Abstract
We analyzed data from a randomized trial of 322 actively depressed smokers and examined the effect of smoking cessation on their mental health functioning. Only 1 of 10 measures at 4 follow-up time points was significant: participants who successfully stopped smoking reported less alcohol use than did participants who continued smoking. Depressive symptoms declined significantly over time for participants who stopped smoking and those who continued smoking; there were no group differences. Individuals in treatment for clinical depression can be helped to stop smoking without adversely affecting their mental health functioning.
Despite elevated rates of tobacco use among individuals who have mental illness, very little is known about how best to treat their tobacco dependence. Prevailing beliefs among mental health professionals, tobacco control advocates, and researchers that patients need to smoke to manage their psychiatric symptoms may reduce access to tobacco treatment.
Alarming case studies have reported the recurrence of major depression following tobacco cessation in smokers who have a history of depression.1 These studies could not, of course, control for the elevated risk of depression recurrence among individuals who had histories of depression.
Two empirical studies examined depression recurrence and smoking cessation. In the first study, 100 individuals who had a history of depression were part of an investigation of the use of sertraline for smoking cessation. Glassman et al.2 reported a 7-fold increase in depression recurrence among participants who successfully stopped smoking. However, 39% of smokers who relapsed were lost to follow-up and their depression status was undetermined; only 5% of successful quitters were lost to follow-up. In the second study, Tsoh et al.3 investigated 304 smokers who were receiving smoking cessation treatment, 32% of whom had a history of depression. They reported a 14% 12-month incidence of major depression. Recurrence of depression was predicted by depression history and not by smoking status.
A recent randomized clinical trial was one of the first to examine tobacco dependence treatment in actively depressed smokers.4 The staged-care intervention, which matched intervention services to participants’ readiness to quit smoking, demonstrated significant cessation effects at 12- and 18-month follow-ups. At 18 months, cessation rates were 20% and 25% in the control and treatment groups, respectively. These data made it possible to examine the effect of smoking cessation on mental health functioning among depressed smokers. If tobacco use serves to self-medicate depressive symptoms, one would expect psychiatric symptoms to worsen and mental health service use to increase following smoking cessation. We tested this hypothesis.
METHODS
Our sample, randomization methods, and treatment conditions have been described elsewhere.4,5 Briefly, 322 daily smokers who had a unipolar depression diagnosis were recruited from 1 of 4 mental health outpatient clinics and provided signed informed consent. All participants in the intervention completed a computer-delivered expert-system program (briefly, a computer program that mimics the reasoning and problem solving of human “experts.”) that provided feedback matched to participants’ stage of change for quitting smoking. The program was completed at baseline, 3 months, and 6 months, and feedback was based on normative data and the participants’ own previous responses. In addition, intervention participants interested in quitting smoking could receive 6 sessions of individual cognitive–behavioral counseling combined with a nicotine patch. The control group received brief cessation advice. Assessments were conducted at baseline, 3, 6, 12, and 18 months. “Quit smoking” status was defined by a 7-day abstinence from cigarettes, verified by expired air carbon monoxide (≤10 ppm). Self-report psychiatric outcome measures included the Beck Depression Inventory-II6 (BDI-II), the Mental Component Summary of the Medical Outcomes Study Short Form7 (SF–36), the State-Trait Anger Expression Inventory8 (STAXI), days with emotional problems and inpatient psychiatric hospitalizations on the Treatment Services Review,9 and alcohol and illicit drug use.
We tested the association between smoking status (quit or smoking) and mental health functioning at each time point with the χ2 and t test, and over time with generalized estimating equations. Generalized estimating equations made it possible to model missing data and control for treatment effects and history of recurrent depression.
RESULTS
Participants’ scores on 10 indicators of mental health functioning at baseline and 4 follow-up assessments are shown by smoking status in Table 1 ▶ and Figures 1 ▶–3 ▶ ▶. Data from the intervention and control groups are combined. Attrition was 17% at 3 months, 24% at 6 months, 30% at 12 months, and 28% at 18 months. Missing an assessment was not associated with previous smoking cessation status. Of the 40 comparisons, 1 was significant: successful quitters were less likely to report alcohol use at 6 months compared with smokers (odds ratio = 0.29, P =.018).
TABLE 1—
Frequency of Mental Health Problems and Changes Over Time, by Smoking Status
| Follow-Up Assessment | |||||
| Smoking Status | Baseline | 3 months | 6 months | 12 months | 18 months |
| Suicidal ideationa | |||||
| Quitter | … | 0% | 0% | 0% | 0% |
| Smoker | 4% | 2% | 3% | 1% | 3% |
| Inpatient psychiatry hospitalizationb | |||||
| Quitter | … | 0% | 4% | 3% | 4% |
| Smoker | 4% | 2% | 3% | 2% | 3% |
| Substance usec | |||||
| Alcohol | |||||
| Quitter | … | 19% | 9% | 24% | 18% |
| Smoker | 39% | 25% | 25% | 26% | 27% |
| Marijuana | |||||
| Quitter | … | 24% | 27% | 29% | 18% |
| Smoker | 35% | 24% | 20% | 31% | 30% |
| Stimulants | |||||
| Quitter | … | 5% | 2% | 5% | 2% |
| Smoker | 11% | 8% | 7% | 10% | 7% |
| Opiates | |||||
| Quitter | … | 11% | 4% | 3% | 2% |
| Smoker | 3% | 4% | 4% | 1% | 1% |
Note. “Quit smoking” status was defined as a 7-day abstinence from cigarettes, verified by expired air carbon monoxide (≤10 ppm). The number of quitters and smokers varied at each assessment: 3 months (37 quit, 230 smoking); 6 months (48 quit, 197 smoking), 12 months (38 quit, 187 smoking), and 18 months (51 quit, 181 smoking). Data from the intervention and control groups are combined. Attrition at each assessment was 3 months = 17%, 6 months = 24%, 12 months = 30%, and 18 months = 28%.
aSuicidal ideation was assessed as a score of 2 or 3 on item #9 of the Beck Depression Inventory-II.6
bInpatient psychiatry hospitalization was assessed for the previous 30 days at baseline and since the previous assessment at each follow-up.
cSubstance use was assessed for the previous 6 months at baseline and since the previous assessment at each follow-up.
FIGURE 1—
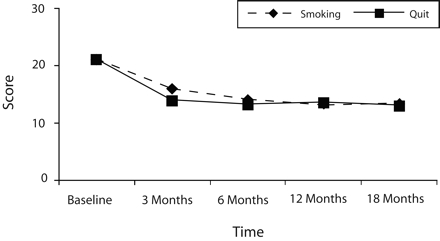
Changes over time in Beck Depression Inventory-II (BDI-II) scores, by smoking status.
Note. BDI-II6 scores range from 0 to 63 and declined over time from moderate to mild levels for both groups.
FIGURE 2—
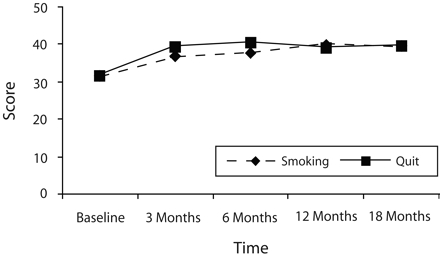
Changes over time in Medical Outcomes Study Short Form (SF-36) Mental Component scores.
Note. Higher values indicate improvements in mental health functioning
FIGURE 3—
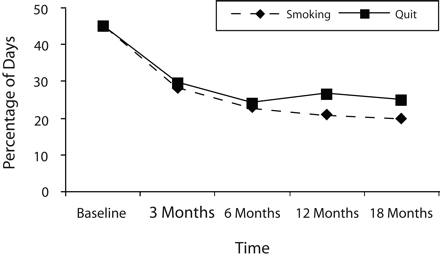
Change over time in percentage of days with emotional problemsa reported for the last 30 days at baseline and since the previous assessment at each follow-up.
aBased on treatment Service Review.9
In separate generalized estimating equation models to predict change in BDI-II, SF–36, STAXI, percentage of days with emotional problems, and substance use, smoking cessation status was significant only in the model for alcohol use: less alcohol use was indicated among quitters than among continued smokers. Missing an assessment was related to alcohol, stimulant, and opiate use. Time effects for BDI-II scores and percentage of days with emotional problems indicated significant reductions from baseline levels and no difference by smoking status. Treatment condition was not significant in any of the models as a main effect or in interaction with smoking cessation status.
DISCUSSION
Combined with the treatment outcome data from Hall et al.,4 our findings indicate that individuals who have clinical depression can be helped to stop smoking without adversely affecting their mental health recovery. We used a variety of mental health measures and found no indication of worse outcomes or compensation with other substance use among successful quitters. The only significant group comparison indicated successful quitters had reduced alcohol use relative to continued smokers.
Importantly, both groups exhibited a significant decline in depressive symptoms and days with emotional problems over time. All of the study participants were in active psychiatric outpatient care for depression. Our findings support concurrent treatment for tobacco dependence and depression rather than delaying smoking cessation until the depression resolves.
One limitation of this study is missing data. However, missing status was controlled for in the analyses and was not associated with treatment condition or previous smoking cessation status; thus, it is unlikely that missing data biased the study findings.
Acknowledgments
This work was supported by the National Institute on Drug Abuse (grants K23 DA018691, K05 DA016752, and P50 DA09253) and the State of California Tobacco-Related Disease Research Program (grant 13KT–0152).
Human Participant Protection This study was approved by the University of California, San Francisco institutional review board. Participants provided written informed consent.
Peer Reviewed
Contributors J. Prochaska conceptualized, conducted, and interpreted the data analyses and wrote the article. S. Hall designed and supervised the main study and contributed to the article. J. Tsoh assisted in conceptualization, served as a study therapist, and provided input on the article. S. Eisendrath was lead clinician and supervised antide-pressant treatment at the University of California, San Francisco, site and provided administrative support. J. Rossi and C. Redding developed the expert system and consulted on the data analysis plan and article. A. Rosen supervised implementation of the study at all sites and served as a therapist. M. Meisner was lead investigator at the Kaiser Permanente health management organization sites and provided general and clinical oversight. G. Humfleet helped with study conceptualization and provided clinical guidance during its execution. J. Gorecki assisted with data analyses and provided input on the article.
References
- 1.Stage KB, Glassman AH, Covey LS. Depression after smoking cessation: case reports. J Clin Psychiatry. 1996;57:467–469. [DOI] [PubMed] [Google Scholar]
- 2.Glassman AH, Covey LS, Stetner F, Rivelli S. Smoking cessation and the course of major depression: a follow-up study. Lancet. 2001;357:1929–1932. [DOI] [PubMed] [Google Scholar]
- 3.Tsoh JY, Humfleet GL, Munoz RF, Reus VI, Hartz DT, Hall SM. Development of major depression after treatment for smoking cessation. Am J Psychiatry. 2000;157:368–374. [DOI] [PubMed] [Google Scholar]
- 4.Hall SM, Tsoh JY, Prochaska JJ, et al. Treatment of depressed mental health outpatients for cigarette smoking: a randomized clinical trial. Am J Public Health. 2006;96:1808–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prochaska JJ, Rossi JS, Redding CA, et al. Depressed smokers and stage of change: implications for treatment interventions. Drug Alcohol Depend. 2004; 76:143–151. [DOI] [PubMed] [Google Scholar]
- 6.Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II Manual. San Antonio, Tex: The Psychological Corporation; 1996.
- 7.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, Mass: The Health Institute, New England Medical Center; 1997.
- 8.Spielberger C. State-Trait Anger Expression Inventory, Professional Manual. Research Edition. Odessa, Fla: Psychological Assessment Resources; 1988.
- 9.McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A new measure of substance abuse treatment. Initial studies of the treatment services review. J Nerv Ment Dis. 1992;180:101–110. [DOI] [PubMed] [Google Scholar]


