Abstract
Objective: The aim of this article is to present the assessment of the presentation of symptoms and psychiatric morbidity of children and adolescents from the Andaman and Nicobar islands during the first 3 months following the December 2004 earthquake and tsunami.
Method: According to predefined criteria, a primary survivor is one who was exposed directly to the earthquake and tsunami, a secondary survivor is one with close family and personal ties to primary survivors, and tertiary survivors are individuals from the communities beyond the impact area, a majority of which were exposed to the earthquake only. This study included 37 primary and secondary survivors (aged ≤ 18 years) and 498 tertiary survivors of the tsunami disaster. Tertiary survivors were recruited from the 10th and 12th grades of schools in Port Blair, India. The following 3 screening and treatment methods were adopted: (1) mental health clinic, (2) art therapy, and (3) group discussions.
Results: The most common psychiatric morbidities observed among the primary and secondary survivors were adjustment disorder (N = 5, 13.5%), depression (N = 5, 13.5%), panic disorder (N = 4, 10.8%), posttraumatic stress disorder (N = 4, 10.8%), schizophrenia (N = 1, 2.7), and other disorders (N = 16, 43.2%). Subclinical syndrome was present in the majority of the primary and secondary survivors. Few tertiary survivors had subsyndromal symptoms.
Conclusion: Only a few of the primary and secondary survivors required intensive individual psychiatric interventions; however, a majority of the primary, secondary, and tertiary survivors required community-based group interventions. Community-based group interventions and group discussions are simple, easy to implement using local resources, and effective in all groups, and provide important components of psychosocial rehabilitation. This kind of approach should be started as early as possible, targeting all children and adolescents affected by any disaster in developing countries.
Natural disasters such as the tsunami can have a devastating impact on the psychological and social well-being of anyone exposed to them. Disasters threaten personal safety, overwhelm defense mechanisms, and disrupt community and family structures.1 Such events may also cause mass casualties and destruction of property and may lead to a collapse of the social networks and daily routines of the individuals affected.2,3 Children and adolescents are more vulnerable than adults to the traumatic events of disasters. Even in preschoolers, the effects can be serious and persistent3–6 and can influence their personality development, but, at the same time, children have plasticity to change if an intervention can be developed to address their coping skills. A World Health Organization (WHO)–funded study conducted in Indonesia reported that 20% to 25% of children affected by the 2004 tsunami in south and southeast Asia required professional treatment for psychosocial problems.7 Depending on the cultural and social contexts, special measures must be taken to ensure the protection from harm of all children, as well as their equitable access to basic services.8,9 During this process of ensuring services to children, there is a high possibility that the support for adolescents may not be addressed effectively.10
Mental health professionals should keep in mind that “off-the-shelf” interventions are difficult to use in diverse settings of developing countries because they are unknowingly embedded with religious and cultural expectations.11 India is a land of diverse religions, languages, cultures, and ethnicities. These diversities may influence the need for help, availability of help, comfort in seeking help, and appropriateness of that help.9,12 Hence, planned interventions should be culturally appropriate to the local needs.8,13 Adding to this, outside agencies, foreign relief efforts, and news media can have an aggravating effect on individuals and their communities.14
Lack of trained mental health manpower and widespread stigma and discrimination add to the difficulty in providing mental health care.15 When resources are limited, it becomes all the more important to identify those people who are at risk for mental health problems and to allocate resources for their care.8,10 During a massive disaster like the 2004 tsunami, rehabilitation assistance should be targeted to empower the local community of the affected population in order to enhance their camaraderie and competence to deal with any kind of disaster in the future.
The main objective of this observational study was to present the assessment of the presentation of symptoms and psychiatric morbidity of children and adolescents in the Andaman and Nicobar islands during the first 3 months following the December 2004 tsunami. We report the clinical findings and interventions used by a National Institute of Mental Health and Neurosciences (NIMHANS) team from Bangalore, India.
METHOD
An earthquake measuring 9.0 on the Richter scale triggered a massive tsunami in the early hours of December 26, 2004, and caused devastation to the population of the Andaman and Nicobar Islands of India in the Bay of Bengal. The Andaman and Nicobar islands comprise a tribal population native to the islands and settlers from various states of India (mainland). The tribal groups have their own system of hierarchy that can be traced to the British naval system. Each village has 1 or more captains and subcaptains, who function like the heads of the joint families. Each family may comprise 40 to 120 members. Any type of intervention requires permission from the captain. These tribal populations are community- and kinship-oriented rather than individualistic. The patterns of the settler population are similar to those of the mainland. The settlers and tribals have their own religion, culture, family system, traditions, belief systems, occupations, and languages, which have been noted in an earlier article.16 NIMHANS was designated by the government of India as the nodal agency for assessment and coordination of psychosocial relief to all the affected populations following the tsunami. The data presented here are part of the community assessment and intervention done by the NIMHANS team.
Subjects
The study included 37 primary and secondary survivors and 498 tertiary survivors of the tsunami disaster from the Andaman and Nicobar islands. Of the primary and secondary survivors' sample, 19 were male and 18 were female in the age group ≤ 18 years. The primary and secondary survivors were assessed at 12 relief (refugee) camps of Port Blair (district headquarters of Andaman). The majority of the relief camps were situated in the schools of Port Blair and managed by the school authorities. Tertiary survivors were recruited from the 10th and 12th grades from schools of Port Blair, which was affected only by the earthquake.
Definitions
The following definitions were used in this study. A primary survivor is one who was exposed directly to both the earthquake and the tsunami. A secondary survivor is one with close family and personal ties to primary survivors. Tertiary survivors include individuals from communities beyond the impact area, the majority of which were exposed to the earthquake only. The definitions are somewhat similar to those of Young et al.17
Assessment and Intervention
The affected population was huge, and the survivors' population in the relief camp was highly mobile, thereby making it difficult to screen every child. Considering the logistics, the team decided to adopt a multitiered approach of assessment and intervention. The team contacted health, education, and social welfare departments of Andaman and Nicobar to educate them on the need for mental health care for disaster survivors and to seek their cooperation. The team also contacted the relief camp organizers, school principals and teachers, community leaders, and volunteers from the survivor groups to seek their cooperation and help. Many classes were held to educate the above groups, and each session lasted 1 to 2 hours. Sessions were focused on the identification of mental disorder symptoms and methods to normalize the daily activities of the children; brief steps of counseling were also taught.
Regarding the intervention, the following 3 methods were adopted: (1) mental health clinic, (2) art therapy, and (3) group discussions. Every visitor to the clinic, regardless of age, was included in the assessment and interventions. During the analysis, data from children and adolescents were considered. Assessment of tertiary survivors was carried out by group discussions in schools and preuniversity colleges after their academic classes.
Mental health clinics
The NIMHANS team approached each relief camp and contacted the medical officer in charge, the principal of the school, and the survivors' community leaders and local camp staff (teachers). These individuals were educated about disaster mental health. The need and process for setting up a mental health clinic for the survivors inside the relief camp was discussed. The consent and cooperation of the survivors' community leaders and the principal of the school were obtained, as this was highly essential for facilitating the process of entry into the community. Next, several announcements were made by the community leaders and the local staff of the camp about the availability of mental health professionals, and the mental health clinic was then started inside the relief camp.
Art therapy
The reason for adopting art therapy was that many parents were distressed by the disaster, did not allow their children to ventilate or speak about the disaster, and discouraged discussion of the event when the children wanted to express their feelings. With the help of the volunteers and teachers, we were able to get the children from the relief camps into art therapy (to participate in drawing). Each session lasted 90 to 120 minutes, and 10 to 20 participants were included in each session. Eight such sessions were conducted in the relief camps, and a total of 72 participants were included. Paper, color pencils, and crayons were provided. Initially, the participants were not given any theme for the drawings, but later they were asked to draw a picture of their place (i.e., village, school home, playground, temple, environment, etc.) after the tsunami. All of the children were asked to describe what they had drawn. This process helped the therapists screen out those who were severely affected by the disaster, and these children were referred to psychiatrists in the mental health clinic.
Group discussions
To assess the needs of the adolescent survivors, the NIMHANS team obtained permission from the principals and interacted through group sessions with nearly 498 students in the 10th and 12th grades of schools in Port Blair. The NIMHANS team conducted 9 such sessions; each lasted 60 to 90 minutes and was attended by 40 to 60 children. During each session, students were asked to describe their experiences regarding the disaster, and the session then focused on problems, concerns, and questions faced by the students. Finally, general “do's” and “don'ts” regarding coping strategies were discussed. This kind of intervention has been found to be useful in survivors of disasters such as the tsunami.18
Data Collection
Information was collected through direct observation, group sessions, individual sessions, and interviews with children, adolescents, and key informants. Data were also collected by interacting with the children and adolescents and reviewing the pictures drawn by them. Psychiatric assessments were not carried out using a structured instrument; however, diagnoses were made by a qualified psychiatrist per the ICD-10 diagnostic criteria.19 Sessions were conducted by a qualified psychiatrist, psychologist, and psychiatric social worker. Informed oral consent was provided by the parents and guardians of the primary and secondary survivors. The study was conducted in compliance with the ethics committee of NIMHANS.
RESULTS
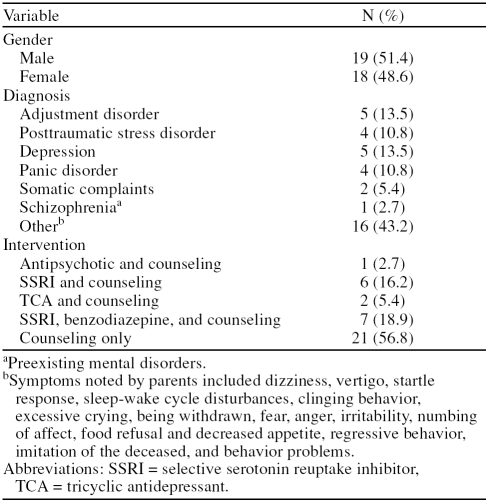
The distribution of diagnoses and interventions among the children and adolescents is shown in Table 1. The most common psychiatric morbidities observed in the primary and secondary survivor groups were adjustment disorder (N = 5, 13.5%), depression (N = 5, 13.5%), panic disorder (N = 4, 10.8%), posttraumatic stress disorder (PTSD) (N = 4, 10.8%), schizophrenia (N = 1, 2.7%), and other disorders (N = 16, 43.2%). Along with counseling, the survivor groups received the following medications: 7 (18.9%) received a combination of selective serotonin re-uptake inhibitors (SSRIs) and benzodiazepines, 6 (16.2%) received SSRIs, 2 (5.4%) received only tricyclic antidepressants, 1 (2.7%) received antipsychotic medication, and 21 (56.8%) received only counseling.
Table 1.
Distribution of Diagnoses and Interventions Among Primary and Secondary Survivors of the 2004 Tsunami (N = 37)
Primary and Secondary Survivors
Symptoms
Symptoms noted in the primary and secondary survivors by their parents were dizziness, vertigo, images of floating dead bodies, startle response, sleep-wake cycle disturbances, clinging behavior, excessive crying, being withdrawn, fear, anger, irritability, numbing of affect, food refusal and decreased appetite, regressive behavior, imitation of the deceased, and other behavior problems. The most common symptoms noted in the primary and secondary survivors were dizziness in 60% (N = 22) and images of floating dead bodies in 40% (N = 15). The majority of these symptoms were triggered by reminders such as noise or the sound of an airplane or helicopter flying past. Many parents were concerned about this phenomenon and consulted the treating team. On evaluation, the majority of the children did not meet any diagnostic criteria but did, however, require intervention.
Diagnosis
As mentioned previously, the most common psychiatric morbidities observed were adjustment disorder, depression, panic disorder, PTSD, schizophrenia, and other disorders. The “other disorders” (Tables 1 and 2) dominated the clinical picture in the present study, which is similar to the findings of a previous study.10 The majority of the primary and secondary survivors had subsyndromal symptoms and did not meet the current diagnostic classificatory system. According to WHO findings, only 5% to 10% of a disaster-affected population requires intensive mental health care, and more than 50% of these individuals require community-based intervention.20
Table 2.
Distribution of Diagnoses by Age Among Primary and Secondary Survivors of the 2004 Tsunami (N = 37)
Intervention
Among the younger children, it was noted that they did not talk or were too scared to recall their experiences. Thus, the therapists adopted art as a therapeutic mode for the catharsis of feelings. Children were encouraged to participate by drawing. Initially, most children did draw pleasant images of rainbows, mountains, and the peaceful sea. Some, however, drew images of destruction caused by the tsunami. Therefore, what could be interpreted for most children was a wish to restore the sense of happiness and contentment that existed before the tsunami. All children were asked to describe what they had drawn. Some children, who had drawn the scenes of destruction, ended their descriptions on a positive note of returning to a “normal life.”
The drawing method helped children express their feelings and at the same time helped the therapists screen out children who were severely affected by the disaster and who required individual intervention. Children whose drawings depicted extreme destruction, which was supported by their explanations of the drawings, were classified as extremely distressed and screened out for further management. Fourteen of the children were referred to mental health camps. Figures 1 through 3 are examples of drawings by children who were referred to such camps.
Figure 1.
A Drawing by a 6-Year-Old Boy Depicts How He Saw People and Houses Being Drowned in Water
Themes such as helplessness, a sense of loss, hopelessness, frustration, and uncertainty did emerge, especially in the adolescent group. However, in the children's group, there was a sense of loss regarding losing their homes and subsequently moving to camps. The psychological impact of losing a “place” or home can be profound and long lasting.21 Individual work focused on encouraging the survivors to speak (ventilation) about the disaster as they had witnessed it and, later, on instilling hope for the future. In certain cases, parents were also counseled on how they could reduce fear in their children by playing with them, spending time with them, reassuring them, keeping them engaged, structuring their daily routine, feeding them at regular intervals, and cuddling the infants frequently. Parents were also advised to allow children to express their feelings about the disaster and to not stop them from doing so. It also became apparent that some of the adolescents did try to save a few lives, and some saw their own family members being taken away by the waves. A few children and adolescents also reported survivor's guilt during the sessions. This guilt was handled in an appropriate manner by validating their emotions and feelings and through supportive therapy.
Tertiary Survivors
Symptoms
One third of the tertiary survivors reported dizziness and giddiness. The other reactions included lack of attention and concentration, worrying about the ongoing earthquake aftershocks and recurrence of tsunami, memory problems, anxiousness, decreased sleep, and apprehension about their future and school exams.
Diagnosis
Many students had a “normal reaction to the abnormal situation,” and few students had subsyndromal symptoms.
Intervention
The focus of the intervention in this group was to facilitate the expression of feelings associated with trauma, to normalize those feelings as appropriate reactions given the stressful reactions, and to reinforce the students' existing coping skills. This was facilitated in supportive personalized and interactive groups. During each session, students were asked to describe their experiences regarding the tsunami, and the session then focused on problems, concerns, and questions faced by the students. The therapists also used the group situation to give factual information about what had happened, thereby dispelling the rumors that were circulating after the tsunami. The students were also asked what they would do if this event were to happen again. Initially, almost every adolescent responded that he or she was scared and thought the disaster could happen again. The therapists explained to them how much they had learned from this experience and what they could do to save themselves, thus enhancing the preparedness of the group for future disasters. Other interventions in the form of ventilation, breathing exercises, and simple tasks for enhancement of attention and concentration were taught to the students. Important among all this is that the gender of the therapist played an important role: community leaders were comfortable allowing female therapists to manage the sessions involving girls. The team complied with this request immediately, because women in developing countries express their problems freely in front of a female therapist.
DISCUSSION
Our experience demonstrates the need for mental health interventions to start as early as possible following a disaster, the importance of using existing resources to empower the community's engagement in responding to the disaster, and the importance of reinforcing the innate resilience of individuals, families, and communities.
In developing countries, there is a lack of trained mental health manpower. This shortcoming was noted when the team contacted the medical personnel in charge of the relief camps, who reported that they had not seen a single case of mental illness following the disaster. During discussion, it was also noted that the knowledge of the medical personnel about mental health was very poor. Hence, mental health professionals should be involved from day 1 with the disaster team. Their responsibilities involve not only treatment but also sensitization of the community in regard to mental health and the disaster.
The majority of the relief camps were situated in the schools and run by school authorities.16 The team utilized the opportunity to train the teachers in disaster mental health and some basic counseling skills. Teachers at the schools were also educated about common mental health disorders so that they could screen out children and refer those who required further intervention. Volunteers from survivor groups were taught to screen out people with distress, to provide basic counseling, and to engage children in informal education. These volunteers were readily accepted by the survivors, as they belonged to their group, which led to community empowerment in disaster management. Therefore, in developing countries, local personnel should be trained for long-term sustainability.9
The resilient factors among the survivors were family systems, culture, and religious faith. The joint family seen in the tribal communities was 1 of the major factors that reduced the psychiatric morbidity, because children who belong to a clan are children of the clan irrespective of their biological parents; thus, children who lost their biological parents were cared for by “clan fathers and mothers.”
Religious institutions assumed different roles, from organizing relief camps to providing food and shelter for the survivors, and religious leaders gave their valuable time to the survivors by providing traditional and spiritual preaching. This religious grounding of the people played a major role in helping them come to terms with the destruction. They started their family and religious rituals by rebuilding their religious institutions collectively within a few weeks after the disaster using their own resources. Religious and family rituals were carried out in the relief camps, which helped children and other survivors deal with their grief.16 This finding is in accordance with previous observations that religious beliefs and social support can provide a basis for coping.22,23
The results presented here require interpretation against the background that these were assessments and clinical interventions following the disaster. Systematic study with rigorous methodology was not possible because of various reasons. No structured instrument was used in diagnosis; however, the diagnoses were made by a qualified psychiatrist per the ICD-10 diagnostic criteria.19
CONCLUSIONS
Only a few of the primary and secondary survivors required intensive individual psychiatric interventions, but the majority of the primary, secondary, and tertiary survivors required community-based group interventions. Therefore, mental health clinics in relief camps are useful in identifying and treating moderate-to-severe cases only. Community-based group interventions like art therapy (painting/drawing); informal education; group discussions; dramas; storytelling; structuring of days; engaging in activities such as yoga, relaxation, sports, and games; providing factual information; and educating parents and teachers help in the recovery of children and adolescents. These interventions are simple, easy to implement using local resources, and effective in all groups and provide important components of psychosocial rehabilitation such as normalizing, stabilizing, socializing, defusing of emotions and feelings, and restoration of a sense of identification with others and of safety and security, while allowing for the normal healing process and hope for the future in children. This kind of approach should be started as early as possible, targeting all children and adolescents affected by a disaster in developing countries.
Figure 2.
A Drawing by an 8-Year-Old Girl Depicts How She Saw People Being Sucked Into the Waves by the Tsunami and How They Cried for Help
Figure 3.
A Drawing by a 12-Year-Old Girl Highlights How Her School and Neighboring Buildings Such as the Primary Health Center, Church, and Bank Were Affected by the Tsunami
Footnotes
Funding was provided by the National Institute of Mental Health and Neurosciences (Deemed University), Bangalore, India.
We would like to express our gratitude to the Departments of Health, Education, and Social Welfare of the Andaman and Nicobar Islands, India. We would like to thank other members of the team who helped us in data collection.
The authors report no other financial affiliations relevant to the subject of this article.
REFERENCES
- Lubit R, Eth S. Children, disasters, and the September 11th World Trade Center Attack. In: Ursano RJ, Norwood AE, eds. Trauma and Disaster, Responses and Management, Review of Psychiatry Series. Arlington, Va: American Psychiatric Publishing. 2003 63–96. [Google Scholar]
- Ursano RJ, McCaughey BG, and Fullerton CS. eds. Individual and Community Responses to Trauma and Disaster. Cambridge, Mass: Cambridge University Press. 1994 [Google Scholar]
- Vogel JM, Vernberg EM.. Children's psychological responses to disasters. J Clin Child Psychol. 1993;22:464–484. [Google Scholar]
- Laor N, Wolmer L, and Mayes LC. et al. Israeli preschool children under scuds: a 30-month follow-up. J Am Acad Child Adolesc Psychiatry. 1997 36:349–356. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B.. Posttraumatic stress disorder in children: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:1503–1511. doi: 10.1016/S0890-8567(09)66558-8. [DOI] [PubMed] [Google Scholar]
- Yule W, Perrin S, and Smith P. Posttraumatic stress reactions in children and adolescents. In: Yule W, ed. Posttraumatic Stress Disorders: Concepts and Therapy. Chichester, United Kingdom: Wiley. 1999 25–50. [Google Scholar]
- Adventist Development and Relief Agency. Tsunami Response Report No. 34. Indonesia, Sri Lanka, India, Thailand; May 16. 2005. [Google Scholar]
- The Sphere Project. Humanitarian Charter and Minimum Standards in Disaster Response. Oxford, England: Oxfam Publishing. 2000 [DOI] [PubMed] [Google Scholar]
- Carballo M, Heal B, Hernandez M.. Psychosocial aspects of the Tsunami. J R Soc Med. 2005;98:396–399. doi: 10.1258/jrsm.98.9.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somasundaram DJ, van de Put WA. Management of trauma in special populations after a disaster. J Clin Psychiatry. 2006 67suppl 2. 64–73. [PubMed] [Google Scholar]
- Vega W.. Theoretical and pragmatic implications of cultural diversity for community research. Am J Community Psychol. 1992;20:375–392. [Google Scholar]
- Norris FH, Alegria M.. Mental health care for ethnic minority individuals and communities in the aftermath of disasters and mass violence. CNS Spectr. 2005;10:132–140. doi: 10.1017/s1092852900019477. [DOI] [PubMed] [Google Scholar]
- Barron RA.. International disaster mental health. Psychiatr Clin North Am. 2004;27:505–519. doi: 10.1016/j.psc.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Hawkins NA, McIntosh DN, and Silver RC. et al. Early responses to school violence: a qualitative analysis of students' and parents' immediate reactions to the shootings at Columbine High School. J Emotional Abuse. 2005 4:197–223. [Google Scholar]
- Chandrashekar CR, Math SB.. Psychosomatic disorders in developing countries: current issues and future challenges. Curr Opin Psychiatry. 2006;19:201–206. doi: 10.1097/01.yco.0000214349.46411.6a. [DOI] [PubMed] [Google Scholar]
- Math SB, Girimaji SC, and Benegal V. et al. Tsunami: psychosocial aspects of Andaman and Nicobar islands: assessments and intervention in the early phase. Int Rev Psychiatry. 2006 18:233–239. [DOI] [PubMed] [Google Scholar]
- Young BH, Ford JD, and Ruzek JI. et al. Disaster Mental Health Services: A Guidebook for Clinicians and Administrators. Menlo Park, Calif: Department of Veterans Affairs, National Center for Posttraumatic Stress Disorder. 1998 Available at: http://www.ncptsd.va.gov/ncmain/ncdocs/manuals/nc_manual_dmhm.html. Accessed Oct 24, 2007. [Google Scholar]
- Austin LS, Godleski LS.. Therapeutic approaches for survivors of disaster. Psychiatr Clin North Am. 1999;22:897–910. doi: 10.1016/s0193-953x(05)70132-5. [DOI] [PubMed] [Google Scholar]
- World Health Organization. ICD-10 Classification of Mental and Behavioural Disorders. Geneva, Switzerland: World Health Organization. 1992 [Google Scholar]
- World Health Organization. Mental Health Assistance to the Populations Affected by the Tsunami in Asia. Available at: http://www.who.int/mental_health/resources/tsunami/en. Accessed Oct 8, 2007. [Google Scholar]
- Fullilove MT.. Psychiatric implications of displacement: contributions from the psychology of place. Am J Psychiatry. 1996;153:1516–1523. doi: 10.1176/ajp.153.12.1516. [DOI] [PubMed] [Google Scholar]
- Fallot RD, Heckman JP.. Religious/spiritual coping among women trauma survivors with mental health and substance use disorders. J Behav Health Serv Res. 2005;32:215–226. doi: 10.1007/BF02287268. [DOI] [PubMed] [Google Scholar]
- Ano GG, Vasconcelles EB.. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. 2005;61:461–480. doi: 10.1002/jclp.20049. [DOI] [PubMed] [Google Scholar]