Abstract
Objectives. We sought to describe health insurance coverage over time among a national sample of children who came into contact with child welfare or child protective services agencies.
Methods. We used data from 4 waves of the National Survey of Child and Adolescent Well-Being to examine insurance coverage among 2501 youths. Longitudinal insurance trajectories were identified using latent class analyses, a technique used to classify individuals into groupings of observed variables, and survey-weighted logistic regression was used to identify variables associated with class membership.
Results. We identified 2 latent insurance classes—1 contained children who gained health insurance, and the other contained children who stably maintained coverage over time. History of sexual abuse, and race/ethnicity other than White, Black, and Hispanic, were associated with membership in the “gainer” class. Foster care placement and poorer health status were associated with membership in the “maintainer” class. Caregiver characteristics were not associated with class membership.
Conclusions. The majority of children in child welfare had stable health insurance coverage over time. Given this vulnerable population’s dependence upon Medicaid, protection of existing entitlements to Medicaid is essential to preserve their stable insurance coverage.
Coverage for children in the child welfare or child protective services system (hereafter termed child welfare) under a health insurance umbrella has been a policy priority for several decades,1 yet relatively little attention has been paid to the stability over time of this insurance coverage. Stable health insurance is critical for these children, who are a highly vulnerable population with considerable physical2–5 and mental health needs.5–8 Currently, there is no information on the extent to which children in child welfare experience stability of health insurance coverage over time.
Children in the child welfare system are dependent upon Medicaid to finance their health needs9 and possess an entitlement to Medicaid based largely upon their residential status or placement. Federal regulations ensure that children who are placed into foster care have categorical eligibility for Medicaid,10 and reportedly 99% of all children in foster care are covered under the program.11 Children maintained within their own homes (in-home) have a Medicaid coverage rate of around 84%. Because there is no categorical entitlement to Medicaid for these children, most of them are covered by income-eligibility rules, or by other local and state regulations.12 But because entitlement to Medicaid is dependent upon the child’s placement status (in-home or in foster care), and because 95% of these children experience changes in placement even as they remain within child welfare,13 it has been suggested that such placement instability can produce instability in Medicaid coverage.14
Somewhat paradoxically for these children, certain types of service utilization can produce insurance loss. In all jurisdictions, youths open to services through child welfare agencies who are then detained or committed to juvenile justice settings face disenrollment from Medicaid because federal law prohibits use of Medicaid funds to serve incarcerated individuals.15,16 The extent to which these youths are successful in re-establishing Medicaid coverage after their release from detention is presently unknown. Funding reductions in the Medicaid program17 and several of the provisions of the Deficit Reduction Act of 200518 can also place children in child welfare at increased risk for disenrollment from Medicaid.
Finally, children in child welfare who have families that receive cash assistance (through Temporary Assistance for Needy Families or food stamps) are at particular risk for Medicaid disenrollment when their families stop receiving these benefits.19,20 Despite the fact that the link between receipt of welfare benefits and Medicaid eligibility was broken in 1997, the existence of administrative data systems that continue to link individuals who receive all forms of public assistance accounts for such insurance loss.
The cumulative effect of these Medicaid and welfare policies is to place children in child welfare at particular risk for insurance instability, the magnitude of which is currently unknown among this population. Data on Medicaid-enrolled children suggest that 13% to 68% have discontinuous insurance coverage in any given year21; approximately 23% of children aged younger than 17 years experience spells of being insured during a 2-year period.22 Longitudinal surveys reveal that 42% of all children spend some time without insurance and 68% of children below 200% of the federal poverty level spend more than 1 year without insurance.23 Insurance instability disproportionately affects children, those from low-income families, minorities, and women leaving welfare programs,24 groups from which many children enter child welfare. Its consequences can be serious—children with discontinuous insurance have higher rates of delayed care, unmet medical needs, and unfilled prescriptions compared with children with uninterrupted private insurance.25 Such consequences are particularly devastating for children in the child welfare system who have very high needs for physical and mental health services.
In an attempt to understand trajectories of insurance coverage possessed by children in the child welfare system, we analyzed nationally representative data on children who came into contact with child welfare agencies and who were then followed for 3 years. We identified child-level (sociodemographic characteristics, maltreatment history, placement, and need) and caregiver-level (education and employment status) variables that may place children at greater risk of insurance instability, to provide child welfare and Medicaid policymakers with information directed toward safeguarding health insurance and, thereby, access to services for this high-need population.
METHODS
Data Sources
The National Survey of Child and Adolescent Well-Being (NSCAW) is the first national probability study of children aged from birth to 14 years who came into contact with child welfare agencies nationwide. In the survey’s baseline wave, 5501 children were sampled in 92 primary sampling units within 97 counties in the United States; all of these children were investigated by their local child protective services for possible abuse and neglect within a 15-month period beginning in October 1999.
We used data from the baseline wave to generate our independent variables, and data from the 12-month (fielded between October 2000 and March 2002), 18-month, and 36-month follow-up waves to obtain information about our dependent variable of insurance coverage. Other details regarding the design and information contained within the NSCAW data are available elsewhere.26 We deleted from our sample all children younger than 2 years because the version of the Child Behavior Checklist (CBCL),27 a measure of need for mental health services that is used in NSCAW, is not normed for that age group. Because of challenges associated with imputing missing data in NSCAW, we used listwise deletion for missing variables; these decisions led to a data set that contained 2501 children, with information from caregivers, caseworkers, and individual children.
Study Variables
Independent variables.
Independent variables included child age, gender, and race/ethnicity. Maltreatment history was obtained from NSCAW’s child welfare worker interviews, and was based on a modified Maltreatment Classification Scale.28 Categories of physical abuse, sexual abuse, neglect, and abandonment were dichotomized such that a child could have more than 1 type of abuse coded. We only coded for neglect if the neglect was at least moderate—failure to ensure availability of food or weather-appropriate clothing, inadequate sleeping arrangements, nonadherence to medication regimens, and failure to change underclothing leading to rashes.
Because of previously cited literature on the relationship between placement and insurance entitlement,11,12 we aggregated children’s placement status into 2 mutually exclusive categories of in-home (living with their permanent primary caregiver, usually their birthparent) and out-of-home (in foster care with either a relative or a nonrelative, or in a group home or residential treatment shelter). Children placed in-home encompassed both those whose families were receiving services from child welfare and those not receiving any services. From NSCAW’s primary caregiver interviews, we obtained data on the caregiver’s highest educational level as well as his or her employment status, given their known effects on securing child health insurance coverage.29
Need can be a cause of stable insurance enrollment; this happens when uninsured children who present to health facilities are enrolled by administrative staff into Medicaid or other forms of insurance. High and ongoing need may also compel caregivers of children to ensure the stability of such coverage. To control for these effects, we constructed 3 variables of emotional or behavioral need, physical health need, and developmental need. Our dichotomous emotional or behavioral need variable was based on the identification of a probable behavioral disorder if the child scored in the clinical range (T score of ≥64) on the internalizing or externalizing scales of the CBCL.27 The CBCL scores were based on reports from the child’s available caregiver, usually the birthparent of children maintained in the home or the temporary caregiver for children placed out of the home.
The CBCL is a well-established measure of childhood behavior problems that has been successfully used in child welfare populations.30–32 The measure for physical health need was based on the 5-point scale that classified self-reported health status into excellent, very good, good, fair, and poor, as used by the National Health Interview Survey since 1982.33 For NSCAW, this information was obtained from the primary caregiver who reported on the health status of the child respondent. We use “poor” and “fair” health status as indicative of needs for physical health services. We followed Stahmer et al.34 in using the Kaufman Brief Intelligence Test35 or the Batelle Developmental Inventory36 to identify developmental need, the Preschool Language Scale–337 to identify language and communication need, and the Vineland Adaptive Behavior Scale screener38 to identify problems with adaptive behaviors, as elicited from available caregivers. We used their cut-point of greater than 2 standard deviations on any of these indices, which suggests significant needs for these services, to generate an indicator variable of developmental need.
Dependent variable.
From NSCAW’s caregiver interviews, we categorized children into mutually exclusive insurance categories of Medicaid, private insurance, federal (Civilian Health and Medical Program of the Uniformed Services), and uninsured. Because of our interest in studying patterns of insurance coverage over time, and because of considerable movement of children among insurance categories, we constructed a binary variable that indicated whether the child was insured at each wave. These 4 indicator variables for insurance coverage, 1 per wave, were used to construct latent insurance trajectories, or patterns of insurance change over time, among this population.
Analyses
We weighted all analyses to account for the complex sampling design of NSCAW, which involved stratification and clustering within primary sampling units (with stratum and primary sampling unit indicators), and varying probabilities of selection (with probability weights).
We performed growth mixture modeling39 with the 4 binary insurance variables described previously to identify classes that could describe trajectories of insurance change over time for NSCAW children. This analytic strategy allowed us to first identify heterogeneous classes, each with a distinct insurance trajectory, and then evaluate the influence of covariates on determination of membership in that class. Classes empirically derived from the data were subject to both statistical measures to assess fit (such as sample size–adjusted Bayesian Information Criterion, entropy [this reflects the quality of classification of individuals into groups], and classification efficiency), as well as the interpretability of these classes, lack of overlap between these classes, and the confidence of the model in assigning individual children into these latent classes.39,40
We tested 2-, 3-, and 4-class models, but chose a 2-class solution based on fit statistics and ease of interpretation. The 4-class model had both a sample size–adjusted Bayesian Information Criterion of 4983.8 (smaller Bayesian Information Criterion values are better), as well as poor entropy of 68.8%. The 3-class solution had good fit statistics and slightly poorer entropy than the 2-class solution, but was less interpretable than the 2-class model. The 2-class solution had slightly poorer fit (size-adjusted Bayesian Information Criterion=5119.7) but very good entropy of 92.9%. All models were fit by using maximum likelihood with robust standard errors, as considered appropriate for binary variables.41
We then developed 2 binary indicator variables, 1 for each of the 2 classes identified by the growth mixture model. These variables were used as dependent variables in separate survey-weighted logistic regression models. We regressed child and caregiver variables on these binary dependent variables in an attempt to identify independent variables associated with membership in each class.
All bivariate (weighted χ2), and survey-weighted regression analyses were performed in Stata version 9 (StataCorp LP, College Station, Tex), and growth mixture modeling was performed in Mplus version 4.1 (Muthén & Muthén, Los Angeles, Calif).
RESULTS
Sample Characteristics
Children in our sample were aged a mean of 8 years (SD = 3.8 years) and were equally divided between the genders. Most children were White (47%), followed by African American (30%), and Hispanic (17%; all percentages weighted). Virtually all children in the sample had a history of abuse or neglect, which included physical abuse (34%), sexual abuse (13%), serious neglect (16%), and abandonment (2%). Most (92%) lived in their own homes, whereas the rest were in family foster care, placed with relatives, or in a congregate care environment. Forty percent reportedly displayed emotional distress as measured by a score in the clinical range on the CBCL’s externalizing scale, and 29% had a clinical score on the CBCL’s internalizing scale. Most (74%) of the children were reported to be in good physical health.
The majority (72%) of children lived with caregivers whose highest level of education was high school or less, 22% lived with caregivers who had an associate degree, and the rest lived with caregivers with undergraduate degrees or higher. Nearly half (43%) of these caregivers worked full time, and 14% worked part time.
Patterns of Insurance Change Over Time
At NSCAW’s wave 1 interview, 10% of children who entered child welfare were uninsured, 63% had Medicaid insurance presumably because of income eligibility, 26% had private insurance, and 0.9% had federal insurance (Figure 1 ▶). Over the 3 years of follow-up, the aggregate percentage of children enrolled in Medicaid increased to 67%, and the percentage of uninsured children declined to 6%.
FIGURE 1—
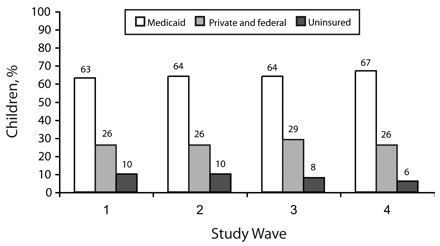
Insurance coverage among 2501 US children in the child welfare system by study wave: National Survey of Child and Adolescent Well-Being, 1999–2004.
Note. All percentages are weighted.
Children, however, displayed considerable child-level heterogeneity in their insurance status over time. Sixty-two percent of children who had been uninsured at wave 1 had secured Medicaid coverage by wave 4. Changes also occurred in the private or federal insurance category—of all children insured by either a private or federal carrier at wave 4, 33% had switched to these carriers from some other insurance category.
These complex and heterogeneous child-level variations in insurance coverage over time were best captured by 2 latent insurance classes (Figure 2 ▶). One class contained children who, on average, gained insurance coverage over the waves of data collection—a class we called the gainers. Children in the other class seemed to successfully maintain insurance coverage over time—we called them the maintainers. Overall, 158 children (7.6%) were gainers, and 2343 (92%) were maintainers. Children in the gainers class had an 89.8% probability of belonging to that class, and those in the maintainers class had a 98.9% probability of belonging to that class, suggesting that these children were appropriately sorted into these classes. These labels described class membership only; individual children in the gainers class included not only those children who secured and maintained coverage, but also those who were episodically insured, with patterns of loss and gain of insurance over time. Similar heterogeneity at the child level may occur within the maintainers class.
FIGURE 2—
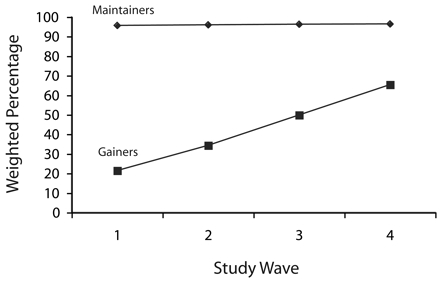
Proportions of 2501 US children in the child welfare system in latent insurance classes, by study wave: National Survey of Child and Adolescent Well-Being, 1999–2004.
Note. Gainers were children who gained insurance coverage over the waves of data collection. Maintainers were children who maintained insurance coverage over time. Sample size-adjusted Bayesian Information Criterion = 5119.7; entropy = 0.93. (Smaller values of Bayesian Information Criterion are better. Entropy indicates quality of classification of individuals who groups, with values close to 1 being beter.)
Characteristics of Gainers and Maintainers
Table 1 ▶ shows bivariate χ2 relationships between child and caregiver characteristics and class membership. Gainers and maintainers did not vary significantly on most characteristics. However, a higher percentage of sexually abused children (18%) were gainers, and maltreatment history was significantly related to class membership. A greater percentage of children placed in foster care at baseline (99%) were members of the maintainers class, as were children reported to be in fair or poor health on their General Health Status measure.
TABLE 1—
Characteristics of US Children in the Child Welfare System (n = 2501) in Each Latent Insurance Class: National Survey of Child and Adolescent Well-Being, 1999–2004
| Variable | Gainer, Unweighted No. (Weighted %) | Maintainer, Unweighted No. (Weighted %) |
| Total | 158 (7.6) | 2343 (92.4) |
| Child characteristics | ||
| Age, y | ||
| 2–5 | 47 (6.3) | 724 (93.7) |
| 6–11 | 68 (6.8) | 1093 (93.2) |
| ≥12 | 43 (11.8) | 526 (88.2) |
| Gender | ||
| Boy | 67 (8.9) | 1099 (91.1) |
| Girl | 91 (6.5) | 1244 (93.5) |
| Race/ethnicity | ||
| African American | 33 (5.3) | 706 (94.7) |
| White | 70 (6.9) | 1107 (93.1) |
| Hispanic | 43 (8.9) | 372 (91.1) |
| Other | 12 (20) | 158 (80) |
| Maltreatment history* | ||
| Physical abuse | 48 (7.6) | 707 (92.4) |
| Sexual abuse | 44 (17.9) | 388 (82.1) |
| Neglect | 19 (5.5) | 348 (94.5) |
| Abandonment | 2 (2.4) | 104 (97.6) |
| Placement** | ||
| In family foster care, placed with relatives, or in group home | 7 (0.9) | 518 (99.1) |
| In own home | 151 (8.2) | 1825 (91.8) |
| Emotional/behavioral need | ||
| ≥64 on the externalizing scale of the CBCL | 60 (6.8) | 976 (93.2) |
| ≥64 on the internalizing scale of the CBCL | 49 (8.4) | 799 (91.6) |
| Physical health need (general health status)* | ||
| Excellent, very good, or good health | 121 (8.6) | 1645 (91.4) |
| Fair or poor health | 37 (4.8) | 698 (95.2) |
| Developmental need | ||
| Score < 2 SD on assessment instruments | 1826 (92.3) | 124 (7.7) |
| Score > 2 SD on assessment instruments | 517 (92.6) | 34 (7.4) |
| Current caregiver characteristics | ||
| Highest educational level | ||
| Less than high school | 52 (7.2) | 654 (92.8) |
| Any high school | 68 (6.7) | 1027 (93.3) |
| High school diploma or any college | 38 (9.6) | 661 (90.4) |
| Employment status | ||
| Full time | 70 (9) | 977 (91) |
| Part time | 27 (6.7) | 333 (93.3) |
| Unemployed | 55 (6.7) | 923 (93.3) |
Note. CBCL = Child Behavior Checklist. Gainers were children who gained insurance coverage over the waves of data collection. Maintainers were children who maintained insurance coverage over time.
* P < .05; **P < .001.
On multivariate analysis (Table 2 ▶), children of “other” race/ethnicity (i.e., not White, Black, or Hispanic) had 3 times the odds of membership in the gainers class compared with Whites, and sexually abused children had 4 times the odds compared with children suffering other types of abuse or neglect. Children in out-of-home placement at wave 1 had 12 times the odds of membership in the maintainers class of children living in their own homes. Each increase in the score on the General Health Status measure (meaning progressively poorer health) produced a 40% increase in the odds of membership in the maintainers class. Caregiver characteristics were not significantly associated with membership in either class.
TABLE 2—
Predictors of Membership in Latent Insurance Classes Among US Children in the Child Welfare System (n = 2501): National Survey of Child and Adolescent Well-Being, 1999–2004
| Variable | Membership in Gainers Class, OR (SE) | Membership in Maintainers Class, OR (SE) |
| Child characteristics | ||
| Age | 1.1 (0.05) | 0.9 (0.04) |
| Gender | ||
| Boy | 1.6 (0.5) | 0.6 (0.2) |
| Girl (Ref) | 1.0 | 1.0 |
| Race/ethnicity | ||
| African American | 0.8 (0.4) | 1.2 (0.6) |
| White (Ref) | 1.0 | 1.0 |
| Hispanic | 1.4 (0.7) | 0.7 (0.3) |
| Other | 3.1* (1.6) | 0.3* (0.2) |
| Maltreatment history | ||
| Physical abuse | 1.2 (0.5) | 0.8 (0.4) |
| Sexual abuse | 4.3** (2.0) | 0.2** (0.1) |
| Neglect | 0.9 (0.4) | 1.1 (0.5) |
| Abandonment | 0.5 (0.4) | 2.2 (1.8) |
| Placement | ||
| In family foster care, placed with relatives, or in group home | 0.1*** (0.05) | 11.8*** (6.9) |
| In own home (Ref) | 1.0 | 1.0 |
| Emotional/behavioral need | ||
| ≥64 on the externalizing scale of the CBCL | 0.8 (0.2) | 1.2 (0.3) |
| ≥64 on the internalizing scale of the CBCL | 1.4 (0.4) | 0.7 (0.2) |
| Presence of physical health need (general health status) | 0.7** (0.1) | 1.4** (0.2) |
| Presence of developmental need | 1.1 (0.4) | 0.9 (0.3) |
| Current caregiver characteristics | ||
| Highest educational level | ||
| Less than high school (Ref) | 1.0 | 1.0 |
| Any high school | 0.9 (0.3) | 1.2 (0.4) |
| High school diploma or any college | 1.0 (0.4) | 1.0 (0.4) |
| Employment status | ||
| Full time | 1.4 (0.5) | 0.7 (0.3) |
| Part time (Ref) | 1.0 | 1.0 |
Note. OR = odds ratio; CBCL = Child Behavior Checklist. For both models F17,68 = 2.7; P = .002. Gainers were children who gained insurance coverage over the waves of data collection. Maintainers were children who maintained insurance coverage over time.
* P < .05; **P < .01; ***P < .001.
DISCUSSION
We have described for the first time longitudinal patterns of health insurance coverage among a nationally representative sample of children in the child welfare system followed up for 3 years. In a testament to the success of policies directed at securing stable insurance coverage for these children,10,11 the majority of these children (92%) maintained some type of health insurance coverage over a 3-year period. There also appeared to be an overall gain of insurance coverage with passage of time within child welfare for the remaining 8% of children (Figure 1 ▶). Although children may not have maintained the same type of health insurance coverage over time, the overall trend in Figure 1 ▶ and other bivariate results suggested that these gains were occurring as a result of enrollments into Medicaid, and aggregate percentages of privately and federally insured children remained relatively stable over time.
This ability to secure insurance coverage may be one mechanism through which child welfare systems obtain health services for their dependants. Although a great deal of the reimbursement for services, especially mental health services, delivered to children in child welfare settings comes from child welfare agencies themselves,42 agencies seem to be also enrolling children into insurance plans. Securing insurance coverage, therefore, may be one way in which entry into child welfare acts as a conduit to services, as has been previously proposed.43
These findings suggested that sexually abused children may have greater rates of entry into health insurance, although the mechanisms that underlie this phenomenon remain unclear. Sexual abuse, in contrast to neglect or abandonment, brings children within defined law enforcement systems, such as children’s advocacy centers that perform forensic interviews, the products of which are subsequently used in criminal proceedings.44–46 Their entry into health insurance, therefore, may be a consequence of increased surveillance necessitated by this specific law-enforcement function. Of greater concern is the finding that history of neglect, physical abuse, and abandonment is not associated with any insurance trajectory over time, despite the considerable service needs of neglected and abused children.47 The implication of these findings is that, absent such defined service pathways for types of maltreatment other than sexual abuse, some form of presumptive eligibility for health insurance is required for all children who come into contact with child welfare agencies to address their physical and mental health needs.
The finding that children in out-of-home placement at wave 1 were more likely to have maintained stable health insurance coverage showed that entitlements were working as intended for these children.11,12 Because of the relatively small number of children who belonged to “other” races/ethnicities (i.e., not White, Black, or Hispanic), our findings on the relationship between race/ethnicity and insurance class should be interpreted with caution.
Our hypothesis that caregiver characteristics would affect insurance coverage was not confirmed in this study. The strongest predictors of insurance coverage seemed to be child-level characteristics. To some extent, this may be reflective of the fact that caregivers and caseworkers of children in the child welfare system changed over time, and although our study allowed for variations in insurance coverage over time, we did not explicitly model change in caregivers and caseworkers for data-related reasons. Longitudinal research that examines changes in caregiver and caseworker agency and their impact on insurance coverage is needed to more fully understand the roles of caregivers and caseworkers.
Limitations
Our study suffered from other limitations. Although our dependent variable was obtained from a technique that incorporated information from all 4 waves of follow-up, our predictors were only obtained from wave 1. Consequently, we were unable to determine the influence of other time-varying events, such as changes in placement over time, on insurance coverage. Future longitudinal data analysis is required to answer such questions. Also, given our emphasis on describing overall insurance patterns and the complexity of trajectories caused by movement between insurance categories, we did not construct separate trajectories for each type of insurance coverage. Our modeling approach also constructed its insurance classes from information available at each of the 4 waves. However, not all children were followed up for all waves, because they were adopted or were lost to follow-up. Consequently, information on class membership was constructed from progressively fewer individuals still retained in the study sample over time. Lastly, insurance was measured at each of the waves and not recorded for the months between waves; hence, brief spells of insurance instability may not have been captured in our analyses.
Conclusions
Despite these limitations, we have presented the first description of health insurance coverage patterns over time among a nationally representative sample of children in the child welfare system. Although the stability of coverage over time was encouraging, these findings support prior work illustrating the dependence of these children on Medicaid.48,49 This dependence on Medicaid may be perilous for children in the welfare system.
In fiscal year 2007, child health insurance programs face a cumulative shortfall of $800 million across 17 states—a situation that can jeopardize stability of Medicaid and State Children’s Heath Insurance Program coverage for children in the welfare system.50 Four key aspects of the Deficit Reduction Act of 2005 (PL 109-171), the greatest restructuring of the Medicaid program at the federal level since its inception, created barriers to Medicaid coverage for children in the welfare system. The Act’s requirement of documentation of citizenship, its creation of “benchmark” benefits as an option to a mandated benefit package, its premium and cost-sharing requirements, and its changes to case management are likely to pose additional challenges to child welfare populations and are likely to increase the burden on child welfare agencies of caring for these children.17,18 At this critical juncture, our findings highlight the fact that insurance coverage for these highly vulnerable children is equally vulnerable and suggest the need to secure Medicaid entitlements for all children in the child welfare system to preserve their access to needed services.
Acknowledgments
This study was supported by the Administration on Children, Youth, and Families, US Department of Health and Human Services (grant 90PH0013). R. Raghavan is an investigator with the Center for Mental Health Services Research, at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (5P30 MH068579).
The authors thank Jinjin Zhang and Peter Dore for assistance with data management; Elliott Smith at the National Data Archive for Child Abuse and Neglect for assistance with data procurement; Susan Ettner, Christopher Wiesen, and Francoise Vermeyen for statistical consultation; and 3 anonymous reviewers for their contributions.
The National Survey of Child and Adolescent Well-Being was developed under contract to the Research Triangle Institute from the Administration on Children, Youth, and Families, US Department of Health and Human Services. The information and opinions expressed herein reflect solely the position of the authors. Nothing herein should be construed to indicate the support or endorsement of its content by the Administration on Children, Youth, and Families, US Department of Health and Human Services.
Human Participant Protection This study was conducted under an exemption from review obtained from the Washington University institutional review board.
Peer Reviewed
Contributors R. Raghavan originated the study, conducted statistical analyses, and led the writing. G. A. Aarons conducted and helped originate the analyses. S. C. Roesch consulted on the analyses. L. K. Leslie assisted with the study and writing. All authors helped to conceptualize ideas, interpret findings, and review drafts of the article.
References
- 1.Small MA. Obstacles and advocacy in children’s mental health services: managing the Medicaid maze. Behav Sci Law. 1991;9:179–188. [DOI] [PubMed] [Google Scholar]
- 2.Schor EL. The foster care system and health status of foster children. Pediatrics. 1982;69:521–528. [PubMed] [Google Scholar]
- 3.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2000;106(suppl 4):909–918. [PubMed] [Google Scholar]
- 4.Halfon N, Klee L. Health services for California’s foster children: current practices and policy recommendations. Pediatrics. 1987;80:183–191. [PubMed] [Google Scholar]
- 5.Halfon N, Mendonca A, Berkowitz G. Health status of children in foster care. The experience of the Center for the Vulnerable Child. Arch Pediatr Adolesc Med. 1995;149:386–392. [DOI] [PubMed] [Google Scholar]
- 6.Pilowsky D. Psychopathology among children placed in family foster care. Psychiatr Serv. 1995;46:906–910. [DOI] [PubMed] [Google Scholar]
- 7.Burns BJ, Phillips SD, Wagner HR, et al. Mental health need and access to mental health services by youths involved with child welfare: a national survey. J Am Acad Child Adolesc Psychiatry. 2004;43: 960–970. [DOI] [PubMed] [Google Scholar]
- 8.Landsverk J, Garland AF, Leslie LK. Mental health services for children reported to Child Protective Services. In: Myers JEB, Berliner L, Briere J, Hendrix CT, Jenny C, Reid TA, eds. APSAC Handbook on Child Maltreatment. Thousand Oaks, Calif: Sage; 2002.
- 9.English A, Freundlich M. Medicaid: a key to health care for foster children and adopted children with special needs. Clgh Rev. 1997;106:109–131. [Google Scholar]
- 10.Centers for Medicare and Medicaid Services, US Depatment of Health and Human Services. Medicaid eligibility: mandatory eligibility groups. Available at: http://www.cms.hhs.gov/MedicaidEligibility/03_MandatoryEligibilityGroups.asp#TopOfPage. Accessed May 23, 2006.
- 11.Geen R, Sommers A, Cohen M. Medicaid Spending on Foster Children. Washington, DC: Urban Institute; 2005.
- 12.Libby AM, Kelleher KJ, Leslie LK, et al. Child welfare systems policies and practices affecting Medicaid health insurance for children: a national study. In press.
- 13.James S, Landsverk J, Slymen DJ, Leslie LK. Predictors of outpatient mental health service use—the role of foster care placement change. Ment Health Serv Res. 2004;6:127–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leslie LK, Kelleher KJ, Burns BJ, Landsverk J, Rolls JA. Foster care and Medicaid managed care. Child Welfare. 2003;82:367–392. [PubMed] [Google Scholar]
- 15.Evans Cuellar A, Kelleher KJ, Rolls JA, Pajer K. Medicaid insurance policy for youths involved in the criminal justice system. Am J Public Health. 2005;95:1707–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koppelman J. Children with mental disorders: making sense of their needs and the systems that help them. NHPF Issue Brief. 2004;(799):1–24. [PubMed]
- 17.Rubin DM, Halfon N, Raghavan R, Rosenbaum S. Protecting Children in Foster Care: Why Proposed Medicaid Cuts Harm Our Nation’s Most Vulnerable Youth. Seattle, Wash: Casey Family Programs; 2005.
- 18.Rubin DM, Halfon N, Raghavan R, Rosenbaum S, Johnson K. The Deficit Reduction Act of 2005: Implications for Children Receiving Child Welfare Services. Seattle, Wash: Casey Family Programs; 2006.
- 19.Summer L, Mann C. Instability of public health insurance coverage for children and their families: causes, consequences, and remedies. Issue Brief (Commonw Fund). 2006.
- 20.Kronebusch K. Medicaid for children: federal mandates, welfare reform, and policy backsliding. Health Aff (Millwood). 2001;20:97–111. [DOI] [PubMed] [Google Scholar]
- 21.Fairbrother G, Jain A, Park HL, Massoudi MS, Haidery A, Gray BH. Churning in Medicaid managed care and its effect on accountability. J Health Care Poor Underserved. 2004;15:30–41. [DOI] [PubMed] [Google Scholar]
- 22.Klein K, Glied S, Ferry D. Entrances and exits: health insurance churning, 1998–2000. Issue Brief (Commonw Fund). 2005;(855):1–12. [PubMed]
- 23.Short PF, Graefe DR, Schoen C. Churn, churn, churn: how instability of health insurance shapes America’s uninsured problem. Issue Brief (Commonw Fund). 2003;(688):1–16. [PubMed]
- 24.Anderson SG, Eamon MK. Health coverage instability for mothers in working families. Soc Work. 2004; 49:395–405. [DOI] [PubMed] [Google Scholar]
- 25.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353:382–391. [DOI] [PubMed] [Google Scholar]
- 26.Dowd K, Kinsey S, Wheeless A, et al. National Survey of Child and Adolescent Well-Being: Combined Waves 1–4, Data File User’s Manual. Ithaca, NY: National Data Archive on Child Abuse and Neglect; 2006.
- 27.Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington: Dept of Psychiatry, University of Vermont; 1983.
- 28.Manly JT, Cicchetti D, Barnett D. The impact of subtype, frequency, chronicity, and severity of child maltreatment on social competence and behavior problems. Dev Psychopathol. 1994;6:121–143. [Google Scholar]
- 29.Heck KE, Makuc DM. Parental employment and health insurance coverage among school-aged children with special health care needs. Am J Public Health. 2000;90:1856–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garland AF, Landsverk JL, Hough RL, Ellis-MacLeod E. Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse Negl. 1996;20:675–688. [DOI] [PubMed] [Google Scholar]
- 31.Zima BT, Bussing R, Yang X, Belin TR. Help-seeking steps and service use for children in foster care. J Behav Health Serv Res. 2000;27:271–285. [DOI] [PubMed] [Google Scholar]
- 32.Kolko DJ, Baumann BL, Caldwell N. Child abuse victims’ involvement in community agency treatment: service correlates, short-term outcomes, and relationship to reabuse. Child Maltreat. 2003;8:273–287. [DOI] [PubMed] [Google Scholar]
- 33.Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Vol 10. Hyattsville, Md: National Center for Health Statistics; 1999. [PubMed]
- 34.Stahmer AC, Leslie LK, Hurlburt M, et al. Developmental and behavioral needs and service use for young children in child welfare. Pediatrics. 2005;116:891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test (K-BIT). Circle Pines, Minn: American Guidance Service; 1990.
- 36.Newborg J, Stock JR, Wnek L, Guidubaldi J, Svinicki J. Battelle Developmental Inventory. Itasca, Ill: Riverside Publishing; 1984.
- 37.Zimmerman I, Steiner V, Pond R. Preschool Language Scale-3. San Antonio, Tex: Psychological Corporation; 1992.
- 38.Sparrow SS, Balla DA, Cicchetti DV. Vineland Adaptive Behavior Scales: Interview Edition, Survey Form Manual. Circle Pines, Minn: American Guidance Service; 1984.
- 39.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24:882–891. [PubMed] [Google Scholar]
- 40.Muthén BO, Muthén LK. The development of heavy drinking and alcohol-related problems from ages 18 to 37 in a US national sample. J Stud Alcohol. 2000;61:290–300. [DOI] [PubMed] [Google Scholar]
- 41.Chou CP, Bentler PM, Satorra A. Scaled test statistics and robust standard errors for non-normal data in covariance structure analysis: a Monte Carlo study. Br J Math Stat Psychol. 1991;44:347–357. [DOI] [PubMed] [Google Scholar]
- 42.McCarthy J. Health Care Reform Tracking Project 2003 State Survey, Child Welfare Special Analysis. Tampa, Fla: Research and Training Center for Children’s Mental Health, University of South Florida; 2005.
- 43.Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang J. Relationship between entry into child welfare and mental health service use. Psychiatr Serv. 2005;56:981–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carnes CN, Nelson-Gardell D, Wilson C. Addressing challenges and controversies in child sexual abuse interviewing: the forensic evaluation protocol and research project. J Aggression Maltreat Trauma. 1999;2:83–103. [Google Scholar]
- 45.Carnes CN, Wilson C, Nelson-Gardell D. Extended forensic evaluation when sexual abuse is suspected: a model and preliminary data. Child Maltreat. 1999;4:242–254. [DOI] [PubMed] [Google Scholar]
- 46.Cramer RE. A community approach to child sexual abuse: the role of the office of the district attorney. Response Victimization Women Child. 1986;9:10–13. [Google Scholar]
- 47.Pecora PJ, Whittaker JK, Maluccio AN, Barth RP. The Child Welfare Challenge: Policy, Practice, and Research. 2nd ed. New York, NY: Aldine de Gruyter; 2000.
- 48.Raghavan R, Leibowitz AA. Medicaid and mental health care for children in the child welfare system. In: Haskins R, Wulczyn F, Webb MB, eds. Child Protection: Using Research to Improve Policy and Practice. Washington, DC: Brookings Press; 2007: 120–139.
- 49.Raghavan R, Leibowitz AA, Andersen RM, Zima BT, Schuster MA, Landsverk J. Effects of Medicaid managed care policies on mental health service use among a national probability sample of children in the child welfare system. Child Youth Serv Rev. 2006; 28:1482–1496. [Google Scholar]
- 50.The number of uninsured Americans is at an all-time high [news release]. Washington, DC: Center on Budget and Policy Priorities; August 29, 2006. Available at: http://www.cbpp.org/8-29-06health.pdf. Accessed November 17, 2007.


