Abstract
Background
Postnatal depression is a serious mental health problem that may be reduced by exercise.
Aim
This study examined the feasibility of an exercise intervention for women with postnatal depression, and assessed which methods of recruitment are most effective.
Design of study
Randomised controlled trial.
Setting
General practice and the community.
Method
Participants were recruited from various sources and randomised to an exercise intervention or usual care with follow-up at 12 weeks. As well as assessing feasibility, other trial outcomes included exercise participation and self-efficacy for exercise. Levels of depression were assessed but the study was not powered to show a difference in this.
Results
The recruitment rate of eligible patients was 23.1%. The highest recruitment rate was via referral from the psychiatric mother and baby unit (9/28; 32.1%), followed by invitation letters from GPs (24/93; 25.8%). Thirty-eight eligible participants were randomised. At follow-up there was no significant difference in exercise participation between groups. The intervention group reported significantly higher self-efficacy for exercise compared to usual care, but depression scores did not differ.
Conclusion
Exercise participation over the 12-week period was not significantly increased, possibly because it is difficult to motivate women with postnatal depression to exercise, or the intervention was not sufficiently intensive. Eligible patients were recruited into this study but response rates were low. Optimum methods of recruitment in this difficult-to-reach population are required prior to a substantive trial. Further research is imperative given poorly-evidenced recommendations by the National Institute for Health and Clinical Excellence to consider this treatment.
Keywords: exercise, postnatal depression, women
INTRODUCTION
Postnatal depression is a serious mental health problem,1 affecting around one in 10 women at some time in the first year.2,3 As well as the morbidity suffered by the mother, studies have found an association between postnatal depression and adverse effects on the child.4,5 Consideration of novel adjunctive interventions for the treatment of postnatal depression is required, given that some women are reluctant to take antidepressants after giving birth,6 and there is limited availability of psychological therapies. Meta-analyses have concluded that exercise may be effective in reducing depression in general populations.7,8 A recent review identified two small randomised controlled trials which examined the effects of exercise on postnatal depression;9–11 both trials reported substantial reductions in postnatal depression scores in participants randomised to receive interventions involving pram pushing. However, the very small samples in these studies limit their validity. Both trials, by the same team, were conducted in the Gold Coast, Australia where the year-round warm weather conditions are likely to have positively influenced mothers' decisions to take part;10,11 thus contextual factors decrease the applicability of these findings to other settings.
Despite the limited evidence in postnatal women,9 the National Institute for Health and Clinical Excellence (NICE) recently recommended in their antenatal and postnatal mental health guidelines that health professionals should consider exercise as a management strategy in women experiencing mild-to-moderate depression.12 Further research into this issue is required in representative settings.
Limited information has been provided by previous study reports about how participants were accessed or recruited. Prior to any substantive trial, it is important to consider the merits of different methods of identifying cases. Once eligible patients have been recruited to an exercise programme, the demands of a new baby may then make regular exercise participation difficult. Therefore, this study investigated the feasibility and acceptability of an exercise intervention in women with postnatal depression.
METHOD
Participant eligibility
Women aged 16 years or more who were experiencing depression, and whose youngest child was less than 12 months' old were eligible. Participants could continue with prescribed medications and any counselling/behavioural treatments, but had to speak English because of lack of interpretation services. Women with severe postnatal depression who required inpatient psychiatric treatment, had psychotic symptoms, or were known to be pregnant were excluded.
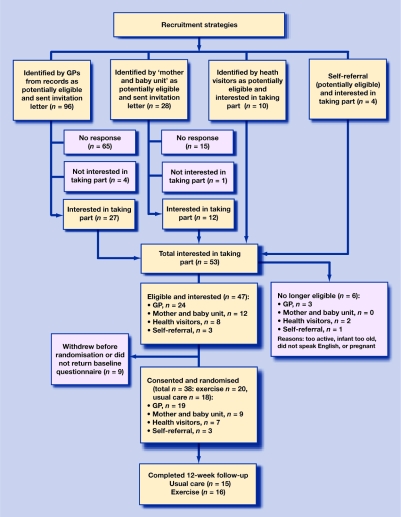
A further eligibility check of these criteria was made by the researchers prior to consent, as well as screening for current activity to exclude women who were already active (defined as exercise three or more times per week for at least 30 minutes per session, for more than 3 months) or those who were unable to provide written informed consent (Figure 1).
Recruitment
To assess the feasibility of a variety of recruitment strategies, cases were identified through four different routes. All general practices within four primary care trusts in Birmingham were informed by letter about the aims of the study. They were invited to assist with recruitment by identifying potentially eligible patients according to trial inclusion criteria. The local specialist mother and baby unit was asked to do the same. General practices and the mother and baby unit then sent invitation letters to eligible women and asked them to contact the trial team if they were interested in participating. Presentations about the trial were made to health visitors in each of the primary care trusts, and they were asked to refer eligible women. Support groups were visited and asked to inform women about the trial so they could self-refer.
How this fits in
Postnatal depression is a serious and common mental health problem. Evidence from depressed general populations has shown that exercise may be effective in reducing depressive symptomatology, but there is inadequate evidence on this in relation to women with postnatal depression. The current study investigated the feasibility and acceptability of an exercise intervention in this population. It illustrates that postnatal women are difficult to access and recruit. The intervention was successful in increasing self-efficacy for exercise, but exercise participation and levels of depression did not differ at follow-up.
Depression was identified using clinical judgement by GPs, psychiatrists, and health visitors, but women recruited by self-referral were screened and had to have a score >12 on the Edinburgh Postnatal Depression Scale (EPDS)13 to be eligible.
Randomisation
After the completion of their baseline assessment, participants were randomised to the exercise intervention group or usual care, according to a computer-generated random list provided by an independent statistician.
Outcomes
Information relating to each method of recruitment was systematically documented. The Godin Leisure-Time Exercise Questionnaire was used to assess participants' levels of involvement in mild, moderate, and vigorous exercise.14 A self-efficacy for exercise questionnaire was used to assess participants' confidence in being active in different situations (for example, when tired, in a bad mood, or when lacking time).15 Members of the exercise group were asked to complete a checklist exercise diary to record the amount of time in minutes of exercise they achieved each day. Levels of depression using the EPDS were obtained,13 but the study was not powered to show a difference in this outcome.
Additional information
Demographic data, current medication, and items relating to participants' health behaviours, including breastfeeding, were collected. If participants were receiving counselling or taking any prescribed medication this was documented, including data regarding participants' exercise history. A social support score was calculated based on women's responses to five items: the amount of help they receive from their partner; the availability of a friend or relative to contact if needed; a local contact who has an infant; the availability of practical help at home; and the duration of residence in the locality.16
Those randomised to the exercise intervention completed a series of open-ended questions about their experiences during the intervention. Participants were offered the opportunity to return these evaluations anonymously.
Assessment of outcomes
All outcomes were assessed at baseline and 12 weeks after the end of exercise intervention using the postal questionnaire at each time point, and with reminders sent to non-responders after 2 weeks.
Exercise intervention
Participants in the intervention group were offered two one-to-one exercise consultations over the 12-week intervention period. Further information regarding the theoretical basis of the intervention and the intervention approach used can be found elsewhere.17 The intervention aimed to equip individuals with the skills, knowledge, and confidence needed to participate in regular exercise, and was delivered in participants' homes by a trained researcher. Consultations lasted about 1 hour.
The first consultation focused on uptake of exercise and enhancing motivation, self-efficacy for exercise, overcoming barriers, and developing appropriate activity goals. Participants were also given a pedometer. A short ‘walk and talk’ pram-pushing session was incorporated within the first consultation so that practical issues, such as perceived exertion monitoring and exercise safety, could be explored with participants.
Four weeks later, a second consultation focused on the prevention of relapse back to sedentary behaviour and/or improving maintenance of an active lifestyle. Follow-up support phone calls lasting about 10 minutes were given during weeks 3 and 9, where any persistent barriers or issues preventing behavioural change were discussed.
The behavioural goal was for women to work towards accumulating participation in moderate-intensity activities for at least 30 minutes per day, five days of the week. Walking in the form of ‘pram pushing’ was advocated and, when appropriate, opportunities for women to exercise without their baby were discussed.
Usual care
Members of the usual care group were asked not to change their current exercise patterns but were offered an exercise consultation at the end of their involvement in the study.
Sample size and analysis plan
The primary outcome was the frequency of moderate-intensity exercise per week. The Department of Health recommends at least 30 minutes of moderate-intensity physical activity per day for at least 5 days per week (minimum total of 150 minutes per week) for the general population.18 This study expected women to achieve 70% (105 minutes) of this target, and the sample was sufficient to estimate weekly exercise with 14% precision (95% confidence level). Analyses of covariance (controlling for baseline scores) were used to compare outcomes between groups at 12-weeks' follow-up. Data were analysed on an intention-to-treat basis.
RESULTS
Recruitment of general practices
Of 262 practices invited to assist with study recruitment, 56 (21%) agreed, 67 (26%) declined, and 139 (53.1%) did not respond. Of those practices that agreed (n = 56), three later withdrew, 18 provided no patient lists when requested, and 10 reported no eligible patients at the time of the study; thus 25/262 (9.5%) practices provided lists of eligible patients.
Patient recruitment
Recruitment took place between October 2005 and May 2006. Fifty-three women expressed an interest in taking part, of whom 27 (51%) were identified from general practice records, 12 (23%) by the specialist mother and baby unit, 10 (19%) from health visitor referral, and four (8%) self-referred. A higher proportion of women responded to an invitation from the mother and baby unit (12/28; 42.9%) than their GP (27/96; 28.1%). Six women were subsequently found to be ineligible, and nine withdrew prior to randomisation or did not return the baseline questionnaire, leaving 38 eligible patients who were randomised (recruitment rate 4–5 patients per month). Denominator data were only available for GPs (n = 96) and the mother and baby unit (n = 28). Trial recruitment from these sources was 23.1% (28/121; 124 potentially eligible minus three screened as further ineligible; Figure 1).
Characteristics of randomised participants
Most participants were aged between 29 and 31 years, had one or two children, lived with their husband/partner, and were not currently breastfeeding their infant. Most participants were employed, taking antidepressants, had low levels of social support, and lived in more deprived communities (Table 1). A total of 26.3% of the sample were of non-white ethnicity. At baseline, 33 of the 38 participants (exercise group, n = 17; usual care, n = 16) recorded an EPDS score >12, and in 4 of the 38 participants the EPDS score was 12 (exercise group, n = 2; usual care, n = 2).
Table 1.
Baseline demographic characteristics of participants by study group.
| Characteristic | Usual care (n = 18), n (%) | Exercise (n = 20), n (%) |
|---|---|---|
| Age, years | ||
| 21–30 | 10 (55.5) | 10 (50.0) |
| 31–40 | 8 (44.5) | 9 (45.0) |
| >40 | 0 | 1 (5.0) |
| Body mass index | ||
| Under/normal weight (≤25) | 11 (61.1) | 10 (50.0) |
| Overweight (>25 to ≤30) | 4 (22.2) | 7 (35.0) |
| Obese (>30 to ≤40) | 1 (5.6) | 3 (15.0) |
| Ethnicity | ||
| White | 12 (66.6) | 16 (80) |
| Parity | ||
| 1–2 | 12 (66.6) | 16 (80) |
| 3–4 | 6 (33.3) | 4 (20) |
| Index of Multiple Deprivation | ||
| Quartile 1 — least deprived | 1 (5.5) | 1 (5.0) |
| Quartile 2 | 1 (5.5) | 1 (5.0) |
| Quartile 3 | 7 (38.9) | 4 (20.0) |
| Quartile 4 — most deprived | 8 (44.4) | 12 (60.0) |
| Married/with partner | 16 (88.9) | 13 (65.0) |
| Employment status | ||
| Paid employment | 11 (61.1) | 15 (75.0) |
| Unemployed | 3 (16.7) | 1 (5.0) |
| Looking after family/home | 3 (16.7) | 3 (15.0) |
| Sick disabled | 0 | 1 (5.0) |
| Other | 1 (5.5) | 0 |
| Mode of delivery | ||
| Normal vaginal delivery | 10 (55.6) | 12 (60.0) |
| Instrumental vaginal delivery | 4 (22.2) | 4 (20.0) |
| Caesarean section | 4 (22.2) | 4 (20.0) |
| Currently breastfeeding | 1 (5.5) | 5 (25.0) |
| Taking antidepressants | 9 (50.0) | 13 (65.0) |
| Receiving psychological support | ||
| Yes | 9 (50.0) | 6 (30.0) |
| No | 7 (38.9) | 9 (45.0) |
| On waiting list | 1 (5.5) | 4 (20.0) |
| Social support scorea (range = 0–15) | ||
| ≤12 | 11 (61.1) | 16 (80.0) |
| 13–14 | 7 (38.9) | 1 (5.0) |
| 15 | 0 | 0 |
| Smokers | 4 (22.2) | 4 (20.0) |
| Physically active prior to pregnancy | 10 (55.6) | 7 (35.0) |
Participant numbers vary due to missing values.
Higher score represents greater social support.
Exercise participation and EPDS score
No significant mean difference between the groups was found for the frequency of participation in mild, moderate, or vigorous exercise, although scores for moderate-intensity exercise favoured the exercise group. The exercise group reported significantly higher adjusted mean self-efficacy for exercise scores than usual care (P = 0.002). EPDS scores did not differ significantly between the groups (Table 2).
Table 2.
Trial outcome data.
| Usual care, mean (SD) | Exercise, mean (SD) | Mean difference (95% CI) | |
|---|---|---|---|
| Mild-intensity exercisea | |||
| Baseline | 2.3 (2.0) | 1.9 (1.4) | 0.7 (−0.8 to 2.3) |
| Follow-upc | 2.4 (1.9) | 3.1 (2.0) | |
| Moderate-intensity exercisea | |||
| Baseline | 0.8 (1.4) | 1.8 (2.9) | 1.6 (−0.8 to 4.0) |
| Follow-upc | 1.8 (3.0) | 3.4 (3.2) | |
| Vigorous-intensity exercise | |||
| Baseline | 0.6 (1.0) | 0.3 (0.8) | 0.06 (−0.9 to 0.7) |
| Follow-upc | 0.7 (1.2) | 0.6 (1.2) | |
| Self-efficacy for exercisea,b | |||
| Baseline | 11.3 (3.8) | 10.5 (3.2) | 4.1 (1.6 to 6.4) |
| Follow-upc | 9.5 (3.1) | 13.6 (3.2) | |
| Postnatal depression (EPDS) | |||
| Baseline | 19.2 (4.7) | 17.7 (5.2) | 1.2 (−5.2 to 2.8) |
| Follow-upc | 14.3 (5.4) | 13.1 (5.2) | |
Mean times per week. Mild-intensity exercise refers to activities such as yoga, golf, and easy walking. Moderate-intensity exercise refers to activities such as fast walking, tennis, cycling, and dancing. Vigorous exercise refers to activities such as jogging and aerobics.
Denotes significant difference between groups at P<0.05.
Follow-up scores are adjusted for baseline. Note: follow-up data: usual care, n = 15; exercise, n = 16.
EPDS = Edinburgh Postnatal Depression Scale.
Adherence (intervention group only)
Descriptive analysis of data from the exercise diaries of the 11 participants who completed and returned these, indicated that participants engaged in exercise for a mean of 174 minutes (standard deviation = 73.6) per week. Ten of these 11 women were able to achieve the intervention goal of at least 105 minutes' exercise per week.
Open-ended questions
Of women who were randomised to the exercise intervention, 14 (70%) returned their responses to the intervention evaluation questionnaire. All responders stated exercise should be encouraged in women who are experiencing low mood. Eleven of the 14 women thought that exercise helped to improve their low mood. Twelve women reported that their general health had improved.
The most popular reasons given for participation in the study were to help depression/low mood (n = 7), enhance motivation to exercise (n = 4), help others experiencing similar symptoms (n = 3), and to have a goal to reach each day and to gain a sense of achievement (n = 2).
Most women reported they had enjoyed the exercise they had been doing during the intervention (n = 11). The most popular type of exercise was walking. The majority (n = 8) felt that they would do more exercise if there were group walking sessions with other women experiencing low mood after childbirth; four women were unsure; and two women did not feel groups would be useful. The main barriers to exercise faced by mothers were childcare and family responsibilities (n = 10), lack of time (n = 6), feeling tired (n = 4), weather (n = 4), and physical and psychological health problems related to mother or infant (n = 3).
DISCUSSION
Summary of main findings and comparison with existing literature
As anticipated, women with postnatal depression proved difficult to access. Responses to the study from general practices was low: only 9.5% of those approached responded and were able or willing to write to their eligible patients to invite them to take part; therefore, many women who may have been eligible were not given the opportunity to participate. The trial recruitment rate from among eligible patients contacted was disappointing (about 23%). This might indicate limited interest in exercise as a therapeutic intervention in women experiencing postnatal depression, or that the recruitment strategies were not as effective as they might have been.
The recruitment rate from the mother and baby unit was the most successful, which was encouraging. Women recruited from the mother and baby unit are likely to be have been more depressed, as more severe cases are referred and accepted for treatment by this service. Therefore, they might have been expected to have been more difficult to recruit than those identified from other routes.
The difficulties experienced in accessing eligible patients further emphasizes recent concerns about the difficulties of identifying women with postnatal depression19 for appropriate treatment to be offered and to diminish potential harm to the infant.4–5
No significant difference was found in the amount of exercise achieved between the groups, although the direction of findings favoured the exercise group. Interestingly, of the women who returned their exercise diary, all except one were able to achieve the intervention goal of at least 105 minutes of exercise per week. The lack of significant differences in exercise outcomes at follow-up may be the result of intervention contamination with trial information, possibly resulting in increased exercise participation in the usual care group, although exercise scores relative to baseline did not generally support this. The intervention applied may not have been adequate to induce an increase in exercise participation for this population of women.
The intervention group reported significantly higher self-efficacy for exercise scores, suggesting the intervention was successful in promoting participants to believe that they could achieve regular participation. Self-efficacy may be a proximal predictor of behaviour, which would impact on mood. Unlike previous research,10,11 no significant difference in EPDS scores was found between the groups, but the ability of the present study to detect a significant group difference in EPDS scores would only have been possible if the effect size had been as large as those found in the two previous trials.
The evaluation questionnaire indicated that participants felt they had experienced some mental health benefits, even though EPDS measurement of postnatal depression did not show a significant difference between the groups. Most participants reported they enjoyed the intervention and thought that exercise should be an activity that is endorsed for postnatal women with low mood. The majority of participants felt they would achieve more exercise if group sessions with other women experiencing low mood after childbirth were available, and this should be considered in the development of any subsequent interventions.
Strengths and limitations of the study
In this study, a range of recruitment strategies were assessed and data were provided on which methods are likely to be most effective. The small sample limits the generalisability of the trial findings, but the sample size is larger than both previous trials.10,11 The low level of attrition across follow-ups was encouraging and this is the first published study to take place in the UK.
Implications for future research
Women experiencing postnatal depression were difficult to access. Recruitment of eligible participants was possible but rates were low. In the absence of any routine system for the identification of patients with postnatal depression, critical to any subsequent trial would be a more effective identification strategy, such as screening by health visitors. The present data did not show a significant increase in exercise from this intervention, although the direction of effect from baseline was positive, and self-efficacy for exercise increased significantly.
Given the recent recommendation from NICE that health professionals should consider promoting exercise for the management of postnatal depression,12 it is imperative to find out whether this advice is warranted. Evidence from a larger trial is needed on whether, with an effective intervention, it is possible to increase exercise and reduce depression in postnatal women.
Acknowledgments
We would like to thank the practices, health visitors, and staff at the Mother and Baby Unit, Queen Elizabeth Psychiatric Hospital, Birmingham, who kindly agreed to assist with participant recruitment. We would particularly like to thank those patients who volunteered to participate in the study.
Funding body
This study was funded by the Midlands Research Practice Consortium (MidReC). Richard McManus is supported by a Department of Health Primary Care Postdoctoral Award
Ethical approval
Ethical approval was obtained from the South Birmingham Local Research Ethics Committee (05/Q2707/96)
Competing interests
The authors have stated that there are none
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Department of Health. Confidential enquiry into maternal and child health: why mothers die 2000–2002. London: Royal College of Obstetricians and Gynaecologists; 2004. [Google Scholar]
- 2.O'Hara M, Swain A. Rates and risk of postpartum depression — a meta analysis. Int Rev Psychol. 1996;8:37–54. [Google Scholar]
- 3.Gaynes BN, Gavin N, Melzer-Brody S, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2005. Perinatal depression: prevalence, screening accuracy and screening outcomes. Summary, Evidence Report/Technology Assessment no.119. Prepared by RTI-University of North Carolina Evidence-based Practice Center under contract No.290-02-0016. AHRQ Publication No.05-E006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray L. The impact of postnatal depression on infant development. J Child Psychol Psychiatry. 1992;33(3):543–561. doi: 10.1111/j.1469-7610.1992.tb00890.x. [DOI] [PubMed] [Google Scholar]
- 5.Caplan H, Cogill S, Alexandra H, et al. Maternal depression and the emotional development of the child. Br J Psychiatry. 1989;154:818–822. doi: 10.1192/bjp.154.6.818. [DOI] [PubMed] [Google Scholar]
- 6.Whitton A, Warner R, Appleby L. The pathway to care in post-natal depression: women's attitudes to post-natal depression and its treatment. Br J Gen Pract. 1996;46(408):427–428. [PMC free article] [PubMed] [Google Scholar]
- 7.Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomized controlled trials. BMJ. 2001;322(7289):1–8. doi: 10.1136/bmj.322.7289.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stathopoulou G, Powers MB, Berry AC, et al. Exercise interventions for mental health: a quantitative and qualitative review. Clin Psychol. 2006;13(2):179–193. [Google Scholar]
- 9.Daley AJ, MacArthur C, Winter H. The role of exercise as a treatment of postnatal depression: a review. J Midwifery Womens Health. 2007;52(1):56–62. doi: 10.1016/j.jmwh.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong K, Edwards H. The effects of exercise and social support on mothers reporting depressive symptoms: a pilot randomized controlled trial. Int J Mental Health Nurs. 2003;12(2):130–138. doi: 10.1046/j.1440-0979.2003.00229.x. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong K, Edwards H. The effectiveness of a pram-walking exercise programme in reducing depressive symptomatology for postnatal women. Int J Nurs Pract. 2004;10(4):177–194. doi: 10.1111/j.1440-172X.2004.00478.x. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. Antenatal and postnatal mental health. clinical management and service guidance. London: NICE; 2006. Reference CG45. [PubMed] [Google Scholar]
- 13.Cox J, Holden J, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 14.Godin G, Shephard RJ. A simple method to assess exercise behaviour in the community. Can J Appl Sport Sci. 1985;10(3):141–146. [PubMed] [Google Scholar]
- 15.Marcus BH, Selby VC, Niaura RS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 16.MacArthur C, Winter HR, Bick DE, et al. Effects of redesigned community postnatal care on women's health 4 months after birth: a cluster randomised controlled trial. Lancet. 2002;2(9304):378–385. doi: 10.1016/s0140-6736(02)07596-7. [DOI] [PubMed] [Google Scholar]
- 17.Daley AJ, Mutrie N, Crank H, et al. Exercise therapy in women who have had breast cancer: design of the Sheffield women's exercise and well-being project. Health Educ Res. 2004;19(6):686–697. doi: 10.1093/her/cyg094. [DOI] [PubMed] [Google Scholar]
- 18.Department of Health. At least five a week: evidence on the impact of physical activity and its relationship to health. A report from the Chief Medical Officer. London: Department of Health; 2004. [Google Scholar]
- 19.Coyne J, Mitchell AJ. NICE may be discouraging detection of postpartum depression. BMJ. 2007;334(7593):550. doi: 10.1136/bmj.39150.424896.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]