Disease detection
The 1st anthrax case of the 2006 outbreak in Saskatchewan occurred on June 26th in the east-central area of the province near the town of Melfort. This case involved an 8-year-old cow that was found dead; anthrax was confirmed as the cause of death by the Canadian Food Inspection Agency (CFIA) Lethbridge Laboratory (OIE Reference Laboratory for Anthrax) on July 4th. After the premises had been declared infected and put under quarantine on July 3rd, 6 additional cattle and 1 pig died there.
Additional cases
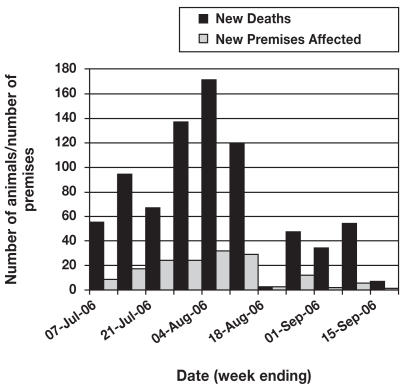
The outbreak continued over the course of the summer and affected a number of animals of several different species on multiple premises. The peak in new deaths and new premises affected occurred in early August, as shown in Figure 1.
Figure 1.
Number of new deaths and new premises affected during the 2006 anthrax outbreak in Saskatchewan.
The last declaration of a new infected premises (a premises on which an animal had died of anthrax that had not previously had any other cases of the disease) occurred on September 6th, near the town of Raymore in east-central Saskatchewan. The last mortality due to anthrax occurred on September 21st (on a premises that had previously experienced other cases of anthrax). In total, 804 livestock deaths were recorded by the CFIA, including 493 cattle, 254 bison, 6 horses, 33 sheep, 13 cervids (white-tailed deer and elk), 3 pigs, and 2 goats.
Outbreak location
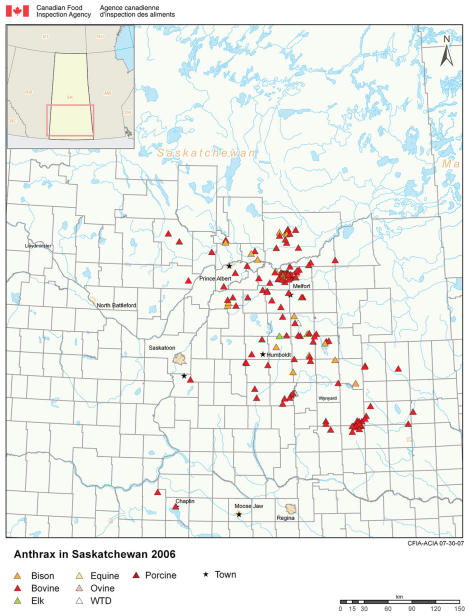
In total, 153 premises were affected in 43 rural municipalities (RMs), as illustrated in Figure 2. Almost all of the anthrax cases took place in 40 of these RMs, which are contiguous and located in the east-central area of the province. The remaining 3 municipalities accounted for 3 infected premises, with 1 in each of the Saskatoon, Swift Current, and Moose Jaw areas. These RMs are in the central and southwest regions of the province and are noncontiguous with the main outbreak area. They had experienced environmental conditions that were dissimilar to those in the east-central RMs. These cases are probably representative of the “normal” occurrence of anthrax in the province (cases of anthrax that may have occurred annually but were only detected in 2006 because of heightened public awareness of the disease) and may not have been associated with the main outbreak.
Figure 2.
Locations of anthrax infected premises during the 2006 anthrax outbreak in Saskatchewan.
Predisposing factors
Anthrax is not a traditionally contagious disease (transmitted directly between animals); rather, it is caused by contact with the anthrax-causing bacterial spores in the environment, primarily through soil ingestion during grazing. Environmental factors, such as precipitation and temperature, play an important role in the number and concentration of exposed spores, thus strongly influencing the probability and location of an outbreak. In the case of the 2006 outbreak in Saskatchewan, the east-central area of the province had experienced extremely wet conditions, with higher than average falls of rain and snow since the fall of 2005. In the Melfort area, near the center of the outbreak, the total precipitation from September 2005 to May 2006 was approximately 296.6 mm, compared with an average of approximately 132.8 mm for the same time period over the preceding 5 y (1). This was followed by a hot, dry summer in 2006. These meteorological conditions may have been associated with the occurrence of anthrax. One could speculate that the excess precipitation served to “flush” spores from deep within the ground to the surface of the soil and then to concentrate them as standing water began to evaporate, thus resulting in increased animal exposure to spores.
Response
The CFIA used a 3-part program to control the anthrax outbreak in 2006, consisting of quarantine, vaccination, and proper carcass handling and disposal.
All premises (as outlined by their land locations — 1/4 section, township, range, and meridian) where an animal had died of anthrax were declared infected and put under quarantine. This restricted the movement of susceptible animals on and off those premises in an attempt to contain the disease. Vaccination was ordered by the CFIA for all susceptible animals on infected premises, except for those species for which the vaccine did not have a label claim (for example, bison and cervids), in which case animals were vaccinated at the discretion of the owner. Vaccination against anthrax was recommended, but not mandatory, for all susceptible animals (cattle, bison, sheep, goats, cervids, horses) within the outbreak area. Lastly, and perhaps most importantly, the CFIA stressed the need for proper carcass management and provided information to producers and veterinarians on how this could be achieved.
Since the carcass of an animal that has died of anthrax has the ability to produce a tremendous number of infectious spores, appropriate carcass handling is key to minimizing environmental anthrax contamination and reducing the risk to animals grazing in the same area in the future. In the Saskatchewan 2006 anthrax outbreak, several aspects of carcass management were considered. They included reducing carcass movement, covering carcasses or coating them with substances such as formaldehyde to deter scavengers and other possible mechanical vectors of spore dissemination (flies), and covering carcass heads and plugging body orifices in order to minimize leakage of spore-laden body fluids from carcasses. Most carcasses were promptly disposed of, using incineration, deep burial, or both. Figure 3 shows incineration of carcasses, using a burn pit.
Figure 3.
Carcass disposal using a burn pit.
Recovery
Quarantine was removed from a premises 21 d after the last anthrax mortality, or 21 d after vaccination of all susceptible animals on the premises, whichever was later. In cases where animals on anthrax-positive premises could not be vaccinated, quarantine was not removed until late November, when a combination of frozen ground and snow cover made it virtually impossible for animals to come into contact with anthrax spores though grazing activity. All quarantines were officially removed by November 24th, 2006.
Indemnity was awarded for each animal that was determined to have died of anthrax during the outbreak to encourage reporting of anthrax cases and offset the cost of disposal.
In order to avert a future outbreak, annual revaccination against anthrax is recommended for all susceptible animals in the 2006 outbreak area for at least the next 3 y.
Footnotes
Reprints will not be available from the authors.
Reference
- 1.National Climate Data and Information Archive [database on the Internet] Ottawa: Environment Canada c; 2006. [Last accessed 20/07/07]. Available from http://www.climate.weatheroffice.ec.gc.ca/Welcome_e.html. [Google Scholar]