the slope factors was significant.
Summary of Models 3a and 3b
Consistent with previous models, Models 3a and 3b suggest that parental alcoholism is predictive of the overall level of internalizing (specifically at age 13) and to some extent with rates of change in self-, though not mother-, reported internalizing. Across reporter, comorbidity impacted these relationships such that COA participants with a depressed parent consistently showed a greater risk for internalizing symptoms relative to COA participants whose parents did not report depression. Participants with antisocial alcoholic parents showed higher levels of mother-, though not self-, reported internalizing scores at age 13 and different patterns of change over time in self-, though not mother-, reported internalizing scores as compared to participants with alcoholic-only parents.
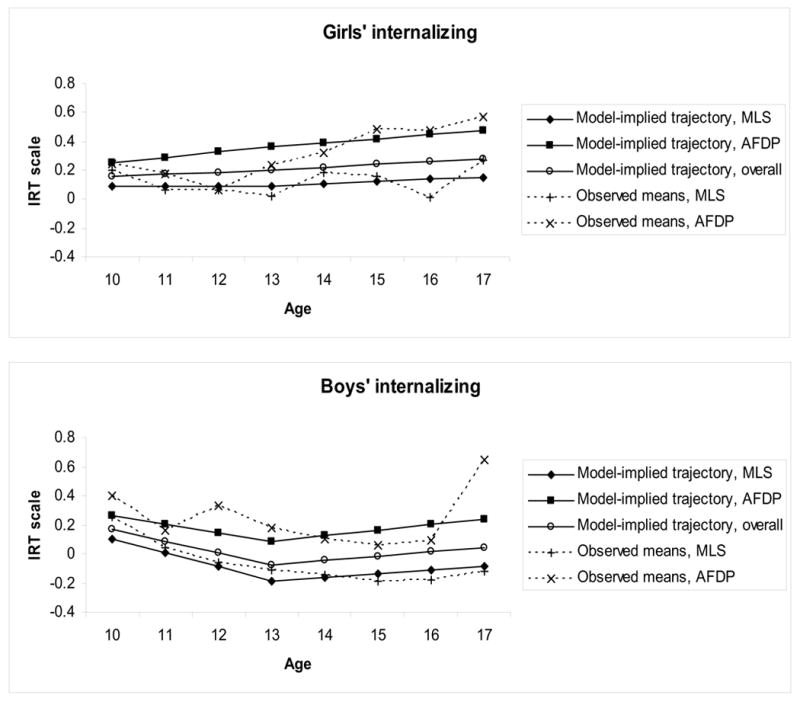
Model 4: Gender differences
This model extended Model 2 to examine whether child gender interacted with the relationship between parent alcoholism and internalizing trajectories when controlling for parent depression and ASP. Specifically, we added the interaction between child gender and (the dummy codes for) the number of alcoholic parents to Model 2. However, none of these interactions was significantly related to the mother-reported internalizing growth factors, indicating that the effects of parental alcoholism on internalizing trajectories for age 2 to 17 are not moderated by gender. For self-reported internalizing, gender significantly moderated the relationship between the dummy code for having two versus one alcoholic parent and the intercept factor (p = .004). Specifically, among girls, participants with two alcoholic parents had significantly higher age 13 internalizing scores than participants with one alcoholic parent (p < .001). Among boys, this comparison was not significant. No other significant interaction involving gender was found.
Discussion
The current study provides a rigorous empirical test of hypotheses based on data drawn from multiple studies, two reporters of child internalizing symptoms, and over an extended period of development. Results offer important qualifications to previous reports of increased internalizing symptomatology associated with parent alcoholism. Specifically, we replicated previous findings that parent alcoholism has a unique effect on child internalizing symptoms, above and beyond those of both parent depression and antisocial personality. However, we also found important subgroup differences, explaining heterogeneity within COAs’ risk profile in terms of the number of alcoholic parents in the family, comorbid diagnoses for the alcoholic parent and, for self-reported symptoms, child gender. Such factors serve to refine the definition of risk among COAs, suggesting a more severely impaired target group for preventive interventions, identifying the significance of familial alcoholism in individual differences underlying internalizing symptoms over time, and further specifying the distal risk matrix for an internalizing pathway to alcohol involvement.
Parent-based factors and COAs’ risk heterogeneity
Results of the current study underscore the conclusion that not all COAs are destined to manifest risk, in this case for internalizing symptoms, in childhood and adolescence. Rather, across reporters, studies, and observed ages, COAs’ risk for internalizing symptoms was significantly greater among participants with two alcoholic parents rather than among those with one alcoholic parents. In addition, this risk from having two alcoholic parents was significant above and beyond that presented by parental depression and antisociality. The findings regarding risk associated with having a single alcoholic parent differed by reporter of child internalizing symptoms. By mother-reports, having a single alcoholic parent conveyed no additional risk for children’s internalizing symptoms above and beyond the comorbid risk of parent depression. By child-reports, COAs with one alcoholic parent still showed greater risk for internalizing symptoms than those without an alcoholic parent, even when controlling for the effects of both parent depression and antisociality. Thus, the risk of having a single alcoholic parent differed by reporter but the risk of having two alcoholic parents, rather than one, was robust.
At least two mechanisms may account for the heightened risk for internalizing symptoms associated with having two alcoholic parents. First, having two affected parents reflects both a higher genetic and environmental risk load for children. With two alcoholic parents, children have an increased risk for genetic factors common to Major Depression and alcoholism that are also associated with depressed alcoholism (Zucker, 2006). However, transmission of genetic risk may also be an indirect influence on risk for internalizing symptoms. For example, Kendler et al. (2003) have shown risk for alcoholism and externalizing conditions (namely, antisocial behavior, conduct disorder and drug disorders) as distinct from that for internalizing disorders (namely, major depression and various anxiety disorders). Children with two alcoholic parents may be more likely to manifest a heightened genetic risk for disinhibitory disorders, especially given triggering environmental concomitants often evident within nested high risk contexts such as greater exposure to stress, violence and abuse (Cairns & Cairns, 1994). In turn, internalizing symptoms may follow as a secondary consequence as described by some psychosocial models of aggression and delinquent behavior (e.g., Davis, Sheeber & Hops, 2002). Even in the absence of disinhibitory behaviors, children with two alcoholic parents may simply experience greater internalizing symptoms via increased environmental risk, including more intense family conflict, marital aggression, and stress as well as greater impaired parenting due to the lack of a non-impaired parent.
Second, given the effects of assortative mating, maternal alcoholism often occurs in the presence of paternal alcoholism such that the risk of having two alcoholic parents becomes synonymous with that of maternal alcoholism. Thus, maternal alcoholism may be particularly detrimental for child internalizing problems due to the greater likelihood of impairment in the primary caretaker. Importantly, the risk for internalizing symptoms associated with having two alcoholic parents was not fully accounted for by parental depression and antisociality. Because families with two alcoholic parents may plausibly create familial contexts with more severe psychopathology more generally, this finding is important.
Parent psychopathology further delineated which COAs showed greatest risk for internalizing symptoms. Specifically, COAs whose alcoholic parent also had depression showed the greatest risk for internalizing symptoms, followed by those whose alcoholic parents also had ASP disorder (either with or without depression). Given that 21% of those families with antisocial alcoholics contained a parent with trimorbidities (i.e., alcoholism, ASP and depression) and 16% contained a second parent with depressive alcoholism, it may be surprising that children whose parents were of the antisocial alcoholism subtype were not at greater risk for internalizing than those whose parents were of the depressive alcoholism subtype. Moreover, children of antisocial alcoholics only showed marginally significant differences from those of alcoholic parents without comorbidities (at all ages in mother-reports, and only in late adolescence in self-reports). The presence of ASP in at least one alcoholic parent may confer greater genetic risk for disinhibitory disorders than for internalizing symptoms, thus changing how symptoms are manifested in these youth but perhaps not the level of risk they experience for problem outcomes more broadly.
These subtype analyses used a group comparison method to test for heterogeneity of risk among COAs. We chose this approach because we were interested in heterogeneity within COAs, rather than the effect of diagnoses across COAs and controls. As such, some of the control participants had parents who were diagnosed with depression (11%) or ASP (1%). This comparison thus speaks to the robust nature of the current findings. An alternative approach would be to test interactions between alcoholism and comorbid diagnoses, permitting control for the main effects of depression and ASP in testing for the multiplicative effect of alcoholism and these comorbid diagnoses. The interaction approach is appropriate for tests of moderation but is less practical where comorbid diagnoses form the predictors of interest, given the high correlation among the predictors (Cohen, Cohen, West, & Aiken, 2003). This was particularly true for testing the interactions between ASP and alcoholism as very few parents evidenced ASP without comorbid alcoholism (n=3).
Reporter differences in these risk factors were minimal, but we did find differences in the impact of parent alcoholism on child internalizing symptoms as a function of having one alcoholic parent versus none and of having an alcoholic parent with no comorbid psychopathology versus a non-alcoholic parent. In both cases, these effects were found for self-, but not for mother-, reported symptoms; thus more severe disturbance was necessary for group differences to emerge in mother-reports of child internalizing. This pattern of findings argues against a potential bias for mothers in alcoholic families to over-report child internalizing problems and may reflect the greater sensitivity of adolescents versus their mothers as reporters of internalizing conditions. However, it may also reflect some extent of reporting bias associated with maternal depression. Previous studies show that depressed mothers tend to overreport child symptomatology to some extent (Boyle & Pickles, 1997). In the current models, such a reporting bias could over-estimate the impact of maternal depression on mother-, though not self-, reported internalizing symptoms, resulting in inappropriately diminished effects of parent alcoholism.
However, differences between mother- and self-report results may also reflect differences in the children’s age spans in the two models (i.e., 2–17 years old in mother-reports and 10–17 years old in self-reports). Thus, some of these differences may be driven by effects pertaining to younger children, although little impact of parent alcoholism on change in internalizing symptoms over time was found. Future work that considers the time-varying impact of parent alcoholism on children’s internalizing symptoms is needed to further disaggregate these influences.
In sum, results suggest that risk for internalizing symptoms associated with parent alcoholism are largely conveyed within those families having two rather than one alcoholic parent or having a parent with a comorbid disorder, particularly depression. Further delineating risk in this manner suggests that families where COAS are more likely to manifest internalizing symptoms may have greater and broader genetic vulnerability as well as more chaotic environmental contexts than previously described.
Gender differences in internalizing symptoms
Gender differences in internalizing symptoms were largely consistent with previous studies showing their emergence with adolescence (e.g., Angold & Costello, 2001; Twenge & Nolen Hoeksema, 2002). Higher rates of mother-reported internalizing scores emerged between ages 13 and 15, largely guided by greater decreases in boys’ symptoms in early adolescence in the face of relatively stable levels of girls’ symptoms. Similarly, self-reported internalizing scores decreased in early adolescence for boys but remained relatively stable for girls, with gender differences emerging by age 13. However, these results of trajectory analyses of internalizing symptoms differ from the widely reported pattern of increasing rates of depression in girls but not boys with the onset of adolescence around age 12. The findings are consistent, however, with work by Angold et al. (1996) showing that reports of gender differences in adolescent depression are in part due to decreasing depression in boys. Other work has indicated that the increasing rates of depression in girls are less consistently found in studies of more broadly defined internalizing symptoms and rating scale versus diagnostic interview assessments (Angold & Costello, 2001; Compas et al., 1997), all of which are relevant to the current study.
Although gender failed to moderate the effects of parent alcoholism on mother-reported internalizing symptoms, gender differences were found in the relation between the number of alcoholic parents in a family and self-reported internalizing symptoms. Specifically, girls were at greater risk for internalizing symptoms if they had two alcoholic parents rather than one, whereas for boys no additional risk was found. Gender specificity in the risk for internalizing symptoms in such severe families may reflect a greater vulnerability to internalized forms of distress with the onset of adolescence in girls, such that boys and girls may experience similar risk for problem outcomes but the form of distress differs. Alternatively, such gender specificity might define a point of emergence for an internalizing pathway to alcoholism. Because parents with two alcoholic parents necessarily include an alcoholic mother, which is rare in one alcoholic parent families (i.e., due to assortative mating), and because women are more likely to show a depressed form of alcoholism, having two alcoholic parents rather than one may increase risk for depressed alcoholism specifically. If the developmental pathway to this form of alcoholism evidences gender differences similar to that of the adult form of depressed alcoholism, then a greater susceptibility for girls is to be expected. Thus, if early internalizing symptoms are a marker of risk for the development of later depressed alcoholism and if having two alcoholic parents does increase risk for the co-transmission of both depression and alcohol disorders, then greater internalizing symptoms in adolescent girls with two alcoholic parents may reflect gender differences in the initial emergence of depressed alcoholism, a pattern of gender differences that is commonly noted in studies of depressed alcoholism in adults.
Conclusions
Based on these findings, we conclude that heterogeneity in COAs’ risk for internalizing symptoms can meaningfully be related to the number of alcoholic parents in the family, the presence of comorbid psychopathology in the alcoholic parent, and the gender of the child. These factors were more often predictors of levels of internalizing symptoms as opposed to change over time. Rather than a limitation, this finding is important and indicates that these moderating effects on COAs’ risk are evident early and remain pervasive from childhood through adolescence. In short, these effects indicate that these at-risk COAs are on an elevated, stable trajectory for internalizing symptoms.
Our conclusions are strengthened by our use of an integrative or cross-study approach, which uses resources efficiently and directly tests for replication across studies, as well as by the rigor of the longitudinal investigations contributing to these analyses, adequate statistical power, and the consistency of our findings. However, these strengths are tempered by limitations in the complexity of our models, which focus on heterogeneity in risk as a primary step before delineating the process of risk manifestation, limited ethnic diversity to examine the generalizability of these findings, reliance on symptom checklists which may not relate directly to risk for disorder, and reliance on an assessment of internalizing symptoms that is unable to effectively distinguish between symptoms of depression and anxiety, limiting specificity (Graber, 2004). Future work is needed to further explore the limits of these findings and to examine the developmental and neurobiological processes that underlie the greater risk for internalizing symptoms found in these subsets of COAs. A more fine-grained understanding of these processes might also emerge were parental diagnosis to be treated as a time-varying covariate rather than as a lifetime attribute (Loukas, Zucker, Fitzgerald, & Krull, 2003).
Although an advantage in many ways, pooling samples across independent data collection efforts can introduce a number of complexities both in constructing appropriate cross-study measurement and in drawing appropriate inferences in hypothesis testing. When the data of interest are longitudinal, these complexities are multiplied. The combination of IRT and LCM permits an optimal approach to creating equivalent measurement across studies that in turn informs hypothesis testing of longitudinal associations. Although both techniques have been widely used in psychosocial research, their combination for purposes of cross-study analysis, or what McArdle and Horn (2002) term mega-analysis, is relatively novel. While having advantages in flexibility over traditional meta-analysis (Berlin, Santanna, Schmid, Szczech, & Feldman, 2002), such cross-study analyses do not overcome common controversies in longitudinal modeling (e.g., the extent of measurement invariance over time necessary to model longitudinal predictions, and the contributions of sampling bias in drawing inferences). Nonetheless, cross-study analyses represent a clear advance in developmental research by permitting the analysis of larger samples over longer periods of ontogeny.
In conclusion, the current study shows that COAs are a heterogeneous risk group, with some manifesting limited risk for internalizing symptoms over the early life course and others substantial and pervasive risk. This risk is independent of that conveyed solely by parent depression and antisociality, although it is heightened in the presence of these comorbid disorders, particularly depression. The extent to which internalizing symptoms and alcohol disorders travel together over time is informed by these findings by suggesting that the two emit from the same family context, with previous studies showing that the early emergence of internalizing symptoms as noted here is a predictor of adolescent alcohol involvement, particularly of problem use. Thus the current findings call for greater attention to risk processes that explain why children of depressed alcoholics and of parents with two alcoholic parents manifest such consistent risk for internalizing symptoms and what are the sequalae of such risk vis-à-vis later forms of adult alcoholism.
Table 6.
LGM results testing effect of parent alcoholism subtypes on self-reported internalizing trajectories
| Growth factor: | Intercept (age 13) | Slope age 10–14 | Slope age 14–17 | |||
|---|---|---|---|---|---|---|
| Covariate | b | se | b | se | b | se |
| Model 3a | ||||||
| Control vs. COA contrast | 0.06a | 0.02 | −0.01 | 0.01 | 0.00 | 0.01 |
| Alcohol-only vs. comorbid contrast | 0.04d | 0.02 | −0.02d | 0.01 | 0.02 | 0.01 |
| Depressed vs. ASP subtype contrast | −0.08 | 0.05 | −0.01 | 0.03 | 0.04 | 0.03 |
| Model 3b | ||||||
| Control vs. alcohol only | −0.15c | 0.06 | −0.03 | 0.03 | 0.04 | 0.03 |
| Depressed subtype vs. alcohol only | 0.20c | 0.09 | −0.06 | 0.06 | 0.01 | 0.05 |
| ASP subtype vs. alcohol only | −0.03 | 0.08 | −0.08d | 0.05 | 0.09d | 0.05 |
Note. N = 833. Effects of study, gender, ethnicity, and parent education are not in the table although they were covariates in each model.
p < .001,
p < .01,
p < .05,
p < .10.
Acknowledgments
This work was supported by grant R01 DA15398 to AMH, grant R37 AA 07065 to RAZ, grant R01 AA16213 to LAC, and grant R01 DA13148 to PJC. We also would like to thank the Centre for Addictions Research in British Columbia at the University of Victoria and the Reynolds Competitive Study Leave program for their support and to acknowledge the contributions of Michael Edwards, RJ Wirth and Daniel Serrano.
Footnotes
Although three year-olds were targeted as the lower bound for study recruitment, because of assessment scheduling issues, 6 boys were assessed shortly before their third birthday.
To test for effects of reporter differences due to sample membership, we re-analyzed a key model (model 3b) using only participants who were included in both the mother- and self-report analysis samples (N = 771). No substantive differences were found.
In all cases, the parent of interest is the biological parent, regardless of residence. Given the inability of the current study designs to parse environmental and genetic risk, we consider this index the most appropriate to the current questions of interest.
The availability of three sources of information collected over three different sessions, separated in some instances by as much as several months, served as an across method validity check on respondent replies. In cases of discrepant information, the data represented by the majority of information sources was used in establishing the diagnosis.
Previous studies have found a high degree of test-retest reliability using this method to diagnose alcoholism (98.8% agreement, Kappa=.95; Zimmerman, Coryell, Pfohl & Stangl, 1988) and excellent specificity (92%) and sensitivity (90%) for wives reporting on their husbands' substance abuse disorders (Kosten, Anton & Rounsaville, 1992).
Differences in the assessment window for this instrument are part of the study effect which was tested in all aspects of analyses.
We chose this age cut-off based on sample size constraints and previous research suggesting changes in the trajectories of internalizing symptoms, particularly gender differences in depression, that occur around this age (Angold & Costello, 2001). We would ideally test for age differences at every pair of adjacent ages, but given the sample size constraints, we chose to dichotomize age for these comparisons.
Because this procedure led to a large number of significance tests (one for each item), we applied the Benjamini-Hochberg procedure (Benjamini & Hochberg, 1995) to control the overall false discovery rate across multiple DIF tests, as recommended by Thissen (2001).
Because all participants in the AFDP were 10 years old or older, we removed observations from the MLS for participants younger than 10 years before testing study DIF in mother-reports.
If DIF testing indicated that an item had a significantly different severity parameter as a function of group membership (e.g., young vs. old) but the discrimination parameter did not significantly differ, we constrained the discrimination parameters of the corresponding sub-items to be equal.
We also fit a piecewise linear model with the linear pieces joined at age 11 and another model with the pieces joined at age 12 to permit gender differences in internalizing symptoms to emerge at these ages (Angold & Costello, 2001). By examining the correspondence between fitted trajectories and observed means, we determined that these models did not fit the data as well as the model with the two linear pieces joined at age 7.
However, we also fit models containing all possible study by covariate interactions to confirm that the absence of these terms did not substantially affect important substantive conclusions.
Although we did not find a gender difference in internalizing at age 13, the relationship between gender and the second slope factor implied that there are gender differences in internalizing at other ages. To evaluate this possibility, we also estimated growth models to probe whether covariate effects on the intercept factor were maintained at ages other than 13 (see Biesanz, Deeb-Sossa, Aubrecht, Bollen, & Curran, 2004). Specifically, we parameterized follow-up models with the intercept factor defined to represent level of internalizing in early childhood (age 3), preadolescence (age 10), and middle-adolescence (age 15). Gender was only significantly related to the age 15 intercept factor (p = .01), such that girls had higher levels of internalizing than boys.
We found no notable differences in interpretation when fitting this model to the full sample of N = 1026, thus minimizing concerns with bias due to attrition.
For both self- and mother-report data, we used the "OLStraj" SAS macro (Carrig, Wirth, & Curran, 2004) to explore the individual, child-level ordinary least-squares (OLS) trajectories for potential outlying observations with respect to both level of internalizing (OLS intercepts) and change (OLS slopes) over time. If an observation was outlying in box plots of these individual intercept and slope estimates, it was temporarily removed from the data set, and Model 2 was re-estimated. For both self- and mother-report, removal of these potentially influential observations (n = 5 for self-report and n = 9 for mother-report) led to trivial changes in all parameter estimates and did not affect any inferential conclusions.
When we reparameterized this model to probe developmental differences due to the prediction of the second slope factor by the dummy code of one versus two alcoholic parents, similar findings emerged for the prediction of the intercept factor at ages 3, 10 and 15.
Specifically, we probed whether age-specific relationships between parental depression and internalizing levels were maintained when the intercept was set at other ages. Parental depression was significantly associated with age 11 internalizing (p = .003), such that participants with a depressed parent had higher scores than those without a depressed parent. However, parental depression was not significantly related to age 17 internalizing (p = .50).
Parents with all three diagnoses were classified into the antisocial subtype because this group constituted a larger proportion of the ASP than depressive subgroups. This subtype is also one known for its substantial internalizing comorbidity (Babor, 1996). If these trimorbid cases are classified under the depressed subtype, internalizing risk for the ASP subgroup is similar to that of the alcohol only group, although with the self-report results, the age 13–17 slope difference between the alcohol-only group and the ASP subgroup remains significant (p = .02).
References
- Achenbach T, Edelbrock C. The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletn. 1981;85:1275–1301. [PubMed] [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Archives of General Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello E. The epidemiology of disorders of conduct: Nosological issues and comorbidity. In: Maughan B, Hill J, editors. Conduct disorders in childhood and adolescence. New York, NY, US: Cambridge University Press; 2001. pp. 126–168. [Google Scholar]
- Angold A, Erkanli A, Loeber R, Costello EJ, Van Kammen W, Stouthamer-Loeber M. Disappearing depression in a population sample of boys. Journal of Emotional and Behavioral Disorders. 1996;4:95–104. [Google Scholar]
- Arbuckle J. Full information estimation in the presence of incomplete data. In: Marcoulides G, Schumacker R, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Babor TF. The classification of alcoholics: Typology theories from the 19th century to the present. Alcohol Health and Research World. 1996;20:6–17. [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B. 1995;57:289–300. [Google Scholar]
- Berlin JA, Santanna J, Schmid CH, Szczech LA, Feldman HI. Individual patient- versus group-level data meta-regressions for the investigation of treatment effect modifiers: Ecological bias rears its ugly head. Statistics in Medicine. 2002;21:371–387. doi: 10.1002/sim.1023. [DOI] [PubMed] [Google Scholar]
- Biesanz JC, Deeb-Sossa N, Aubrecht AM, Bollen KA, Curran PJ. The role of coding time in estimating and interpreting growth curve models. Psychological Methods. 2004;9:30–52. doi: 10.1037/1082-989X.9.1.30. [DOI] [PubMed] [Google Scholar]
- Bingham CR, Fitzgerald WW, Fitzgerald HE, Zucker RA. Prenatal history, parental alcoholism, and the development of preschool aged sons of alcoholics (Abstract) Alcoholism: Clinical and Experimental Research. 1996;20:469. [Google Scholar]
- Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Approach. New York: Wiley & Sons; 2005. [Google Scholar]
- Boye-Beaman J, Leonard KE, Senchak M. Assortative mating, relationship development, and intimacy among offspring of alcoholics. Family Dynamics of Addiction Quarterly. 1991;1:20–33. [Google Scholar]
- Boyle MH, Pickles A. Maternal depressive symptoms and ratings of emotional disorder symptoms in children and adolescents. Journal of Child Psychology and Psychiatry. 1997;38:981–992. doi: 10.1111/j.1469-7610.1997.tb01615.x. [DOI] [PubMed] [Google Scholar]
- Cairns RB, Cairns BD. Lifelines and risks: Pathways of youth in our time. New York: Cambridge University Press; 1994. [Google Scholar]
- Carrig M, Wirth RJ, Curran PJ. A SAS Macro for Estimating and Visualizing Individual Growth Curves. Structural Equation Modeling: An Interdisciplinary Journal. 2004;11:132–149. [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Chassin L, Barrera M, Jr, Bech K, Kossak-Fuller J. Recruiting a community sample of adolescent children of alcoholics: A comparison of three subject sources. Journal of Studies on Alcohol. 1992;53:316–319. doi: 10.15288/jsa.1992.53.316. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pillow DR, Curran PJ, Molina BS. Relation of parental alcoholism to early adolescent substance use: A test of three mediating mechanisms. Journal of Abnormal Psychology. 1993;102:3–19. doi: 10.1037//0021-843x.102.1.3. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomatology among adolescent children of alcoholics. Journal of Abnormal Psychology. 1991;100:449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SJ, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Compas BE, Oppedisano G, Connor JK, Gerhardt CA, Hinden BR, Achenbach TM. Gender differences in depressive symptoms in adolescence: Comparison of national samples of clinically referred and nonreferred youths. Journal of Consulting & Clinical Psychology. 1997;65:617–626. doi: 10.1037//0022-006x.65.4.617. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A. Development and Epidemiology. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. 2. Hoboken, NJ: Wiley & Sons; 2006. pp. 41–75. Edition, Volume One: Theory and Method. [Google Scholar]
- Costello E, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Chassin L. A longitudinal study of parenting as a protective factor for children of alcoholics. Journal of Studies on Alcohol. 1996;57:305–313. doi: 10.15288/jsa.1996.57.305. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Edwards MC, Wirth RJ, Hussong AM, Chassin L. The application of categorical measurement models in the analysis of individual growth. In: Little TD, Bovaird J, Marquis J, editors. Modeling developmental processes in ecological context. Mahwah, NJ: Erlbaum; in press. [Google Scholar]
- Davis B, Sheeber L, Hops H. Coercive family processes and adolescent depression. In: Patterson GR, Reid JB, editors. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. Washington DC: American Psychological Association; 2002. pp. 173–192. [Google Scholar]
- DuRocher TD, Cummings EM. Parental dysphoria and children's internalizing symptoms: Marital conflict styles as mediators of risk. Child Development. 2006;74:1663–1681. doi: 10.1046/j.1467-8624.2003.00630.x. [DOI] [PubMed] [Google Scholar]
- Edwards EP, Leonard KE, Eiden RD. Temperament and behavioral problems among infants in alcoholic families. Infant Mental Health Journal. 2001;22:374–392. doi: 10.1002/imhj.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embretson SE, Reise SP. Item response theory for psychologists. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RA, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Archives of General Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Fitzgerald HE, Sullivan LA, Ham HP, Zucker RA, Bruckel S, Schneider AM, et al. Predictors of behavior problems in three-year-old sons of alcoholics: early evidence for the onset of risk. Child Development. 1993;64:110–123. doi: 10.1111/j.1467-8624.1993.tb02898.x. [DOI] [PubMed] [Google Scholar]
- Fitzgerald HE, Zucker RA, Yang HY. Developmental systems theory and alcoholism: Analyzing patterns of variation in high-risk families. Psychology of Addictive Behaviors. 1995;9:8–22. [Google Scholar]
- Ge X, Lorenz FL, Conger RD, Elder GH, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology. 1994;30:467–483. [Google Scholar]
- Graber J. Internalizing problems during adolescence. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. Hoboken, NJ: Wiley & Sons; 2004. pp. 587–626. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou S, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Chassin L. Stress and coping among children of alcoholic parents through the young adult transition. Development and Psychopathology. 2004;16:985–1006. doi: 10.1017/s0954579404040106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Zucker RA, Wong MM, Fitzgerald HE, Puttler LI. Social Competence in Children of Alcoholic Parents Over Time. Developmental Psychology. 2005;41:747–759. doi: 10.1037/0012-1649.41.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Leonard K. Psychosocial functioning in children of alcoholic fathers, depressed fathers and control fathers. Journal of Studies on Alcohol. 1986;47:373–380. doi: 10.15288/jsa.1986.47.373. [DOI] [PubMed] [Google Scholar]
- Jansen RE, Fitzgerald HE, Ham HP, Zucker RA. Pathways into risk: Temperament and behavior problems in three- to five- year old sons of alcoholics. Alcoholism: Clinical and Experimental Research. 1995;25:835–843. doi: 10.1111/j.1530-0277.1995.tb01538.x. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Deering CG, Racusin GR. Depressed children and their families. Clinical Psychology Review. 1994;14:39–59. [Google Scholar]
- Kellam SG, Ensminger ME, Simon MB. Mental health in first grade and teenage drug, alcohol and cigarette use. Drug and Alcohol Dependence. 1980;5:273–304. doi: 10.1016/0376-8716(80)90003-4. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Heath AC, Kessler RC, Eaves LJ. A twin-family study of alcoholism in women. American Journal of Psychiatry. 1994;15:707–715. doi: 10.1176/ajp.151.5.707. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Khoo ST, West SG, Wu W, Kwok OM. Longitudinal methods. In: Eid M, Diener E, editors. Handbook of multimethod measurement in psychology. Washington, DC: American Psychological Association; 2006. pp. 301–317. [Google Scholar]
- Kim HK, Capaldi DM, Stoolmiller M. Depressive symptoms across adolescence and young adulthood in men: Predictions from parental and contextual risk factors. Development and Psychopathology. 2003;15:469–495. doi: 10.1017/s0954579403000257. [DOI] [PubMed] [Google Scholar]
- Kosten TA, Anton SF, Rounsaville BJ. Ascertaining Psychiatric Diagnoses with the Family History Method in a Substance-Abuse Population. Journal of Psychiatric Research. 1992;26:135–147. doi: 10.1016/0022-3956(92)90005-9. [DOI] [PubMed] [Google Scholar]
- Loukas A, Piejak LA, Bingham CR, Fitzgerald HE, Zucker RA. Parental distress as a mediator of problem behaviors in sons of alcohol-involved families. Family Relations. 2001;50:293–301. [Google Scholar]
- Loukas A, Zucker RA, Fitzgerald HE, Krull JL. Developmental trajectories of disruptive behavior problems among sons of alcoholics: Effects of parent psychopathology, family conflict, and child undercontrol. Journal of Abnormal Psychology. 2003;112:119–131. [PubMed] [Google Scholar]
- Maes HHM, Neale MC, Kendler KS, Hewitt JK, Silberg JL, Foley DL, et al. Assortative mating for major psychiatric diagnoses in two population-based samples. Psychological Medicine. 1998;28:1389–1401. doi: 10.1017/s0033291798007326. [DOI] [PubMed] [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. American Journal of Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- McArdle JJ. Dynamic but structural equation modeling of repeated measures data. In: Cattell RB, Nesselroade JR, editors. Handbook of multivariate experimental psychology. 2. New York: Plenum Press; 1988. pp. 561–614. [Google Scholar]
- McArdle JJ, Horn JL. The benefits and limitations of mega-analysis with illustrations for the WAIS; International meeting of CODATA; Montreal, QE. October, 2002.2002. [Google Scholar]
- Mehta PD, West SG. Putting the individual back into individual growth curves. Psychological Methods. 2000;5:23–43. doi: 10.1037/1082-989x.5.1.23. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Leckman JF, Prusoff BA, Pauls DL, Weissman MM. Familial transmission of depression and alcoholism. Archives of General Psychiatry. 1985;42:367–372. doi: 10.1001/archpsyc.1985.01790270057006. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Muthén & Muthén; 2004. [Google Scholar]
- Muthén BO, Satorra A. Complex sample data in structural equation modeling. In: Marsden P, editor. Sociological Methodology. Washington DC: American Sociological Association; 1995. pp. 267–316. [Google Scholar]
- Noll RB, Zucker RA, Fitzgerald HE, Curtis WJ. Cognitive and motoric functioning of sons of alcoholic fathers and controls: The early childhood years. Developmental Psychology. 1992;28(4):665–675. [Google Scholar]
- Preisig M, Fenton BT, Stevens DE, Merikangas KR. Familial relationship between mood disorders and alcoholism. Comprehensive Psychiatry. 2001;42:87–95. doi: 10.1053/comp.2001.21221. [DOI] [PubMed] [Google Scholar]
- Puttler LI, Zucker RA, Fitzgerald HE, Bingham C. Behavioral outcomes among children of alcoholics during the early and middle childhood years: Familial subtype variations. Alcoholism: Clinical and Experimental Research. 1998;22:1962–1972. [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. The NIMH Diagnostic Interview Schedule: Its History, Characteristics and Validity. St. Louis, MO: Washington University School of Medicine; 1980. [Google Scholar]
- Selzer ML, Vinokur A, van Rooijan L. A self-administered short Michigan Alcoholism Screening Test (SMAST) Journal of Studies on Alcohol. 1975;36:117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- Sher KJ. Children of alcoholics: A critical appraisal of theory and research. Psychology of Addictive Behaviors. 1993;7:201–202. [Google Scholar]
- Sokol RJ, Claren SK. Guidelines for use of terminology describing the impact of prenatal alcohol on the offspring. Alcoholism: Clinical and Experimental Research. 1989;13:597–598. doi: 10.1111/j.1530-0277.1989.tb00384.x. [DOI] [PubMed] [Google Scholar]
- Thissen D. Computer software. Chapel Hill, NC: L.L. Thurstone Psychometric Laboratory; 2001. IRTLRDIF v. 2.01b: Software for the computation of the statistics involved in item response theory likelihood-ratio tests for differential item functioning. [Google Scholar]
- Thissen D. Computer Software. Chicago, IL: Scientific Software; 1991. MULTILOG user's guide: Multiple, categorical item analysis and test scoring using item response theory. [Google Scholar]
- Thissen D, Orlando M. Item response theory for items scored in two categories. In: Wainer H, Thissen D, editors. Test scoring. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. pp. 73–140. [Google Scholar]
- Thissen D, Steinberg L, Wainer H. Detection of differential item functioning using the parameters of item response models. In: Wainer H, Holland P, editors. Differential item functioning. Hillsdale, NJ: Lawrence Erlbaum Associates; 1993. pp. 67–113. [Google Scholar]
- Tubman JG. Family Risk-Factors, Parental Alcohol-Use, and Problem Behaviors among School-Age-Children. Family Relations. 1993;42:81–86. [Google Scholar]
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, SES, and birth cohort differences on the Children’s Depression Inventory: A meta-analysis. Journal of Abnormal Psychology. 2002;111:578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- Werner EE. Resilient offspring of alcoholics: A longitudinal study from birth to age 18. Journal of Studies on Alcohol. 1986;47:34–40. doi: 10.15288/jsa.1986.47.34. [DOI] [PubMed] [Google Scholar]
- Wichstrom L. The emergence of gender difference in depressed mood during adolescence: The role of intensified gender socialization. Developmental Psychology. 1999;35:232–245. [PubMed] [Google Scholar]
- Wingersky MS, Lord FM. An investigation of methods for reducing sampling error in certain IRT procedures. Applied Psychological Measurement. 1984;8:347–364. [Google Scholar]
- Wong M, Zucker R, Puttler L, Fitzgerald H. Heterogeneity of risk aggregation for alcohol problems between early and middle childhood: Nesting structure variations. Development and Psychopathology. 1999;11:727–744. doi: 10.1017/s0954579499002291. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Coryell W, Pfohl B, Stangl D. The Reliability of the Family History Method for Psychiatric Diagnoses. Archives of General Psychiatry. 1988;45:320–322. doi: 10.1001/archpsyc.1988.01800280030004. [DOI] [PubMed] [Google Scholar]
- Zucker RA. Alcohol use and alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. 2. Vol. 3. Hoboken, NJ: Wiley & Sons; 2006. pp. 620–656. Risk, Disorder and Adaptation. [Google Scholar]
- Zucker RA, Chermack ST, Curran GM. Alcoholism: A lifespan of etiology and course. In: Sameroff A, Lewis M, Miller S, editors. Handbook of developmental psychoapthology. 2. New York: Plenum Press; 2000. pp. 569–587. [Google Scholar]
- Zucker RA, Ellis DA, Bingham CR, Fitzgerald HE. The Development of Alcoholic Subtypes: Risk Variation Among Alcoholic Families During the Early Childhood Years. Alcohol Health and Research World. 1996;20:46–55. [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Ellis DA, Fitzgerald HE, Bingham CR, Sanford K. Other evidence for at least two alcoholisms, II: Life course variation in antisociality and heterogeneity of alcoholic outcome. Development and Psychopathology. 1996;8:831–838. [Google Scholar]
- Zucker RA, Fitzgerald H, Noll RB. Unpublished manuscript, East Lansing. Rev. 1990. Drinking and drug history. version 4. [Google Scholar]
- Zucker RA, Fitzgerald HE, Refior SK, Puttler LI, Pallas DM, Ellis DA. The clinical and social ecology of childhood for children of alcoholics: Description of a study and implications for a differentiated social policy. In: Fitzgerald HE, Lester BM, Zuckerman BS, editors. Children of addiction: Research, health and policy issues. New York: Garland Press; 2000. pp. 174–222. [Google Scholar]


