Abstract
Objectives. We sought to examine whether there were differential rates of HIV incidence among Aboriginal and non-Aboriginal injection drug users in a Canadian setting.
Methods. Data were derived from 2 prospective cohort studies of injection drug users in Vancouver, British Columbia. Using the Kaplan–Meier method and Cox proportional hazards regression, we compared HIV incidence among Aboriginal and non-Aboriginal participants.
Results. Overall, 2496 individuals were recruited between May 1996 and December 2005. Compared with that of non-Aboriginal persons, the baseline HIV prevalence was higher among Aboriginal persons (16.0% vs 25.1%; P<.001). Among participants who were HIV negative at baseline, the cumulative HIV incidence at 48 months was higher among Aboriginal persons (18.5% vs 9.5%; P<.001). In multivariate analyses, Aboriginal ethnicity was independently associated with elevated HIV incidence (relative hazard=1.59; 95% confidence interval=1.12, 2.26; P=.009).
Conclusions. Aboriginal persons in Vancouver had a significantly elevated burden of HIV infection, which calls for a culturally sensitive and evidence-based response. Policymakers in other settings with at-risk Aboriginal populations should seek to avert similar public health emergencies by being proactive with evidence-based HIV-prevention programs.
During the past 2 decades, the HIV epidemic has transitioned from primarily a sexually driven epidemic to one in which syringe sharing among illicit injection drug users contributes to a significant proportion of new infections.1 The United Nations Program on HIV/AIDS estimates that one third of new HIV infections outside sub-Saharan Africa is attributable to injection drug use.2 In North America, injection drug use accounts for approximately 1 in 4 cases of HIV,1 and in some areas where HIV is spreading most rapidly, such as Eastern Europe and Central Asia, more than 80% of all HIV cases occur among injection drug users.2 Among populations of injection drug users, recent surveillance reports have suggested that ethnic minorities may be particularly vulnerable to HIV infection.1
At the same time, there are growing concerns about the health of Aboriginal and Indigenous populations.3 The health status of Aboriginal populations varies across settings around the globe, as has recently been well articulated.3–6 However, Aboriginal persons have been shown to commonly have lower life expectancy as a result of higher rates of chronic diseases, such as heart disease and diabetes, and lower access to healthcare and prevention services. Access not only means physical access but also culturally appropriate and meaningful access to health services.3–6 High rates of poverty and illicit drug use, including injection drug use, have also been documented among Aboriginal populations.7 These conditions may make Aboriginal populations particularly vulnerable to the spread of HIV, although few studies have examined this issue.8,9 Therefore, we sought to examine rates of HIV infection among Aboriginal and non-Aboriginal injection drug users in a Canadian setting.
METHODS
We pooled participants being followed in 2 well-characterized cohorts of injection drug users in Vancouver, British Columbia. The first, the Vancouver Injection Drug Users Study (VIDUS) cohort, is an ongoing open prospective cohort study that is based on snowball sampling methods and outreach efforts at local services for injection drug users, primarily the city’s needle exchange program.10 The second, the Scientific Evaluation of Supervised Injecting (SEOSI) cohort, is an ongoing open prospective cohort study that is based on random sampling methods from the city’s supervised injecting facility.11 Recruitment was initiated for VIDUS in 1996 and for SEOSI in 2003, and both cohorts have been described in detail.12,13 As previously outlined,11 the follow-up procedures and questionnaire items were identical in both studies to allow for the merging of data sets.
In brief, the studies are observational in nature and, aside from pre– and post–HIV test counseling, no other intervention is involved. Rather, both studies involve HIV and hepatitis C testing and response to an interviewer-administered questionnaire at baseline and on a semiannual basis. Although services such as methadone treatment and needle exchange are accessed independent of the study, the staff seek to actively refer participants to health and social services. The cohorts receive annual ethical approval from the University of British Columbia/Providence Healthcare Research Ethics Board and are conducted in a fashion consistent with other prospective cohort studies of injection drug users. Participants were eligible for our study if they were recruited between May 1996 and December 2005.
We compared HIV prevalence levels at the time of recruitment and subsequent HIV incidence rates among Aboriginal and non-Aboriginal participants. As previously described,9,14 Aboriginal ethnicity was defined as self-reporting being First Nations, Inuit, Métis, or Aboriginal. All individuals recruited during the study period were eligible for the analysis of baseline HIV prevalence, whereas individuals who were HIV negative at baseline and who had at least 1 follow-up visit (to retest for HIV infection) were eligible for the analysis of HIV incidence. To avoid duplication, any individual who was recruited into both cohorts was retained only in the cohort into which they were first enrolled.
The statistical analyses of HIV incidence were undertaken with an a priori–defined statistical protocol as follows. First, baseline characteristics of study participants stratified by ethnicity (Aboriginal vs other) were examined to evaluate potential baseline differences between these populations. Variables considered included gender, age, unstable housing, residency in Vancouver’s HIV epicenter known as the Downtown Eastside, use of methadone, having sought but having been unable to obtain addiction treatment, sex-trade involvement, daily heroin injection, daily cocaine injection, used-syringe borrowing, requiring help injecting, binge drug use, and unsafe sexual intercourse (defined as vaginal or anal intercourse without a condom). All variable definitions were identical to those in earlier studies.10,15 All behavioral variables were in reference to the prior 6 months, except for methadone use, which referred to current use. The Pearson χ2 test was used to compare categorical variables, and the Wilcoxon rank sum test was used to compare continuous variables.
Kaplan–Meier Analyses
We calculated the cumulative HIV incidence among Aboriginal versus non-Aboriginal participants. We also conducted analyses that compared these rates when the cohort was restricted to male injection drug users, female injection drug users, younger injection drug users, and older injection drug users. Younger and older categories were defined a priori by stratifying the cohort on the basis of the median baseline age. As previously described,16 the date of HIV seroconversion was estimated by using the midpoint between the last negative and the first positive antibody test results. Participants who remained persistently HIV seronegative were censored at the time of their most recent available HIV antibody test result prior to December 2005. Time-zero for all prospective analyses was the date of recruitment into the respective study (SEOSI or VIDUS). Although it would have been informative to use time from the initiation of injecting, all participants were injecting at the time of recruitment into SEOSI and VIDUS (i.e., this was an eligibility criterion).
Multivariate Analyses
We also calculated the unadjusted and adjusted relative hazards of HIV seroconversion with Cox proportional hazards regression. Here, all behavioral variables were treated as time-updated covariates on the basis of semiannual follow-up data. For the multivariate model, a fixed model was built that adjusted for all variables described previously that were statistically associated with HIV seroconversion in unadjusted analyses. Cox models were prepared for the overall cohort, with Aboriginal ethnicity included as an independent variable and as part of stratified analyses that considered Aboriginal and non-Aboriginal participants separately. Analyses were conducted with SAS 8.0 (SAS Institute Inc, Cary, NC); the threshold for statistical significance was set at P<.05. All P values were 2-sided.
RESULTS
During the study period, 2496 unique individuals were recruited into either VIDUS or SEOSI, among whom 585 (23.4%) reported being Aboriginal, First Nations, Inuit, or Métis. Overall, the baseline HIV prevalence was 18.2%. In both VIDUS (26.9% vs 17.6%; P <.001) and SEOSI (27.0% vs 14.1%; P <.001), the baseline HIV prevalence was higher among Aboriginal participants than among non-Aboriginals (combined cohort: 25.1% vs 16.0%; P <.001).
Among the 2043 participants who were HIV negative at baseline, 1639 (80.2%) had at least 1 follow-up visit. Compared with the 404 (19.8%) individuals who were HIV negative at baseline and who were excluded from analyses of HIV incidence because they did not have follow-up data to ascertain HIV incidence, the 1639 individuals included in these analyses were more likely to be older and Aboriginal (both P <.05).
Table 1 ▶ shows the demographic and risk behavior profile of participants who were HIV negative at baseline stratified by ethnicity. As shown here, compared with non-Aboriginal participants, Aboriginal participants were more likely to be women (P <.001), to be younger (P <.001), to reside in the Downtown Eastside (P =.007), to be involved in the sex trade (P <.001), to inject cocaine daily (P =.016), and to report having had unsafe sex (P =.003). Aboriginal participants were less likely to report methadone use (P <.001) and daily heroin injection (P =.013). There were no significant differences on the basis of housing status, having sought but having been unable to access addiction treatment, syringe sharing, requiring help injecting, and reporting binge drug use.
TABLE 1—
Baseline Demographic Characteristics of Injection Drug Users, by Ethnicity: Scientific Evaluation of Supervised Injecting Study and the Vancouver Injection Drug Users Study, Vancouver, British Columbia, 1996–2005
| Characteristic | Non-Aboriginal (n = 1272), No. (%)a | Aboriginal (n = 367), No. (%) | OR (95% CI) | P |
| Female | 333 (26.2) | 191 (52.0) | 3.06 (2.41, 3.89) | <.001 |
| Age, median (IQR) | 37 (29–43) | 34 (26–40) | 0.98 (0.97, 0.99) | <.001 |
| Unstable housinga | 727 (57.2) | 227 (61.9) | 1.22 (0.96, 1.54) | .108 |
| Downtown Eastside residenceb | 746 (58.7) | 244 (66.5) | 1.40 (1.10, 1.79) | .007 |
| Currently on methadone | 211 (16.6) | 21 (5.7) | 0.31 (0.19, 0.49) | <.001 |
| Denied treatmentb,c | 255 (20.1) | 71 (19.4) | 0.96 (0.71, 1.28) | .767 |
| Involved in sex tradeb | 275 (21.6) | 132 (36.0) | 2.03 (1.58, 2.62) | <.001 |
| Daily heroin injectionb | 561 (44.1) | 135 (36.8) | 0.74 (0.58, 0.94) | .013 |
| Daily cocaine injectionb | 380 (29.9) | 134 (36.5) | 1.35 (1.06, 1.72) | .016 |
| Syringe sharingb | 397 (31.2) | 98 (26.7) | 0.80 (0.62, 1.04) | .098 |
| Require help injectingb | 480 (37.7) | 144 (39.2) | 1.07 (0.84, 1.35) | .602 |
| Binge drug useb | 677 (53.2) | 188 (52.2) | 0.92 (0.73, 1.16) | .500 |
| Unsafe sexual intercourse | 674 (53.0) | 227 (61.9) | 1.44 (1.13, 1.82) | .003 |
Notes: OR = odds ratio; CI = confidence interval; IQR = interquartile range.
aUnless noted.
bBehavior during the 6-month period prior to the baseline interview.
cHaving sought but having been unable to access addiction treatment.
As of December 2005, 159 HIV seroconversions were observed. The incidence density was 3.9 per 100 person-years among Aboriginal persons and 2.32 among non-Aboriginal persons (P <.001). As shown in Figure 1 ▶, at 48 months after recruitment the Kaplan–Meier cumulative HIV incidence was 18.5% among Aboriginal participants compared with 9.5% among non-Aboriginal participants (log-rank P <.001). Figure 2 ▶ shows the 48-month cumulative HIV incidence among Aboriginal and non-Aboriginal participants when the population at risk was restricted to younger injection drug users (Figure 2a ▶: 22.1% vs 9.8%; log-rank P =.001), older injection drug users (Figure 2b ▶: 14.5% vs 9.1%; log-rank P =.343), female injection drug users (Figure 2c ▶: 21.1% vs 11.9%; log-rank P =.101), and male injection drug users (Figure 2d ▶: 16.6% vs 8.5%; log-rank P =.028). Although some of these differences were not statistically significant when the smaller subpopulations were examined, the trend toward higher HIV incidence among Aboriginal persons was clearly evident in each case (Figure 2 ▶).
FIGURE 1—

Cumulative HIV incidence rates, by ethnicity: Scientific Evaluation of Supervised Injecting Study and the Vancouver Injection Drug Users Study, Vancouver, British Columbia, 1996–2005.
Note. Log-rank = P < .001
FIGURE 2—
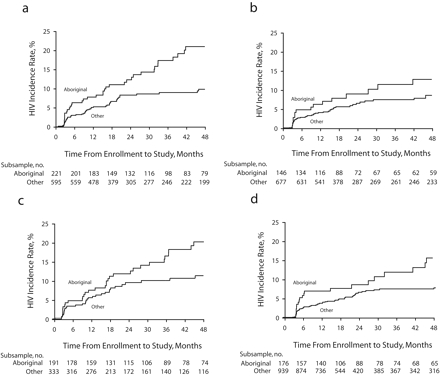
Cumulative HIV incidence, by ethnicity, among younger injection drug users (a), older injection drug users (b), women (c), and men (d): Scientific Evaluation of Supervised Injecting Study and the Vancouver Injection Drug Users Study, Vancouver, British Columbia, 1996–2005.
Note. Younger and older age were defined on the basis of the median age. The log-rank for a was P = .001; for b, P = .343; for c, P = .101; for d, P = .028.
Table 2 ▶ shows the results of the unadjusted and adjusted Cox proportional hazard regression analysis of the time to HIV infection for HIV risk behaviors and demographic characteristics. As shown here, in unadjusted Cox regression analyses, the relative hazard (RH) of HIV seroconversion for Aboriginal versus non-Aboriginal persons was 1.85 (95% confidence interval [CI] = 1.33, 2.56; P <.001). After we adjusted for all variables associated with the time to HIV infection in univariate analyses (ethnicity, Downtown Eastside residence, borrowing syringes, daily cocaine injection, daily heroin injection, gender, sex-trade involvement, and binge drug use), as well as for cohort of initial recruitment, the RH of HIV infection was 1.59 (95% CI = 1.12, 2.26; P = .009) for Aboriginal versus non-Aboriginal persons. Cohort of recruitment, age, unstable housing, use of methadone, inability to access addiction treatment, and unsafe sexual intercourse were not associated with HIV incidence in univariate analyses (all P > .05). We found that the proportional hazards assumption of the Cox model was satisfied when we tested the coefficients for time dependence.
TABLE 2—
Univariate and Multivariate Cox Proportional Hazard Analyses of the Time to HIV Infection Among 1639 Injection Drug Users: Scientific Evaluation of Supervised Injecting Study and the Vancouver Injection Drug Users Study, Vancouver, British Columbia, 1996–2005
| Unadjusted | Adjusteda | |||
| Relative Hazard (95% CI) | P | Relative Hazard (95% CI) | P | |
| Ethnicity (Aboriginal vs other) | 1.85 (1.33, 2.56) | <.001 | 1.59 (1.12, 2.26) | .009 |
| Downtown Eastside residenceb (yes vs no) | 2.83 (1.98, 4.06) | <.001 | 2.40 (1.65, 3.45) | <.001 |
| Syringe sharingb (yes vs no) | 2.14 (1.49, 3.09) | <.001 | 1.58 (1.08, 2.32) | .020 |
| Require help injectingb (yes vs no) | 2.52 (1.80, 3.52) | <.001 | 1.74 (1.23, 2.50) | .002 |
| Cocaine injectionb (daily vs not daily) | 3.56 (2.57, 4.93) | <.001 | 2.37 (1.67, 3.45) | <.001 |
Notes. CI = confidence interval. Only significant variables are shown.
aModel was fit-adjusted for initial cohort of recruitment, gender, involvement in sex trade, daily heroin injection, binge drug use (all P > .05 after adjustment).
bIn the past 6 months.
When this statistical model fitting protocol was restricted to Aboriginal participants, only Downtown Eastside residence (RH = 4.0; 95% CI = 1.91, 8.29; P < .001) and daily cocaine injection (RH = 1.95; 95% CI = 1.11, 3.45; P = .021) were independently associated with HIV seroconversion. In a model restricted to non-Aboriginal persons, Downtown Eastside residence (RH = 1.94; 95% CI = 1.26, 3.00; P = .003), daily cocaine injection (RH = 2.58; 95% CI = 1.67, 3.99; P < .001), requiring help injecting (RH = 1.92; 95% CI = 1.25, 2.96; P = .003), and sharing syringes (RH = 1.77; 95% CI = 1.10, 2.83; P = .018) were independently associated with HIV seroconversion.
DISCUSSION
Our study demonstrated significantly elevated baseline HIV prevalence and subsequent significantly elevated HIV incidence among Aboriginal injection drug users. Although not statistically significant in all cases, the trend toward elevated HIV rates was apparent in subgroup analyses in which men and women were considered separately, and when the cohort was stratified into younger and older participants.
A preliminary study from the VIDUS cohort reported HIV incidence rates among Aboriginal persons, although this study was limited because it only considered 230 Aboriginal persons, and only 44 HIV seroconversions were observed between 1996 and 2000 among this population.9 These limitations precluded a detailed evaluation of HIV incidence and comparison of risk factors for HIV incidence between Aboriginal and non-Aboriginal persons, both of which were addressed by the additional 5 years of follow-up and the merging of cohorts in our study.
Our findings demand a culturally appropriate and evidence-based response to the HIV epidemic among Aboriginal injection drug users. Canada’s drug strategy has recently been the subject of significant criticism.17 This criticism stems from the fact that resources are overwhelmingly devoted to law enforcement–based interventions, which have been shown to have negative health consequences related to health service interruption18 and limited evidence of effectiveness as evidenced by increased illicit drug supply and decreasing drug prices.19,20 Aboriginal communities have become particularly affected by this approach. Aboriginal persons currently represent approximately 3% of the Canadian population but more than 20% of the incarcerated population, and many of these cases relate to illicit drug offenses.21,22
Our findings suggest the need for immediate action on the part of health policymakers. A plan of action will require policymakers to recognize that addiction is primarily a health and social issue and to acknowledge the harms of seeking to address addiction through a strategy that largely relies on law enforcement as an isolated intervention.20,23 These harms disproportionately affect the most vulnerable injection drug users.17,24 This strategy will also require evidence-based decisionmaking, whereby funding is channeled toward those interventions in which there is known or increasing evidence of effectiveness and away from interventions that have proven ineffective.25–27 Finally, to effectively address the HIV epidemic among Aboriginal populations, culturally sensitive interventions must be developed through a partnership that involves full participation of the Aboriginal community in their design, implementation, and evaluation.28
Our study had several limitations. Most importantly, studies of injection drug users have suggested that socially desirable reporting may lead to an underestimation of certain HIV risk behaviors,29 although other studies have suggested self-reports to be valid.30 Although this may have influenced our risk factor analyses, it does not explain the observed differences in both HIV prevalence and incidence. Similarly, studies of marginalized populations, such as injection drug users, may be subject to concerns related to generalizability because it is not possible to derive a random sample of the overall population. This concern is relevant to all prospective cohort studies of injection drug users, and it is noteworthy that the demographics of both VIDUS and SEOSI were largely consistent with what is known about the demographics of the populations of injection drug users in the local community.11
A final limitation was that differing recruitment methods were used to derive the VIDUS and SEOSI cohorts, and the cohorts initiated recruitment at different times. Thus, there may have been differences between cohorts, and there is also the potential of a cohort effect in which risk factors for HIV acquisition changed over time. We sought to address this limitation by adjusting for cohort of recruitment, and despite these issues, the fact that we observed an elevated burden of HIV infection in 2 independent cohorts lends support to the idea that the HIV rate among Aboriginal injection drug users requires a special and appropriate response.
Our findings demonstrate that Aboriginal persons experience a significantly elevated burden of HIV infection in the Vancouver setting, which requires an urgent, culturally sensitive, and evidence-based response. Policy-makers in other settings with at-risk Aboriginal populations should seek to avert similar public health emergencies by being proactive with evidence-based HIV-prevention programs.
Acknowledgments
The Scientific Evaluation of Supervised Injecting Study was supported by Health Canada, although the views expressed herein do not represent the official policies of Health Canada. The Vancouver Injection Drug Users Study was supported by the US National Institutes of Health and the Canadian Institutes of Health Research. M. W. Tyndall was supported by a Michael Smith Foundation for Health Research Senior Scholar award. T. Kerr was supported by a Canadian Institutes of Health Research New Investigator award and a Michael Smith Foundation for Health Research Scholar award.
We would like to thank the participants in the Scientific Evaluation of Supervised Injecting Study and Vancouver Injection Drug Users Study for their ongoing contribution to these studies and the Vancouver Injection Drug Users Study Community Advisory Board members for their input. We also thank Caitlin Johnston, Deborah Graham, Cari Miller, Steve Kain, Peter Vann, Cody Callon, Sidney Crosby, Vanessa Volkommer, Aaron Eddie, Trevor Logan, Cristy Power, Daniel Kane, Calvin Lai, and Will Small for their administrative assistance. The authors also wish to thank the 3 external peer reviewers for their thoughtful comments on the original draft of this article.
Human Participant Protection This research was approved by the University of British Columbia/Providence Healthcare Research Ethics Board.
Peer Reviewed
Contributors E. Wood designed the study, drafted the original article, and addressed the reviewers’ comments. J.S.G. Montaner, K. Li, L. Barney, S. A. Strathdee, M. W. Tyndall, and T. Kerr contributed to the writing and revision of the article. K. Li conducted the statistical analyses.
References
- 1.Karon JM, Fleming PL, Steketee RW, De Cock KM. HIV in the United States at the turn of the century: an epidemic in transition. Am J Public Health. 2001;91:1060–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joint United Nations Programme on HIV/AIDS. 2006 report on the global AIDS epidemic. Available at: http://www.unaids.org/en/HIV_data/2006GlobalReport/default.asp. Accessed September 15, 2006.
- 3.Horton R. Indigenous peoples: time to act now for equity and health. Lancet. 2006;367:1705–1707. [DOI] [PubMed] [Google Scholar]
- 4.Stephens C, Porter J, Nettleton C, Willis R. Disappearing, displaced, and undervalued: a call to action for Indigenous health worldwide. Lancet. 2006;367:2019–2028. [DOI] [PubMed] [Google Scholar]
- 5.Stephens C, Nettleton C, Porter J, Willis R, Clark S. Indigenous peoples’ health—why are they behind everyone, everywhere? Lancet. 2005;366:10–13. [DOI] [PubMed] [Google Scholar]
- 6.Anderson I, Crengle S, Kamaka ML, Chen TH, Palafox N, Jackson-Pulver L. Indigenous health in Australia, New Zealand, and the Pacific. Lancet. 2006;367:1775–1785. [DOI] [PubMed] [Google Scholar]
- 7.Perkins JJ, Sanson-Fisher RW, Blunden S, Lunnay D, Redman S, Hensley MJ. The prevalence of drug use in urban aboriginal communities. Addiction. 1994;89:1319–1331. [DOI] [PubMed] [Google Scholar]
- 8.Breen C, Roxburgh A, Degenhardt L. Gender differences among regular injecting drug users in Sydney, Australia, 1996–2003. Drug Alcohol Rev. 2005;24:353–358. [DOI] [PubMed] [Google Scholar]
- 9.Craib KJ, Spittal PM, Wood E, et al. Risk factors for elevated HIV incidence among Aboriginal injection drug users in Vancouver. CMAJ. 2003;168:19–24. [PMC free article] [PubMed] [Google Scholar]
- 10.Strathdee SA, Patrick DM, Currie SL, et al. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS. 1997;11:F59–F65. [DOI] [PubMed] [Google Scholar]
- 11.Wood E, Kerr T, Lloyd-Smith E, et al. Methodology for evaluating Insite: Canada’s first medically supervised safer injection facility for injection drug users. Harm Reduct J. 2004;1, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerr T, Tyndall M, Li K, Montaner J, Wood E. Safer injection facility use and syringe sharing in injection drug users. Lancet. 2005;366:316–318. [DOI] [PubMed] [Google Scholar]
- 13.Wood E, Tyndall MW, Zhang R, et al. Attendance at supervised injecting facilities and use of detoxification services. N Engl J Med. 2006;354:2512–2514. [DOI] [PubMed] [Google Scholar]
- 14.Wood E, Kerr T, Palepu A, et al. Slower uptake of HIV antiretroviral therapy among Aboriginal injection drug users. J Infect. 2006;52:233–236. [DOI] [PubMed] [Google Scholar]
- 15.Miller CL, Spittal PM, LaLiberte N, et al. Females experiencing sexual and drug vulnerabilities are at elevated risk for HIV infection among youth who use injection drugs. J Acquir Immune Defic Syndr. 2002;30:335–341. [DOI] [PubMed] [Google Scholar]
- 16.Tyndall MW, Currie S, Spittal P, et al. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17:887–893. [DOI] [PubMed] [Google Scholar]
- 17.deBeck K, Wood E, Montaner J, Kerr T. Canada’s 2003 renewed drug strategy—an evidence-based review. HIV AIDS Policy Law Rev. 2006;11:1, 5–12. [PubMed] [Google Scholar]
- 18.Bluthenthal RN, Lorvick J, Kral AH, Erringer EA, Kahn JG. Collateral damage in the war on drugs: HIV risk behaviours among injection drug users. Int J Drug Policy. 1999;10:25–38. [Google Scholar]
- 19.Wood E, Tyndall MW, Spittal PM, et al. Impact of supply-side policies for control of illicit drugs in the face of the AIDS and overdose epidemics: investigation of a massive heroin seizure. CMAJ. 2003;168:165–169. [PMC free article] [PubMed] [Google Scholar]
- 20.Drucker E. Drug prohibition and public health: 25 years of evidence. Public Health Rep. 1999;114:14–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.PrisonJustice. CA. Facts and statistics. Available at: http://www.prisonjustice.ca/politics/facts_stats.html. Accessed January 16, 2007.
- 22.Canadian Foundation for Drug Policy. Drugs and drug policy in Canada. Available at: http://www.cfdp.ca/sen8ex1.htm. Accessed January 16, 2007.
- 23.Wood E, Spittal P, Small W, et al. Displacement of Canada’s largest public illicit drug market in response to a police crackdown. CMAJ. 2004;170:1551–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Small D. The war on drugs is a war on racial justice. Soc Res. 2001;68:896–903. [Google Scholar]
- 25.Des Jarlais DC, Hagan H, Friedman SR, et al. Maintaining low HIV seroprevalence in populations of injecting drug users. JAMA. 1995;274:1226–1231. [DOI] [PubMed] [Google Scholar]
- 26.Des Jarlais DC. Harm reduction—a framework for incorporating science into drug policy. Am J Public Health. 1995;85:10–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wood E, Tyndall MW, Montaner JS, Kerr T. Summary of findings from the evaluation of a pilot medically supervised safer injecting facility. CMAJ. 2006;175:1399–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benoit C, Carroll D, Chaudhry M. In search of a healing place: Aboriginal women in Vancouver’s Downtown Eastside. Soc Sci Med. 2003;56:821–833. [DOI] [PubMed] [Google Scholar]
- 29.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353:1657–1661. [DOI] [PubMed] [Google Scholar]
- 30.Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. [DOI] [PubMed] [Google Scholar]


